Abstract
Objective
To examine the longitudinal association between changes in health behaviors and depression, and to determine the mediating effect of health characteristics on this association.
Method
Based on the first and second waves of the Survey of Health, Aging and Retirement in Europe (SHARE)-Israel, depressive symptoms of 1,524 Israelis aged 50 or older were analyzed using logistic regression.
Results
Changes in physical activity and body weight are associated with depressive symptoms after adjusting for confounders. However, after adding measures of health, the respective correlations of weight gain and commenced physical activity with depression disappear, and the correlation between continued activity and depression is reduced.
Discussion
Changes in health behaviors are related to mental health in late life, but their effect is mediated by physical and functional health. Future interventions should nevertheless target older individuals who stop physical activity and those who remain inactive to lessen the risk of depression.
Keywords: life style, physical activity, mental health, Arabs, SHARE
Introduction
The World Health Organization defines health as a state of complete physical, mental, and social wellbeing, but the literature on the health of mature adults emphasizes physical health more than mental wellbeing. Depression is the most prevalent mental health problem among older people (Castro-Costa et al., 2007) and it has numerous negative results. For example, the appearance of depressive symptoms at an advanced age increases the risk of cardiovascular events, inflammatory diseases and physical disability (Duivis et al., 2011; Lenze et al., 2001; Whooley et al., 2008). These same studies show that health behaviors, body mass index and lack of physical activity contribute to the correlation between depression and its outcomes.
Health behaviors are predictive of depression among older people, but studies distinguish between health enhancing behaviors, such as proper nutrition and physical activity, and health risk factors, i.e., smoking, drug and alcohol consumption. In several cases, lack of engagement in health enhancing behaviors becomes a health risk factor, as in the case of lack of physical exercise and change in body weight (Fulkerson, Sherwood, Perry, Neumark-Sztainer, & Story, 2004; Matheson, King & Everett, 2012; Reeves & Rafferty, 2005). The correlation between health promoting behaviors and depression has been examined in both cross-sectional (Allgower, Wardle & Steptoe, 2001; Teychenne, Ball & Salmon, 2008a; Wada, Satoh, Tsunoda & Aizawa, 2006) and longitudinal studies (Brown, Ford, Burton, Marshall & Dobson, 2005; Vogelzangs et al., 2010; Win et al., 2011). However, the correlation between change in health behaviors over time and the appearance of depressive symptoms has rarely been studied (Ball, Burton & Brown, 2009). The purpose of this study, therefore, is to examine the association between changes in health behaviors and depressive symptoms.
Several cross-sectional studies show that depression is correlated with lack of physical activity among young and old women and men (Allgower et al., 2001; Jones, Rovner, Crews & Danielson, 2009; Teychenne, Ball & Salmon, 2008a). One such study found that the development of depressive symptoms was associated with physical activity less than once a week among older adults (Wada et al., 2006). Others have found that moderate – vigorous leisure time physical activity was negatively associated with depressive symptoms among women (Teychenne et al., 2008b) and among men (Fulkerson, Sherwood, Perry, Neumark-Sztainer, & Story, 2004). But one study found that of the three parameters of leisure-time physical activity (intensity, duration, and frequency), only intensity was associated with depressive symptoms (Chen, Stevinson, Ku, Chang & Chu, 2012). Longitudinal studies show a correlation between decreasing levels of physical activity intensity and the appearance of depressive symptoms (Duivis et al., 2011; Brown et al., 2005), and an association between leisure time physical activity and reduced risk of depressive symptoms in older adults (Ku, Fox, Chen & Chou, 2009; 2012).
A systematic review of observational and intervention studies also showed that physical activity of both short and long duration was associated with a reduced likelihood of depression (Teychenne et al., 2008a). Four of the studies revealed that vigorous physical activity was more strongly associated with a decreased likelihood of depression than was lower intensity activity. Two of them found a stronger inverse relationship of leisure time physical activity with depression than work related and domestic physical activity. In addition, Chen et al. (2012) found that leisure time physical activity, but not non-leisure time physical activity, was associated with decreased depressive symptoms among older people.
The literature defines change in body weight or body mass index (BMI) as unhealthy weight – control behaviors (Duivis et al., 2001; Fulkerson et al., 2004). In studies of weight change in old age, a loss or gain of 5—10 % (about 5 to 10 pounds) has been cited as meaningful change that predicts morbidity and mortality (Harris, Launer, Madans, & Feldman, 1997; Newman et al., 2001). However, there are relatively few longitudinal studies examining the associations between weight change and depression, (Singh, Jackson, Dobson & Mishra, 2013). One such study showed that weight gain was associated with an increased risk of prevalence and incidence of depression (Singh et al., 2013). Another found that increased BMI was associated with increased odds of depressive symptoms at follow-up, but the same was not the case for decreased BMI (Ball et al., 2009).
The literature also notes a relationship between smoking and depressive symptoms. Cross-sectional studies revealed that among older adults, current and former smokers were both more likely to have depressive symptoms than non-smokers, and that former smokers were less likely to have depressive symptoms than current smokers (Lam et al., 2004; Wada et al., 2006).
Health is related to depression independently of the effect of health behaviors. For example, the negative effect of depression on self-rated health among older people has been demonstrated in both cross-sectional studies (Beekman, Kriegsman, Deeg & van Tilburg, 1995; Millan – Calenti, Sanchez, Lorenzo, & Maseda, 2012; Mulsant, Ganguli & Seaberg, 1997) and longitudinal studies (Han & Jylha, 2006; Ruo et al., 2006). The effect of self-rated health on depressive symptoms has yet to be evaluated in longitudinal study. Nevertheless, several studies show that self-rated health is strongly predictive of mortality and future health states (Cesari et al., 2008; Ford, Spallek & Dobson, 2008) and is a reliable index of predicting survival, life span and quality of life among the general population (Idler & Benyamini, 1997).
Great emphasis is placed in the literature on the relationship between physical health and depression in later life. For example, individuals with good physical health and no history of previous episodes of ill health have a relatively low risk of developing depression at a later age (Beekman et al., 1995). In addition, chronic diseases and long-term illness (such as cancer, hypertension, stroke, congestive heart failure, and diabetes mellitus), which frequently occur in old age, have been shown to be closely related to depressive symptoms in older adults (Braam et al., 2005; Buber & Engelhardt, 2011; Duivis et al., 2011; Gale et al., 2011; Geerlings, Beekman, Deeg & van Tilburg, 2000). Moreover, illness in old age may result in functional disabilities that restrict mobility and require assistance with self-care. This may lead to loss of dignity and the onset of depressive symptoms (Braam et al., 2005; Buber & Engelhardt, 2011; Gale et al., 2011; Geerlings et al., 2000; Yang, 2006). One longitudinal study showed a prospective positive association of activities of daily living (ADL) and instrumental activities of daily living (IADL) with depressive symptoms (Yang & George, 2005).
