Abstract
Background
Elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP) is associated with clinically overt heart failure (HF). However, whether it provides additive prognostic information for incident HF beyond traditional risk factors and left ventricular (LV) mass index among multi-ethnic asymptomatic individuals has not yet been determined. We studied the associations of plasma NT-proBNP and magnetic resonance imaging defined LV mass index with incident HF in an asymptomatic multi-ethnic population.
Methods and Results
A total of 5597 multi-ethnic participants without clinically apparent cardiovascular disease underwent baseline measurement of NT-proBNP and were followed for 5.5±1.1 years. Among them, 4163 also underwent baseline cardiac magnetic resonance imaging. During follow-up, 111 participants experienced incident HF. Higher NT-proBNP was significantly associated with incident HF, independent of baseline age, sex, ethnicity, systolic blood pressure, diabetes mellitus, smoking, estimated glomerular filtration rate, medications (anti-hypertensive and statin), LV mass index, and interim myocardial infarction (hazard ratio: 1.95 per 1U log NT-proBNP increment, 95% CI 1.54–2.46, P<0.001). This relationship held among different ethnic groups, non-Hispanic whites, African-Americans, and Hispanics. Most importantly, NT-proBNP provided additive prognostic value beyond both traditional risk factors and LV mass index for predicting incident HF (integrated discrimination index=0.046, P<0.001; net reclassification index; 6-year risk probability categorized by <3%, 3–10%, >10% =0.175, P=0.019; category-less net reclassification index=0.561, P<0.001).
Conclusions
Plasma NT-proBNP provides incremental prognostic information beyond traditional risk factors and the magnetic resonance imaging-determined LV mass index for incident symptomatic HF in an asymptomatic multi-ethnic population.
Clinical Trial Registration
URL: http://www.clinicaltrials.gov. Unique identifier: NCT00005487.
Keywords: N-terminal pro-B-type natriuretic peptide, heart failure, left ventricular mass
Neurohormonal activation and left ventricular (LV) remodeling are important contributors to progressive cardiac dysfunction and heart failure (HF).1 N-terminal pro-B-type natriuretic peptide (NT-proBNP), as an index of neurohormonal activation, has been shown to be associated with mortality and rehospitalization in patients with clinically overt HF.2 Moreover, recent studies have shown that the level of plasma NT-proBNP is associated with risk of future HF in population-based studies.3,4 However, previous studies have not addressed 2 important questions: (1) whether the predictive value of NT-proBNP is additive beyond traditional HF risk factors and LV hypertrophy; and (2) whether NT-proBNP levels predict HF across different ethnic groups of asymptomatic individuals. Plasma natriuretic peptide level has been shown to be affected by several factors, including age, sex, and body habitus. Moreover, there is controversy concerning ethnic difference in HF severity and NT-proBNP levels.5 As previous population-based studies were mainly conducted in whites, the applicability of their study results to multi-ethnic populations remains to be investigated.3 In addition, a recent study showed that the predictive value of NT-proBNP for incident HF was poor in healthy populations with structurally normal hearts,6 suggesting that NT-proBNP may function as a risk factor by virtue of detecting advanced LV remodeling.
LV hypertrophy, which reflects LV remodeling, has also been shown to be a strong predictor of incident HF in asymptomatic populations.7,8 However, it is unclear whether there is an additive prognostic role for NT-proBNP beyond direct measurements of LV mass in predicting incident HF in multiethnic populations without previous history of cardiovascular disease. Therefore, a systematic approach to answer this question using LV mass measured by cardiac magnetic resonance imaging (MRI), currently the most accurate method, is needed. Improved understanding of the interplay between NT-proBNP and LV mass for prognostic purposes could also provide unique pathophysiologic insight into how these factors relate to the development of symptomatic HF.
Therefore, in this study, we sought to evaluate the predictive ability of NT-proBNP in comparison with cardiac MRI-determined LV mass for incident symptomatic HF, in a large multi-ethnic population comprising non-Hispanic whites, Chinese, Hispanics, and African-Americans.
