Abstract
Objective:
The objective was to quantify the specialists' prescription pattern in Iran and to point out the prescribing behavioral differences among several specialties.
Methods:
A retrospective cross-sectional study was carried out on the claim data. National prescription data were obtained on the basis of the claims that the pharmacies submitted to the insurers during 1 year period of the study. More than 85 million prescriptions were analyzed using “Rx-Analyst” software that is designed and applied by National Committee of Rational Use of Medicines in Iran. Specified medical specialties were considered and the World Health Organization prescription indicators were used to evaluate the physicians' prescribing behavior.
Findings:
Average items per prescription were ranged from 3.68 in cardiologists' to 2.06 in dermatologists' prescriptions. The highest and the lowest mean price were belonged to neurologists' and ophthalmologists' prescriptions, respectively. In addition, 45% of patients received antibiotics, 41% of patients received injectable form of drugs, and 23% received corticosteroids. A high tendency toward prescribing corticosteroids and antibiotics as well as an injectable form of medicines was observed among general physicians.
Conclusion:
There is an inevitable need to improve prescription habits among different specialties, especially among general practitioners. This causes the policymakers to put more emphasis on priorities such as continuous education.
Keywords: Medical specialty, prescribing pattern, rational drug prescription, World Health Organization prescribing indicators
INTRODUCTION
Although drugs are not the only therapeutic interventions, which provide a desirable health level, rational use of them plays an important role in the efficacy and sufficiency of therapeutic interventions. Rational drug utilization means that each individual receives the right medicine, in an adequate dose for an adequate duration, with appropriate information and follow-up treatment, and at an affordable cost.[1]
Some examples of irrational prescription are over- and under-prescribing, polypharmacy, no indicated drug prescription, unreasonable use of expensive medicines and inappropriate use of antibiotics.[2,3,4,5,6] In addition to high cost of treatment, inappropriate prescribing causes ineffective, unsafe treatment, exacerbation or prolongation of illness, distress, and harm to the patient.[7]
Like other countries, inappropriate use of drugs due to irrational prescription practices is a common problem in Iran, and requires being concisely controlled.[8,9]
Due to the high cost of inappropriate use of drugs, developing countries face more problems because of the limited economic resources and lack of organized drug policy.[10]
In order to improve the prescription quality and rational prescription pattern promotion there is an inevitable need to investigate the factors that affect doctors' prescription patterns.[11] Studies have shown that there is a correlation between prescription patterns and gender, age, educational status, work experience, economic situation, and physician's specialty.[11] Defining drug prescription and consumption pattern provides advantageous feedback to prescribers in order to improve their prescribing behavior. Prescription analyzing studies help the policymakers to set the priorities to promote the rational use of medicines nationwide.[7]
This study aims to quantify the current situation of drug use pattern in correlation with prescribing behavior of physicians based on their different specialties.
METHODS
A retrospective cross-sectional study was carried out on prescription data collected during the year 2011. Physicians' prescription data were obtained from the insurance organizations, based on the claims that the pharmacies submitted electronically to the insurers. Information were obtained including prescribing date, physician specialty, and the prescribed items related information such as dosage forms and the number of medicines per prescription. The prescription data were included in specifically designed data management computer software called “Rx Analyst”. Rx Analyzer (Noskheh-Pardaz; designed and applied by National Committee of Rational Use of Medicines in Iran) is professional software, which is designated to accumulate and analyze the prescription data considering the defined World Health Organization (WHO) indicators. Using the mentioned software, the population cumulative data and its related analysis are available. The following indicators were considered for evaluation of the prescription patterns for physicians: (a) Average medicine items per prescription (it has to be stated that each medicine assumed as an individual item, for example, although two items in one prescription may belong to the same therapeutic class, they are counted as two different individual items); (b) average price per prescription; (c) proportion of prescriptions that includes at least one injectable medicine; (d) proportion of prescriptions that included at least one antibiotic medicine item; and (e) proportion of prescriptions that included at least one corticosteroid medicine item. The following medical specialists were considered as the sample population: General practitioners (GPs), pediatricians, cardiologists, internists, gynecologists, ophthalmologists, orthopedists, ear-nose-throat (ENT) specialists, general surgeons, neurologists, psychiatrists, infectious diseases specialists and urologists. Other specialties were excluded from the survey due to their little amount of prescriptions in comparison to the mentioned ones.
