Abstract
Background:
Type-D personality has been identified as a risk factor for general and cardiac mortality in patients with coronary artery disease (CAD). Dobutamine-atropine stress echocardiography (DASE) is an established method for non-invasive evaluation of myocardial ischemia in patients with CAD. The objective of this study was to evaluate the prevalence of type-D personality and its association with the occurrence of myocardial ischemia as assessed by DASE.
Methods:
This case-control study enrolled 306 patients (61 ± 9.6 years, 57.8% female) who were referred by physicians to assessment of myocardial ischemia. Before undergoing DASE, the patients answered the type-D scale, which identifies type-D personality.
Results:
Type-D personality was identified in 106 patients (34.6%). DASE was positive for myocardial ischemia in 32.4% (99) of 306 participants there was no significant association between type-D personality and ischemic changes on DASE (P = 0.941; odds ratio: 0.98; confidence interval 95%: 0.57-1.69). Chest pain was the only clinical variable with statistically significant prevalence in type-D personality patients (77.4% vs. 57.0%; P < 0.001).
Conclusions:
Type-D personality was not a significant risk factor for the presence of ischemic changes on DASE. Patients with type-D personality tended to complain more frequently of chest pain than non-type-D patients.
Keywords: Coronary artery disease, myocardial ischemia, psychological risk factor, stress echocardiography, type-D personality
INTRODUCTION
Efforts have subsequently been made to identify new predictors of coronary artery disease (CAD)[1,2,3] as 20% of coronary events occur in the absence of traditional risk factors.[4] To determine whether there are psychological risk factors for CAD has been a challenge for evidence-based medicine, however, it is not prudent to affirm that they do not affect it pathogenesis, since depression and psychological stress have been associated with increased risk of CAD.[5,6,7,8,9] Denollet et al. proposed that there is a type-D or “distressed” personality that describes individuals with high levels of negative affectivity (NA) and social inhibition (SI). NA is characterized by the tendency to experience negative emotions, and SI by the tendency to inhibit the expression of these emotions during social interactions, due to fear of disapproval or rejection by others.[10] High-NA individuals have a negative view of self and experience feelings of dysphoria, anxiety, irritability.[11] High-SI individuals tend to feel inhibited, tense, and insecure when with others.[11] NA and SI combine synergistically to influence clinical outcomes, and their interaction can be viewed as a form of stress that may induce or exacerbate serious health problems.[12,13] Type-D personality has been shown to have effects on cardiac prognosis independent of mood states such as anxiety and depression.[14,15] The first study to suggest that type-D personality had adverse health effects was published in 1995,[13] and other subsequent studies have shown type-D personality as an independent risk factor for general and cardiac mortality in patients with CAD.[10,16] The dobutamine-atropine stress echocardiography (DASE) for the detection of CAD is well-established both by American Heart Association/American College of Cardiology and European Society of Cardiology Guidelines.[17,18] This study aims to assess the prevalence of type-D personality and its association with the occurrence of myocardial ischemia as assessed by DASE.
METHODS
Study design and participants
This study has followed the guidelines of the Declaration of Helsinki and the Brazilian Resolution 196/96 for biomedical research in humans. The study was approved by the Ethics Committee on Human Research at the Clinical Hospital of the Universidade Federal do Paraná. The sample size for this study was based on previous studies that identified a 30% prevalence of type-D personality among patients with cardiac disease, and mortalities of 5% among non-type-D and 39% among type-D patients (16). For an α error of 95% and β error of 80%, 76 patients (57 non-type-D patients and 19 type-D patients) were needed for statistically significant results. This was a case-control study using a non-consecutive convenience sampling (according to availability of the researchers). The inclusion criterion was patients aged ≥18 years old, referred to assessment of myocardial ischemia by pharmacological stress echocardiography. Between March 2010 and April 2012, a total of 321 in- and out-patients were included in the study. Exclusion criteria were patients referred to DASE to assessment of pathologies other than myocardial ischemia, and patients with inconclusive DASE.
