Abstract
AIM: To study the cloning of α-β fusion gene from Clostridium perfringens and the immunogenicity of α-β fusion expression.
METHODS: Cloning was accomplished after PCR amplification from strains NCTC64609 and C58-1 of the protective antigen genes of α-toxin and β-toxin. The fragment of the gene was cloned using plasmid pZCPAB. This fragment coded for the gene with the stable expression of α-β fusion gene binding. In order to verify the exact location of the α-β fusion gene, domain plasmids were constructed. The two genes were fused into expression vector pBV221. The expressed α-β fusion protein was identified by ELISA, SDS-PAGE, Western blotting and neutralization assay.
RESULTS: The protective α-toxin gene (cpa906) and the β-toxin gene (cpb930) were obtained. The recombinant plasmid pZCPAB carrying α-β fusion gene was constructed and transformed into BL21(DE3). The recombinant strain BL21(DE3)(pZCPAB) was obtained. After the recombinant strain BL21(DE3)(pZCPAB) was induced by 42°C,its expressed product was about 22.14% of total cellular protein at SDS-PAGE and thin-layer gel scanning analysis. Neutralization assay indicated that the antibody induced by immunization with α-β fusion protein could neutralize the toxicity of α-toxin and β-toxin.
CONCLUSION: The obtained α-toxin and β-toxin genes are correct. The recombinant strain BL21(DE3)(pZCPAB) could produce α-β fusion protein. This protein can be used for immunization and is immunogenic. The antibody induced by immunization with α-β fusion protein could neutralize the toxicity of α-toxin and β-toxin.
Keywords: Clostridium perfringens, α-β fusion gene, Cloning and expression
INTRODUCTION
Clostridium perfringens is an anaerobe, forming a part of normal intestinal flora in humans and animals[1]. This organism is the causative agent of diseases such as gas gangrene, hemorrhagic enteritis, enterotoxemia[2]. It is also a secondary pathogen in various diseases, such as necrotic enteritis[3]. Clostridium perfringens can produce extra cellular toxins and enzymes including α-toxin and β-toxin produced by Clostridium perfringens types A and C respectively. These toxins are significant virulence factors in case of gas gangrene or clostridial myonecrosis[4,5].
In this study, α-toxin and β-toxin protective antigen genes were amplified by PCR from Clostridium perfringens type A strain NCTC64609 and type C strain C58-1 respectively. The recombinant plasmid pZCPAB carrying α-β fusion gene was constructed by transforming it into BL21(DE3). The fusion protein that could produce α-β was obtained. The expressed α-β fusion protein could resist the attack of α-toxin or β-toxin.
MATERIALS AND METHODS
Materials
Clostridium perfringens type A strain NCTC64609 and type C strain C58-1 were purchased from China Institute of Veterinary Drug Control. Plasmid pBV221 and E coli DH5α, BL21(DE3) were kept in our Laboratory. Plasmid pMD18-T was purchased from TaKaRa Company. Taq DNA polymerase, T4 DNA ligase, restriction endonuclease and DNA markers DL2000 were purchased from TaKaRa Company. DNA fragment recover kit, SDS, IPTG, Rnase A and lysozyme were purchased from Promega Company. Other reagents if not described, were of analytic purity.
Extraction of genomic DNA of clostridium perfringens
Clostridium perfringens strains were incubated in TYG medium at 37 °C overnight. Bacterium cells were harvested by centrifugation, dissolved in TE buffer containing lysozyme(2 g/L) and incubated at 37°C for 1 h. Then SDS(final concentration was 1%), EDTA(final concentration was 50 mmol/L) and proteinase K(final concentration was 150 mg/L) were added. The reaction mixture was incubated at 58 °C for 4 h and extracted three times with equal volume of saturated phenol. The aqueous phase was transferred to an Eppendorf tube. Then 0.2 volume of ammonium acetate(10 mol/L) and 2 volumes of ice-cold absolute alcohol were added, mixed well and deposited for 10 min at room temperature. Chromosome DNA deposition like clew was picked with a glass stick to another Eppendorf tube. Appropriate TE was added to dissolve DNA and stored at 4 °C.
PCR amplification of α-toxin and β-toxin protective antigen genes
Chromosome DNA of Clostridium perfringens was amplified by PCR from genomic DNA using forward primers designed from the available sequence.
