Abstract
Background:
Anemia is the most common blood disorder observed in vulnerable groups and affects their efficiency in their everyday activities. Possible complications of the disease may be reduced or prevented by screening of patients. Screening programs impose certain costs upon the health system, which may offset their positive effects. Whether the positive impacts of screening outweigh its costs is a subject of debate among policy-makers. In this research, we have conducted a systematic review of the cost-effectiveness of anemia screening.
Methods:
The Pubmed, Science Direct, SCOPUS, EMBASE, and CINAHL databases were searched for relevant results dating between 1962-2010 using key words. The references of the related articles were gone over manually. In the end, Persian databases were also examined for results.
Results:
Using data from the four mentioned databases, a total of 722 articles were elected, which, after evaluation, were narrowed down to 4. Of these, 3 focused on newborns and infants. Disparity existed among obtained results, such that no two articles were similar, and this made making comparisons between them cumbersome and sometimes even impossible. Only one study evaluated cost-effectiveness of anemia screening in vulnerable target groups.
Conclusions:
Research findings show that there is not enough evidence of cost-effectiveness of screening for decision-making. Bearing in mind the importance of the matter to health policy-makers, due to high prevalence of iron-deficiency anemia in low- and middle-income countries, conduction of research in this field seems necessary.
Keywords: Anemia, cost-effectiveness, screening, systematic review
INTRODUCTION
Anemia is the most common blood disorder in low- and middle-income countries (LMICs)[1,2,3] Globally, over two billion people suffer from anemia, specially vulnerable groups such as women and children[4] including 10% and 42% of women in LMICs and high-income countries, respectively[5] Anemia treatment results in 10-30% increase in productivity[1,2,3] Anemia screening is recommended in certain groups in some countries. The national screening committee of England recommended the use of the anemia screening policy in at-risk groups in 2007.[6]
But, screening is costly to the health system. That is why cost-effectiveness of the policy is debated amongst policy-makers. In recent years, policy-makers in Iran have shown interest in the use of anemia screening in vulnerable women[7] In this study, we systematically reviewed international evidence for the cost-effectiveness of screening in the diagnosis and treatment of iron-deficiency anemia.
METHODS
Study design
This study is a systematic review of cost-effectiveness of anemia screening.
Inclusion criteria
Articles were chosen that gave a report of cost-effectiveness of anemia screening. In addition, articles that focused on the economic burden resulting from anemia in people with underlying illnesses were also paid particular attention to, as well as those which analyzed cost-effectiveness of screening in various blood disorders.
Search strategy
In order to find articles related to cost-effectiveness of anemia screening, a search of articles in international databases up to April 2011 was conducted. The search was limited to articles written in the English language.
In addition, a separate study was conducted of articles in Persian databases. In order to separate related articles, advanced and subject-specific search options were used as follows. At first, a sensitive search strategy was designed, and the major databases (Pubmed, Science Direct, SCOPUS, EMBASE and CINAHL) were searched for relevant results from 1962-2011. The dominant search strategy used was as follows: (Anemia OR Anaemia) AND (economic OR cost OR burden). Other relevant strategies were also used, such as anemia case finding or anemia AND screening. In order to increase chances of finding relevant articles, the databases BMJ, EBM review, tripdatabase, and Cochrane were searched separately. Relevant printed articles such as those released by WHO concerning anemia were also gone over manually.
Due to the mother tongue of the conductors of this study being Persian, Persian scientific databases such as SID (www.sid.ir) and IranMedex (www.iranmedex.com) were searched using relevant Persian key-words. This latter search yielded no relevant studies; the majority of studies carried out in Iran concerning anemia focused on its distribution and frequency throughout the country.
RESULTS
Study selection, data extraction, and analysis
Initially, the selected articles were entered into article managing software, and duplicate articles were eliminated. The titles of the remaining articles were then analyzed by a team of 4 author and those that were clearly irrelevant were also eliminated. All the abstracts of the remaining articles were assessed for inclusion by authors. The studies that we all agreed that they were unrelated to our study were omitted at this stage. The complete text of the remaining articles prepared and analyzed in a group meeting, and decisions were made regarding their suitability to be entered into the study. These articles were none of them similar enough to the others for synthesis to be put into effect and, therefore, each was analyzed separately [Figure 1].
Figure 1.