Inaccessibility to patients' age and sex and also disease diagnosis were introduced as the software limitations. Therefore, the study was designed based on the data that could be accessible using the software, including number and type of prescribed medicines and prescribers' medical specialty.
In this study, the indicators are reported as means and proportions; since the entire population data is collected, and the population is so large in size, there is no standard deviation calculated by the software because these parameters can be negligible in this huge data.[12]
RESULTS
More than 85 million prescriptions were analyzed through this survey. The collected prescriptions were mostly belonged to general physicians (57.51%), pediatricians (4.97%), gynecologists (4.60%) and internists (4.23%). Other specialists' prescription proportion were almost close together (orthopedists' 1.90%, dentists' 1.75%, ophthalmologists' 1.74%, ENT specialists' 1.53%, neurologists' 1.49%, cardiologists' 1.38%, psychiatrists' 1.35%, and general surgeons' 1.33%). Dermatologists (0.93%), urologists (0.90%), infectious disease specialists (0.88%) and neurosurgeons (0.77%) prescription proportion were <1%.
The mean items per prescription were 3.07 considering the total amount of prescriptions. Furthermore, assuming each prescription as an individual patient, 45% of patients received antibiotics, 41% of patients received injectable form of drugs, and 23% received corticosteroids. Among all items prescribed by physicians, dexamethasone ampoule was the most frequently prescribed medication. According to Table 1 which demonstrates top five medicines prescribed by different medical specialties, dexamethasone was accounted for 15.27% of GPs' prescriptions as their most frequently prescribed medicine [Table 1]. Dexamethasone was also observed in top five prescribed medicines of several medical specialties, but the rate was much lower than that of general physicians. About 3.31% of specialists' prescription contained dexamethasone.
Table 1.
Top five medicines prescribed by different medical specialties in Iran in 2011
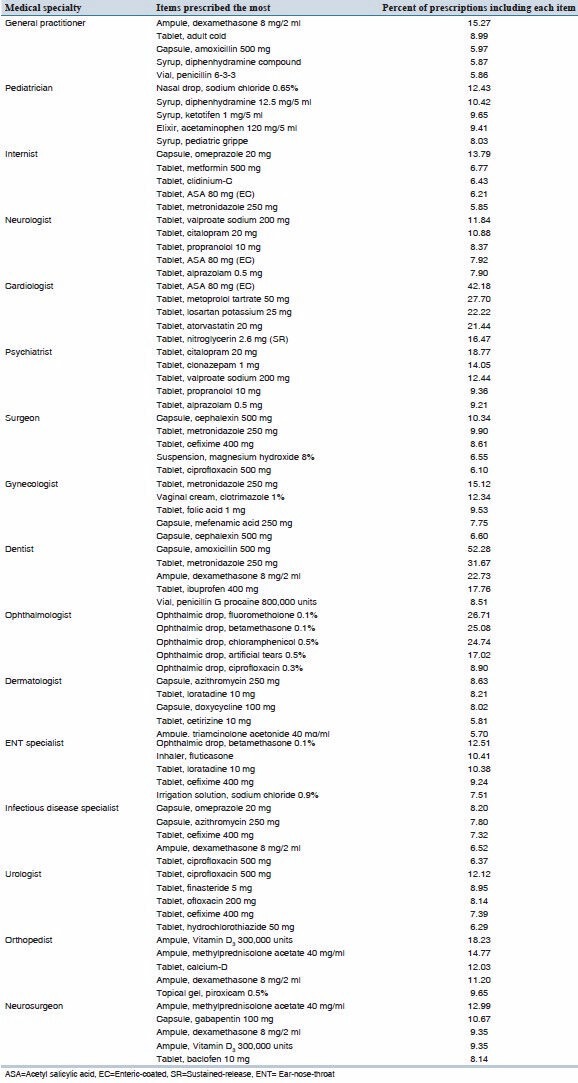
The most prevalent prescribed antibiotic was amoxicillin 500 mg capsules (2.13% of specialists' prescriptions and 5.97% of GPs' prescriptions).
The variation between the averages items prescribed per prescription is shown in Table 1. Average items per prescription were ranged from 3.68 in cardiologists' to 2.06 in dermatologists' prescriptions. Table 2 shows, the prescription pattern and the variation among different physicians according to WHO indicators.