Methods
Study Population
The Multi-Ethnic Study of Atherosclerosis (MESA) is a prospective study designed to evaluate mechanisms underlying the development and progression of subclinical cardiovascular diseases among asymptomatic individuals in the general population. Details of the MESA study design have been previously described.9 In short, 6814 American men and women, 45 to 84 years of age and of 4 self- reported ethnicities (non-Hispanic white, African-American, Hispanic, and Chinese) who were free of known cardiovascular disease and free of any history of HF were enrolled in 6 participating centers in the United States. Upon entry, all participants underwent extensive evaluations, including questionnaires, physical examination, and laboratory tests, subjects diagnosed with cardiovascular disease or symptomatic HF were then excluded. Among the 6814, 5597 underwent plasma NT-proBNP measurements, and the clinical characteristics of this subpopulation were very similar to the entire MESA cohort. Among them, 4163 also underwent cardiac MRI. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or treatment for hypertension. Individuals with diabetes were defined as either having fasting plasma glucose ≥126 mg/dL or receiving treatment for diabetes mellitus. Estimated glomerular filtration rate was calculated using the Modification of Diet in Renal Disease equation.10
Plasma NT-proBNP Measurements
The plasma concentration of NT-proBNP was measured using a highly sensitive and specific Elecsys electrochemiluminescence immunoassay based on the double-antibody sandwich method (Roche Diagnostics Corporation, Indianapolis, IN). A 250 μl serum sample previously unthawed or only thawed once was used for analysis. All analyses were performed at the core-lab ((University of California, San Diego)) and the intra-and interassay coefficients of variation were as follows: at 175 pg/mL, 2.7% and 3.2%; at 355 pg/mL, 2.4% and 2.9%; at 1068 pg/mL, 1.9% and 2.6%; and at 4962 pg/mL, 1.8% and 2.3%, respectively.11
Global Left Ventricular Structure and Function
Baseline MRI of the heart was acquired using 1.5T magnetic resonance scanners. Short-axis cine images were obtained with retrospective gating with a temporal resolution of ≤50 msec, from above the mitral valve plane to the LV apex using fast gradient echo sequence. LV structural parameters and LV ejection fraction were measured using standard commercially available software (MASS 4.2, MEDIS, Leiden, The Netherlands), as previously described.7 In brief, the endocardial and epicardial myocardial borders were contoured using a semiautomated method. The difference between the epicardial and endocardial areas for all slices was multiplied by slice thickness and section gap and then multiplied by the specific myocardial density (1.04 g/mL) to determine LV mass. The LV mass index was defined as LV mass divided by body surface area.
Clinical Follow-Up
A telephone interviewer contacted each participant (or representative) every 6 to 9 months to inquire about interim hospital admissions, cardiovascular outpatient diagnoses, and deaths. During follow-up, 5 participants were lost. Medical records were successfully obtained for 96% of the hospitalized cardiovascular events and 95% of the outpatient cardiovascular diagnostic encounters. Two physicians reviewed all records for independent end point classification and assignment of event dates. Reviewers classified HF as definite, probable, or absent. Definite or probable HF required HF symptoms, such as shortness of breath or edema. In addition to symptoms, classification of probable HF required diagnosis of HF by a physician and a receipt for medical treatment for HF. Classification of definite HF required the fulfillment of one or more additional criteria, such as evidence of pulmonary edema/congestion by chest X-ray; dilated ventricle or poor LV systolic function (LV ejection fraction <40%) by imaging methods; or evidence of LV diastolic dysfunction by echocardiography.7 Myocardial infarction was diagnosed on the basis of a combination of symptoms, electrocardiogram, and cardiac biomarker levels. Interim myocardial infarction was defined as “newly diagnosed acute myocardial infarction during the follow period.” A more detailed description of the MESA longitudinal follow-up methods is available at http://www.mesa-nhlbi.org.
Statistical Analysis
Summary Analysis and Group Comparisons
Continuous variables were presented as mean±SD or median (interquartile range) for variables with skewed distribution and categorical variables were presented as percentages. Differences in clinical characteristics, risk factors, MRI parameters, and incidence of HF by NT-proBNP quartiles were tested with analysis of variance (continuous variables) or χ2 tests (categorical variables). Baseline characteristics were stratified by sex. The Kruskal-Wallis test was used for variables with a skewed distribution. Trends across quartiles were tested by 1-way analysis of variance using polynomials equations for continuous variable and by Spearman correlation between incidence number and quartile order from χ2 statistic in cross tab analysis. Because NT-proBNP distributions were skewed, their log-transformed values were used for linear regression analysis.