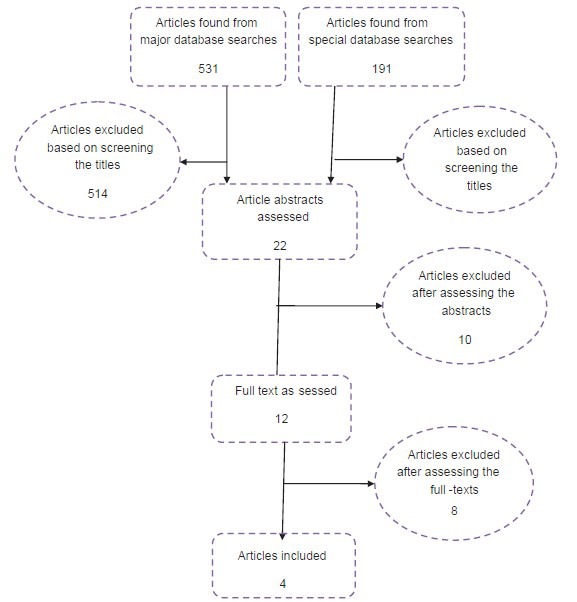
Summary of the articles found
Seven hundred and twenty-two articles were separated from scientific databases, 700 of which were eliminated after analysis of the title of the article. Analysis of a summary of the remaining 22 articles narrowed them down to 12. Of these 12 articles, examination of the full article found 4 to be completely relevant to the subject in question. All these studies were found to have been conducted in the US, and of these 4 studies, only 1 had assessed cost-effectiveness of anemia in a healthy target group (neonates), and 2 had assessed cost-effectiveness in patients suffering from blood-related disorders such as sickle-cell anemia and hemoglobin-related diseases. As a whole, results showed that little research has been done on cost-effectiveness of anemia-screening.
Quality appraisal
The quality of the accepted articles was analyzed using CASP.[8] The quality of all the articles was found to be satisfactory; article[9] was found to have the highest score. A summary of the 4 articles found to be relevant after complete analyses can be found in Table 1.
Table 1.
Summary of the studies conducted about cost-effectiveness of anemia screening

Summary of related articles
In a study conducted by Hutchinson et al., (1997) 48 ESRD (End-Stage Renal Disease) patients consisting of 45 men and 3 women with an average age of 61.8 years were assessed. The aim of the research was analysis of the cost-effectiveness of anemia screening in these patients before they underwent therapy with erythropoietin. Effectiveness data was gathered from patients who had referred there for anemia-screening between the years 1992 and 1995, and cost-related data was gathered from the same sample.
In this study, direct costs consisted of the costs of evident services, such as screening tests, EPO drug therapy lasting a month, and other EPO therapy-related costs (such as the costs of syringes, hiring of nurses etc). Indirect costs were not taken into account. Effectiveness was calculated by the number of patients who showed positive on screening tests.
The total cost of iron-deficiency screening was $862.22 (48 patients, screening costs for each amounted to $18.01). EPO drug therapy using a standard dose over a period of 4 weeks amounted to $172 per capita. Twenty-five patients in the sample suffered from iron-deficiency and did not respond to EPO treatment. Therefore, the non-effective cost was 25 * 172 = 4300 dollars.
The cost of saving is calculated by dividing the total cost of anemia screening by the cost of non-efficient EPO treatment, which equals $862.22/4300= $0.2019, or, stated more simply, $4.95 per every dollar that is spent on screening tests. In other screening tests, the cost of saving is greater than 1 dollar.[10]
In a research conducted by Shaker (2008), with an aim of analyzing cost-effectiveness in the prevention of iron-deficiency anemia in early childhood (9-12 months), 3 different screening strategies were assessed:
Hb test, which is a common method used in anemia diagnosis (Hb < 11 g/dl)
CHr test, which shows decreased iron levels before the onset of anemia, and
CBC test.
The aim of these tests is early diagnosis of anemia in children. Two different methods, short-term (by ‘decision tree’) and long-term (for period of 10 years, by ‘Markov model’), were used in the analysis of the cost-efficiency of the different iron-deficiency screening strategies (Hb, CHr, CBC).
Costs in the long-term method are calculated using a 3% discounting rate for services and goods. Approximate costs of anemia screening tests were calculated using laboratory tariffs, and the cost for anemia treatment was estimated at $20.30 per month.
Screening using the CHr test correctly diagnoses 33% of anemic children, and with the help of the HB test, a further 7% can be correctly diagnosed. Screening via CHr costs $31 per newborn and $440 per each case diagnosed. Anemia screening via Hb and CBC cost $9 and $15, respectively. Final cost of anemia prevention by CHr surmounts to $22 per newborn, $25 by Hb, and $55 by CBC screening.
Research shows that for children aged between 9 and 12 months, CHr is an appropriate screening method. Early diagnosis of anemia lessens the amount of time required for its successful treatment, and this results in the overall cost of anemia prevention being near the sum $180 per patient.[11]
Panepinto's research (1999) consists of 3 strategies
No screening
Screening of a certain target group (American infants of African descent)
Screening of all newborn infants in the USA.