Table 2.
Number of prescriptions, mean items and mean price per prescriptions regarding different medical specialties in Iran in 2011
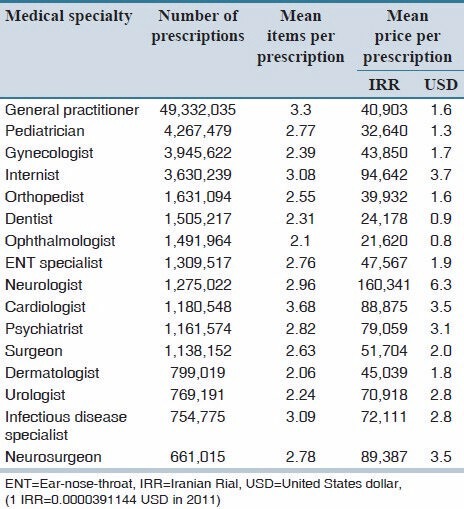
A wide variation among the mean price per prescription is observed depending on physicians' specialties [Table 2]. The highest and the lowest mean price were belonged to neurologists' and ophthalmologists' prescriptions, respectively, with the value of 160,341 and 21,620 Iranian Rials (6.27 and 0.85 United States Dollars, respectively); one Iranian Rial equals to 0.0000391144 United States Dollars in 2011.
Antibiotics were mostly included in prescriptions prescribed by dentists 89%, ENT specialists 52%, general physicians 51%, infectious disease specialists 49%, gynecologists 48%, urologists 47%, general surgeons 46%, pediatricians 44%, and dermatologists 41%. In other words, more than 50% of the patients referred to dentists, ENT specialists and GPs received at least one antibiotic, while for the patients who referred to neurologists, psychiatrists, cardiologists, and ophthalmologists, this rate was <10% [Figure 1].
Figure 1.
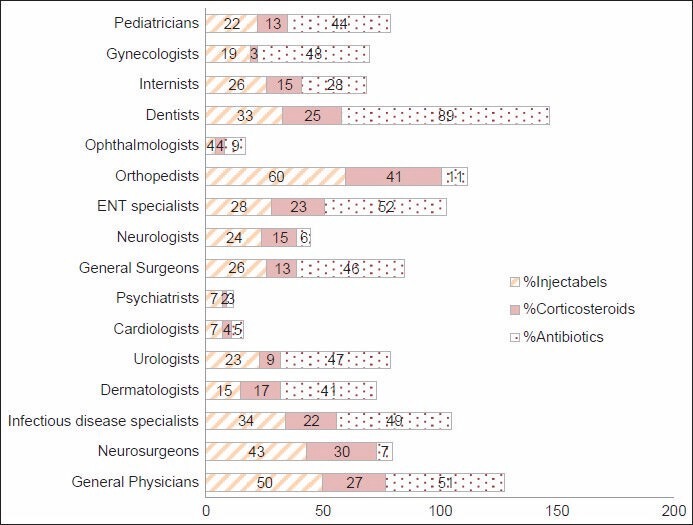
Percentage of prescriptions containing main indicator medications regarding different medical specialties in Iran in 2011
More than 50% of GPs' and orthopedists' patients received at least one injection form of drug, while <10% of psychiatrists', cardiologists' and ophthalmologists' prescriptions contained an injection form of drug [Figure 1].
A rate of <10% of corticosteroid prescription was observed among urologists, cardiologists, ophthalmologists, gynecologists, and psychiatrists, while orthopedists were the highest corticosteroid prescribers (41%), followed by neurosurgeons (30%) and GPs (27%) [Figure 1].
DISCUSSION
According to our findings, there is a significant difference between prescribing behavior of physicians depending on their specialties. This finding was also revealed in other studies.[4,13]
Considering the defined indicators, which are set by WHO in order to assess the quality of prescription, the results showed that except for the mean price per encounter, GPs were among the top three physicians' group who prescribed the most antibiotics, corticosteroids and injection form of drugs. Frequent prescription of above-mentioned categories may suggest an increasing risk of inappropriate use of medicines.[14,15,16]
Although there are no defined standards regarding prescription quality indicators available worldwide, there is undoubtedly a correlation between the number of items per prescription and increasing risk of polypharmacy.[2,11] In this study, the average items per prescription was 3.07, which is higher than those of Inner Mongolia (2.7), Beijing (2.63), Guangdong (2.36), and Guangxi (1.95) provinces of China. The average item per prescription was even higher than those of Zimbabwe (1.3), Sudan (1.4), and Palestine (1.3) as developing countries.[11,17] According to other studies, this indicator ranges from 1.4 to 4.8 in developing countries and 1.3-2.2 in developed countries.[2] The contrast would be observed even more significantly when comparing the average item per prescription for ophthalmologists (2.06) as the lowest one in Iran with the recommended value of WHO (1.3-2.0).[11] Since each item considered as an individual-even if the therapeutic classes were the same - the difference between the results may base on the different calculation method used in this study.