Physical health and self-rated health both depend, in the short and long term, on health behaviors. It was found, for example, that lack of physical activity increases the risk of illness and death (Hurley & Reuter, 2011; Reddigan, Arden, Riddell & Kuk, 2011), physical disabilities (Gretebeck, Ferraro, Black, Holland & Gretebeck, 2012) and low self-rated health (Molarius et al., 2007). It was also found that weight change (loss or gain) is a risk factor for morbidity and mortality. For example, weight gain has been shown to lead to coronary heart disease, hypertension, diabetes, and hyperlipidemia, (Harris et al., 1997; Nelsson, 2008), functional disabilities and lowered mobility (Harris et al., 1997), and low self-rated health (Simonsen, Hundrup, Grønbæk & Heitmann, 2008). Weight loss is associated with morbidity (Nelsson, 2008) and increased mortality risk (Nelsson, 2008; Newman et al., 2001). Smoking is related to chronic respiratory diseases, cardiac diseases, cancers and hypertension (Freedman et al., 2006), as well as low self-rated health (Komar, Nagymajtenyi, Nyari & Paulik, 2006: Lim, Ma, Heng, Bhalla & Chew, 2007). Given these correlations, the current study considers the mediating effect of subjective health, physical health, and functional disability on the association between changes in health behaviors and depressive symptoms.
Socio-demographic characteristics are also related to depression in advanced age. These include female gender (Duivis et al., 2011; Geerlings et al., 2000; Prince et al., 1999a), older age (Buber & Engelhardt, 2011; Geerlings et al., 2000; Prince et al., 1999b), low education (Buber & Engelhardt, 2011; Duivis et al., 2011; Geerlings et al., 2000), unmarried status (Geerlings et al., 2000; Prince et al., 1999b), being unemployed (Chen et al., 2012; Ku et al., 2009), and belonging to an ethnic minority (Duivis et al., 2011).
To our knowledge, there has been no longitudinal study to date on the association between changes in health behaviors and depressive symptoms. We employ panel data to address the following two study questions:
Does change in health behaviors over time, specifically changes in physical activity, weight and smoking behaviors, predict depressive symptoms after controlling for baseline depression and background variables?
Do health (that is, physical and subjective health) and functional disability mediate the presumed associations between change in health behaviors and depressive symptoms?
Sample
The study is based on the first and second waves of the Israeli component of the Survey of Health, Aging and Retirement in Europe (SHARE), a longitudinal survey of persons age 50 and older. Israel is an interesting case study for the effects of health behaviors on depressive symptoms for several reasons. First, rates of depression in that country are relatively high (Geulayov, Lipsitz, Sabar, & Gross, 2007), as they are in other Mediterranean countries (Ploubidis & Grundy, 2009). Second, life expectancy in Israel is among the highest and the gender gap in life expectancy is relatively narrow (men=80 years, women = 84 years) (Glicksman & Litwin, 2011; Staetsky & Hide, 2009). Third, older Israelis have experienced many stressful life events over the years due to war, migration and hardship (Shrira, Shmotkin, & Litwin, 2012). The data for the analysis were collected in 2005-2006 and 2009-2010, respectively. The current analytic sample comprises 1,524 individuals who participated in both waves and for whom there was no missing data on the relevant study variables (63.3% of the respondents from Wave I). Respondents from the first wave who did not participate in the second wave (and hence were not included in this analysis) reported poorer baseline health, including subjective health, and were less active (data not shown).
Variables
Depression was assessed on the EURO-D scale which was developed to compare symptoms of depression across European countries (Prince et al., 1999a). It covers 12 symptom domains: depressed mood, pessimism, suicidal tendencies, guilt, sleep, interest, irritability, appetite, fatigue, concentration, enjoyment, and tearfulness. Each item is rated 0 (symptom not present) or 1 (symptom present). The total score ranges from 0 to 12, with higher scores indicating greater depressive symptomatology. Dewey and Prince (2005) define clinically significant depression as a EURO-D score greater than 3. Therefore, the score was dichotomized in the current inquiry as: 3 or less = “0”, and greater than 3 = “1.” The baseline depression score at Wave I was considered as a control variable, while the Wave II depression status served as the dependent variable in the analysis.
Changes in health behaviors included physical activity, smoking and weight change. Physical activity was measured in the survey on two measures: moderate activity and vigorous activity. These two measures were combined in the current analysis insofar as about 80 percent of respondents reporting vigorous activity also reported doing moderate activity. The combined measure thus reflected two levels: no physical activity (0) or moderate to vigorous physical activity (1), as has been done elsewhere (Fulkerson et al., 2004). To measure the change in physical activity from Wave 1 to Wave II, we constructed a variable with four categories: (1) no physical activity (in either wave); (2) stopped physical activity (in Wave II); (3) commenced activity (in Wave II); and (4) physically active in both waves. Current smoking was measured as a dichotomous variable with the values of “non-smoker” (0) and “current smoker” (1). To calculate the change in this measure, we generated a variable composed of four categories: (1) smoked in both waves; (2) commenced smoking; (3) stopped smoking; and (4) no smoking (in either wave). The weight variable was self-reported, in kilograms. The change in weight indicator generated a variable composed of four categories: (1) loss of 4.5 k”g (10 pounds) or less; (2) loss of more than 4.5 k”g ; (3)gain of 4.5 k”g or less; and (4) gain of more than 4.5 k”g.
Health variables included self perceived health, physical health (chronic disease and long-term health problems) and baseline weight. Self-perceived health in Wave II was elicited by asking the respondents to describe their general health on a scale that ranged from “excellent” to “poor.” The variable was dichotomized to: less than good (fair or poor) = “1”, and good or more (excellent, very good or good) = 0.” Thus, the variable reflects poor self-perceived health.
In terms of physical health, respondents specified if they were ever diagnosed with a chronic illness from a list of 14 diseases, which included: heart failure, hypertension, cerebral vascular disease, diabetes, hyperlipidemia, chronic lung disease, asthma, arthritis, osteoporosis, cancer, peptic ulcer, parkinson disease, cataracts, and hip or femoral fracture. This variable was dichotomized to: (0) “less than 2 diseases” and (1) “2 or more diseases.” In addition, each participant indicated whether s/he suffered long-term health problems, illness, disability or infirmity over a period of time (1) or not (0). As mentioned in the literature, these measures are long-term outcomes of health behaviors. Therefore, data about these measures were selected from the Wave II survey. Baseline weight in kilograms was recorded in the survey by self report.