Study instrument and variable assessment
After filling out consent forms and before undergoing DASE, patients were asked about chest pain, presence of classic risk factors for CAD (age, smoking, hypertension, diabetes mellitus, dyslipidemia, sedentary lifestyle, obesity, drug therapy, family history of CAD), and a positive CAD history (defined as a history of myocardial infarction, angioplasty, or coronary artery bypass surgery). A questionnaire designed for type-D personality (DS14) was completed and were identified as type-D personality those individuals whose total NA and SI scores were ≥10. The standard DS14 presented construct validity and high level of internal consistency.[11] The standardized DASE protocol consisted of dobutamine infusion starting at 5 μg/kg/min and increasing at 3-min intervals to 10, 20, 30 and 40 μg/kg/min. Atropine, in divided doses of 0.25-0.5 mg to a total of 2.0 mg, was used as needed to achieve the target heart rate. Atropine could be used in early stages of the test, to reduce infusion times. At peak stress or during recovery, a beta-blocker was administered to reverse the side effects of dobutamine and increase test sensitivity. Interruption end points included the achievement of target heart rate (defined as 85% of the age-predicted maximum heart rate), significant arrhythmias, hypotension, severe hypertension, and intolerable symptoms. Positivity criteria were electrocardiographic ST segment changes (with > 2 mV ST segment shift) and new or worsening wall-motion abnormalities.[17,18] Patients whose DASE did not present new or worsening wall-motion abnormalities and who did not reach the target heart rate at the end of the protocol were excluded from the study (inconclusive DASE).
Statistical analysis
The mean age and standard deviation were determined. Frequencies and percentages were determined for qualitative variables. Fisher's exact test or the Chi-square test was used to evaluate the association between qualitative variables and the presence of ischemia on stress echocardiography. Multivariate analysis was performed by means of a logistic regression model. First, we evaluated the association between each variable and the presence or absence of ischemia. Variables that showed P < 0.20 were included in the multivariate model, adjusted for type-D personality. The Wald test was used to assess the effect of variables on the probability of ischemia on DASE. P < 0.05 was considered to be statistically significant. Data were analyzed using the software program Statistica version 8.0 (StatSoft, Inc., 2300 East 14th Street, Tulsa, Oklahoma, USA).
RESULTS
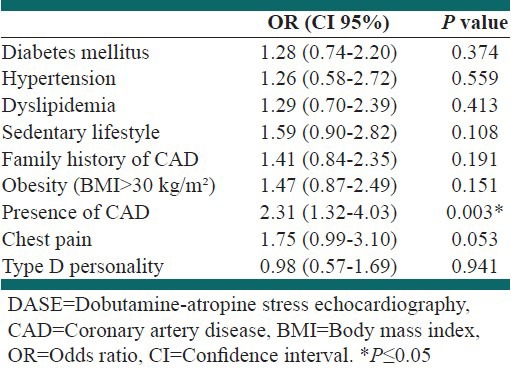
Of the 321 participants enrolled in the study, 15 (4.7%) were excluded as follows: 10 (3.1%) for inconclusive stress echocardiography; 2 (0.6%) with contraindications for undergoing DASE (abdominal aortic aneurysm), and 3 (0.9%) for incomplete data collection. Therefore, a total of 306 patients were included in the study. The mean age of participants was 61 ± 9.6 years and 57.8% were female. At the time of testing, 287 (93.8%) of the patients were under medical therapy, 82% taking antihypertensives, 58.5% statins, 29.1% oral hypoglycemic agents, 13.4% insulin, 59.5% platelet antiaggregants, and 17.3% antidepressants (tricyclics or selective serotonin reuptake inhibitors). The prevalence of type-D personality was 34.6% (106 patients). Regarding the classic risk factors for CAD, 38.9% of the patients had diabetes, 83.3% hypertension, 68.0% dyslipidemia, 69.6% sedentary lifestyle, 44.4% family history of CAD, 14.7% were smokers, 34.6% were obese (body mass index >30 kg/m2), 66.0% had visceral obesity, 34.0% CAD, and 10.5% presented cerebrovascular ischemia. To assess the prevalence of risk factors for CAD and sample homogeneity, the clinical characteristics were also analyzed according to personality type (D or non-D). Chest pain was the only statistically significant variable observed in 77.4% (82) of the type-D patients versus 57.0% (115) of non-type-D patients with P < 0.001. DASE was positive for myocardial ischemia in 32.4% (99) of the 306 participants. Univariate analysis for positivity on DASE showed that there was no significant difference in gender, age, visceral obesity, cerebrovascular ischemia, smoking, and type-D personality. For the logistic regression model for multivariate analysis, the authors included type-D personality, adjusted for diabetes, hypertension, dyslipidemia, sedentary lifestyle, familiar history of CAD, obesity, CAD, and chest pain. The results showed that, in the presence of those variables, there was no significant association between type-D personality and ischemic changes on DASE (P = 0.941; odds ratio [OR]: 0.98; confidence interval 95%: 0.57-1.69). Only the presence of CAD showed a significant difference (P = 0.003) for prediction of ischemia on DASE. Chest pain showed a tendency to positivity on DASE (P = 0.053) [Table 1].