One set of primers of α-toxin protective antigen gene (cpa906) was synthesized. The EcoRIand BamHIsites were inserted to the 5’ and 3’ ends of α-toxin genes via PCR. The sequence of α-toxin primers is as follows:
Up-stream primer:
P1: CCGGAATTCATGGGTCGGGATCCTGAT
EcoRI
Down-stream primer:
P2: GGCGGATCCCTTAATTTTATATTATA
BamH I
Another set of primers of β-toxin protective antigen gene was synthesed. The BamH I and Pst I sites were inserted to the 5’ and 3’ ends of β-toxin genes via PCR. The sequence of β-toxin primers is as follows:
Up-stream primer:
P1: 5’-CGCGGATCCAATGATATAGGTAAAACT-3’
BamH I
Down-stream primer:
P2: 5’-CCGCTGCAGCTACTTAATAGCTGT-3
Pst I
The following components were added into a 500 μL microcentrifuge tube. Each PCR contained 0.1 μmol/L primer1, 0.1 μmol/L primer2, 0.25 mmol/L dNTP, 1.5 mmol/L MgCl2, 10 μL 10×PCR buffer and appropriate template DNA. Sterile distilled water was added into a 100 μL reaction system. After the tubes were heated at 95°C for 5 min, 5 u Taq DNA polymerase was added into each tube. Thirty cycles of PCR were performed (denaturation at 94 °C for 1 min, annealing at 55 °C for 1 min, and extension at 72 °C for 1 min) . The amplified α- and β-toxin genes were purified separately by agarose gel electrophoresis to remove primers and extraneous amplification products.
Cloning and sequencing of α-toxin and β-toxin protective antigen genes
The α-toxin and β-toxin protective antigen genes were separated and purified by agarose gel electrophoresis alongside DNA marker DL2000 and sequentially ligated to the pMD18-T cloning vector. Sequencing was performed with ABI 377 sequencer from Takara Company.
Construction of expression vector carrying α-β fusion gene
The α-toxin protective antigen gene and expression plasmid pBV221 were digested by restrictive enzymes EcoR I and BamH I respectively to generate cohesive ends. The α-toxin gene was inserted into the vector pBV221 and the recombinant vector pZBVA1 containing α-toxin protective antigen genes of Clostridium perfringens was constructed. Then the β-toxin protective antigen gene and the recombinant vector pZBVA1 were digested by restrictive enzymes BamH I and Pst I respectively to generate cohesive ends. The β-toxin gene was inserted into the vector pZBVA1 and recombinant expression vector pZCPAB containing α-β fusion gene was obtained. The sequence of inserted fragment was confirmed by DNA sequencing.
Growth condition for α-β fusion gene expression
The recombinant was transformed into E. coli BL21(DE3) and selected by agar plate containing ampicillin and confirmed by restriction enzyme mapping. E. coli BL21(DE3) cells transformed with the plasmids described above were grown in LB medium with 50 mg/mL ampicillin (1/50) at 30°C to OD600 = 0.4~0.6. The growth was conditioned at 42°C for 5 h in order to express α-β fusion protein.
Analysis of bacterial samples
The cultured cells were collected by centrifugation at 5000 r/min for 10 min at 4°C. The optimum time of maximum expression of proteins was analyzed through SDS-PAGE. The expressed protein was tested through Western blot with specific antiserum. SDS-PAGE and Western blotting were performed as previously described[6,7]. The antigen-binding activity of the α-β fusion protein was determined by ELISA as previously described[8]. For determination of protein expression, the absorption value at 560 nm was measured by thin-layer chromatogram scanner type CS-9000.
Protective effect of α-β fusion protein on mice
The 8-wk old Kunming mice were divided into 8 groups randomly, 10 mice in each group. In treatment groups, each mouse was inoculated with inactive recombinant strains that could express α-β fusion protein. In control groups, each mouse was inoculated with strains that could not express α-β fusion protein. After 4 wk, each mouse of 4 groups was treated with one minimum lethal dose (MLD) of α-toxin or β-toxin. Another 4 groups were treated with 2 MLD of α-toxin or β-toxin. The survived mice/total mice were counted in a week. The segments of liver, lung, heart, spleen and intestines of mice in treatment group and control group were tested by LM assay.