Approximately 1 million infants of different races born in America in the year 1994 were screened for sickle cell disease. Infants who tested positive started penicillin prophylactic treatment and their parents participated in courses that trained them in delivering complementary care. Infants who were not screened or failed to take follow-up measures after screening received no antibiotics or complementary care.
Screening of the target group (African Americans) proved to be cost-effective in comparison with not screening, whereas screening a larger group of newborns helped diagnose many cases and prevent many deaths (high effectiveness) but was also extremely costly.
Total costs per life saved in targeted screening amounted to $3575, as opposed to $16353 for universal screening.[9]
Another research was conducted by Gessner (2001). In this study, 4 different Hb screening strategies were analyzed for use among newborns, with the aim of preventing complications arising from sickle-cell anemia.
The strategies in use were:
Universal screening with complete follow-up procedures (USCF)
Targeted screening with selective follow-up (TSSF)
Universal screening with selective follow-up (USSF)
Targeted screening with complete follow-up (TSCF)
Universal screening means screening of all newborns, while targeted screening means screening of black newborns.
Selective follow-up refers to the follow-ups of all newborns whose unnatural consists of homozygous or heterozygous Hb, whereas complete follow-up refers to the follow-up who have unnatural hemoglobin in any form.
Follow-up consists of contacting the newborn's family and offering them advice and information on drug interventions and hemoglobin pathology tests.
The aim of the study was evaluation of cost-effectiveness of the screening methods in comparison with there being no screening in preventing SCD complications from a health-care system viewpoint.
Hypotheses and estimations in this study were made based on researches that had taken place between the years 1972-1991, and the decision tree was used for estimation of costs and effectiveness of each strategy.
The most important achievement of this screening is the prevention of death and mental retardation in newborns. Another achievement is the identification of cases of homozygous or compound heterozygous hemoglobinopathy. The costs of this study comprised direct costs of screening (costs of lab tests and cost of therapy). Indirect costs were not taken into account.
The number of deaths prevented via the 4 different screening strategies is as follows:
0.026 in the TSCF strategy, 0.039 in USCF, 0.026 in TSSF, and 0.039 in USCF, and the number of cases of mental retardation prevented have been approximated at 0.001, 0.0015, 0.001, 0.0015, respectively. Total net expenditures for a 1-year screening period in Alaska for TSCF, USCF, TSSF, and USCF are $17011, $69453, $5361, and $31863, respectively.
In this study, cost of every one unit of effectiveness (each life saved) for the 4 different strategies is as follows: $654000 for the TCSF strategy, $1780000 for the USCF strategy, $206000 for the TSSF strategy, and $817000 for the USCF strategy.[12]
DISCUSSION
Search results that little studies have been done on anemia screening, and none has been done on apparently healthy populations with no underlying diseases. It was also shown that no study has been done on cost-effectiveness of screening in vulnerable groups such as women. On the other hand, the sparse study done has covered a wide range of methods and focused on people from different age-groups, suffering from different kinds of anemia, and different complications, which made it difficult to compare obtained results.
The 4 selected articles had all done in the USA. Three of them focused on newborns and children. For example,[11] focused on children of 9-12 months and early diagnosis of anemia in these children and[9,10,11,12] focused on early diagnosis of newborns suffering from SCD, in order to prevent future complications and costs arising from this disease, reduce death rate and increase life expectancy.
In all these studies, absence of screening was used as a basis for evaluating the effectiveness of different screening methods. As most of these studies were evaluated from a health-care perspective, screening costs consist of direct costs (cost of screening tests and cost of early treatment), and the indirect costs and costs imposed on society were not taken into account.
The standard of effectiveness in these studies is timely diagnosis of anemic patients using lab tests, although analysis of the different articles showed considerable disparity in obtained results concerning cost-effectiveness, although all in all the practice of anemia screening was considered to be cost-effective in most cases.
Variance in estimated costs and effectiveness can be linked to the method used, the target group, and the effectiveness criteria focused upon.
To give an example for this, cost of anemia diagnosis in children was calculated to be $22, whereas the cost per lives saved and cost per each newborn death prevented are $3575 and $206000, respectively.
Several important results can be obtained from these studies: The most cost-effective anemia screening test in infants is CHr[11] and that anemia screening in ESRD patients before they start therapy with erythropoietin reduces treatment costs and is, therefore, cost-effective.[10]
This study has attempted to conduct a systematic review of economic evaluation research done in relation to anemia screening programs. It has tried to analyze all related articles on economic evaluation of anemia screening in different age groups that were written in English.
Unfortunately, great disparity exists among different studies conducted in this field, such that no two studies were alike, and this made comparison of obtained results difficult and sometimes nigh on impossible.
