Abstract
Background:
Studies of hepatitis A virus (HAV) seroprevalence in sub-Saharan Africa have generally found very high anti-HAV IgG seroprevalence rates, but economic development and improved drinking water access may be contributing to decreasing incidence.
Materials and Methods:
This review evaluates all 19 articles that have been published on HAV epidemiology in West Africa.
Results:
Nearly all studies conducted before 1990 found that the majority of preschool-aged children had already developed immunity due to prior infection. However, several recent studies have observed that the age at midpoint of population immunity in some urban populations has shifted to school-aged children.
Conclusion:
There is preliminary evidence that some West-African countries are beginning the transition towards lower hepatitis A endemicity levels. Additional studies of child seroprevalence rates in diverse parts of West Africa are required in order to clarify the extent to which an early transition may be occurring.
Keywords: Hepatitis A, hepatitis A virus, health transition, prevalence, seroprevalence, West Africa
INTRODUCTION
Hepatitis A virus (HAV) can cause severe acute liver disease. While many young children who become infected with the virus remain asymptomatic, older children and adults may develop jaundice and severe illness, be absent from school or work for weeks or even months, and be at risk of liver failure and death. The most common risk factors for hepatitis A infection include unreliable access to safe drinking water and other indicators of low socioeconomic status.1 A growing economy and improved access to water often correspond with a decrease in hepatitis A incidence.2 Reduced incidence is soon reflected in age-specific seroprevalence data that show few children have developed active immunity and fewer new infections are occurring in older age groups.
Hepatitis A seroprevalence rates have decreased in many world regions during the past two decades.1,2,3,4 In populations with very high rates of HAV transmission, the majority of young children and almost all older children and adults have immunologic evidence of past infection in the form of anti-HAV IgG antibodies, which usually persist for life following an initial infection. (Long-term immunity is also conferred through immunisation, but vaccines are not routinely available in the low-income countries that have the highest HAV incidence rates). As incidence rates decrease and the population shifts towards intermediate endemicity, the average age at infection increases and a growing proportion of children remain susceptible to HAV. With sustained low transmission rates, the population will eventually shift to a low endemicity profile in which the majority of children and a growing proportion of adults are vulnerable to outbreaks of HAV unless universal vaccination programmes are implemented.
Previous examinations of hepatitis A seroprevalence in sub-Saharan Africa have generally found very high endemicity levels, with more than half of children having serological evidence of prior infection by their fifth birthdays.1,3,4 However, the growth of the economy in many African countries over the two past decades means that it is possible that HAV infection rates are beginning to decrease in some populations within sub-Saharan Africa.5 This comprehensive review presents all reports on hepatitis A seroprevalence rates across West Africa since the late 1970s when the first anti-HAV IgG studies were conducted, and examines whether there is evidence of decreasing seroprevalence rates, especially among children.
MATERIALS AND METHODS
Countries included in the West sub-Saharan African region during the 2010 Global Burden of Disease (GBD 2010) study were considered to be in West Africa for this analysis.4 Medline/PubMed, CINAHL, Google Scholar, AJOL (African Journals Online), IMEMR (Index Medicus for the Eastern Mediterranean Region), and SciELO (Scientific Electronic Library Online) were searched using the terms hepatitis A, seroprevalence or prevalence, and the names of countries in the West-African region. Papers focusing solely on high-risk populations such as those with HIV or chronic liver disease were excluded. The reference lists of all relevant articles were scanned for additional items of potential relevance.
The age at midpoint of population immunity is the youngest age at which half of the members of the population who are within that age group have developed immunity to HAV due to prior infection.6 More precisely, the age at midpoint of population immunity is the youngest age at which 50% of the members of that age group have immunity to HAV due to prior exposure and 50% remain susceptible to the infection. In other words, the age at midpoint of population immunity is identical to the age at midpoint of population susceptibility. For example, if 42% of 3-year-old children, 54% of 4-year-old children, and 67% of 5-year-old children have anti-HAV IgG, the age at midpoint of population immunity in that population will be approximately 4 years of age.