RESULTS
Gene cloning and identification of α-toxin gene from clostridium perfringens type A
The α-toxin gene from Clostridium perfringens type A strain NCTC64609 was isolated from genomic DNA-extracted template by PCR amplification. The reaction yielded a single product. Electrophoresis of PCR products confirmed the length of PCR fragment, which was approximately 900 bp (Figure 1A). The α-toxin gene was purified with DNA fragment recover kit and evaluated by agarose gel electrophoresis. The α-toxin gene fragment was ligated to the cloning vector pMD18-T with T4 DNA ligase. The cloning vector containing the α-toxin gene was introduced into competent E. coli DH5αcells by CaCl2 transformation. Transformed E. coli were grown at 37°C in medium containing X-gal/IPTG and ampicillin. The positive plasmids were identified via sequential digestion with EcoR I and BamH I and α-toxin protective antigen gene about 900 bp was obtained (Figure 1B). Sequence of inserted DNA was analyzed with automatic sequence analyzer and about 906 bp in size and encoded 302 amino acid residues (Figure 2). The recombinant plasmid was named pMD 906.
Figure 1.
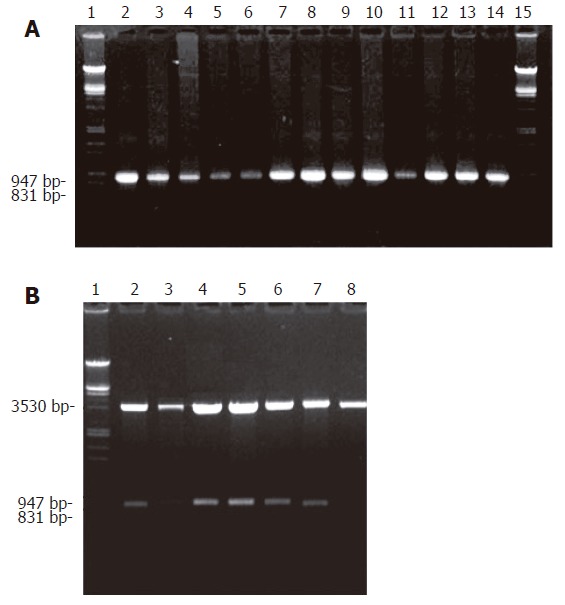
Identification of α-toxin gene product amplified by PCR (A) and recombinant plasmid by enzyme digestion (B). In A, lanes 1, 15: DNA markers; lanes 2-14: product of α-toxin gene amplified by PCR; In B, lane 1: DNA markers; lanes 2-7: pMD 906/ EcoR I + BamH I; lane 8: pMD 906/ EcoR I.
Figure 2.
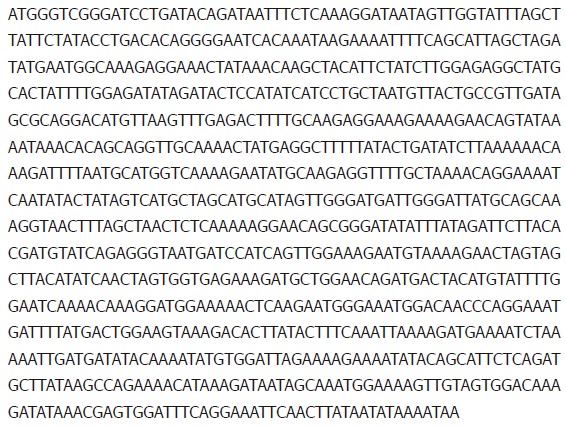
Nucleotide sequence of α-toxin gene from Clostridium perfringens type A strain NCTC64609.
Cloning and identification of β-toxin gene from clostridium perfringens type A
The β-toxin protective antigen genes were amplified from Clostridium perfringens type C and strain C58-1 by PCR. The PCR products were approximately 930 bp in length (Figure 3A). The β-toxin gene was purified and ligated to the cloning vector pMD18-T as α-toxin gene. The positive plasmids were identified via sequential digestion with Pst I and BamH I and about 930 bp β-toxin genes were obtained (Figure 3B). Sequence of inserted DNA was analyzed with automatic sequence analyzer and bout 930 bp in length and encoded 310 amino acid residues (Figure 4). The recombinant plasmid was named pMD 930.
