Abstract
Background:
Method of testing clinical competence of medical students in this setting has been controversial. This report evaluates the perceptions and preferences of 5th and 6th year medical students about traditional clinical examination (TCE) and objective structured clinical examination (OSCE).
Materials and Methods:
A cross-sectional study using a structured questionnaire, administered to 156 students, who had been previously exposed to TCE and OSCE.
Results:
There were 110 (70.5%) males and 46 (29.5%) females, with median age group of 26–30 years. One hundred and thirty-one respondents (84%) felt TCE is more difficult and 20 (12.8%) felt OSCE was more difficult. One hundred and forty-two (91%) felt OSCE was easier to pass, 8 (5.1%) felt TCE was easier to pass and 6 (3.8%) were undecided. Majority of the 5th and 6th year students (95.5% and 100%, respectively) preferred OSCE for assessment. In relation to validity and reliability of OSCE, 124 (79.5%) of all the students felt it provides a true measure of essential clinical skills, 130 (83.3%) felt its scores are standardised, 143 (91.7%) felt it is a practical and useful experience and 135 (86.5%) felt students’ personality, ethnicity and gender will not affect OSCE scores. Overall, there were no significant differences in preference and perceptions between 5th and 6th year students and between males and females.
Conclusion:
Students preferred OSCE as method of assessing clinical competence and considered it a more valid and reliable method of examination.
Keywords: Clinical year medical students, objective structured clinical examination, perceptions, preferences, traditional clinical examination
INTRODUCTION
Medical students in the clinical years are required to undergo various tests in their training to become doctors. There are 2 main methods used to assess these students: the traditional clinical examination (TCE) and objective structured clinical examination (OSCE).1,2 The need for a new method of assessing students clinically arose because of certain flaws noticed in TCE.2,3,4
This is a report of a study ascertaining the preference and perceptions of clinical year medical students regarding the use of TCE and OSCE for their assessment.
MATERIALS AND METHODS
A cross-sectional survey using a structured questionnaire that was self-administered to 5th and 6th year medical students who had previously passed through a 16-week posting and had been assessed using both TCE and OSCE. Permission for the study was obtained from the Ethical Committee of the Ahmadu Bello University Teaching Hospital, Zaria, Nigeria. The results were analysed using Excel Analyse-it®. Level of statistical significance was set at P < 0.05.
RESULTS
There were 146 students in the 5th year and 144 in the 6th year. Every student who attended lectures on the day of the study and consented was given the questionnaire by two of the authors to complete. A total of 156 out of the 290 students completed and returned the questionnaire. The questionnaire sought demographic information and the students’ views and perception about TCE and OSCE. The respondents included 110 males and 46 females (5th year 88, 6th year 68) with median age group of 26-30 years.
Comparing OSCE and TCE, 131 (84%) respondents felt TCE was a more difficult examination and 142 (91%) felt OSCE was easier to pass [Figure 1]. One hundred and fifty-two (97.4%) felt that OSCE is a more objective test than TCE. Eighty-four (95.5%) of 5th year and all (68, 100%) of 6th year students preferred OSCE for assessment of their clinical competence [Figure 2].
Figure 1.
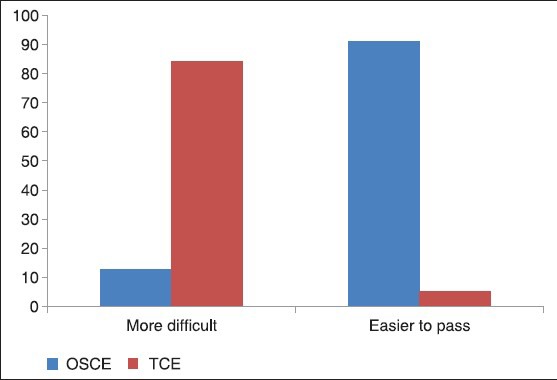
Perceptions of clinical year student about OSCE and TCE
Figure 2.