The age at midpoint of population immunity for each study included in this review was estimated by plotting the median of each reported age group (x-axis) against the seroprevalence rate for that age group (y-axis), interpolating all the points for each study using a smoothed curve, and identifying the age (on the x-axis) at which the interpolated line crossed the 50% mark on the y-axis. For curve fitting, all studies were assumed to have a 0% anti-IgG seroprevalence rate for children 9-months old, the approximate age at which maternal immunity wanes. This method can provide only approximations of the age at midpoint of population immunity, and the accuracy of the estimates is dependent on the range of ages included in the study and the ranges of the age groups for which seroprevalence data were reported. An age at midpoint of population immunity cannot be estimated for some studies that do not include at least one age group with a seroprevalence rate less than 50% as well as at least one age group with a rate greater than 50%. Even with these limitations, the approximations provide useful information about the endemicity of HAV in the study countries at the time of data collection. To match previous examinations of hepatitis A burden,6 studies with an age at midpoint of population immunity to HAV of less than 5-years old were considered to have very high endemicity and studies with an age at midpoint of population immunity of 5-14 years were considered to have high endemicity.
RESULTS
Eighteen studies (reported in 19 articles) of hepatitis A seroprevalence in West-African countries have been published [Table 1], including four from Cameroon,13,14,15,17 three each from Nigeria9,10,20 and Senegal,21,22,23,26 two from Liberia,19,24 and one each from Burkina Faso,8 Cabo Verde,18 Côte d’Ivoire,11 Gambia,25 Guinea,16 and Sierra Leone.12 Three studies published data collected in or after 2009,8,9,10 one presented data from the early 2000s,11 six reported on data collected between 1985 and the mid-1990s,12,13,14,15,16,17 and the remaining eight studies described data collected in the 1970s and early 1980s. (Note that the results from older studies showing waning immunity among older adults16,19,25,26 may be attributable to the HAV IgG/IgM assay in use in the 1970s and early 1980s, which was found to have poor reliability for serum samples with low titres.27 New test kits were introduced in the 1980s, and waning immunity among older adults has not been observed in studies conducted since then.)