Survival Analysis With Continuous Log NT-proBNP
Cox Proportional Hazard regression analysis was performed for the probability distribution of time to HF with log NT-proBNP. The hazard ratio (HR) per 1 unit baseline log NT-proBNP was presented. The association between log NT-proBNP and time to HF was analyzed using a series of models with different covariate adjustments: Model 1 included age, sex, and ethnicity; Model 2 included the covariates of Model 1, plus diabetes, systolic blood pressure, current smoking, low-density lipoprotein-cholesterol, high-density lipoprotein-cholesterol, glomerular filtration rate, and current medications (anti-hypertensive therapy and statins); Model 3 included the covariates of Model 2 plus LV mass index; and in Model 4, we added interim myocardial infarction to the co-variates of Model 3. To explore the potential interactions of NT-proBNP with sex and ethnicity on the incidence of HF, we evaluated the relationship between log NT-proBNP and time to HF separately in each sex/ethnic group. In secondary analyses, we incorporated interaction terms individually in multivariate analysis (log NT-proBNP × covariate) to test for the presence of effect modification by age, sex, and LV mass index.
Survival Analysis With Categorical NT-proBNP and LV Mass Index
Categorical variables were generated by dichotomizing NT-proBNP and LV mass index at the 75th percentile. The Cox Proportional Hazard models for NT-proBNP quartiles and LV mass index were investigated. The HR for the fourth NT-proBNP quartile was compared with a group comprising the 3 lower quartiles in the successive models described earlier. Then, the group of participants who underwent both NT-proBNP and cardiac MRI measurements were cross-classified into 4 subgroups comprising those with NT-proBNP in the fourth quartile (>112.5 pg/mL) or lower, and those with LV mass index above or below the 75th percentile (86.78 g/m2). The HR of each subgroup for incident HF was compared after adjustment for the covariates of Model 2.
Discrimination and Calibration Analysis
We tested and compared the discrimination ability of NT-proBNP for HF beyond traditional risk factors and the LV mass index via differences in the area under the curve (AUC) derived from receiver operating characteristic curve analysis. AUCs were computed based on the predicted risk from Cox hazards modeling and compared using a parametric method.12 We also evaluated the added predictive ability of NT-proBNP as a new marker for the distributions of time to HF with and without LV mass index using the newly developed Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI) calculations.13–16 As NRI and IDI are defined by comparing the predicted probability of HF at a given time point and the median follow-up time of MESA participants was ≈5.5 years, we calculated the AUCs and the predicted probabilities of having HF within 6 years using Cox Proportional Hazard models with and without log NT-proBNP for each MESA participant who had the observed covariates. Details of the calculations were described in a supplemental appendix. Numerical computations of the parameter estimates and test statistics were carried out using Splus 8 (TIBCO, Palo Alto, CA) software. For the calibration of predictive models, deciles of risk were calculated for each model, after which the Hosmer-Lemeshow χ2 test was conducted for each model. All statistical analyses were performed using SPSS (version 15.0, Chicago, IL), STATA (version 9.0, College Station, TX), and Splus 8 (TIBCO, Palo Alto, CA) software and 2-sided P-values <0.05 were considered to be significant.
Results
Baseline MESA Cohort Characteristics
Unadjusted baseline characteristics according to NT-proBNP quartiles are shown in Table 1. Mean age was 62±10 years, and the median (interquartile range) NT-proBNP was 55 (24.0–112.5) pg/mL. NT-proBNP levels in women were higher than in men (72.0 [37.5–138.8] versus 38.5[15.7–81.4] pg/mL, P<0.001) and the log NT-proBNP correlated significantly with age (r=0.465, P<0.001). Non-Hispanic whites had higher log NT-proBNP compared with the other ethnic groups, even after adjustment for age, sex, glomerular filtration rate, LV ejection fraction, and LV mass index (B= 0.378 higher in Non-Hispanic white, 95% CI, 0.15–1.04, P<0.001). Chinese and African-Americans had lower NT-proBNP than Hispanics. After adjustment for age, sex, and ethnicity log NT-proBNP was inversely correlated with LV ejection fraction (B= −0.42, 95% CI −0.63 to −0.21, P<0.001), and positively correlated with the LV mass index (B=3.09, 95% CI 2.66–3.52, P<0.001). Log NT-proBNP remained inversely associated with glomerular filtration rate (B= −0.005, −0.006 to −0.003, P<0.001) after adjustment for age, sex, and ethnicity.
