Abstract
Objective
Addiction is often considered a dissociative behavior that is related to alexithymia and developmental trauma. The study aims were to explore the relationships between early trauma, alexithymia, and dissociation.
Methods
A total of 117 (males=60; females=57) alcohol-addicted individuals and 117 healthy individuals (males=60; females=57) were administered a series of self-report questionnaires that assess traumatic experiences, alexithymia, and pathological dissociation.
Results
Correlation analyses indicated significant correlations between alexithymia, dissociation, and trauma and a significant difference between the target and control groups, with higher alexithymia and dissociation scores in the target group.
Conclusion
These findings suggest that trauma, alexithymia, and dissociation are predictors of alcohol addiction.
Keywords: Alcohol addiction, Dissociation, Alexithymia, Early trauma
INTRODUCTION
Alcohol addiction is a major public health issue worldwide1 and is associated with a range of psychiatric disorders.2,3,4 Research has indicated that childhood trauma is a predictor of the co-occurrence of trauma-related disorders5,6,7 and alcohol dependence.8,9 Several studies have shown a relationship between alcohol dependence, post-traumatic stress disorder,10,11,12,13,14 and dissociation.9,10,11,12,13,14,15,16,17 Alcohol abuse may, therefore, constitute one component of a constellation of psychopathological responses to trauma.12
Early trauma disturbs the development of cognitive and affective processing, the integration of thinking and feeling, and the capacity to understand and express emotional states; these disturbances are linked to post-traumatic reactions, dissociation, and alexithymia.18,19 Alexithymia is a multifaceted construct that represents difficulty in identifying, describing, and analyzing emotions and an externally oriented cognitive style.20 The inability to identify or name emotions, coupled with the feeling of being overwhelmed, may cause individuals to experience trauma. These individuals may become accustomed to expressing their affect21 through the development of a compensatory, non-verbal strategy, such as pathological drinking, to disrupt a sense of psychological numbing and/or to avoid and manage intense, seemingly uncontrollable emotions.18
Recently, alexithymia has been examined as a possible predictor of dissociative tendencies.8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25 Indeed, some theorists have suggested that alexithymia may be a reaction to early interpersonal traumas, such as abuse,26 and is a dysfunctional coping mechanism that "numbs"21 the buffer between bodily sensations and emotions.27 This numbness has often been observed in individuals with dissociative disorders. Higher rates of illness, anxiety,28,29 and depression have consistently been linked with the traumatic triad of alexithymia, alcohol, and dependency.30,31,32
Dissociation may interfere with the connections between affects, cognitions, and voluntary behavior control by influencing the development of alexithymia and resulting in the "dissociation" of the physiological, cognitive, and affective components of emotions. Both dissociation and alexithymia have been considered impairments of emotive perception that help trauma survivors manage overwhelming or difficult affective states.33 Several studies have investigated the impact of trauma on alexithymia.34,35 In some cases, including in a study on dissociation,17 the emotional experience itself was influenced.36 Frewen and colleagues37 conducted a meta-analysis that showed that individuals with post-traumatic stress disorder (PTSD) have a greater difficulty in identifying, describing, and experiencing emotions compared to individuals with no PTSD symptoms.
However, little is known about the interplay between early trauma, alexithymia, and dissociation. Research has yet to clarify the direction of causality and the specific role of dissociation in the development of alexithymia or vice versa.38 The current study aimed to explore the incidence of early trauma, alexithymia, and dissociation and to better understand the interaction between alexithymia, dissociation, and trauma in a sample of individuals with alcohol abuse. This population was selected because several studies have found that alcohol-dependent individuals often present a history of early trauma (mainly childhood abuse and neglect) in conjunction with alexithymic traits and dissociative tendencies.39,40 The present study's main hypothesis was that alexithymia and dissociation would be associated with alcohol consumption and severity in individuals with a history of trauma. Furthermore, it was hypothesized that a higher prevalence of a traumatic history, alexithymia, and dissociation would present in the alcohol-dependent group compared to a control group of healthy individuals.