Table 1.
Descriptions of age-seroprevalence studies from West Africa, in reverse chronological order
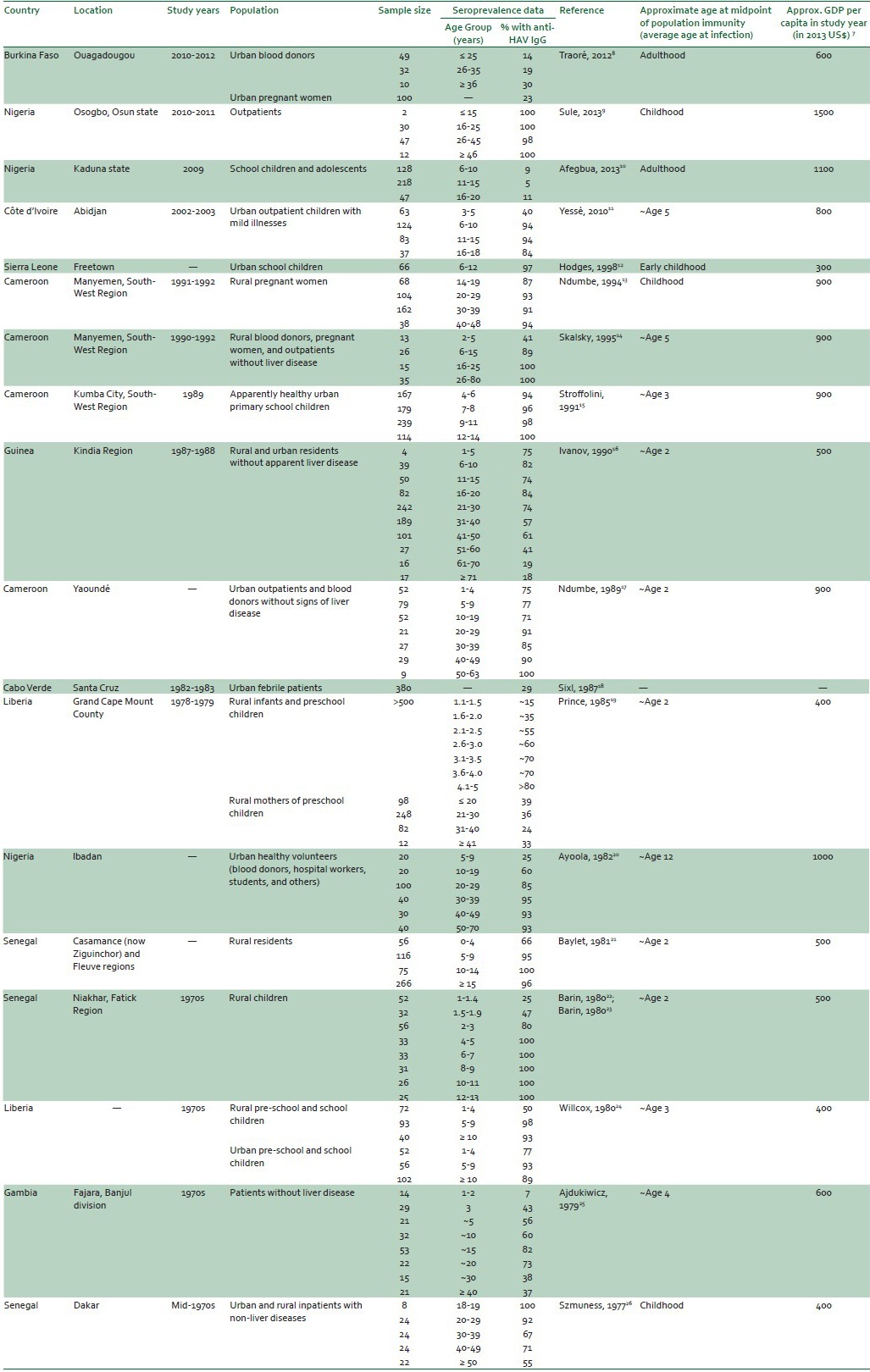
All but one of the studies with data collected prior to 1990 found that the age at midpoint of population immunity was in early childhood. The one study from this time period with an age at midpoint of population immunity in older childhood was from an urban population in Nigeria,20 a country that had a much higher GDP per capita than the countries hosting other pre-1990 studies.
In contrast, many of the studies with data collected after 1990 suggested an age at midpoint of population immunity in school-aged children. The one study from this more recent time period that included young children and had an age at midpoint of population immunity in early childhood was conducted in Sierra Leone,12 which had a much lower GDP per capita than other post-1990 study countries. All of the studies from all data collection years in which the countries had a GDP per capita (in 2013 international dollars) of $500 or less had an age at midpoint of population immunity of less than 5-years old. Countries with higher GDPs showed a range of ages at midpoint of population immunity ranging from less than 5 years old to early adolescence or even adulthood.
DISCUSSION
Many populations in the West-African region continue to have an age at midpoint of population immunity in early childhood, and therefore can be considered to have ‘very high’ endemicity. However, there is preliminary evidence that some West-African populations, especially those in countries with relatively higher GDPs, are beginning to shift from ‘very high’ endemicity with an age at midpoint of population immunity of less than 5 years toward a ‘high’ endemicity level with an age at midpoint of population immunity of 5-14 years.6 Further investigations of the seroprevalence rates in children in diverse parts of West Africa (including higher-income urban areas as well as lower-income and rural areas) will be required in order to clarify the extent to which an early transition may be occurring.