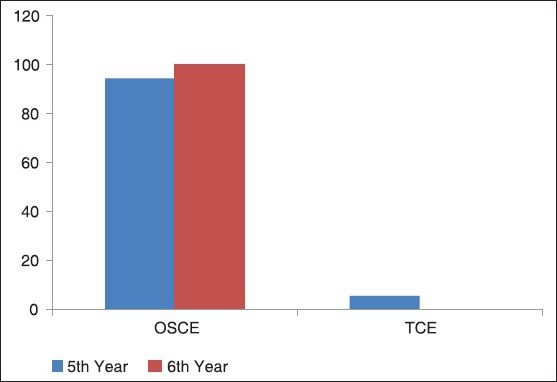
OSCE Vs TCE: Preference of 5th and 6th Year clinical students
One hundred forty-eight (94.9%) students indicated that OSCE is a fair examination [Table 1]. Majority of the students felt that OSCE covers a wide knowledge area (142, 91.7%) and wide range of clinical skills (126, 80.8%) and reduces the chances of failing (112, 71.8%). Most of the students felt that tasks included in OSCE examinations reflect tasks taught (120, 76.9%), setting and context of station felt authentic (114, 73.1%), tasks they were asked to perform were fair (138, 88.5%) and that the OSCE examination provided opportunities to learn (116, 74.4%).
Table 1.
Student’ perception about OSCE
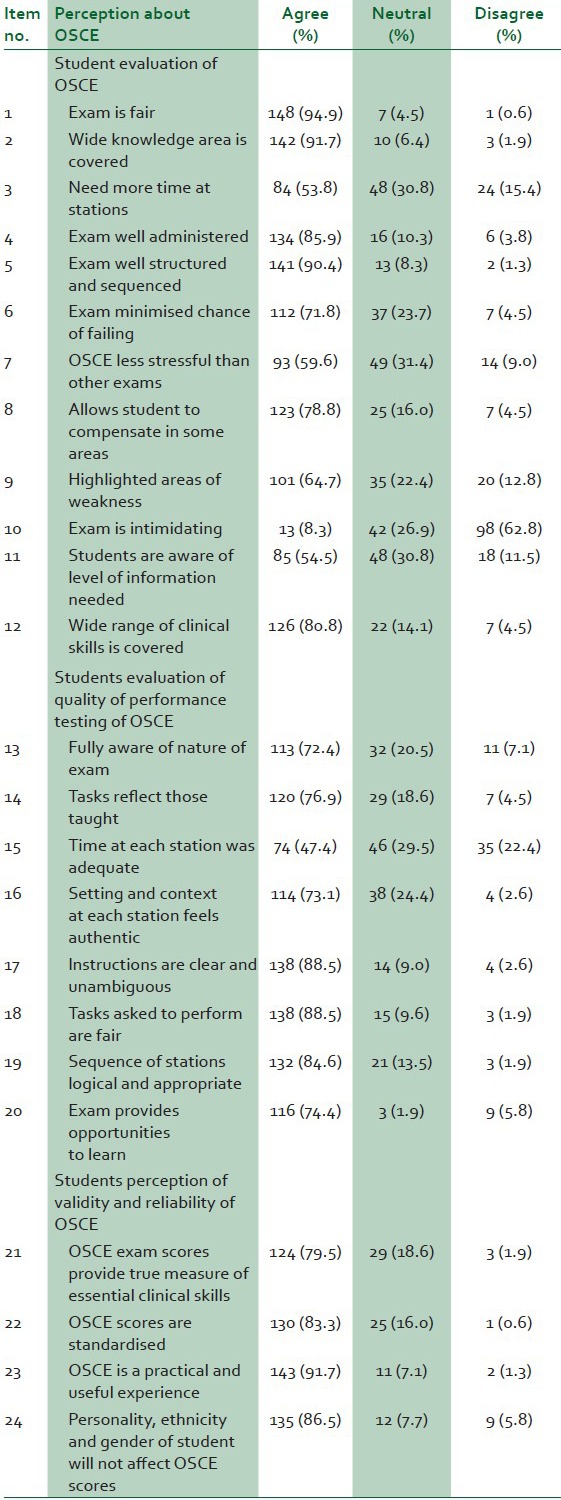
Regarding the reliability and validity of the OSCE examination, most student indicated that the examination scores provided a true measure of essential clinical skills (124, 79.5%), the examination is a practical experience (143, 91.7%) and is not affected by students’ personality, ethnicity and gender (135, 86.5%). Overall, there was no statistically significant difference in perceptions and preferences between 5th and 6th year students and between males and females [Figure 3].