METHODS
Participants
The study population was selected from patients with an alcohol problem who had consulted local Mental Health Departments clinics in a city of Southern Italy as well as individuals without the disorder who inhabited the city. The inclusion criterion consisted of a diagnosis of alcohol-dependence in accordance with the DSM-IV-TR41 criteria. All participants were evaluated before pharmacotherapy (including anti-craving medication) was introduced. Exclusion criteria included a co-morbid psychiatric disorder (e.g., schizophrenia), an organic brain syndrome, and poly-substance use.
The final sample included 234 individuals (120 males and 114 females). Participants were divided into two groups, a target group and a control group. The target group consisted of 117 participants who were recruited from an outpatient program for alcohol-dependence in Southern Italy (males=60, females=57), with an age range from 19 years to 66 years (M=44.85; SD=9.94). In this group, 62 (53%) had graduated from primary school, 48 (41%) had graduated from high school, and 7 (6%) were university graduates. The control group matched the target group on gender (males=60, females=57), with an age range from 20 years to 66 years (M=43.98; SD=9.57). The level of education in the control group was higher than that in the target group, as 84 (72%) had graduated from high school and 33 (28%) were university graduates. The control group consisted of volunteers who were self-declared non-drinkers. The data showed no significant age difference between the target and control groups [t(116)=0.697, p=0.487].
Measures
The Dissociative Experiences Scale-II (DES-II)42 is a 28-item self-report scale. This scale is not a diagnostic tool; rather, it serves as a screening device for chronic dissociative disorders. Respondents are asked to rate various dissociative experiences that occur in their daily life when they are not under the influence of alcohol or drugs. The reliability and validity of the Italian version of this scale are as high as those of the original form,43 with a good Cronbach's alpha (0.81-0.94). Scores range from 0% to 100%, with a cut-off of ≥30% representing potential dissociative mental states.
The Toronto Alexithymia Scale-20 (TAS-20)44 is a 20-item self-report that assesses alexithymia. It has a three-factor structure, as follows: 1) Difficulty Identifying Feelings (DIF); 2) Difficulty Describing Feelings (DDF); 3) Externally Oriented Thinking (EOT). Cut-off scores have been established to categorize individuals as alexithymic (≥61), borderline (52-60), and non-alexithymic (≤51). The TAS-20 has shown adequate validity and reliability (α=0.81; r=0.77). The Italian version45 also demonstrates good internal consistency (Cronbach's alpha of 0.75 and 0.82 in normal and clinical groups, respectively).
The Traumatic Experiences Checklist (TEC)46 is a self-report measure that assesses 29 potentially traumatizing events, such as emotional abuse, neglect, sexual assault, and physical abuse. The TEC also addresses trauma severity across the following four variables: 1) event occurrence; 2) early traumatic experiences; 3) the duration of trauma; 4) subjective reaction to trauma.
Procedure
Alcohol-dependent participants were recruited from NHS outpatient clinics for substance abuse treatment in a region of Southern Italy. The control group included normal subjects who were matched on age and sex. A plain language statement was attached to the front of the questionnaires to explain the nature of the study. Participants were asked to be as honest and spontaneous as possible in their responses and were assured of anonymity and confidentiality. Participants returned their completed questionnaires to health professionals at the outpatient clinics or to a university office in a sealed envelope supplied by the researcher. All participants provided informed consent and were given the opportunity to withdraw from the study at any time. Furthermore, participants were later debriefed about the study by NHS staff. The study obtained ethics approval from the university that employed the principal investigator and the NHS ethics committee.
Data analysis
The statistical package SPSS 18 for Windows was used for all analyses (SPSS, Chicago, IL, USA).
Descriptive statistics were performed across all study variables. A paired t-test was used to compare the two groups.
A series of two-tailed Pearson linear correlations were conducted to test the relationships between variables.
Furthermore, a stepwise linear regression was used to analyze the relationship between variables.
RESULTS
In the target group, the TAS-20 mean score (Table 1) showed a borderline alexithymia threshold (M=58.92, SD=15.19). By contrast, the control group presented a mean score below the cut-off for alexithymia (M=47.24, SD=13.35).
Table 1.