At present, there is no evidence that universal vaccination is indicated in any West-African country, and visitors to the region from lower-endemicity areas should still be advised to receive pre-travel vaccinations.6 However, if lower incidence rates are maintained for the next decade or longer, a growing proportion of adolescents and young adults — especially those who live in relatively high income, urban areas — may remain susceptible to HAV. At that time, public health officials in West-African countries may wish to consider whether targeted hepatitis A vaccination would be beneficial to some populations within their countries.6 In the meanwhile, clinicians practicing medicine in West Africa should be aware of the growing possibility of acute hepatitis A among older children, adolescents and young adults.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jacobsen KH, Koopman JS. Declining hepatitis A seroprevalence: A global review and analysis. Epidemiol Infect. 2004;132:1005–22. doi: 10.1017/s0950268804002857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobsen KH, Koopman JS. The effects of socioeconomic development on worldwide hepatitis A virus seroprevalence patterns. Int J Epidemiol. 2005;34:600–9. doi: 10.1093/ije/dyi062. [DOI] [PubMed] [Google Scholar]
- 3.Jacobsen KH, Wiersma ST. Hepatitis A virus seroprevalence by age and world region, 1990 and 2005. Vaccine. 2010;28:6653–7. doi: 10.1016/j.vaccine.2010.08.037. [DOI] [PubMed] [Google Scholar]
- 4.Jacobsen KH. Geneva: World Health Organization; 2009. The global prevalence of hepatitis A virus infection and susceptibility: A systematic review. Report No. WHO/IVB/10.01. [Google Scholar]
- 5.Addis Ababa: ECA; 2013. United Nations Economic Commission for Africa. Economic report on Africa 2013. Making the most of Africa's commodities: Industrializing for growth, jobs and economic transformation. [Google Scholar]
- 6.Mohd Hanafiah K, Jacobsen KH, Wiersma ST. Challenges to mapping the health risk of hepatitis A virus infection. Int J Health Geogr. 2011;10:57. doi: 10.1186/1476-072X-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United nations statistics division. Per capita GDP at current prices – US dollars. [Last access date on 2013 Dec 05]. Available from: http://data.un.org .
- 8.Traoré KA, Rouamba H, Nébié Y, Sanou M, Traoré AS, Barro N, et al. Seroprevalence of fecal-oral transmitted hepatitis A and E virus antibodies in Burkina Faso. PLoS One. 2012;7:e48125. doi: 10.1371/journal.pone.0048125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sule WF, Kajogbola AT, Adewumi MO. High prevalence of anti-hepatitis A virus immunoglobulin G antibody among healthcare facility attendees in Osogbo, Nigeria. J Immunoassay Immunochem. 2013;34:75–82. doi: 10.1080/15321819.2012.683502. [DOI] [PubMed] [Google Scholar]
- 10.Afegbua SL, Bugaje MA, Ahmad AA. Seroprevalence of hepatitis A virus infection among schoolchildren and adolescents in Kaduna, Nigeria. Trans R Soc Trop Med Hyg. 2013;107:627–30. doi: 10.1093/trstmh/trt072. [DOI] [PubMed] [Google Scholar]
- 11.Yessé ZN, Thérèse KAB, Serge OA, Everali A, Guillaume LY. Seroprevalence and risk factors of hepatitis A virus among school children from different socioeconomic status in Abidjan, Cote d’Ivoire. J Med Medical Sci. 2010;1:65–70. [Google Scholar]