There is some explanation for different specialties, which prescribe numerous items per prescription. For example, it is assumed that cardiologists, who are accounted for the highest item prescribing per prescription, prescribed more items because normally their patients are seriously sick, and they are more complicated due to their underlying diseases.[2,17]
On the other hand, general physicians are the first healthcare professionals to whom patients refer and as a result they face numerous patients and a huge variety of illnesses as well.[2] But still, the high number of medicine per GPs' prescription suggests that further effort is needed in order to evaluate and improve the general physicians' prescribing habits.
In this study, the ratio of antibiotic used per prescription was 45%, which is higher than what is recommended by WHO (no higher than 30%). It was lower than Nigeria (72.8%), Zimbabwe (58%) and close to Laos (47%), and Sri Lanka (47%), but higher than in Yemen (24.6%) and Saudi Arabia (20%).[11,18]
The percentage of dentists' prescription, including at least one antibiotic was significantly higher than other specialists and general physicians, but it has to be stated as an explanation that they are permitted to prescribe a limited list of medicines, which are mostly analgesics and antibiotics.
It was expected for specialists, especially for infectious diseases specialists to prescribe more antibiotics comparing to other physicians, but as it was reported by the results, general physicians were tended to prescribe more antibiotics than infectious diseases specialists. This might be an evidence of excessive prescription of antibiotics by general physicians, which may cause irrational use of antibiotics and may result in antibiotic resistance as a threat to human health globally.[15] This suggests that still further management and regulatory by health policymakers are needed to prevent the excessive use of antibiotics.
The results showed that 41% of patients received injection form of drugs; this is much higher than what WHO recommends (1%),[11] but close to Hogerzeil's findings in Uganda, Sudan and Nigeria (36-48%).[18]
The results of the current study showed that GPs prescribe more injection form of drugs comparing to other physicians. Considering the fact that unnecessary injections result in wasting medical cost, medical staff, time, and medical equipment, there is a concise monitoring system needed to reduce these economic consequences. Irrational use of injection form of drugs increases the risk of infection by viruses, like hepatitis C and AIDS; therefore, improving the prescribing habits, especially among GPs may help improving the public health levels and healthcare facilities in long-term.[11,16]
Regarding the results, GPs also prescribed a high amount of corticosteroids. Although orthopedists and neurosurgeons tend to prescribe more corticosteroid than GPs, GPs' corticosteroid prescription seems more irrational due to the large amount of dexamethasone recorded in their prescriptions (15.27%).
Based on what the results revealed in this study, there is an inevitable need to improve prescription habits among different specialties, especially GPs. This causes the policymakers to put more emphasis on priorities such as continuous education[19,20] and supporting the researches concerning the current situation assessment and prescription analysis.