Mean differences in trauma, alexithymia, and dissociation between the two groups of participants
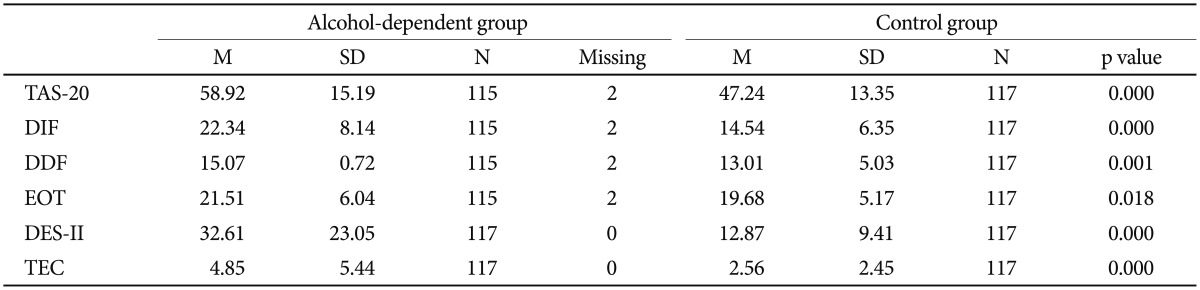
TAS-20: Twenty-Item Toronto Alexithymia Scale, DIF: difficulty modulating and identifying feelings, DDF: difficulty describing one's feelings to others, EOT: externally oriented thinking, DES-II: Dissociative Experiences Scale, TEC: Traumatic Experiences Checklist
Half of the target group (N=58, 49.57%; 22 males, 36%; 36 females, 64%) had alexithymia (TAS-20 total score ≥61). Chi square tests revealed an effect of gender on both the TAS-20 total score (χ2=9.45, df=1, p=0.002) and the Difficulty Identifying Feelings score (χ2=17.26, df=1, p<0.001). By contrast, only 18 individuals in the control group (7 males, 11.6%; 11 females, 19.2%) displayed alexithymic symptoms. In this group, there were no gender differences in the TAS-20 total score or its three factors (Table 2).
Table 2.
Mean differences in trauma, alexithymia, and dissociation between males and females of the two groups
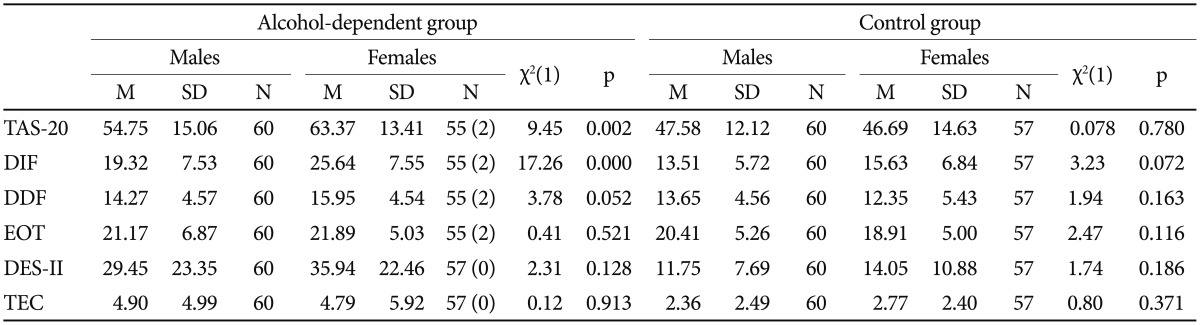
TAS-20: Twenty-Item Toronto Alexithymia Scale, DIF: difficulty modulating and identifying feelings, DDF: difficulty describing one's feelings to others, EOT: externally oriented thinking, DES-II: Dissociative Experiences Scale, TEC: Traumatic Experiences Checklist
For the DES-II scores, the target group displayed a mean score (M=32.61; SD=23.05) above the clinical cut-off, whereas the mean score of the control group was under the clinical cut-off (M=12.87; SD=9.41) [t(116)=8.32, p<0.001]. There were no significant gender differences within the two groups (χ2=ns).
The TEC total score indicated a higher prevalence of traumatic events in the target group (M=4.85, SD=5.44) compared to the control group [M=2.56, SD=2.45; t(116)=4.09, p<0.001]. In particular, emotional abuse [t(116)=3.61, p<0.001] and physical abuse [t(116)=3.40, p<0.001] showed significant differences. Alcohol-dependent individuals (M=11.85, SD=9.65) had experienced a traumatic event at an earlier age than controls (M=18.24, SD=12.40) [t(80)=-4.13, p<0.001]. There were no significant gender differences in the typology of trauma within the two groups.