Functional disability was obtained at Wave II by reported difficulties in activities of daily living (ADL) (Katz, Downs, Cash & Grotz, 1970), and in instrumental activities of daily living (IADL) (Lawton & Brody, 1969). The former counts reported difficulties in the following six areas: dressing, bathing, eating, getting in/out of bed, walking across the room and using the toilet, with a possible score of 0-6. The score was dichotomized in this analysis to: (0) “no ADL difficulty” and (1) “one ADL difficulty or more”. IADL difficulties included using the telephone, shopping, housekeeping, laundry, transportation, managing medications, and managing finances, with a possible score of 0-7. Here too, the score was dichotomized to: (0) “no IADL difficulty” and (1) “one IADL difficulty or more”.
Background variables were obtained in Wave I regarding participants’ gender, employment status, marital status, ethnicity, age, and years of education. Gender was coded as female (1) or male (0). Employment status was measured as presently working (1) or not working (0). Marital status was assessed as having a partner (1) or not (widowed, divorced, or never married) (0). Ethnicity reflected Arabic (1) or Jewish (0). Age was categorized as (0) 50 - 64 years old, (1) between 65 - 74, and (2), 75 years old or more. Education level reflected: (0) 12 years of education or less, (1) more than 12 years.
Data analyses
Descriptive statistics were employed to calculate the means and standard deviations of the continuous variables and the percentages and frequencies of the categorical variables. Next, chi-square tests were used to identify unadjusted differences between depressed and non-depressed participants by background variables, changes in health behaviors, physical and subjective health, and the functional disability measures (p<.05). Depression status at Wave II was regressed on the study variables using binary logistic regression. Specifically, we examined the extent to which the changes in health behaviors were associated with depressive symptoms after adjustments for the effects of the control (baseline depression at Wave I) and background variables. Accordingly, baseline depression and the background variables were entered in the first model and the health behavior changes were entered in model 2, which allowed examination of the first question. (The respective reference categories for the health behavior and all other study variables are indicated in Table 3).
Table 3.
Binary logistic regression analysis with depression (EURO-D scale at wave II) as dependent variable (N =1524)
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | OR | 95% CI | B | OR | 95% CI | B | OR | 95% CI | B | OR | 95% CI | |
| Depression – Wave I | 1.34 | 3.9*** | 2.9-5.0 | 1.17 | 3.2*** | 2.4-4.3 | 1.07 | 2.9*** | 2.2-3.9 | 1.03 | 2.8*** | 2.0-3.7 |
| Ethnicity (RC= Jewish) | ||||||||||||
| Arab | .79 | 2.2*** | 1.6-3.1 | .96 | 2.6*** | 1.8-3.7 | 1.12 | 3.1*** | 2.0-4.5 | .80 | 2.2** | 1.4-3.3 |
| Gender (RC=male) | ||||||||||||
| Female | .06 | 1.1 | 0.8-1.4 | .14 | 1.1 | 0.8-1.5 | .24 | 1.2 | 0.9-1.9 | .22 | 1.2 | 0.9-1.7 |
| Marital status (RC=with partner) | ||||||||||||
| Without partner | .27 | 1.3 | 0.9-1.8 | .27 | 1.3 | 0.9-1.9 | .25 | 1.3 | 0.7-1.3 | .19 | 1.2 | 0.8-1.7 |
| Employment status (RC= working) | ||||||||||||
| Not working | .64 | 1.9*** | 1.3-2.6 | .54 | 1.7** | 1.2-2.4 | .31 | 1.4 | 0.9-1.9 | .17 | 1.2 | 0.8-1.7 |
| Age (RC= 50 – 64) | ||||||||||||
| 65 – 74 | -.03 | 0.9 | 0.7-1.3 | -.05 | 0.9 | 0.7-1.3 | -.07 | 0.9 | 0.7-1.3 | -.11 | 0.9 | 0.6-1.2 |
| 75+ | .27 | 1.6 | 0.9-1.9 | .13 | 1.1 | 0.7-1.7 | -.01 | 0.9 | 0.7-1.5 | -.19 | 0.8 | 0.5-1.3 |
| Education (RC: >12) | ||||||||||||
| ≤12 | .79 | 2.2*** | 1.6-2.9 | .66 | 1.9*** | 1.4-2.6 | .59 | 1.8*** | 1.3-2.5 | .50 | 1.7*** | 1.2-2.3 |
| Change in physical activity (RC= remained inactive) | ||||||||||||
| Stopped activity | -.27 | 0.8 | 0.4-1.3 | -.21 | 0.8 | 0.4-1.5 | -.01 | 1.01 | 0.5-1.9 | |||
| Commenced activity | -.81 | 0.4** | 0.2-0.8 | -.67 | 0.5* | 0.2-0.9 | -.35 | 0.7 | 0.3-1.4 | |||
| Remained active | -1.4 | 0.3*** | 0.1-0.4 | -1.05 | 0.3*** | 0.2-0.6 | -.65 | 0.5** | 0.3-0.9 | |||
| Change in weight (RC= loss 0 - 4.5 k”g) | ||||||||||||
| Loss > 4.5 k”g | .20 | 1.2 | 0.9-1.8 | 0.17 | 1.2 | 0.8-1.7 | .15 | 1.1 | 0.8-1.7 | |||
| gain ≤ 4.5 k”g | -.33 | 0.7 | 0.5-1.1 | -.33 | 0.7 | 0.5-1.1 | -.32 | 0.7 | 0.5-1.09 | |||
| gain > 4.5 k”g | .39 | 1.6* | 1.03-2.2 | .40 | 1.5* | 1.03-2.1 | .37 | 1.4 | 0.9-2.0 | |||
| Long-term illness(RC = No) | ||||||||||||
| Yes | .46 | 1.6** | 1.1-2.2 | .42 | 1.5* | 1.1-2.1 | ||||||
| Chronic disease (RC = less than 2 diseases) | ||||||||||||
| 2+ chronic diseases | .45 | 1.6** | 1.1-2.2 | .44 | 1.6** | 1.1-2.2 | ||||||
| Self-perceived health (RC = excellent/ very good/ good) | ||||||||||||
| Fair/poor | .61 | 1.9*** | 1.3-2.5 | .41 | 1.5** | 1.01-2.1 | ||||||
| ADL limitations (RC = no) | ||||||||||||
| Yes (1+) | .92 | 2.5*** | 1.5-4.2 | |||||||||
| IADL limitations (RC = no) | ||||||||||||
| Yes (1+) | .70 | 2.0*** | 1.4-2.8 | |||||||||
| Model summary | ||||||||||||
| Chi-square | 239.83*** | 308.32*** | 364.81*** | 403.14*** | ||||||||
| Log likelihood | 1404.98 | 1336.51 | 1280.01 | 1241.68 | ||||||||
| Nagelkerke (R2) | 0.23 | 0.29 | 0.34 | 0.37 | ||||||||
Note: OR=odds ratio, CI = confidence interval, RC= reference category
p < .05.
p < .01.
p< .001.
