Abstract
A 66-year-old man presented with decompensated acute liver failure with no clear etiology. Eventually, a bone marrow biopsy revealed hemophagocytic cells, and he was diagnosed with hemophagocytic lymphohistiocytosis. This is an uncommon condition in adults, with high morbidity and mortality, and it is often indistinguishable from other forms of acute liver failure. Early clinical suspicion is critical to making the diagnosis, based on meeting at least four of nine specified criteria.
Keywords: acute liver failure, hemophagocytic lymphohistiocytosis
INTRODUCTION
In patients with idiopathic acute liver failure, failure to accurately diagnose the underlying cause early in the patient's course may make the difference between treatment success and failure. Liver biopsy is not always revealing, and patients with such severe illness are often unable to provide an adequate history. In such cases, physicians must consider and evaluate for unusual diagnoses, as well as more commonly seen conditions. We present a case with an unexpected diagnosis in a patient with acute liver failure.
CASE PRESENTATION
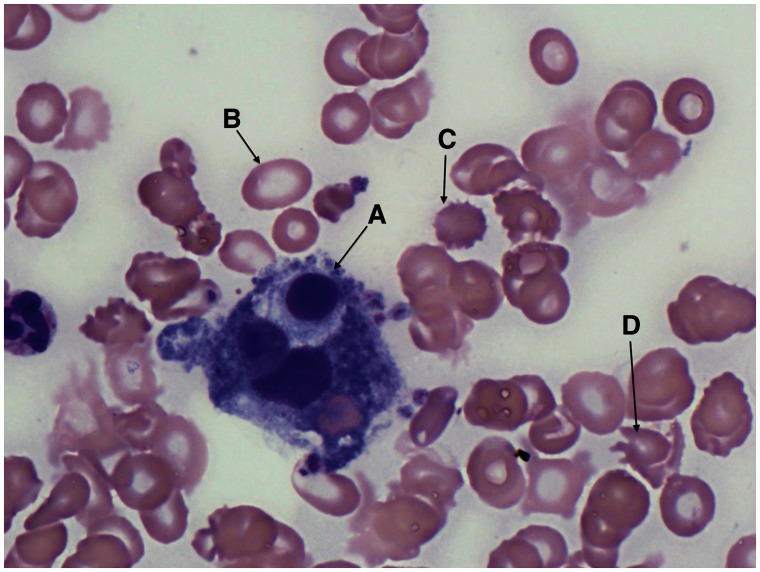
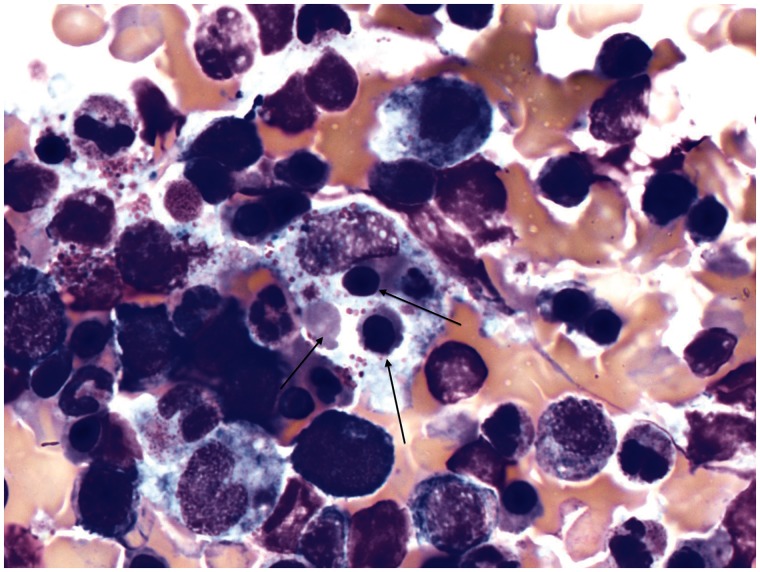
A 66-year-old man with no known liver disease presented to his primary care provider with abdominal pain and jaundice. Laboratory evaluation demonstrated a total bilirubin level >5.0 mg/dL. He was admitted for observation and evaluation of his hyperbilirubinemia. Over the next few days, he developed progressive jaundice and coagulopathy without significant elevation in transaminases. Virological, auto-immune and genetic studies were negative for causes of chronic liver disease and he was not known to be an alcoholic. His condition rapidly worsened and he was transferred to a regional liver transplant center for consideration for liver transplant. Unfortunately, he quickly deteriorated in the intensive care unit, requiring multiple vasopressor agents, continuous hemodialysis (for complete renal failure), frequent transfusions of blood products for disseminated intravascular coagulopathy (DIC), and respiratory support. A liver biopsy showed significant hepatocyte necrosis (>60%). During the liver transplant evaluation, he was found to have splenic lesions that were incompletely characterized on a CT scan of the abdomen. Suspecting lymphoma or other occult malignancy, an in-depth analysis of the peripheral blood (Figure 1) and a bone marrow biopsy (Figure 2) were performed, which demonstrated a large number of hemophagocytic cells, leading to a diagnosis of hemophagocytic lymphohistiocytosis (hemophagocytic syndrome or HLH). By this time, his condition had continued to worsen and he was deemed to not be a candidate for either liver transplant or chemotherapy. In consultation with the patient's family, life support measures were withdrawn. He expired approximately 24 hours later.