Table 1. Baseline Characteristics of NT-proBNP Quartiles According to Sex in the MESA Population (n=5597).
| Women (n=2882) | Men (n=2715) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| 1st Q(n=720) | 2nd Q(n=721) | 3rd Q(n=721) | 4th Q(n=720) | P for trend | 1st Q(n=680) | 2nd Q(n=678) | 3rd Q(n=679) | 4th Q(n=678) | P for trend | |
| NT-proBNP*, pg/mL | 21.4 | 53.1 | 99.3 | 214.9 | <0.001 | 6.7 | 25.8 | 55.2 | 146.9 | <0.001 |
| Age, y | 57.0±8.4 | 59.9±9.6 | 63.4±10.0 | 69.1±9.3 | <0.001 | 55.1±8.0 | 60.1±9.2 | 64.4±9.1 | 69.4±8.8 | <0.001 |
| Ethnicity, n (%)† | ||||||||||
| Non-Hispanic white | 174 (16) | 268 (24) | 316 (28) | 364 (32) | <0.001 | 187 (17) | 273 (25) | 304 (28) | 331 (30) | <0.001 |
| Chinese | 107 (29) | 106 (28) | 100 (27) | 62 (17) | <0.001 | 125 (34) | 93 (25) | 85 (23) | 64 (17) | <0.001 |
| African-American | 262 (36) | 175 (24) | 144 (20) | 144 (20) | <0.001 | 205 (33) | 145 (23) | 146 (23) | 132 (21) | <0.001 |
| Hispanic | 177 (27) | 172 (26) | 161 (24) | 150 (23) | 0.068 | 163 (26) | 167 (27) | 144 (23) | 151 (24) | 0.238 |
| Risk factors | ||||||||||
| Current smoking, n (%) | 112 (16) | 81 (11) | 68 (10) | 55 (8) | <0.001 | 114 (17) | 100 (15) | 78 (12) | 92 (14) | 0.029 |
| Hypertension, n (%) | 436 (31) | 511 (37) | 627 (45) | 889 (64) | <0.001 | 176 (26) | 228 (34) | 311 (46) | 422 (62) | <0.001 |
| Diabetes mellitus, n (%) | 112 (16) | 62 (9) | 77 (11) | 80 (11) | 0.034 | 86 (13) | 95 (14) | 82 (12) | 103 (15) | 0.336 |
| Body mass index, kg/m2 | 29.9±6.4 | 28.8±6.3 | 28.1±6.0 | 27.8±6.0 | <0.001 | 28.3±4.3 | 28.0±4.2 | 27.6±4.4 | 27.4±4.6 | <0.001 |
| GFR, ml/min | 85.6±17.6 | 81.5±16.3 | 78.2±16.3 | 73.0±17.6 | <0.001 | 86.3±16.5 | 82.9±20.5 | 79.9±16.7 | 74.8±18.8 | <0.001 |
| Hemodynamic parameters | ||||||||||
| SBP, mm Hg | 120±19 | 124±21 | 126±23 | 138±26 | <0.001 | 119±14 | 122±17 | 128±19 | 134±22 | <0.001 |
| DBP, mm Hg | 70±10 | 69±10 | 69±10 | 69±11 | 0.08 | 75±8 | 75±9 | 75±9 | 74±10 | 0.001 |
| Ventricular function or geometry | ||||||||||
| LV ejection fraction, % | 71±6 | 71±6 | 72±6 | 72±8 | 0.001 | 67±7 | 66±6 | 67±7 | 67±9 | 0.63 |
| LV mass index, g/m2 | 71±11 | 70±11 | 69±11 | 73±15 | 0.001 | 83±13 | 85±14 | 84±15 | 91±22 | <0.001 |
| LV mass/volume, g/mL | 1.11±0.20 | 1.08±0.20 | 1.09±0.20 | 1.13±0.23 | 0.05 | 1.21±0.23 | 1.23±0.27 | 1.22±0.25 | 1.27±0.29 | 0.002 |
| Current use of cardiovascular medication | ||||||||||
| ACE inhibitors, n (%) | 156 (11) | 150 (11) | 164 (12) | 240 (17) | 0.016 | 71 (10) | 89 (13) | 89 (13) | 129 (19) | <0.001 |
| ARB, n (%) | 37 (5) | 39 (5) | 41 (6) | 59 (8) | 0.018 | 10 (2) | 23 (3) | 41 (6) | 33 (5) | <0.001 |
| β-blockers, n (%) | 31 (4) | 38 (5) | 64 (9) | 152 (21) | <0.001 | 25 (4) | 22 (3) | 55 (8) | 130 (19) | <0.001 |
| Diuretics, n (%) | 105 (15) | 97 (14) | 96 (13) | 164 (23) | <0.001 | 37 (5) | 51 (8) | 69 (10) | 107 (16) | <0.001 |
| Statins, n (%) | 106 (15) | 91 (13) | 98 (14) | 132 (18) | 0.046 | 96 (14) | 81 (12) | 103 (15) | 120 (18) | 0.022 |
| Incident HF, n (n per 1000-y) | 3 (0.75) | 3 (0.75) | 10 (2.5) | 27 (7.0) | <0.001 | 1 (0.26) | 4 (1.1) | 9 (2.4) | 54 (15.7) | <0.001 |