AUTHORS' CONTRIBUTION
A. Karimi, M. Haerizadeh and F. Soleymani designed the study with contributions from M. Haerizadeh, and F. Taheri. M. Haerizadeh collected data and prepare the first draft. F. Soleymani and M. Haerizadeh analyzed the data. F. Soleymani and F. Taheri wrote the manuscript. All the authors approved the final manuscript. F. Soleymani is the guarantor.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization. Expert Committee. Geneva: World Health Organization; 1977. Report of a WHO 1977. The Selection of Essential Drugs; pp. 7–35. WHO Technical Report Series, No. 615. [Google Scholar]
- 2.Sadeghian GH, Safaeian L, Mahdanian AR, Salami S, Kebriaee-Zadeh J. Prescribing quality in medical specialists in Isfahan, Iran. Iran J Pharm Res. 2013;12:235–41. [PMC free article] [PubMed] [Google Scholar]
- 3.Aronson JK. Medication errors: What they are, how they happen, and how to avoid them. QJM. 2009;102:513–21. doi: 10.1093/qjmed/hcp052. [DOI] [PubMed] [Google Scholar]
- 4.Garjani A, Salimnejad M, Maleki N. The effect of interactive group discussion among physicians to promote rational use of drugs. J Med Educ. 2006;8:73–81. [PubMed] [Google Scholar]
- 5.Ahmadizar F, Soleymani F, Abdollahi M. Study of drug-drug interactions in prescriptions of general practitioners and specialists in Iran 2007-2009. Iran J Pharm Res. 2011;10:921–31. [PMC free article] [PubMed] [Google Scholar]
- 6.Soleymani F, Abdollahi M. Management information system in promoting rational drug use. Int J Pharmacol. 2012;8(Suppl 6):586–9. [Google Scholar]
- 7.Pavani V, Mihir YP, Shravani K, Prabhakar RV. Study of prescribing pattern for evaluation of rational drug therapy in Warangal. Indian J Pharm Pract. 2011;4(Suppl 4):77–9. [Google Scholar]
- 8.Cheraghali AM, Nikfar S, Behmanesh Y, Rahimi V, Habibipour F, Tirdad R, et al. Evaluation of availability, accessibility and prescribing pattern of medicines in the Islamic Republic of Iran. East Mediterr Health J. 2004;10:406–15. [PubMed] [Google Scholar]
- 9.Gholamreza-Sepehri, Meimandi MS. The quality of prescribing in general practice in Kerman, Iran. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2005;18:353–60. doi: 10.1108/09526860510612207. [DOI] [PubMed] [Google Scholar]
- 10.Kshirsagar MJ, Langade D, Patil S, Patki PS. Prescribing patterns among medical practitioners in Pune, India. Bull World Health Organ. 1998;76:271–5. [PMC free article] [PubMed] [Google Scholar]
- 11.Wang H, Li N, Zhu H, Xu S, Lu H, Feng Z. Prescription pattern and its influencing factors in Chinese county hospitals: A retrospective cross-sectional study. PLoS One. 2013;8:e63225. doi: 10.1371/journal.pone.0063225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glenberg A, Andrzejewski M. Learning from Data: An Introduction to Statistical Reasoning. 3rd ed. Routlege Publishers; 2012. ISBN 1136676627, 0781136676628. [Google Scholar]
- 13.Yousefi N, Majdzadeh R, Valadkhani M, Nedjat S, Mohammadi H. Reasons for physicians' tendency to irrational prescription of corticosteroids. Iran Red Crescent Med J. 2012;14:713–8. doi: 10.5812/ircmj.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holloway K. Who contributes to misuse of antimicrobials? Essent Drugs Monit No 9. 2000:9. [Google Scholar]
- 15.Hutin YJ, Hauri AM, Armstrong GL. Use of injections in healthcare settings worldwide, 2000: Literature review and regional estimates. BMJ. 2003;327:1075. doi: 10.1136/bmj.327.7423.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kravitz RL, Greenfield S, Rogers W, Manning WG, Jr, Zubkoff M, Nelson EC, et al. Differences in the mix of patients among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992;267:1617–23. [PubMed] [Google Scholar]
- 17.Hogerzeil HV, Bimo, Ross-Degnan D, Laing RO, Ofori-Adjei D, Santoso B, et al. Field tests for rational drug use in twelve developing countries. Lancet. 1993;342:1408–10. doi: 10.1016/0140-6736(93)92760-q. [DOI] [PubMed] [Google Scholar]
- 18.Vallano A, Montané E, Arnau JM, Vidal X, Pallarés C, Coll M, et al. Medical speciality and pattern of medicines prescription. Eur J Clin Pharmacol. 2004;60:725–30. doi: 10.1007/s00228-004-0802-8. [DOI] [PubMed] [Google Scholar]
- 19.Soleymani F, Valadkhani M, Dinarvand R. Challenges and achievement of promoting rational use of drug in Iran. Iran J Public Health. 2009;38:166–8. [Google Scholar]
- 20.Laing R, Hogerzeil H, Ross-Degnan D. Ten recommendations to improve use of medicines in developing countries. Health Policy Plan. 2001;16:13–20. doi: 10.1093/heapol/16.1.13. [DOI] [PubMed] [Google Scholar]