Figure 1.
Peripheral blood smear demonstrating a lymphohistiocyte (A) in a background of burr cells (B), ovalocytes (C), and schistocytes (D).
Figure 2.
Bone marrow aspirate with lymphohistiocyte formation. Note that multiple erythrocyte precursors (see arrows) are contained within this abnormal cell, having undergone phagocytosis. Images are courtesy of the Pathology Department, University of California-San Diego.
DISCUSSION
HLH is a rare condition that is variably associated with infections, auto-immune conditions, malignancy, and lymphoproliferative disorders. Its pathology is not entirely understood and it is sufficiently rare in adults, that the true incidence is unknown [1]. HLH may mimic more common conditions such as septic shock, acute leukemia and severe infections, making it very difficult to diagnose early enough to treat. Bilirubin levels may rapidly rise as high as 20–25 mg/dL in some patients. Our patient's bilirubin peaked at approximately 46 mg/dL. DIC is seen in up to 95% of patients as well. 85–90% of patients present with fever, hepatomegaly and splenomegaly, which may not distinguish them significantly from patients admitted to a liver transplant service with decompensated cirrhosis [2].
HLH is more common in children, particularly familial HLH (it is rare in adults), which is acquired as an autosomal, recessive condition. Skin manifestations, such as purpura and morbilifom eruptions, may be early manifestations of this condition. This form may be more easily treated if recognized early. Acquired HLH is typically more aggressive and nearly 100% fatal if untreated. This may manifest in adults who are heterozygotes for the related gene mutations and may manifest severe disease when triggered by an immune response. Epstein-Barr Virus is one of the more commonly associated infections.
The diagnosis of HLH is made by identifying at least five of the following nine criteria (although early treatment may benefit a patient with only four of the nine criteria if the clinical suspicion is high) [2]:
Cytopenias in at least two cell lines
Ferritin >500 mg/dL (>3000 mg/dL is more specific)
Splenomegaly
Hepatitis
Hypofibrinoginemia or hypertriglyceridemia
Hemophagocytosis on biopsy of bone marrow, spleen, or lymph node (in absence of malignancy)
Low natural killer cell activity. Natural killer cells are part of the innate immune system and typically respond to viral infections and tumor formation.
Fever for at least seven days
CD25 level >2400 units/mL. CD25 is expressed on the IL-2 receptor and is highly expressed in many leukemias and lymphoproliferative disorders.
When the diagnosis of HLH is suspected, a hematology/oncology specialist should be consulted immediately, as delays in treatment may result in progression to multiorgan dysfunction syndrome. Bone marrow biopsy may be necessary to make the diagnosis in uncertain cases. Treatment regimens, such as the HLH-94 protocol, are largely based on pediatric trials. This treatment consists of induction with dexamethasone and etoposide, along with cyclosporine and/or methotrexate [3]. Even with early recognition, this condition is highly morbid. In the HLH-94 study, 5-year mortality was approximately 50%. Even so, this was a dramatic improvement over the typical non-treatment mortality rate, which approaches 100% [2]. Liver and renal failure were significant risk factors for early death. The primary limitation to using these treatments is that the diagnosis is often not made until the patient is too sick to safely undergo such cytotoxic medications.
CONCLUSION
This patient was critically ill very early in his presentation to the liver transplant center and was unfortunately not a candidate for liver transplant or chemotherapy. We acknowledge the difficulty in making this diagnosis and advise that HLH should be considered in any patient presenting with unexplained liver failure who meets at least four criteria for this syndrome [2].
ACKNOWLEDGEMENTS
The author wishes to acknowledge the pathology department of University of California, San Diego for providing the pathology images.
Conflict of interest: none declared.
REFERENCES
- 1.Risdall RJ, McKenna RW, Nesbit ME, et al. Virus-associated hemophagocytic syndrome: a benign histiocytic proliferation distinct from malignant histiocytosis. Cancer. 1979;44:993–1002. doi: 10.1002/1097-0142(197909)44:3<993::aid-cncr2820440329>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 2.Henter JI, Horne A, Aricò M, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 3.Henter JI, Samuelsson-Horne A, Aricò M, et al. Treatment of hemophagocytic lymphohistiocytosis with HLH-94 immunochemotherapy and bone marrow transplantation. Blood. 2002;100:2367–73. doi: 10.1182/blood-2002-01-0172. [DOI] [PubMed] [Google Scholar]