Figure 3.
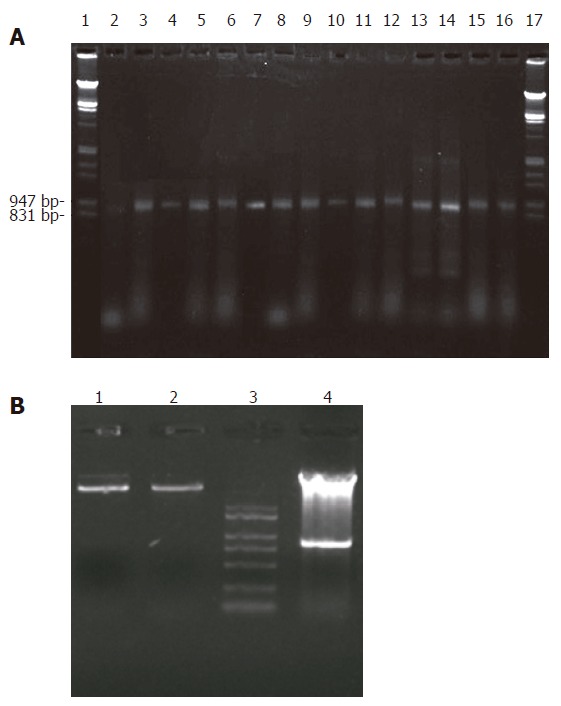
Identification of β-toxin gene product amplified by PCR (A) and recombinant plasmid by enzyme digestion (B). In A, lanes 1,17: DNA markers; lanes 2-16: product of β-toxin gene amplified by PCR; In B, lane 1: pMD930/EcoR I; lane 2: pMD930/ Pst I; lane 3: DNA Markers; lane 4: pMD930/BamH I+Pst I
Figure 4.

Nucleotide sequence of β-toxin gene from Clostridium perfringens type C strain C58-1
Construction of recombinant expression vector pzcpab
The recombinant expression plasmids containing α-β fusion gene were constructed. The positive plasmids were identified via sequential digestion with EcoR I and Pst I and about 1.8 kb α-β fusion genes were obtained (Figure 5). Sequence of α-β fusion genes was analyzed with automatic sequence analyzer and about 1842 bp in length and encoded 614 amino acid residues. The recombinant plasmid was named pZCPAB.
Figure 5.

Agarose gel electrophoresis of restriction endonucleases-digested plasmid pZCPAB. Lane 1: DNA markers; lane 2: pZCPAB / EcoR I; lanes 3-5: pZCPAB / EcoR I+Pst I; lane 6: pZCPAB / BamH I.
Expression of α-β fusion gene in E coli BL21 (DE3) (PZCPAB)
The recombinant plasmid pZCPAB carrying α-β fusion gene was transformed into E coli BL21(DE3) and the recombinant strain BL21(DE3)(pZCPAB) was obtained. SDS-PAGE and Western blotting of the bacterial protein showed that a specific protein band with a molecular weight of 66 kD emerged in the bacterial protein of E coli BL21(DE3)(pZCPAB). SDS-PAGE gel-scanning showed that the expressed α-β fusion protein accounted for 22.14% of the total bacterial protein (Figure 6). ELISA results indicated that the expressed fusion protein could be recognized by anti-α toxin antibody and anti-β toxin antibody respectively (Table 1).
Figure 6.