MESA indicates Multi-Ethnic Study of Atherosclerosis; NT-proBNP, N-terminal–pro B type natriuretic peptide; GFR, glomerular filtration rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; LV, left ventricular; ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker; HF, heart failure.
Median value.
Percentage within each ethnicity; NT-proBNP (pg/mL) quartiles for women: first, 4.90–37.52; second, 37.53–72.02; third, 72.03–138.83; fourth, 138.84–3851.00. NT-proBNP (pg/mL) quartiles for men; first, 4.90–15.69; second, 15.70–38.48; third, 38.49–81.42; fourth, 81.43–11699.00.
Incident Heart Failure
The mean duration of follow-up was 5.5±1.1 years, during which 111 participants developed symptomatic HF (3.6 per 1000 person-years), of which men had a higher incidence than women (68 [4.6 per 1000 person-years] in men and 43 [2.7 per 1000 person-years] in women). Chinese had a lower HF event rate compared with participants of other ethnicities (6 [1.5 per 1000 person-years] Chinese, 25 [3.6 per 1000 person-years] Hispanics, 44 [3.6 per 1000 person-years] non-Hispanic whites, and 36 [5.0 per 1000 person-years] African-Americans).
Association of Incident HF with Plasma NT-proBNP
Participants in the fourth quartile of NT-proBNP had a higher incidence of HF compared with those in the lower quartiles (Figure 1). The HR of HF for those in the fourth NT-proBNP quartile was 10.52 (95% CI 6.78–16.33, P<0.001), compared with those in the 3 lower quartiles. Similarly, as a continuous variable, each unit log NT-proBNP augmentation was associated with a HR of 3.00 for HF (95% CI=2.59–3.42, P<0.001) in univariate analysis. This relationship persisted both in continuous and categorical analyses after adjustment for age, sex, and ethnicity (Model 1) and after further adjustment for systolic blood pressure, diabetes mellitus, current smoking, LDL-cholesterol, HDL-cholesterol, glomerular filtration rate, and current therapy with anti-hypertensives and/or statins (Model 2). Among MRI-derived variables, LV mass index was the best predictor for HF (LV mass index, AUC=0.745, P<0.001; LV ejection fraction, AUC=0.632, P<0.001) in univariate analysis. The relationship was modestly attenuated but remained significant when the LV mass index was added in Model 3. Moreover, NT-proBNP was further attenuated but remained significantly associated with a higher incidence of HF when interim myocardial infarction was added in Model 4 (Table 2). Finally, the association of NT-proBNP with incident HF did not vary by age, sex, or LV mass index based on incorporating interaction terms in the analysis (Appendix 1). To investigate the confounding effect of body mass index, we included body mass index and LV mass separately among Model 3 covariates instead of LV mass index, and their relationship remained significant (HR 2.29, 95% CI 1.85–2.85, P<0.001 with logNT-proBNP; 6.61, 3.64–12.01, P<0.001 with fourth quartile of NT-proBNP). In addition, when we added LV ejection fraction to the Model 3 covariates, NT-proBNP remained significant (2.16, 1.74–2.70, P<0.001; 6.01, 3.32–10.88, P<0.001, respectively).