Table 1.
Association between type D personality and ischemic changes on DASE adjusted for clinical characteristics
DISCUSSION
The present study revealed a high risk population for cardiovascular disease due to of the high prevalence of classic risk factors for CAD. The prevalence of type-D personality in this case-control study was similar to that observed in other studies.[7,19,20] Although the prevalence of type-D personality in this population was similar to that observed in the literature, type-D personality was not found to be a statistically significant risk factor for myocardial ischemia assessed by DASE. Recent reports have questioned the relevance of type-D personality as a risk factor for CAD. Grande et al.,[21] in a recent meta-analysis, identified a significant association between type-D personality and cardiovascular events. However, the importance of this association has been declining over the years (OR changed from 5.02 to 1.54) and studies with high methodological quality failed to confirm this association. In another study, Schmidt et al.[20] evaluated patients who underwent percutaneous coronary intervention and major cardiovascular events were not associated with type-D personality. In our study, among patients with and without type-D personality, there were no statistically significant differences in the prevalence of classical risk factors for CAD. However, Kupper et al.,[22] after evaluating 6222 patients with CAD in 22 European countries, concluded that there was a significant pancultural association between type-D personality and some cardiovascular risk factors, including hypertension, smoking, and sedentary lifestyle. Kuijpers et al.[23] observed that type-D personality was independently associated with psychopathology (panic disorder and depression) in patients referred to emergency rooms with non-cardiac-associated chest pain. In our study, chest pain was the only clinical variable with statistically significant prevalence in type-D personality patients. However, we could not identified significant correlation between chest pain and ischemic changes on DASE in this group. Some doubts still prevail about the pain pathophysiology in these patients: would they be more sensitive to ischemic and/or non-ischemic pain? Would they present a higher prevalence of non-cardiac chest pain? Would it be accounted for by the psychological characteristics and associated disorders of these patients? The present study confirmed the trend of recent findings that previous results might be spurious, leading to overestimations of the effects of type-D personality on the prognosis of cardiac patients. The authors argue that the practice of dichotomization of the interaction of NA and SI were methodologically problematic in type-D studies.[21,24,25,26] de Voogd et al.[26] argued that previous studies that identified type-D personality as a predictor of negative cardiovascular outcomes and mortality, came from small studies (4, 6, 8, 12 and 47 deaths)[10,27,28,29,30] conducted by a single investigative group (Denollet's group at Tilburg University). A larger study of mortality with 192 deaths, conducted by Coyne et al., identified no association between type-D personality and mortality.[31] Our study has some limitations, such as its cross-sectional nature, which does not allow to test the prognostic validity, and a pre-selected patient sample. Additional well-designed studies are needed to clarify the role of type-D personality in CAD patients.
CONCLUSIONS
The prevalence of type-D personality in the present study was similar to previously published results. Type-D personality was not a significant risk factor for the presence of ischemic changes on DASE. Patients with type-D personality tended to complain more frequently of chest pain than non-type-D patients.