Next, we examined the second question about the extent to which the health and functional disability characteristics mediated the association between health behaviors and depressive symptoms. Thus, model 3 added the three mediating variables of health: self-perceived health, chronic diseases, and long-term health problems; and model 4 added two additional mediating variables of functional disability (ADL and IADL). [No evidence was discerned for the presence of multicollinearity among the variables in tests that were performed prior to the regressions (Stevens, 2002)]. A supplementary analysis examined change in depression score by time and by changes in each health behavior using repeated measures ANOVA. The Statistical Package for Social Sciences (SPSS) version 20.0 was used for the data analysis.
Results
The results show that the majority of participants in the study population were women (57.3%), had a partner (80.5%) and were not working (66.3%). The mean years of education was 11.4 (SD = 4.9, range = 0-25). Their ages ranged from 50 to 98 years (Mean = 67.2, SD = 9.5). Respondents reported mild to moderate levels of depressive symptoms with a mean of 2.51 (SD= 2.6) and a range of 0-12 (data not shown). Twenty eight percent of the sample scored greater than 3, the threshold indicating risk for clinical depression (Dewey & Prince, 2005).
Table 1 reveals that all the Wave 1 background variables were related to depressive symptoms at Wave II. Arabs were more likely to be depressed, as were women. Those with a partner were less likely to be depressed while the unemployed were more likely. Older respondents and those with lower education were also more depressed.
Table 1.
Depression scores by background variables: Descriptive statistics and bivariate analysis (N=1524).
| Depression –EURO-D | ||||
|---|---|---|---|---|
| Variables | Measurement | No (N=1098) | Yes (N=426) | χ2 |
| Ethnicity n (%) | Arab | 164 (60.1)* | 109 (39.9)* | 23.7*** |
| Jewish | 934 (74.1)* | 317 (24.3)* | ||
| Gender n (%) | female | 601 (69.1)* | 267 (30.9)* | 8.8** |
| male | 497 (76.0)* | 157 (24.0)* | ||
| Marital status n (%) | without partner | 176 (64.0)* | 99 (36.0)* | 10.7** |
| with partner | 920 (73.8)* | 327 (26.2)* | ||
| Employment status n (%) | not working | 647 (65.1)* | 347 (34.9)* | 71.1*** |
| working | 430 (85.8)* | 71 (14.2)* | ||
| Age n (%) | 50 – 64 | 571 (77.3)* | 168 (22.7)* | 29.7*** |
| 65 – 74 | 328 (71.5) | 131 (28.5) | ||
| 75+ | 199 (61.0)* | 127 (39.0)* | ||
| Education n (%) | ≤12 | 588 (63.4)* | 340 (36.6)* | 91.3*** |
| >12 | 503 (86.0)* | 82 (14.0)* | ||
p < .01.
p< .001.
Standardized adjusted residuals: < -2.0 or > 2.0.
Table 2 shows that respondents who remained physically active or started being active between the two waves were less likely to report depressive symptoms than those who remained inactive or stopped physical activity between the two periods. Additionally, those whose weight loss or gain was more than 4.5 kilograms (10 pounds) between the two waves were more depressed than those whose weight gain or loss was less than 4.5 kilograms. In contrast, a change in smoking behavior was not associated with depressive symptoms. In addition, all the health and functional disability variables, except for participants’ weight at W1, were associated with increased depressive symptoms.
Table 2.
Depression scores at wave II by health behaviors, perceived health, physical health, and functional disabilities characteristics: Descriptive statistics and bivariate analysis (N=1524)
| Depression –EURO-D | |||||
|---|---|---|---|---|---|
| Variables | Measurements | No (N=1098) | Yes (N=426) | test | |
| Change in health behaviors between Wave I and Wave II | Change in physical activity n (%) | remained inactive | 40 (35.1)* | 74 (64.9)* | χ2=165.0*** |
| stopped activity | 99 (51.8)* | 92 (48.2)* | |||
| commenced activity | 88 (62.4)* | 53 (37.6)* | |||
| remained active | 864 (81.0)* | 203 (19.0)* | |||
| Change in smoking pattern n (%) | remained smoking | 129 (73.3) | 47 (26.7) | χ2=1.10 | |
| began smoking | 16 (69.6) | 7 (30.4) | |||
| stopped smoking | 49 (74.2) | 17 (25.8) | |||
| remained non smoking | 277 (76.5) | 85 (23.5) | |||
| Change in weight n (%) | loss 0 - 4.5 k”g | 404 (74.3)* | 140 (25.7)* | χ2=32.42*** | |
| loss > 4.5 k”g | 190 (63.8)* | 108 (36.2)* | |||
| gain ≤ 4.5 k”g | 246 (80.1)* | 61 (19.9)* | |||
| gain > 4.5 k”g | 174 (62.6)* | 104 (37.4)* | |||
| Subjective and physical health | Self-perceived health-Wave II n (%) | excellent/ very good/ good | 732 (83.6)* | 144 (16.4)* | χ2=135.6*** |
| fair/ poor | 366 (56.6)* | 282 (43.5)* | |||
| Chronic disease-Wave II n (%) | less than 2 diseases | 551 (86.2)* | 88 (13.8)* | χ2=111.1*** | |
| 2+ chronic diseases | 539 (61.6)* | 336 (38.4)* | |||
| Long-term illness-Wave II n (%) | no | 560 (85.2)* | 97 (14.8)* | χ2=100.3*** | |
| yes | 536 (62.0)* | 329 (38.0)* | |||
| Weight-Wave 1 mean (SD) | 74.5 (14.0) | 75.1 (14.1 | t=-0.76 | ||
| Functional disability (Wave II) | ADL limitations n (%) | no limitations | 1061 (77.6)* | 307 (22.4)* | χ2=209.8*** |
| yes (1+ limitations) | 32 (21.5)* | 117 (78.5)* | |||
| IADL limitations n (%) | no limitations | 845 (84.1)* | 160 (15.9)* | χ2=213.9*** | |
| yes (1+ limitations) | 248 (48.4)* | 264 (51.6)* | |||
p< .001.