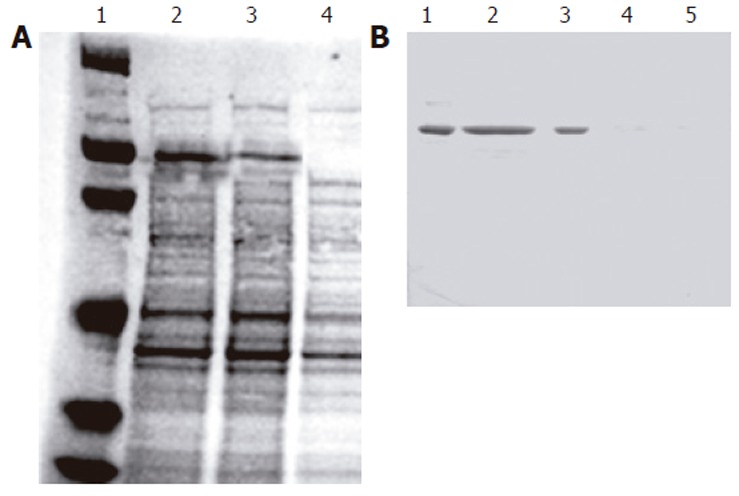
Analysis of expressed products of α-β fusion gene in E.coli by SDS-PAGE (A) and Western blot (B) In A, lane 1: protein markers (97400, 66200, 43000, 31000, 20100, 14400); lanes 2, 3: BL21(DE3)( pZCPAB); lane 4: BL21(DE3)(pBV221); In B, lane 1: BL21(DE3)(pZCPAB)/α; lane 2: BL21(DE3)(pZCPAB)/α+β; lane 3: BL21(DE3)( pZCPAB)/β; lanes 4, 5: BL21(DE3)(pBV221).
Table 1.
Detection of the fusion protein by ELISA assay
| Antibody | pZCPAB | pBV221 | pXETA | pXETB |
| Anti-α-toxin | 0.66 ± 0.08 | 0.001 | 0.92 ± 0.13 | |
| Anti-β-toxin | 0.72 ± 0.12 | 0.002 | 0.97 ± 0.19 |
Bioactivity assay of expressed α-β fusion protein
The expressed α-β fusion protein yielded in bacteria could provide protection of mice against the challenge of lethal doses of α-toxin or β-toxin of Clostridium perfringens (Table 2).
Table 2.
Expressed α-β fusion protein in mice
| Challenge dose | α-toxin(survived mice/total mice) Control group Treatment group | β-toxin(survived mice/total mice) Control group Treatment group | ||
| 1 MLD | 0/10 | 10/10 | 0/10 | 10/10 |
| 2 MLD | 0/10 | 8/10 | 0/10 | 9/10 |
Pathological changes in different organs
The segments of liver, lung, heart, spleen and intestine were sampled from the control group in which mice died of toxicosis and the treatment group in which survived mice were immunized with α-β fusion protein. Then they were observed by LM assay.
In treatment group, the structure of liver was seen clearly except that a few central veins of hepatic lobules were full of blood. The liver cytoarchitectures were intact (Figure 7A). In control group, the structure of hepatocytes was grain-like metamorphic. The nuclei of hepatocytes were concentrated and collapsed. Swollen hepatic sinusoids, veins of hepatic lobules and central veins were full of red cells or red thrombi, swollen Kupffer cells in the margin of hepatic sinusoids (Figure 7B).
Figure 7.
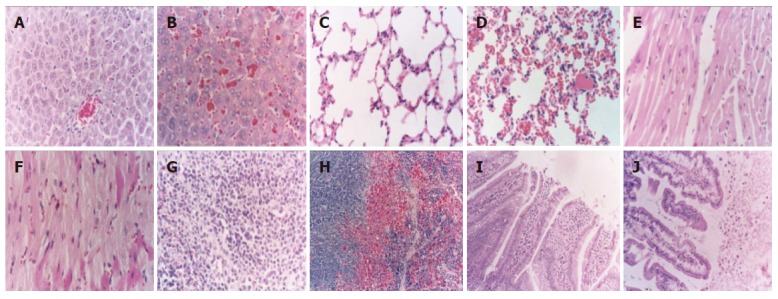
Pathological changes in livers of survived mice (A) and dead mice (B), in lung of survived mice (C) and dead mice (D), in heart of survived mice (E) and dead mice (F), in spleen of survived mice (G) and dead mice (H), in intestine of survived mice (I) and dead mice (J).
The capillaries in alveolar septum of the lung in treatment group were slightly bloodshot with no other abnormalities (Figure 7C). The swollen capillaries in alveolar septum were full of red cells. Some of capillaries were full of red thrombi (Figure 7D).
The structure of cardiac muscle fibers in treatment group was intact (Figure 7E). The capillary vessels and cardiac muscle fibres were swollen and bloodshot (Figure 7F).
There was no abnormal structure of spleen in treatment group (Figure 7G). The splenic cord was extruded and could not be seen clearly (Figure 7H).