Correlations among variables in the alcohol-dependent group
The TEC total score was positively correlated with only the DES-II (r=0.22, p<0.05). With respect to specific types of traumatic experiences, we found significant correlations (Table 3) between emotional abuse and dissociation (r=0.28, p<.01), physical abuse and the DDF TAS-20 factor (r=0.22, p<0.05), physical abuse and dissociation (r=0.22, p<0.05), sexual abuse and the TAS-20 total score (r=0.31, p<0.01), sexual abuse and the DDF (r=0.31, p<0.01), and sexual abuse and the EOT (r=0.36, p<0.01). Dissociation was positively correlated with the TAS-20 total score (r=0.60, p<0.01) and the three TAS-20 subscales (DIF, r =0.49, p<0.01; DDF, r=0.38, p<0.01; EOT, r=0.56, p<0.01). An interesting outcome was the negative correlation between dissociation and early traumatic experiences (r=-0.35, p<0.01).
Table 3.
Correlation matrix for all variables in the alcohol-dependent group
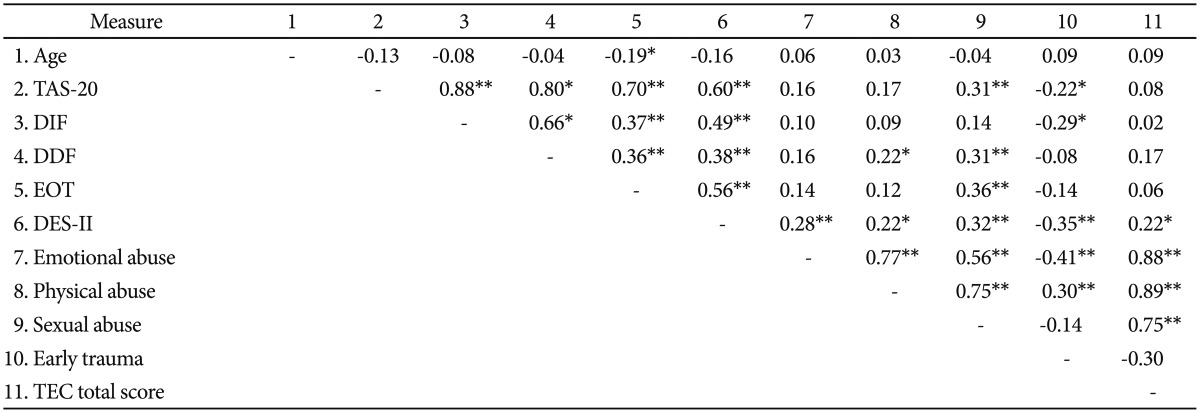
*all coefficients are significant at the 0.05 level, **all coefficients are significant at the 0.01 level. TAS-20: Twenty-Item Toronto Alexithymia Scale, DIF: difficulty modulating and identifying feelings, DDF: difficulty describing one's feelings to others, EOT: externally oriented thinking, DES-II: Dissociative Experiences Scale, TEC: Traumatic Experiences Checklist
Correlations among variables in the control group
The data showed that dissociation was significantly and positively correlated with the TAS-20 total score (r=0.36, p<0.001) and the DIF (r=0.450, p<0.001) and DFF (r=0.21, p<0.05) TAS-20 factors. In the target group, the TEC total score was correlated with both the DIF TAS-20 factor and the DES-II (Table 4). In regards to traumatic experiences, we observed a significant correlation between the DES-II and emotional trauma.
Table 4.