Standardized adjusted residuals: < -2.0 or > 2.0.
The hierarchical logistic regression analyses which examined the research questions are presented in Table 3. We included only significant independent variables in the regressions. The first two steps of the analysis examined the first research question: step (1) control and background variables from Wave 1; and step (2) changes in health behaviors. The last two steps of the analysis examined the second research question: step (3) health characteristics from Wave II; and step (4) functional disability (Wave II). The control and background variables produced a pseudo R2 of .23 (Model 1). [We note that 14 percent of the explained variance was accounted for by the depression score at Wave I]. Participants with more years of education were less likely to be depressed. Arabs and unemployed participants were more likely. The entry of the health behavior variables added 6 percent to the explained variance (Model 2). Those who started physical activity between the two waves or remained active were less likely to report depressive symptoms than those who remained inactive. A weight gain of more than 4.5 kilograms between the two waves increased the probability of reporting depressive symptoms by about 1.6 times in comparison to the reference category (loss of 4.5 kilograms or less). With the inclusion of the health behaviors, the control and background variables maintained their previous significance.
Health characteristics were also significant and contributed moderately to the dependent variable when entered in the third step (Δ R2=.05, p<0.01). The table shows that except for employment status, all the other background variables, as well as weight gain of more than 4.5 kilograms and the two physical activity measures kept their previous significance. It was also found that having long-term illness, chronic diseases, and perceived poor health were associated with increased depressive symptoms.
The final model identified a total of nine predictors of Wave II depression, with a pseudo R2 of .37. These included depression at Wave I, two background variables—ethnicity and education, and five mediator variables—self-perceived health, long-term illness, chronic diseases, ADL, and IADL. In addition, the final model shows that participants who remained physically active were less likely to have depressive symptoms than those who remained inactive. However, the risk ratios for the change in physical activity (commenced physical activity) and for weight gain of more than 4.5 kilograms were not significant in the final model. These results suggest a mediation path between the changes in physical activity and weight, on the one hand, and the likelihood of being depressed, on the other hand, via the health characteristics.
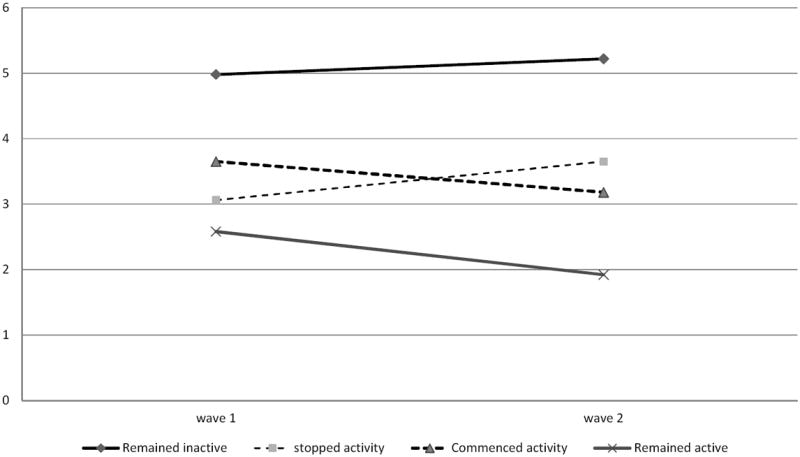
In order to further clarify the results, we executed an additional analysis of the change in depression scores across time in each category of physical activity. The results revealed that the effect of time on depressive symptoms was not significant [F(1,1509)= 0.2, P >0.05]. However, a significant interaction emerged between change in physical activity and depression over time [F(3,1509)= 6.7, P<0.001]. Three of the four categories of physical activity showed significant changes in depressive symptoms. The depression score among participants who stopped physical activity increased from a mean of 3.0 (SD=2.4) in Wave I to a mean of 3.7 (SD=2.7) in Wave II (p< .01), while participants who commenced activity or remained active decreased their depression scores from a mean of 3.7 (SD=2.8) and 2.6 (SD=2.0) respectively, to means of 3.2 (SD=2.7; p<.05) and 1.9 (SD=2.0; p<.01).. The depression outcome did not change among participants who remained inactive (see Figure. 1).
Figure 1. Change in depression mean scores across two time-points in each change in physical activity.
Discussion
This study considered two related questions. The first examined whether changes in health behaviors among older Israeli adults were related to depressive symptoms. We found that changes in two of the three domains of health behaviors examined—changes in physical activity and weight—were indeed associated with risk of depressive symptoms after adjustments for baseline depression and background variables.
The multivariate results showed that the two change measures in relation to physical activity (remained in physical activity and commenced activity across the two waves of the study) were both related to lower risk of depressive symptoms as compared to those who remained inactive. This finding is supported by previous studies which point to the reduced risk of depressive symptoms in older adults who commenced or continued physical activity (Ku et al., 2009; 2012). It has been hypothesized that physical activity reduces the risk of depression through physiological pathways, as for example, the activation of endorphin secretion which reduces pain and produces a euphoric sensation (Paluska & Schwenk, 2000). The current analysis also showed a positive association between a weight gain of more than 4.5 kilograms and depressive symptoms, after controlling for the baseline depression and background characteristic. This result confirms the correlation between weight gain and depression that was found in one previous longitudinal study on this topic (Ball et al., 2009).
Contrary to expectations, the current study failed to show an association between changes in smoking and depressive symptoms. This finding reinforces those of some cohorts (Takeuchi, Nakao & Yano, 2004), but is incompatible with other cross-sectional studies that showed a significant association between smoking and depressive symptoms (Allgower et al., 2001). A possible explanation for the discrepancy in our findings stems from the limited variance in the smoking variable. Fewer respondents answered this question compared to the two other health behavior measures and among them, very few indicated a change in their smoking behavior. Further study is required, therefore, to clarify the prospective effect of smoking on the onset of depressive symptoms.
The second research question considered was whether physical health, subjective health and/or functional disability variables mediate the association between change in health behaviors and depression. The results revealed that after physical health or functional disability variables were taken into account, the correlation between change in weight and depression disappeared, while the correlation between physical activity and depression decreased in one category and disappeared in the others. The tentative conclusion, therefore, is that physical and/or functional health mediates the association between health behaviors and mental health.