Figure 1.
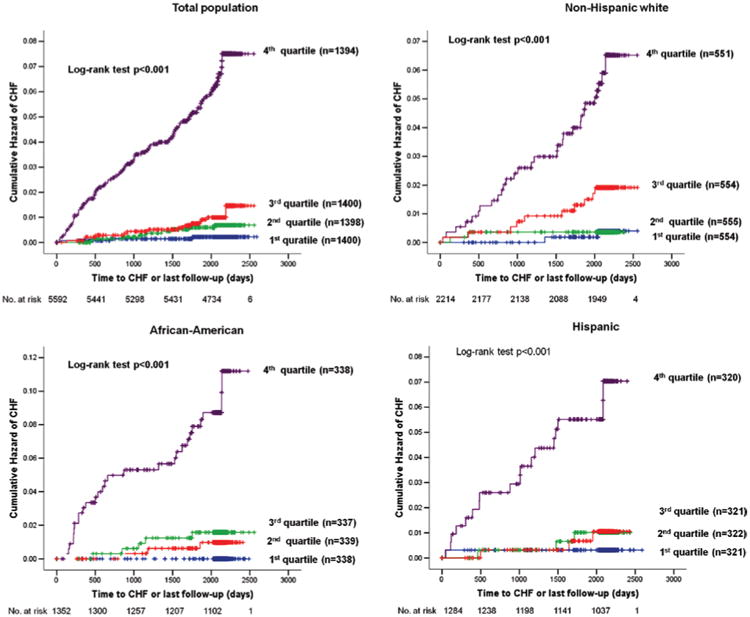
Kaplan-Meier curves of unadjusted cumulative hazard of incident heart failure according to quartiles of N-terminal–pro B type natriuretic peptide in the entire study population (A) and each ethnicity group (B, C, D). CHF indicates congestive heart failure.
Table 2. Hazard Ratio of Incident Heart Failure for Log NT-proBNP and NT-proBNP in the Fourth Quartile, Overall and by Ethnicity.
| All (n=5597) | Participants With Both NT-proBNP and Cardiac MRI (n=4163) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| HR per 1U Log NT-proBNP Increment (95% CI) |
HR per 1U Log NT-proBNP Increment (95% CI) |
HR for 4th Quartile NT-proBNP (>112.5 pg/mL) (95% CI) |
||||||||||
|
|
|
|
||||||||||
| All* (111/5597)† |
White (44/2217) |
AA (36/1353) |
Hispanic (25/1285) |
All* (76/4163) |
White (30/1640) |
AA (23/949) |
Hispanic (19/968) |
All* | White | AA | Hispanic | |
| Model 1 | 2.73 | 3.19 | 2.92 | 2.53 | 2.59 | 3.36 | 2.61 | 2.49 | 10.02 | 10.95 | 9.75 | 9.54 |
| (2.4–3.2) | (2.3–4.4) | (2.3–3.8) | (2.0–3.2) | (2.2–3.1) | (2.3–4.9) | (1.9–3.6) | (1.9–3.2) | (5.6–17.8) | (4.1–29.6) | (3.6–26.5) | (3.2–28.7) | |
| Model 2 | 2.73 | 2.83 | 3.10 | 2.73 | 2.71 | 2.95 | 2.92 | 2.92 | 9.14 | 9.83 | 10.51 | 7.04 |
| (2.3–3.2) | (2.0–4.1) | (2.3–4.2) | (2.0–3.8) | (2.2–3.3) | (1.9–4.6) | (2.0–4.2) | (2.0–4.3) | (5.1–16.3) | (3.5–27.4) | (3.9–28.7) | (2.3–21.9) | |
| Model 3 | 2.24 | 2.35 | 2.66 | 2.06 | 6.53 | 7.52 | 7.95 | 4.86 | ||||
| (1.8–2.8) | (1.5–3.7) | (1.85–4.0) | (1.3–3.2) | (3.6–11.9) | (2.6–21.8) | (2.8–22.7) | (1.5–15.8) | |||||
| Model 4 | 1.95 | 2.38 | 2.35 | 1.55 | 5.55 | 6.82 | 6.29 | 3.62 | ||||
| (1.5–2.5) | (1.4–3.9) | (1.5–3.6) | (1.0–2.4) | (3.0–10.3) | (2.3–20.1) | (2.1–18.7) | (1.1–11.8) | |||||
NT-proBNP indicates N-terminal–pro B type natriuretic peptide; HR, hazard ratio; AA, African-American.