The structure of duodenum and jejunum in treatment group was intact (Figure 7I). The capillary vessels of lamina propria of tunica mucosa had little bleeding. The epithelia of tunica mucosa were metamorphic and necrotic, one or many of intestinal villi fell into the enterocele (Figure 7J).
DISCUSSION
Clostridium perfringens is ubiquitous in the environment and has been found in soil, decaying organic matter and a member of the gut flora in humans and animals. Different strains of C perfringens can be classed into one of the five biotypes (A-E) according to the spectrum of toxins produced[9]. Clostridium perfringens is a Gram-positive anaerobic spore-forming bacterium which is widely found in the environment and also in the intestinal tract of humans and animals. Due to the production of several exotoxins, C perfringens is of great importance as a pathogen in humans, domestic animals and wildlife[10]. The production of four major toxins alpha (α), beta (β), epsilon (ε) and iota (ι) allows the discrimination into five types from A to E. In veterinary medicine, each of these types has been linked to specific diseases[11]. Clostridium perfringens enterotoxin (CPE) serves as an additional virulence factor which is believed to cause enteritis in pigs, cats and dogs[12]. The Gram-positive pathogen Clostridium perfringens is a major cause of human and veterinary enteric disease largely because this bacterium can produce several toxins when present inside the gastrointestinal tract[13].
Biotype A strains of Clostridium perfringens are of particular importance as the aetiological agents of gas gangrene in humans. Gangrenous disease is of increasing significance in elderly and diabetic population, especially in those who have undergone lower limb surgery, where impaired blood supply to tissues can lead to anoxic conditions suitable for proliferation of bacteria[14]. The disease can also arise in patients who have undergone surgery of the gastrointestinal tract when contamination of damaged tissues with gut contents can result in the establishment of disease[15]. Clostridium perfringens β-toxin is known to be the primary pathogenic factor of necrotic enteritis in type C strains that produce β-toxin. Necrotizing enteritis is believed to be due to the production of β-toxin by Clostridium perfringens type C. Clostridium perfringens β-toxin can also cause dermonecrosis and oedema in the dorsal skin of animals[16-18].
This paper describes the successful isolation and cloning of α-toxin and β-toxin genes from the strains NCTC64609 and C58-1 of Clostridium perfringens respectively. The construction and expression of α-β fusion gene, and the biological activities of α-β fusion protein have a significant impact on mice. To our knowledge, this is the first successful experiment of the development of a recombinant α-β fusion protein. We believe that it could serve as a model for development and construction of novel fusion protein for α-toxin, β-toxin and other potential toxins. In this study, the expressed α-β fusion protein could provide protection of mice against the challenge of lethal dose of α-toxin and β-toxin of Clostridium perfrigens. These findings indicate that the expressed α-β fusion protein can be applied in preventing toxicosis of α-toxin and β-toxin of Clostridium perfringens.
Footnotes
Supported by Natural Science Foundation of Hebei Province, No. 012201130
S- Editor Guo SY L- Editor Wang XL E- Editor Liu WF
References
- 1.Awad MM, Ellemor DM, Bryant AE, Matsushita O, Boyd RL, Stevens DL, Emmins JJ, Rood JI. Construction and virulence testing of a collagenase mutant of Clostridium perfringens. Microb Pathog. 2000;28:107–117. doi: 10.1006/mpat.1999.0328. [DOI] [PubMed] [Google Scholar]
- 2.Ochi S, Oda M, Matsuda H, Ikari S, Sakurai J. Clostridium perfringens alpha-toxin activates the sphingomyelin metabolism system in sheep erythrocytes. J Biol Chem. 2004;279:12181–12189. doi: 10.1074/jbc.M307046200. [DOI] [PubMed] [Google Scholar]