More importantly, the present analysis showed that one change measure in relation to physical activity—having commenced activity between the two waves—lost its initial significance after adjusting for functional disability. Previous studies have documented a positive correlation between ADL and IADL and depressive symptoms in late life (Braam et al., 2005; Buber & Engelhardt, 2011; Gale et al., 2011; Geerlings et al., 2000; Yang, 2006; Yang & George, 2005). In addition, the literature has also revealed that physical activity; even minimal exercise, can reduce the risk of functional limitations and disability in older adults (Miller, Rejeski, Reboussin, Ten Have & Ettinger, 2000; Paterson & Warburton, 2010). It seems, therefore, that the association between physical activity and depressive symptoms is correlated with other measures common to both. Consequently, it is likely that the impact of this particular measure of physical activity (commenced activity across the two waves of the study) on depressive symptoms was blocked by functional disability measures having stronger predictability. This is a plausible interpretation in light of the fact that the older adults in this sample who kept doing physical activity across the two waves of the study were less likely to have functional disability than their counterparts who did not.
The analysis also showed that the association between weight gain from Wave 1 to Wave II and depressive symptoms, was no longer significant after adjustments were made for functional disability. One possible explanation for the lack of association in this analysis is that the correlation between weight gain and depressive symptoms is mediated by functional disability. Indeed, functional impairment is recognized as an important risk factor for depression in older adults (Buber & Engelhardt, 2011; Gale et al., 2011; Geerlings et al., 2000). One longitudinal study underscores the association between ADL and IADL and depression (Yang & George, 2005). Moreover, an increase in weight can negatively affect functional activity (Harris et al., 1997). Therefore, the association between weight gain and depression is likely to be correlated with other health characteristics common to both variables. Indeed, when entering all of these variables in the same model, the impact of weight gain on depression was blocked by the other indices of health having stronger predictability, particularly ADL and IADL difficulties.
In addition, the findings in the present study point to two background variables that predict depressive symptoms independently of the other variables considered, namely ethnicity and education. Of note, in this regard, is that older Arabs were more likely to be depressed than older Jews. Since there is no previous comparative study of depression among these two populations, this finding is unique to the present study. One possible explanation for this finding is its association with additional factors common to both variables, such as physical health and disabilities. Indeed, a recent study (Osman & Walsemann, 2013) documented that Arab adults aged 50 and older suffer from chronic illnesses, long-term health problems and functional disabilities more than their Jewish counterparts. It may also be that the differences between Arabs and Jews in reporting depressive symptoms arose from socioeconomic factors, such as the social gaps and the inequalities between these two populations, which were not taken into account in the current study.
We should point out three limitations of the current study. First, despite it being a longitudinal study, the ability of the analysis to predict a causal association between the variables is still incomplete. A further limitation relates to sample size, due to attrition between Wave I and Wave II, and from the limited number of Arab respondents in the current study. Finally, although we address weight change as a health behavior, it may be contended that weight change is a product of behaviors and metabolism.
Despite these limitations, the contribution of the current study lies in its being the first inquiry to address the longitudinal effects of changes in health behaviors on depressive symptoms in older Israeli adults. Moreover, the study has implications for policy. The findings suggest a possible need for primary prevention programs related to health behaviors, particularly physical activity. According to the current results, physical activity intervention for adults aged 50 and over, such as a consistent exercise program with adjusted levels of intensity and frequency, may facilitate improving subjective health, on the one hand, and reducing functional disability and physical illness, on the other. This, in turn, could contribute to decreasing the extent of depressive symptoms among older adults over time.
However, an opposite interpretation of the findings is also plausible. That is, it could be that prevention programs would have only limited impact on depression reduction insofar as the effect of changes in health behaviors on depression are mediated by health status and disability. Such health-related conditions may be the effect of lifelong processes that are difficult to ameliorate in late life through short term interventions. Additional study of this field of inquiry is, thus, clearly warranted.
Acknowledgments
Funding for data collection in Israel was provided by the U.S. National Institute of Aging (R03AG029258, R01AG031729, R21AG025169), the National Insurance Institute of Israel, The German-Israeli Foundation for Scientific Research and Development (GIF), the Ministry of Science, and the Ministry for Senior Citizens. Central funding for SHARE came from the European Commission through the 5th framework programme (project QLK6-CT-2001-00360 in the thematic programme Quality of Life), the 6th framework programme (projects SHARE-I3, RII-CT-2006-062193, as an Integrated Infrastructure Initiative), and through the 7th framework programme (SHARE-PREP (No 211909) and SHARE-LEAP (No 227822)).
References
- Allgower A, Wardle J, Steptoe A. Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychology. 2001;20:223–227. [PubMed] [Google Scholar]
- Ball K, Burton NW, Brown WJ. A prospective study of overweight, physical activity, and depressive symptoms in young women. Obesity. 2009;17:66–71. doi: 10.1038/oby.2008.497. [DOI] [PubMed] [Google Scholar]
- Beekman ATF, Kriegsman DMW, Deeg DJH, van Tilburg W. The association of physical health and depressive symptoms in the older population: age and sex differences. Social Psychiatry and Psychiatric Epidemiology. 1995;30:32–38. doi: 10.1007/BF00784432. [DOI] [PubMed] [Google Scholar]