Correlation matrix for all variables in the control group
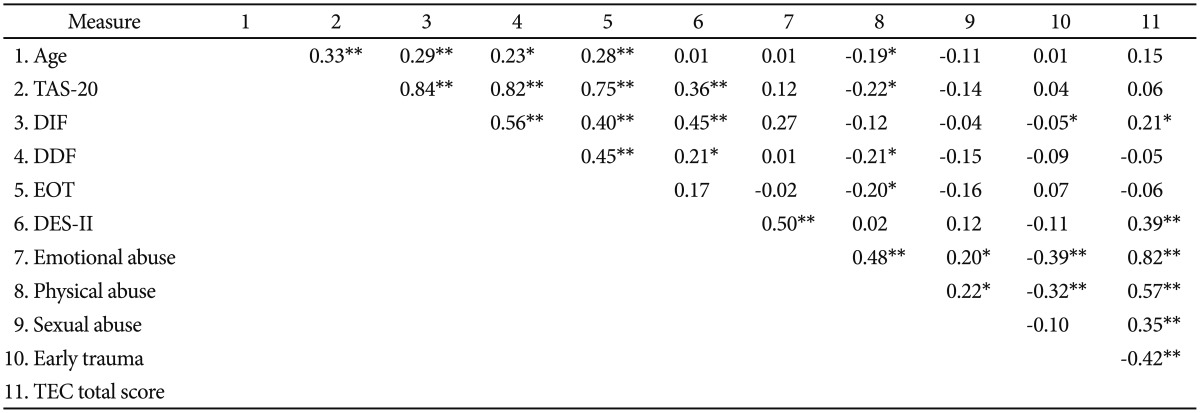
*all coefficients are significant at the 0.05 level, **all coefficients are significant at the 0.01 level. TAS-20: Twenty-Item Toronto Alexithymia Scale, DIF: Difficulty modulating and identifying feelings, DDF: difficulty describing one's feelings to others, EOT: externally oriented thinking, DES-II: Dissociative Experiences Scale, TEC: Traumatic Experiences Checklist
Predictive relationships among variables in the two groups
A stepwise regression linear showed that the TAS-20 total score predicted dissociation in the target group (F=65.40, df=1, adjusted R2=0.361, p<0.001). In the control group, only the DIF TAS-20 factor was a good predictor of dissociation (F=29.24, df=1, adjusted R2=0.196, p<0.001) (Table 2).
DISCUSSION
This study confirmed the existing research regarding the role of trauma in addiction behavior.15,47,48 Alcohol dependency can be considered a dissociative reaction of individuals with difficulties in identifying, expressing, and regulating emotions. The present findings also showed that age at first traumatic experience (in particular, emotional abuse) plays a major role in activating dissociative reactions (such as, dissociative defense mechanisms and pathological alcohol consumption).49,50,51,52,53,54 Alexithymia, dissociation, and trauma are interrelated among individuals with alcoholism. This triad's relevance for the prevention and treatment of alcohol dependence requires attention in future studies. The current results suggest that addictive behaviors have a dissociative nature that allows individuals to manage negative and unregulated emotions.
The present study measured chronic (trait) dissociation rather than acute and transient dissociative states. Although chronic dissociation contributes to difficulties in identifying feelings, chemically (alcohol-induced) transient dissociative states may be a paradoxical effort to identify and express feelings that are otherwise difficult to access. Thus, alcohol appears to influence the interplay between trauma, dissociation, and alexithymia. This interplay may be an important factor in the prevention and treatment of alcoholism in the addicted population.
Given that this study was cross-sectional, the long-term stability of these findings requires further inquiry. Future research should also explore whether female patients display dissociative experiences and alexithymia profiles that differ from those of male patients.