Figure 3.
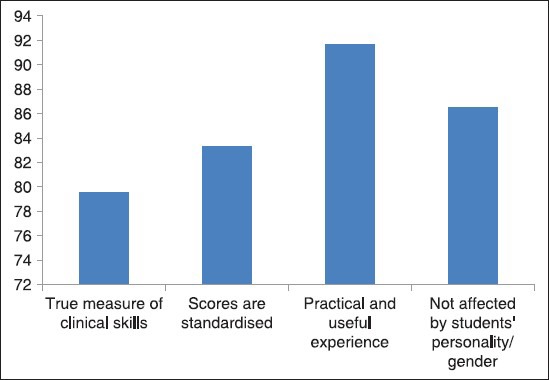
Perceptions of students on validity and reliability of OSCE
DISCUSSION
OSCE is gradually being recognised and adapted by medical faculties all over the world.5,6,7 Since its inception in the 1970s, its use is spreading to other continents including Africa and Nigeria, particularly. It was introduced into our department more than a decade ago.6 Dissatisfaction with previous methods of clinical assessment by both teachers and students led to a search for a more appropriate method and the creation of OSCE by Harden and colleagues in 1975.7
Four criteria, mainly those of validity, reliability, objectivity and practicability, must be considered in the use of any method for assessment of clinical competence of students.8 Validity is defined as the extent to which an instrument measures what it is supposed to assess. The students in the present report, as in other reports, consider OSCE to be more valid than the TCE. Reliability addresses the consistency of an instrument's measurement; that is, would the instrument measure the same way always or over and over again.8 The students in the present report, as in other reports,9,10 felt that OSCE was more valid and reliable than TCE because everyone is assessed on the same kind of patient, whether real or virtual and all the questions are the same even at the viva voce stations.9
The use of objectivity is obviously more reliable in an OSCE examination than a TCE. The students in the present report, felt that the OSCE score is not influenced by ethnicity, religion or gender. This is true only to some extent because the examiners still have to score the candidates after observing their performance at the manned station and so the scoring can still be affected by gender, religion or ethnicity.
The students felt the OSCE covers a wider range of topics than the TCE and allows them to make up for any areas they may have performed poorly.11 This is true to the extent that the student does not mix up the answers with the wrong questions. This is important as some complained of feeling stressed by the OSCE and not having enough time at the stations. This is similar to other studies where a few students made similar complaints, but most students did not perceive these as a problem. The pitfall is that unlike in the TCE where a student can be safely guided out of trouble, in the OSCE the examiners do not communicate with the students and so cannot correct an erring student.
A technique of student assessment has a huge impact on their study strategies, their performance and general attitude towards a subject.12 Faulty methods of assessment can lead to wrong decisions on the part of the examiners on the one hand and to the future activity of students including the welfare of the community whom they will serve in the future on the other hand.7 The students in this report, as in other reports,5,6 felt that OSCE was easier to pass and less difficult than TCE. Whether this implies that an easier and less difficult method of examination leads to the promotion of weak students who would have otherwise failed if a more difficult and challenging method of assessment was used is yet to be ascertained. This is also important because in real life, patients are not usually standardised, valid, reliable or objective but vary in all these areas from one patient to another and depend on the ethnicity (language barriers), gender and even religion of the doctors attending to them.