- Braam AW, Prince MJA, Beekman TF, Delespaul P, Dewey ME, Geerlings SW, Copeland JRM, et al. Physical health and depressive symptoms in older Europeans. Results from EURODEP. British Journal of Psychiatry. 2005;187:35–42. doi: 10.1192/bjp.187.1.35. [DOI] [PubMed] [Google Scholar]
- Brown WJ, Ford JH, Burton NW, Marshall AL, Dobson AJ. Prospective study of physical activity and depressive symptoms in middle-aged women. American Journal of Preventive Medicine. 2005;29:265–272. doi: 10.1016/j.amepre.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Buber I, Engelhadt H. The association between age and depressive symptoms among older men and women in Europe. Findings from SHARE. Comparative Population Studies. 2011;36:103–126. [Google Scholar]
- Castro-Costa E, Dewey M, Stewart R, Banerjee S, Huppert F, Lima Mendonca, Prince M, et al. Prevalence of depressive symptoms and syndromes in later life in ten European countries. The SHARE study. British Journal of Psychiatry. 2007;191:393–401. doi: 10.1192/bjp.bp.107.036772. [DOI] [PubMed] [Google Scholar]
- Cesari M, Onder G, Zamboni V, Manini T, Shorr RI, Russo A, Landi F, et al. Physical function and self-rated health status as predictors of mortality: results from longitudinal analysis in the ilSIRENTE study. BMC Geriatrics. 2008;8 doi: 10.1186/1471-2318-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LG, Stevinson C, Ku PW, Chang YK, Chu DC. Relationships of leisure-time and non-leisure-time physical activity with depressive symptoms: A population-based study of Taiwanese older adults. International Journal of Behavioral Nutrition and Physical Activity. 2012;9 doi: 10.1186/1479-5868-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey ME, Prince MJ. Mental Health. In: Börsch-Supan A, Jürges H, editors. Health, Ageing and Retirement in Europe - First Results from the Survey of Health, Ageing and Retirement in Europe. Mannheim: MEA Eigenverlag; 2005. pp. 108–117. [Google Scholar]
- Duivis H, de Jonge P, Penninx BW, Na BY, Cohen BE, Whooley MA. Depressive symptoms, health behaviors, and subsequent inflammation in patients with coronary heart disease: prospective findings from the heart and soul study. American Journal of Psychiatry. 2011;168:913–920. doi: 10.1176/appi.ajp.2011.10081163. [DOI] [PubMed] [Google Scholar]
- Ford J, Spallek M, Dobson A. Self-rated health and a healthy lifestyle are the most important predictors of survival in elderly women. Age & Aging. 2008;37:194–200. doi: 10.1093/ageing/afm171. [DOI] [PubMed] [Google Scholar]
- Freedman DM, Sigurdson AJ, Rajaraman P, Doody MM, Linet MS, Ron E. The mortality risk of smoking and obesity combined. American Journal of Preventive Medicine. 2006;31:355–362. doi: 10.1016/j.amepre.2006.07.022. [DOI] [PubMed] [Google Scholar]
- Fulkerson JA, Sherwood NE, Perry CL, Neumark-Sztainer D, Story M. Depression symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Preventive Medicine. 2004;38:865–875. doi: 10.1016/j.ypmed.2003.12.028. [DOI] [PubMed] [Google Scholar]
- Gale CR, Aihie Sayer A, Cooper C, Dennison EM, Starr JM, Whalley LJ, Deary IJ, et al. Factors associated with symptoms of anxiety and depression in five cohorts of community-based older people: the HALCyon (Healthy Ageing across the Life Course) Programme. Psychological Medicine. 2011;41:2057–2073. doi: 10.1017/S0033291711000195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerlings SW, Beekman ATF, Deeg DJH, van Tilburg W. Physical health and the onset and persistence of depression in older adults: an eight-wave prospective community-based study. Psychological Medicine. 2000;30:369–380. doi: 10.1017/s0033291799001890. [DOI] [PubMed] [Google Scholar]
- Geulayov G, Lipsitz J, Sabar R, Gross R. Depression in primary care in Israel. IMAJ. 2007;9:571–578. [PubMed] [Google Scholar]
- Glicksman A, Litwin H. International Spotlight: Israel. The Gerontologist. 2011;51:734–738. doi: 10.1093/geront/gnr104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gretebeck RJ, Ferraro KF, Black DR, Holland K, Gretebeck KA. Longitudinal change in physical activity and disability in adults. American Academy of Health Behavior. 2012;36:385–394. doi: 10.5993/AJHB.36.3.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Jylha M. Improvement in depressive symptoms and changes in self-rated health among community-dwelling disabled older adults. Aging and Mental Health. 2006;10:599–605. doi: 10.1080/13607860600641077. [DOI] [PubMed] [Google Scholar]
- Harris TB, Launer LJ, Madans J, Feldman JJ. Cohort study of effect of being overweight and change in weight on risk of coronary heart disease in old age. BMJ. 1997;314:1791–1794. doi: 10.1136/bmj.314.7097.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley B, Reuter I. Aging, physical activity, and disease prevention. Journal of Aging Research. 2011 doi: 10.4061/2011/782546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Jones GC, Rovner BW, Crews JE, Danielson ML. Effects of depressive symptoms on health behavior practices among older adults with vision loss. Rehabilitation Psychology. 2009;54:164–172. doi: 10.1037/a0015910. [DOI] [PubMed] [Google Scholar]
- Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. The Gerontologist. 1970;1:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Komar M, Nagymajtenyi L, Nyari T, Paulik E. The determinants of self-rated health among ethnic minorities in Hungary. Ethnicity & Health. 2006;11:121–132. doi: 10.1080/13557850500485378. [DOI] [PubMed] [Google Scholar]
- Ku PW, Fox KR, Chen LJ, Chou P. Physical activity and depressive symptoms in older adults: a seven-year follow-up study. Preventive Medicine. 2009;48:250–255. doi: 10.1016/j.ypmed.2009.01.006. [DOI] [PubMed] [Google Scholar]
- Ku PW, Fox KR, Chen LJ, Chou P. Physical activity and depressive symptoms in older adults: 11-year follow-up. American Journal of Preventive Medicine. 2012;42:355–362. doi: 10.1016/j.amepre.2011.11.010. [DOI] [PubMed] [Google Scholar]
- Lam TH, Li ZB, Ho SY, Chan WM, Ho KS, Leung GM. Smoking and depressive symptoms in Chinese elderly in Hong Kong. Acta Psychiatrica Scandinavica. 2004;110:195–200. doi: 10.1111/j.1600-0447.2004.00342.x. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, Reynolds CF, et al. The association of late-life depression and anxiety with physical disability: A review of literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- Lim WY, Ma S, Heng D, Bhalla V, Chew SK. Gender, ethnicity, health behavior & self-rated health in Singapore. BMC Public Health. 2007;7 doi: 10.1186/1471-2458/184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson EM, King DE, Everett CJ. Healthy lifestyle habits and mortality in overweight and obese individuals. Journal of the American Board of Family Medicine. 2012;25:9–15. doi: 10.3122/jabfm.2012.01.110164. [DOI] [PubMed] [Google Scholar]