References
- 1.Harper C, Matsumoto I. Ethanol and brain damage. Curr Opin Pharmacol. 2005;5:73–78. doi: 10.1016/j.coph.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 2.Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings. Clin Psychol Rev. 2000;20:149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- 3.Lyne JP, O'Donoghue B, Clancy M, O'Gara C. Comorbid psychiatric diagnoses among individuals presenting to an addiction treatment program for alcohol dependence. Subst Use Misuse. 2011;46:351–358. doi: 10.3109/10826081003754757. [DOI] [PubMed] [Google Scholar]
- 4.Walvoort SJW, Wesyer AJ, Egger JIM. Assessment of psychopathology and personality with the MMPI-2 in Patients with alcohol use disorder (AUD): should we not correct for associated cognitive dysfunctions? Clin Neuropsychiatry. 2012;9:212–220. [Google Scholar]
- 5.Gershuny BS, Thayer JF. Relations among psychological trauma, dissociative phenomena, and trauma-related distress: a review and integration. Clin Psychol Rev. 1999;19:631–657. doi: 10.1016/s0272-7358(98)00103-2. [DOI] [PubMed] [Google Scholar]
- 6.Chu JA, Dill DL. Dissociative symptoms in relation to childhood physical and sexual abuse. Am J Psychiatry. 1990;147:887–892. doi: 10.1176/ajp.147.7.887. [DOI] [PubMed] [Google Scholar]
- 7.Craparo G. Internet addiction, dissociation, and alexithymia. Procedia Soc Behav Sci. 2011;30:1051–1056. [Google Scholar]
- 8.Zlotnick C, Shea MT, Pearlstein T, Simpson E, Costello E, Begin A. The relationship between dissociative symptoms, alexithymia, impulsivity, sexual abuse, and self-mutilation. Compr Psychiatry. 1996;37:12–16. doi: 10.1016/s0010-440x(96)90044-9. [DOI] [PubMed] [Google Scholar]
- 9.Evren C, Sar V, Evren B, Semiz U, Dalbudak E, Cakmak D. Dissociation and alexithymia among men with alcoholism. Psychiatry Clin Neurosci. 2008;62:40–47. doi: 10.1111/j.1440-1819.2007.01775.x. [DOI] [PubMed] [Google Scholar]
- 10.Chilcoat H, Menard C. Epidemiological Investigations: Comorbidity of Posttraumatic Stress Disorder and Substance Use Disorder. In: Ouimette P, Brown PJ, editors. Trauma and Substance Abuse: Causes, Consequences and Treatment of Comorbid Disorders. Washington, DC: American Psychological Publishing; 2003. pp. 9–28. [Google Scholar]
- 11.Faraci P, Craparo G, Messina R, Severino S. Internet Addiction Test (IAT): which is the best factorial solution? J Med Internet Res. 2013;15:e225. doi: 10.2196/jmir.2935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foa EB, Williams MT. Methodology of a randomized double-blind clinical trial for comorbid posttraumatic stress disorder and alcohol dependence. Ment Health Subst Use. 2010;3:131–147. doi: 10.1080/17523281003738661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Craparo G, Faraci P, Rotondo G, Gori A. The Impact of Event Scale - Revised: psychometric properties of the Italian version in a sample of flood victims. Neuropsychiatr Dis Treat. 2013;9:1427–1432. doi: 10.2147/NDT.S51793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bermond B, Moormann PP, Albach F, van Dijke A. Impact of severe childhood sexual abuse on the development of alexithymia in adulthood. Psychother Psychosom. 2008;77:260–262. doi: 10.1159/000128167. [DOI] [PubMed] [Google Scholar]
- 15.Schäfer I, Langeland W, Hissbach J, Luedecke C, Ohlmeier MD, Chodzinski C, et al. Childhood trauma, dissociation and posttraumatic stress disorder in patients with alcohol dependence, drug dependence or both - a multi-center study. Drug Alcohol Depend. 2010;109:84–89. doi: 10.1016/j.drugalcdep.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Franzoni E, Gualandi S, Caretti V, Schimmenti A, Di Pietro E, Pellegrini G, et al. The relationship between alexithymia, shame, trauma, and body image disorders: investigation over a large clinical sample. Neuropsychiatr Dis Treat. 2013;9:185–193. doi: 10.2147/NDT.S34822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craparo G. Addiction, dissociation, and the unrepressed unconscious. A theoretical contribution from a developmental-relational perspective. Ric Psic. 2013;2:73–84. [Google Scholar]