One of the few screening methods recommended is that of iron-deficiency anemia, especially among gestating women (e.g., recommendations and clinical guide of the Screening committee of England)[6]
Even though, comprehensive search methods show that only one research has been conducted on cost-effectiveness of screening in iron-deficiency anemia[1] in at-risk target groups, and none have focused on pregnant women. As well as that, cited evidence of screening recommendations mentioned above has not evaluated the effectiveness of these screening interventions.[13] The only exception to this is the research that conducted anemia screening in infants of less than one year.
In effect, results obtained by this study show that not enough evidence of cost-effectiveness exists for decision-making. Bearing in mind the importance of this issue for health policymakers, conduction of research in this field appears crucial.
Study of cost-effectiveness of anemia screening, alongside clinical trial of it, especially in countries which have a high prevalence of anemia due to demographic and epidemiologic traits (countries with low and middle incomes) would appear to be beneficial. For if screening results in better diagnosis and reduction of anemia in target groups, this method would appear to be a suitable one for reduction of iron-deficiency anemia in society, taking into account its low cost.
CONCLUSIONS
There is high prevalence of iron deficiency anemia in low and middle income countries that indicated the importance of cost - effectiveness of anemia screening to policy making. But the finding of systematic review study shows that there is not enough evidence of cost-effectiveness of screening, only one study evaluated the cost effectiveness of anemia screening in vulnerable target groups then conduction of research in this field seems necessary.
Footnotes
Source of Support: We received research funding from Ministary of Health and Medical Education for conducting this study
Conflict of Interest: None declared
REFERENCES
- 1.Benoist BD, McLean E, Egli I, Cogswell M. Geneva: World Health Organization; 2008. Worldwide prevalence of anaemia 1993-2005, report in WHO global database on anaemia. [Google Scholar]
- 2.Balducci L, Ershler WB, Krantz S. Anemia in crit rev oncol hemat. 2006;58:156–65. doi: 10.1016/j.critrevonc.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Burrener LS, Suddarth DS. Blood Diseases. In: Sami P, translator. Tehran: Boshra Publication; 2008. [Google Scholar]
- 4.Bharati P, Som S, Chakrabarty S, Bharati S, Pal M. Prevalence of anemia and its determinants among nonpregnant and pregnant women in India. APJPH. 2008;20:347–59. doi: 10.1177/1010539508322762. [DOI] [PubMed] [Google Scholar]
- 5.A guide for programme managers. Geneva, Switzerland: World Health Organization; 2001. Iron Deficiency Anaemia: Assessment, Prevention, and Control. [Google Scholar]
- 6.National Screening Committee. National Screening Committee's Policy - anemia screening, Editor: UK 2006 [Google Scholar]
- 7.Barooti E, Haghdoost AA, Hosseini H, Tabibzadeh Z, Bahmani S, Taheri S, et al. Vulnerable Household Women's Health Assessment (VH-WHAT): Protocol Design and Implemention. IRCMJ. 2010;12:358–64. [Google Scholar]
- 8.England: 2006. CASP critical appraisal checklists for economic evaluation studies, Public Health Resource Unit. Available: http://www.casp-uk.net/find-appraise-act/appraising-the-evidence . [Google Scholar]
- 9.Panepinto JA, Magid D, Rewers MJ, Lane PA. Universal versus targeted screening of infants for sickle cell disease: A cost-effectiveness analysis. The Journal of Pediatrics, 2000;136:201–8. doi: 10.1016/s0022-3476(00)70102-8. [DOI] [PubMed] [Google Scholar]
- 10.Hutchison FN, Jones WJ. A cost-effectiveness analysis of anemia screening before erythropoietin in patients with end-stage renal disease. AJKD. 1997;29:651–7. doi: 10.1016/s0272-6386(97)90116-5. [DOI] [PubMed] [Google Scholar]
- 11.Shaker M, Jenkins P, Ullrich C, Brugnara C, Nghiem BT, Bernstein H, et al. An economic analysis of anemia prevention during infancy. Journal of Pediatrics. 2009;154:44–9. doi: 10.1016/j.jpeds.2008.06.038. [DOI] [PubMed] [Google Scholar]
- 12.Gessner BD, Teutsch SM, Shaffer PA. A cost-effectiveness evaluation of newborn hemoglobinopathy screening from the perspective of state health care systems. Early Hum Dev. 1996;45:257–75. doi: 10.1016/0378-3782(96)01761-6. [DOI] [PubMed] [Google Scholar]
- 13.National Collaborating Centre for Women's and Children's Health, Antenatal care, routine care for the healthy pregnant woman, commissioned by the National Institute for Health and Clinical Excellence. 2008:120. [Google Scholar]