ACKNOWLEDGMENT
This study is an integral part of the internal medicine thesis by Rafael Borsoi at the Universidade Federal do Paranα.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ridker PM. Evaluating novel cardiovascular risk factors: Can we better predict heart attacks? Ann Intern Med. 1999;130:933–7. doi: 10.7326/0003-4819-130-11-199906010-00018. [DOI] [PubMed] [Google Scholar]
- 2.Hackam DG, Anand SS. Emerging risk factors for atherosclerotic vascular disease: A critical review of the evidence. JAMA. 2003;290:932–40. doi: 10.1001/jama.290.7.932. [DOI] [PubMed] [Google Scholar]
- 3.Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C, et al. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006;355:2631–9. doi: 10.1056/NEJMoa055373. [DOI] [PubMed] [Google Scholar]
- 4.Braunwald E, Libby P, Zipes DP, Bonow RO. 7th ed. Philadelphia: Saunders Elsevier; 2006. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine; p. 947. [Google Scholar]
- 5.Suarez EC, Kuhn CM, Schanberg SM, Williams RB, Jr, Zimmermann EA. Neuroendocrine, cardiovascular, and emotional responses of hostile men: The role of interpersonal challenge. Psychosom Med. 1998;60:78–88. doi: 10.1097/00006842-199801000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 7.Hemingway H, Marmot M. Evidence based cardiology: Psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318:1460–7. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kop WJ. Chronic and acute psychological risk factors for clinical manifestations of coronary artery disease. Psychosom Med. 1999;61:476–87. doi: 10.1097/00006842-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med. 2002;23:51–61. doi: 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- 10.Denollet J, Vaes J, Brutsaert DL. Inadequate response to treatment in coronary heart disease: Adverse effects of type D personality and younger age on 5-year prognosis and quality of life. Circulation. 2000;102:630–5. doi: 10.1161/01.cir.102.6.630. [DOI] [PubMed] [Google Scholar]
- 11.Denollet J. DS14: Standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med. 2005;67:89–97. doi: 10.1097/01.psy.0000149256.81953.49. [DOI] [PubMed] [Google Scholar]
- 12.Kupper N, Denollet J. Type D personality as a prognostic factor in heart disease: Assessment and mediating mechanisms. J Pers Assess. 2007;89:265–76. doi: 10.1080/00223890701629797. [DOI] [PubMed] [Google Scholar]
- 13.Denollet J, Sys SU, Brutsaert DL. Personality and mortality after myocardial infarction. Psychosom Med. 1995;57:582–91. doi: 10.1097/00006842-199511000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Pedersen SS, Denollet J. Is type D personality here to stay? Emerging evidence across cardiovascular disease patient guoups. Curr Cardiol Rev. 2006;2:205–13. [Google Scholar]
- 15.Denollet J, Pedersen SS, Ong AT, Erdman RA, Serruys PW, van Domburg RT. Social inhibition modulates the effect of negative emotions on cardiac prognosis following percutaneous coronary intervention in the drug-eluting stent era. Eur Heart J. 2006;27:171–7. doi: 10.1093/eurheartj/ehi616. [DOI] [PubMed] [Google Scholar]
- 16.Denollet J, Sys SU, Stroobant N, Rombouts H, Gillebert TC, Brutsaert DL. Personality as independent predictor of long-term mortality in patients with coronary heart disease. Lancet. 1996;347:417–21. doi: 10.1016/s0140-6736(96)90007-0. [DOI] [PubMed] [Google Scholar]
- 17.Sicari R, Nihoyannopoulos P, Evangelista A, Kasprzak J, Lancellotti P, Poldermans D, et al. American Society of Echocardiography. Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC) Eur J Echocardiogr. 2008;9:415–37. doi: 10.1093/ejechocard/jen175. [DOI] [PubMed] [Google Scholar]