A study described OSCE as making students to manage patients in bits rather than as a whole individual and that study felt that OSCE is less holistic and is a shortcut of the real scenario of clinical practice, unlike TCE.10
Some examiners also favour the OSCE in view of the shorter time it takes to examine a large group of students.5 This is true because many streams can run concurrently, but after the OSCE, the time spent in marking the students’ OSCE scripts can be tasking and can even overshoot the total time of the TCE since in TCE no clinical scripts are marked, the students are scored on the spot. This may also account for the higher cost of organising an OSCE compared with TCE.5
The OSCE type employed in our institution is highly modified and standardised because it consists of various examination methods packaged into one. It will also be useful if the teaching methods can be re-assessed with the intent to prepare students to sit for the OSCE. In one report,13 video-projected structured clinical examinations were used instead of the traditional viva to assess final year medical students.
Further studies would be necessary to ascertain if there is any difference in actual clinical performance of doctors who are assessed by OSCE and TCE during their clinical years and what impacts the method of assessment has on patient management after graduation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Harden RM, Gleeson FA. Assessment of clinical competence using an objective structured clinical examination (OSCE) Med Educ. 1979;13:41–54. [PubMed] [Google Scholar]
- 2.Johnson G, Reynard K. Assessment of an objective structured clinical examination (OSCE) for undergraduate students in accident and emergency medicine. J Accid Emerg Med. 1994;11:223–6. doi: 10.1136/emj.11.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guraya SY, Alzobydi AH, Salman S. Objective structured clinical examination. Examiner's bias and recommendations to compare its reliability. J Med Med Sci. 2010;17:269–72. [Google Scholar]
- 4.Smith J, Plotkin M, Vinh Q, Thanh CN, Huu NV, Ha NT, et al. Introduction of OSCE for clinical assessment in obstetrics and gynaecology in Hue, Vietnam. South East Asian J Med Educ. 2008;2:25–30. [Google Scholar]
- 5.Eldarir SA, El Sebaae HA, El Feky HA, Hussein HA, El Fadil NA, El Shaeer IH. An introduction of OSCE versus traditional method in nursing education: Faculty capacity building and students’ perspectives. J Am Sci. 2010;6:1002–14. [Google Scholar]
- 6.Pierre PB, Wierenga A, Barton M, Branday JM, Christie CD. Student evaluation of an OSCE in paediatrics at the University of West Indies, Jamaica. BMC Med Educ. 2004;4:22. doi: 10.1186/1472-6920-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barman A. Critiques on the objective structured clinical examination. Ann Acad Med Singapore. 2005;34:478–82. [PubMed] [Google Scholar]
- 8.Rasoulian M, Taghva A, Panaghi L, Salehi M, Zahiraldin A, Ghalebandi MF. A qualitative study of psychiatrist's view about a pilot objective structured clinical examination (OSCE) in Iran. Iran J Psychiatry Behav Sci. 2007;1:27–9. [Google Scholar]
- 9.Smith LJ, Price DA, Houston IB. Objective structured clinical examination compared with other forms of student assessment. Arch Dis Child. 1984;59:1173–6. doi: 10.1136/adc.59.12.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazarus J, Kent AP. Student attitudes towards the objective structured clinical examination (OSCE) and conventional methods of assessment. S Afr Med J. 1983;64:390–4. [PubMed] [Google Scholar]
- 11.Khattiab AD, Rawlings B. Assessing nurse practitioners students using a modified objective structured clinical examination (OSCE) Nurse Educ Today. 2001;21:541–50. doi: 10.1054/nedt.2001.0590. [DOI] [PubMed] [Google Scholar]
- 12.Wanstall H. Objective structured clinical examination (OSCE) as predictors of performance on work-based placements. Investig Univ Teach Learn. 2010;6:57–64. [Google Scholar]
- 13.El Shallaly GH, Ali E. Use of Video-Projected Structured Clinical Examination (ViPSCE) instead of traditional oral (viva) examination in the assessment of final year medical students. Educ Health. 2004;17:17–26. doi: 10.1080/13576280310001656123. [DOI] [PubMed] [Google Scholar]