- 18.Yates TM. Developmental Pathways from Child Maltreatment to Nonsuicidal Self-Injury. In: Nock MK, editor. Understanding Nonsuicidal Self-Injury: Origins, Assessment and Treatment. Washington, DC: American Psychological Association; 2009. pp. 117–137. [Google Scholar]
- 19.Craparo G, Faraci P, Fasciano S, Carrubba S, Gori A. A factor analytic study of the Boredom Proneness Scale (BPS) Clin Neuropsychitary. 2013;10:164–170. [Google Scholar]
- 20.Nemiah JC, Freyberger H, Sifneos PE. Alexithymia: A View of the Psychosomatic Process. In: Hill OW, editor. Modern Trends in Psychosomatic Medicine, Vol. 3. London: Butterworths; 1976. pp. 430–439. [Google Scholar]
- 21.van der Kolk BA, McFarlane AC, Weisaeth L. Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body, and Society. New York: Guilford Press; 1996. [Google Scholar]
- 22.Berenbaum H, James T. Correlates and retrospectively reported antecedents of alexitymia. Psychosom Med. 1994;56:353–359. doi: 10.1097/00006842-199407000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Craparo G, Faraci P, Fasciano S, Carrubba S, Gori A. A factor analytic study of the Boredom Preneness Scale (BPS) Clin Neuropsychiatry. 2013;10:164–170. [Google Scholar]
- 24.Elzinga BM, Bermond B, van Dyck R. The relationship between dissociative proneness and alexithymia. Psychother Psychosom. 2002;71:104–111. doi: 10.1159/000049353. [DOI] [PubMed] [Google Scholar]
- 25.Grabe HJ, Spitzer C, Freyberger HJ. Alexithymia and the temperament and character model of personality. Psychother Psychosom. 2001;70:261–267. doi: 10.1159/000056264. [DOI] [PubMed] [Google Scholar]
- 26.Berenbaum H. Childhood abuse, alexithymia and personality disorder. J Psychosom Res. 1996;41:585–595. doi: 10.1016/s0022-3999(96)00225-5. [DOI] [PubMed] [Google Scholar]
- 27.Wise TN, Mann LS, Sheridan MJ. Relationship between alexithymia, dissociation and personality in psychiatric out patients. Psychother Psychosom. 2000;69:123–127. doi: 10.1159/000012379. [DOI] [PubMed] [Google Scholar]
- 28.Fukunishi I, Rahe RH. Alexithymia and coping with stress in healthy persons: alexithymia as a personality trait is associated with low social support and poor responses to stress. Psychol Rep. 1995;76:1299–1304. doi: 10.2466/pr0.1995.76.3c.1299. [DOI] [PubMed] [Google Scholar]
- 29.Gori A, Giannini M, Socci S, Luca M, Dewey D, Schuldberg D, et al. Assessing social anxiety disorder: psychometric properties of the Italian social phobia inventory (I-SPIN) Clin Neuropsychitary. 2013;10:37–42. [Google Scholar]
- 30.Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamäki H. Depression is strongly associated with alexithymia in the general population. J Psychosom Res. 2000;48:99–104. doi: 10.1016/s0022-3999(99)00083-5. [DOI] [PubMed] [Google Scholar]
- 31.Marchesi C, Brusamonti E, Maggini C. Are alexithymia, depression, and anxiety distinct constructs in affective disorders? J Psychosom Res. 2000;49:43–49. doi: 10.1016/s0022-3999(00)00084-2. [DOI] [PubMed] [Google Scholar]
- 32.Thorberg FA, Young RM, Sullivan KA, Lyvers M. Alexithymia and alcohol use disorders: a critical review. Addict Behav. 2009;34:237–245. doi: 10.1016/j.addbeh.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 33.Sayar K, Kose S, Grabe HJ, Topbas M. The relationship between alexithymia and dissociation in an adolescent sample. Psychiatry Clin Neurosci. 2005;59:127–134. doi: 10.1111/j.1440-1819.2005.01346.x. [DOI] [PubMed] [Google Scholar]
- 34.Goldsmith R, Freyd JJ. Awareness for emotional abuse. J Emot Abuse. 2005;5:95–123. [Google Scholar]
- 35.Zlotnick C, Mattia J, Zimmerman M. The relationship between posttraumatic stress disorder, childhood trauma and alexithymia in an outpatient sample. J Trauma Stress. 2001;14:177–188. [Google Scholar]
- 36.Foa EB, Hearst-Ikeda D. Emotional Dissociation in Response to Trauma: An Information; Processing Approach. In: Michelson LK, Ray WJ, editors. Handbook of Dissociation: Theoretical, Empirical, and Clinical Perspectives. NewYork: Plenum Press; 1996. pp. 207–224. [Google Scholar]