- 3.Sheedy SA, Ingham AB, Rood JI, Moore RJ. Highly conserved alpha-toxin sequences of avian isolates of Clostridium perfringens. J Clin Microbiol. 2004;42:1345–1347. doi: 10.1128/JCM.42.3.1345-1347.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Brien DK, Melville SB. Effects of Clostridium perfringens alpha-toxin (PLC) and perfringolysin O (PFO) on cytotoxicity to macrophages, on escape from the phagosomes of macrophages, and on persistence of C. perfringens in host tissues. Infect Immun. 2004;72:5204–5215. doi: 10.1128/IAI.72.9.5204-5215.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flores-Díaz M, Alape-Girón A. Role of Clostridium perfringens phospholipase C in the pathogenesis of gas gangrene. Toxicon. 2003;42:979–986. doi: 10.1016/j.toxicon.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 6.Sambrook J, Fristch EF, Maniatis T. Molecular Cloning. 2nd Ed. Cold Spring Harbor. New York: Cold Spring Harbor Laboratory Press; 1989. [Google Scholar]
- 7.Rood JI, Cole ST. Molecular genetics and pathogenesis of Clostridium perfringens. Microbiol Rev. 1991;55:621–648. doi: 10.1128/mr.55.4.621-648.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennett AM, Lescott T, Phillpotts RJ, Mackett M, Titball RW. Recombinant vaccinia viruses protect against Clostridium perfringens alpha-toxin. Viral Immunol. 1999;12:97–105. doi: 10.1089/vim.1999.12.97. [DOI] [PubMed] [Google Scholar]
- 9.Abraham LJ, Rood JI. Molecular analysis of transferable tetracycline resistance plasmids from Clostridium perfringens. J Bacteriol. 1985;161:636–640. doi: 10.1128/jb.161.2.636-640.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagahama M, Morimitsu S, Kihara A, Akita M, Setsu K, Sakurai J. Involvement of tachykinin receptors in Clostridium perfringens beta-toxin-induced plasma extravasation. Br J Pharmacol. 2003;138:23–30. doi: 10.1038/sj.bjp.0705022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smedley JG 3rd, Fisher DJ, Sayeed S, Chakrabarti G, McClane BA. The enteric toxins of Clostridium perfringens. Rev Physiol Biochem Pharmacol. 2004;152:183–204. doi: 10.1007/s10254-004-0036-2. [DOI] [PubMed] [Google Scholar]
- 12.Schotte U, Truyen U, Neubauer H. Significance of beta 2-toxigenic clostridium perfringens infections in animals and their predisposing factors--a review. J Vet Med B Infect Dis Vet Public Health. 2004;51:423–426. doi: 10.1111/j.1439-0450.2004.00802.x. [DOI] [PubMed] [Google Scholar]
- 13.Justin N, Walker N, Bullifent HL, Songer G, Bueschel DM, Jost H, Naylor C, Miller J, Moss DS, Titball RW, et al. The first strain of Clostridium perfringens isolated from an avian source has an alpha-toxin with divergent structural and kinetic properties. Biochemistry. 2002;41:6253–6262. doi: 10.1021/bi012015v. [DOI] [PubMed] [Google Scholar]
- 14.Clark GC, Briggs DC, Karasawa T, Wang X, Cole AR, Maegawa T, Jayasekera PN, Naylor CE, Miller J, Moss DS, et al. Clostridium absonum alpha-toxin: new insights into clostridial phospholipase C substrate binding and specificity. J Mol Biol. 2003;333:759–769. doi: 10.1016/j.jmb.2003.07.016. [DOI] [PubMed] [Google Scholar]
- 15.Ochi S, Oda M, Nagahama M, Sakurai J. Clostridium perfringens alpha-toxin-induced hemolysis of horse erythrocytes is dependent on Ca2+ uptake. Biochim Biophys Acta. 2003;1613:79–86. doi: 10.1016/s0005-2736(03)00140-8. [DOI] [PubMed] [Google Scholar]
- 16.Goswami PP, Girish KS, Chaudhuri P, Tiwari V, Akare SJ, Harbola PC. Cloning and sequencing of beta toxin gene of Clostridium perfringens type C. Indian J Exp Biol. 2002;40:109–110. [PubMed] [Google Scholar]
- 17.Luginbühl A. [The necrotizing enteritis by Clostridium perfringens type C in piglets: practical observations, control and epidemiology] Schweiz Arch Tierheilkd. 2002;144:263–273. doi: 10.1024/0036-7281.144.6.263. [DOI] [PubMed] [Google Scholar]
- 18.Bacciarini LN, Boerlin P, Straub R, Frey J, Gröne A. Immunohistochemical localization of Clostridium perfringens beta2-toxin in the gastrointestinal tract of horses. Vet Pathol. 2003;40:376–381. doi: 10.1354/vp.40-4-376. [DOI] [PubMed] [Google Scholar]