- Millan – Calenti J, Sanchez A, Lorenzo T, Maseda A. Depressive symptoms and other factors associated with poor self-rated health in the elderly: gender differences. Geriatrics & Gerontology International. 2012;12:198–206. doi: 10.1111/j.1447-0594.2011.00745.x. [DOI] [PubMed] [Google Scholar]
- Miller ME, Rejeski WJ, Reboussin BA, Ten Have TR, Ettinger WH. Physical activity, functional limitations, and disability in older adults. Journal of the American Geriatrics Society. 2000;48:1264–1272. doi: 10.1111/j.1532-5415.2000.tb02600.x. [DOI] [PubMed] [Google Scholar]
- Molarius A, Berglund K, Eriksson C, Lambe M, Nordstrom E, Eriksson HG, Feldman I. Socioeconomic conditions, lifestyle factors, and self-rated health among men and women in Sweden. European Journal of Public Health. 2007;17:125–133. doi: 10.1093/eurpub/ckl070. [DOI] [PubMed] [Google Scholar]
- Mulsant BH, Ganguli M, Seaberg EC. The relationship between self- rated health and depressive symptoms in an epidemiological sample of community-dwelling older adults. Journal of the American Geriatrics Society. 1997;45:954–958. doi: 10.1111/j.1532-5415.1997.tb02966.x. [DOI] [PubMed] [Google Scholar]
- Nilsson PM. Is weight loss beneficial for reduction of morbidity and mortality? what is the controversy about? Diabetes Care. 2008;31:S278–S283. doi: 10.2337/dc08-s268. [DOI] [PubMed] [Google Scholar]
- Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP. Weight change in old age and its association with mortality. Journal of the American Geriatrics Society. 2001;49:1309–1318. doi: 10.1046/j.1532-5415.2001.49258.x. [DOI] [PubMed] [Google Scholar]
- Osman A, Walsemann KM. Ethnic disparities in disability among middle-aged and older Israeli adults. The role of socioeconomic disadvantage and traumatic life events. Journal of Aging & Health. 2013;25:510–531. doi: 10.1177/0898264313478653. [DOI] [PubMed] [Google Scholar]
- Paluska SA, Schwenk TL. Physical activity and mental health: current concepts. Sports Medicine. 2000;29:167–180. doi: 10.2165/00007256-200029030-00003. [DOI] [PubMed] [Google Scholar]
- Paterson HD, Warburton DER. Physical activity and functional limitations in older adults: a systematic review related to Canada’s physical activity guidelines. International Journal of Behavioral Nutrition and Physical Activity. 2010;7 doi: 10.1186/1479-5868-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ploubidis GB, Grundy E. Later-Life Mental Health in Europe: A Country-Level Comparison. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2009;64:666–676. doi: 10.1093/geronb/gbp026. [DOI] [PubMed] [Google Scholar]
- Prince MJ, Reischies F, Beekman ATF, Fuhrer R, Jonker C, Kivela SL, Copeland JRM, et al. Development of the EURO-D scale – a European Union initiative to compare symptoms of depression in 14 European centres. British Journal of Psychiatry. 1999a;174:330–38. doi: 10.1192/bjp.174.4.330. [DOI] [PubMed] [Google Scholar]
- Prince MJ, Beekman ATF, Deeg DJH, Fuhrer R, Kivela S-L, Lawlor BA, Copeland JRM, et al. Depression symptoms in late-life assessed using the EURO-D scale. Effect of age, gender and marital status in 14 European centres. The British Journal of Psychiatry. 1999b;174:339–45. doi: 10.1192/bjp.174.4.339. [DOI] [PubMed] [Google Scholar]
- Reddigan JI, Arden CI, Riddell MC, Kuk JL. Relation of physical activity to cardiovascular disease mortality and the influence of cardiometabolic risk factors. The American Journal of Cardiology. 2011;108:1426–1431. doi: 10.1016/j.amjcard.2011.07.005. [DOI] [PubMed] [Google Scholar]
- Reeves MJ, Rafferty AP. Healthy lifestyle characteristics among adults in the US. Archives of Internal Medicine. 2005;165:854–857. doi: 10.1001/archinte.165.8.854. [DOI] [PubMed] [Google Scholar]
- Ruo B, Bertenthal D, Sen S, Bittner V, Ireland CC, Hlatky MA. Self-rated health among women with coronary disease: depression is as important as recent cardiovascular events. American Heart Journal. 2006;152:e1–e7. doi: 10.1016/j.ahj.2006.01.012. [DOI] [PubMed] [Google Scholar]
- Shrira A, Shmotkin D, Litwin H. Potentially traumatic events at different points in the life span and mental health: Findings from SHARE-Israel. American Journal of Orthopsychiatry. 2012;82:251–259. doi: 10.1111/j.1939-0025.2012.01149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G, Jackson CA, Dobson A, Mishra GD. Bidirectional association between weight change and depression in mid-aged women: a population – based longitudinal study. International Journal of Obesity. 2013 doi: 10.1038/ijo.2013.127. [DOI] [PubMed] [Google Scholar]
- Staetsky L, Hinde A. Unusually small sex differentials in mortality of Israeli Jews: What does the structure of causes of death tell us? Demographic Research. 2009;20:209–251. [Google Scholar]
- Stevens J. Applied multivariate statistics for the social sciences. 4. Mahwah, NJ: Erlbaum; 2002. pp. 92–93. [Google Scholar]
- Takeuchi T, Nakao M, Yano E. Relationship between smoking and major depression in a Japanese workplace. Journal of Occupational and Health. 2004;46:489–492. doi: 10.1539/joh.46.489. [DOI] [PubMed] [Google Scholar]
- Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: A review. Preventive Medicine. 2008a;46:397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Teychenne M, Ball K, Salmon J. Associations between physical activity and depressive symptoms in women. International Journal of Behavioral Nutrition and Physical Activity. 5 doi: 10.1186/1479-5868-5-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogelzangs N, Kritchevsky SB, Beekman AT, Brenes GA, Newman AB, Satterfield S, Penninx BW. Obesity and onset of significant depressive symptoms: results from a prospective community-based cohort study of older men and women. Journal of Clinical Psychiatry. 2010;71:391–399. doi: 10.4088/JCP.08m04743blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wada K, Satoh T, Tsunoda M, Aizawa Y. Associations of health behaviors on depression symptoms among employed men in Japan. Industrial Health. 2006;44:486–492. doi: 10.2486/indhealth.44.486. [DOI] [PubMed] [Google Scholar]
- Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Browner WS, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Win S, Parakh K, Eze-Nliam CM, Gttdiener JS, Kop WJ, Ziegelstein RC. Depressive symptoms, physical activity and risk of cardiovascular mortality in older adults: the cardiovascular health study. Heart. 2011;97:500–505. doi: 10.1136/hrt.2010.209767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. Journal of health and social behavior. 2006;47:355–372. doi: 10.1177/002214650604700404. [DOI] [PubMed] [Google Scholar]
- Yang Y, George LK. Functional disability, disability transitions, and depressive symptoms in late life. Journal of Aging and Health. 2005;17:263–292. doi: 10.1177/0898264305276295. [DOI] [PubMed] [Google Scholar]