- 37.Frewen PA, Dozois DJA, Neufeld RWJ, Lanius RA. Meta-analysis of alexithymia in posttraumatic stress disorder. J Trauma Stress. 2008;21:243–246. doi: 10.1002/jts.20320. [DOI] [PubMed] [Google Scholar]
- 38.Irwin HJ, Melbin-Helberg EB. Alexithymia and dissociative tendencies. J Clin Psychol. 1997;53:159–166. doi: 10.1002/(sici)1097-4679(199702)53:2<159::aid-jclp9>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 39.Bujarski S, Klanecky AK, McChargue DE. The relationship between alexithymia and alcohol-related risk perceptions: the moderating effect of general trauma in a college population. Addict Behav. 2010;35:363–366. doi: 10.1016/j.addbeh.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 40.Klanecky AK, Harrington J, McChargue DE. Child sexual abuse, dissociation, and alcohol: Implications of chemical dissociation via blackouts among college women. Am J Drug Alcohol Abuse. 2008;34:277–284. doi: 10.1080/00952990802013441. [DOI] [PubMed] [Google Scholar]
- 41.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition, Text revision. Washington D.C: American Psychiatric Press Inc; 1994. [Google Scholar]
- 42.Carlson EB, Putnam FW. An update on the dissociative experiences scale. Dissociation. 1993;6:16–27. [Google Scholar]
- 43.Schimmenti A, Craparo G, Caretti V. Validity and reliability of the Revised Dissociative Experience Scale (DES-II) in an Italian sample. Unpublished manuscript. Faculty of Human and Social Sciences, Kore University, Enna; [Google Scholar]
- 44.Bagby RM, Taylor GJ, Parker JD. The Twenty-Item Toronto Alexithymia Scale-II. Convergent discriminant, and concurrent validity. J Psychosom Res. 1994;38:33–40. doi: 10.1016/0022-3999(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 45.Bressi C, Taylor G, Parker J, Bressi S, Brambilla V, Aguglia E, et al. Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: an Italian multicenter study. J Psychosom Res. 1996;41:551–559. doi: 10.1016/s0022-3999(96)00228-0. [DOI] [PubMed] [Google Scholar]
- 46.Nijenhuis ERS. Somatoform Dissociation: Phenomena, Measurement, and Theoretical Issues. Assen, The Netherlands: Van Gorcum; 1999. [Google Scholar]
- 47.Najavits LM, Weiss RD, Shaw SR. The link between substance abuse and posttraumatic stress disorder in women. A research review. Am J Addict. 1997;6:273–283. [PubMed] [Google Scholar]
- 48.Speranza M, Corcos M, Stéphan P, Loas G, Pérez-Diaz F, Lang F, et al. Alexithymia, depressive experiences, and dependency in addictive disorders. Subst Use Misuse. 2004;39:551–579. doi: 10.1081/ja-120030058. [DOI] [PubMed] [Google Scholar]
- 49.Craparo G, Faraci P, Rotondo G, Gori A. The Impact of Event Scale-Revised: Psychometric properties of the Italian version in a sample of flood victims. Neuropsychiatr Dis Treat. 2013;9:1427–1432. doi: 10.2147/NDT.S51793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Faraci P, Triscari MT, D'Angelo V, Urso V. Fear of flying assessment: a contribution to the Italian validation of two self-report measures. Rev Psychol. 2011;18:91–100. [Google Scholar]
- 51.Manna G, Faraci P, Como MR. Factorial structure and psychometric properties of the Sensation Seeking Scale - Form V (SSS-V) in a sample of Italian adolescents. Eur J Psychol. 2013;9:276–288. [Google Scholar]
- 52.Giannini M, Gori A, De Sanctis E, Schuldberg D. Attachment in psychotherapy: psychometric properties of the psychological treatment inventory attachment styles scale (PTI-ASS) J Psychother Integrat. 2011;21:363–381. [Google Scholar]
- 53.Craparo G, Schimmenti A, Caretti V. Traumatic experiences in childhood and psychopathy: a study on a sample of violent offenders from Italy. Eur J Psychotraumatol. 2013;4 doi: 10.3402/ejpt.v4i0.21471. doi: 10.3402/ejpt.v4i0.21471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Luca M, Giannini M, Gori A, Littleton H. Measuring dysmorphic concern in Italy: Psychometric properties of the Italian Body Image Concern Inventory (I-BICI) Body Image. 2011;8:301–305. doi: 10.1016/j.bodyim.2011.04.007. [DOI] [PubMed] [Google Scholar]