- 18.Pellikka PA, Nagueh SF, Elhendy AA, Kuehl CA, Sawada SG. American Society of Echocardiography recommendations for performance, interpretation, and application of stress echocardiography. J Am Soc Echocardiogr. 2007;20:1021–41. doi: 10.1016/j.echo.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Minozzo EL, De Luca G, Wottrich SH, Kunert HZ, Vigueras ES, Diemer F. Prevalence of Type D personality in patients undergoing coronary stent implantation. Arq Bras Cardiol. 2007;89:19. [Google Scholar]
- 20.Schmidt MM, Quadros AS, Abelin AP, Minozzo EL, Wottrich SH, Kunert HZ, et al. Psychological characteristics of patients undergoing percutaneous coronary interventions. Arq Bras Cardiol. 2011;97:331–7. doi: 10.1590/s0066-782x2011005000104. [DOI] [PubMed] [Google Scholar]
- 21.Grande G, Romppel M, Barth J. Association between type D personality and prognosis in patients with cardiovascular diseases: A systematic review and meta-analysis. Ann Behav Med. 2012;43:299–310. doi: 10.1007/s12160-011-9339-0. [DOI] [PubMed] [Google Scholar]
- 22.Kupper N, Pedersen SS, Höfer S, Saner H, Oldridge N, Denollet J. Cross-cultural analysis of type D (distressed) personality in 6222 patients with ischemic heart disease: A study from the International HeartQoL Project. Int J Cardiol. 2013;166:327–33. doi: 10.1016/j.ijcard.2011.10.084. [DOI] [PubMed] [Google Scholar]
- 23.Kuijpers PM, Denollet J, Wellens HJ, Crijns HM, Honig A. Noncardiac chest pain in the emergency department: The role of cardiac history, anxiety or depression and Type D personality. Eur J Cardiovasc Prev Rehabil. 2007;14:273–9. doi: 10.1097/HJR.0b013e32801da0fc. [DOI] [PubMed] [Google Scholar]
- 24.Borkoles E, Polman R, Ski CF, Thompson DR. Type D personality and cardiovascular outcomes. Ann Behav Med. 2012;44:139–40. doi: 10.1007/s12160-012-9373-6. [DOI] [PubMed] [Google Scholar]
- 25.Bacon SL, Moullec G. Type-D personality and heart disease: It might be ‘one small step’, but it is still moving forward: A comment on Grande et al. Ann Behav Med. 2012;43:280–1. doi: 10.1007/s12160-012-9357-6. [DOI] [PubMed] [Google Scholar]
- 26.de Voogd JN, Sanderman R, Coyne JC. A meta-analysis of spurious associations between type D personality and cardiovascular disease endpoints. Ann Behav Med. 2012;44:136–7. doi: 10.1007/s12160-012-9356-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schiffer AA, Smith OR, Pedersen SS, Widdershoven JW, Denollet J. Type D personality and cardiac mortality in patients with chronic heart failure. Int J Cardiol. 2010;142:230–5. doi: 10.1016/j.ijcard.2008.12.090. [DOI] [PubMed] [Google Scholar]
- 28.Denollet J, Holmes RV, Vrints CJ, Conraads VM. Unfavorable outcome of heart transplantation in recipients with type D personality. J Heart Lung Transplant. 2007;26:152–8. doi: 10.1016/j.healun.2006.11.600. [DOI] [PubMed] [Google Scholar]
- 29.Pedersen SS, Denollet J, Ong AT, Sonnenschein K, Erdman RA, Serruys PW, et al. Adverse clinical events in patients treated with sirolimus-eluting stents: The impact of Type D personality. Eur J Cardiovasc Prev Rehabil. 2007;14:135–40. doi: 10.1097/HJR.0b013e328045c282. [DOI] [PubMed] [Google Scholar]
- 30.Denollet J, Pedersen SS, Vrints CJ, Conraads VM. Usefulness of type D personality in predicting five-year cardiac events above and beyond concurrent symptoms of stress in patients with coronary heart disease. Am J Cardiol. 2006;97:970–3. doi: 10.1016/j.amjcard.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 31.Coyne JC, Jaarsma T, Luttik ML, van Sonderen E, van Veldhuisen DJ, Sanderman R. Lack of prognostic value of type D personality for mortality in a large sample of heart failure patients. Psychosom Med. 2011;73:557–62. doi: 10.1097/PSY.0b013e318227ac75. [DOI] [PubMed] [Google Scholar]