- 12.Hodges M, Sanders E, Aitken C. Seroprevalence of hepatitis markers; HAV, HBV, HCV and HEV amongst primary school children in Freetown, Sierra Leone. West Afr J Med. 1998;17:36–7. [PubMed] [Google Scholar]
- 13.Ndumbe PM, Skalsky J, Joller-Jemelka HI. Seroprevalence of hepatitis and HIV infection among rural pregnant women in Cameroon. APMIS. 1994;102:662–6. doi: 10.1111/j.1699-0463.1994.tb05217.x. [DOI] [PubMed] [Google Scholar]
- 14.Skalsky JA, Joller-Jemelka HI, Bianchi L, Knoblauch M. Liver pathology in rural south-west Cameroon. Trans R Soc Trop Med Hyg. 1995;89:411–4. doi: 10.1016/0035-9203(95)90034-9. [DOI] [PubMed] [Google Scholar]
- 15.Stroffolini T, Chiaramonte M, Ngatchu T, Rapicetta M, Sarrecchia B, Chionne P, et al. A high degree of exposure to hepatitis A virus infection in urban children in Cameroon. Microbiologica. 1991;14:199–203. [PubMed] [Google Scholar]
- 16.Ivanov AP, Ivanova OE, Pozdniakov SV, Andzhaparidze AG, Kusov IuIu, Donets MA. [The results of serological research to determine hepatitis A and B markers in the blood sera of the population of the Republic of Guinea] Vopr Virusol. 1990;35:382–4. [PubMed] [Google Scholar]
- 17.Ndumbe PM, Njie TK. Hepatitis A and B infections in Youndé, Cameroon. Res Virol. 1989;140:253–61. doi: 10.1016/s0923-2516(89)80102-5. [DOI] [PubMed] [Google Scholar]
- 18.Sixl W, Sixl-Voigt B. Serological screenings of various infectious diseases on the Cap Verde Islands (West Africa) J Hyg Epidemiol Microbiol Immunol. 1987;31:469–71. [PubMed] [Google Scholar]
- 19.Prince AM, Brotman B, Richardson L, White T, Pollock N, Riddle J. Incidence of hepatitis A virus (HAV) infection in rural Liberia. J Med Virol. 1985;15:421–8. doi: 10.1002/jmv.1890150411. [DOI] [PubMed] [Google Scholar]
- 20.Ayoola EA. Antibody to hepatitis A virus in healthy Nigerians. J Natl Med Assoc. 1982;74:465–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Baylet R, Lemaire JM, Ridet J. Sero-epidemiology of hepatitis A. Results obtained in Senegal (Fleuve and Casamance regions) (author's transl) Pathol Biol. 1981;29:217–21. [PubMed] [Google Scholar]
- 22.Barin F, Denis F, Chotard J, Paulin R, Chiron JP, Maupas P, et al. Early asymptomatic hepatitis A in Senegalese children. Lancet. 1980;1:212–3. doi: 10.1016/s0140-6736(80)90706-0. [DOI] [PubMed] [Google Scholar]
- 23.Barin F, Denis F, Chotard J, Paulin R, Diop Mar I, Chiron JP, et al. Sero-epidemiological study of hepatitis A infection in Senegalese children (author's transl) Ann Pediatr. 1980;27:539–42. [PubMed] [Google Scholar]
- 24.Willcox M, Brohult J, Olsson I, Bengtsson E. Antibody to hepatitis A virus in Liberians. Trans R Soc Trop Med Hyg. 1980;74:690. doi: 10.1016/0035-9203(80)90174-1. [DOI] [PubMed] [Google Scholar]
- 25.Ajdukiewicz A, Mosley JW. Hepatitis-A-virus exposure in the Gambia. Lancet. 1979;2:966. doi: 10.1016/s0140-6736(79)92667-9. [DOI] [PubMed] [Google Scholar]
- 26.Szmuness W, Dienstag JL, Purcell RH, Stevens CE, Wong DC, Ikram H, et al. The prevalence of antibody to hepatitis A antigen in various parts of the world: A pilot study. Am J Epidemiol. 1977;106:392–8. doi: 10.1093/oxfordjournals.aje.a112481. [DOI] [PubMed] [Google Scholar]
- 27.Cuthbert JA. Hepatitis A: Old and new. Clin Microbiol Rev. 2001;14:38–58. doi: 10.1128/CMR.14.1.38-58.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]