Model 1 includes age, sex, and ethnicity as covariates.
Model 2 includes presence of diabetes mellitus, systolic blood pressure, current smoking, LDL-cholesterol, HDL-cholesterol, glomerular filtration rate, and current medications (anti-hypertensive medication and statin) in addition to the covariates of Model 1.
Model 3 includes left ventricular mass index in addition to the covariates of Model 2.
Model 4 includes interim myocardial infarction in addition to the covariates of Model 3.
All category includes the Chinese-Americans.
No. of HF/total participants number.
Association of Incident HF with Plasma NT-proBNP by Sex and Ethnicity
Despite the fact that mean log NT-proBNP differed among ethnic groups, higher log NT-proBNP was significantly related to incident HF within each ethnicity (Figure 1 and Table 2). However, among Chinese-Americans, the number of incident HF events was too small (6 cases among 742 participants) for reliable analysis. Likewise, NT-proBNP significantly predicted HF in participants of both sexes in adjusted models (data not shown).
Effects of NT-proBNP on Improvement in Model Performance
Comparison of C-statistics showed that NT-proBNP provided additive prognostic value beyond traditional risk factors in Model 2 (C-index: 0.88 with versus 0.81 without NT-proBNP, P<0.001) and in Model 3 (C-index: 0.89 with NT-proBNP versus 0.85 without NT-proBNP, P=0.01) for predicting HF (Figure 2). The IDI showed significantly better discrimination by the models that included NT-proBNP compared with Model 2 (IDI=0.088, SE=0.017, z=5.062, P<0.001) and Model 3 (IDI=0.046, SE=0.014, z=3.327, P<0.001). The NRIs after adding NT-proBNP to Model 2 was 0.370 (with <6%, 6–20% and >20% category; SE=0.069, z-value=5.381, P<0.001) and 0.304 (with <3%, 3–10% and >10% category; SE=0.069, z-value=4.415, P<0.001), respectively. NRIs after adding NT-proBNP to Model 3 were 0.131 (SE=0.063, z-value=2.097, P=0.036 with <6%, 6–20% and >20% category) and 0.175 (SE=0.074, z-value=2.347, P=0.019 with <3%, 3–10% and >10% category), respectively (Table 3). Category-less NRI was 0.561 (model 3+NT-proBNP; 50 cases move-up and 25 cases move-down, 2495 noncases move-down and 1570 noncases move-up; SE=0.117, z-value=4.813, P<0.001). The Hosmer-Lemeshow χ2 for the calibration was 7.112 (P=0.525) in Model 3 without NT-proBNP and 10.55 (P=0.228) in Model 3 with NT-proBNP.
Figure 2.
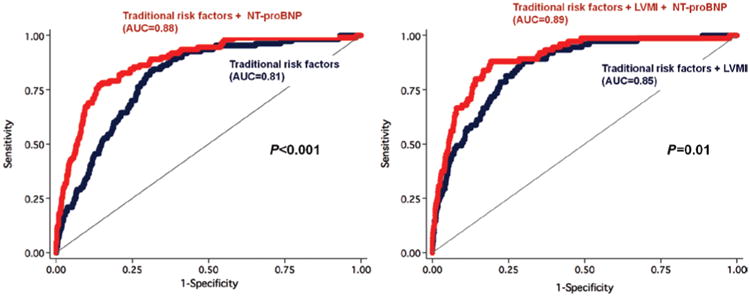
Additive prognostic value of NT-proBNP beyond traditional risk factors and LV mass index. A, NT-proBNP significantly improved receiver operating characteristic curve (ROC) area by 7% compared with traditional risk factors (covariates used in Model 2). B, NT-proBNP significantly improved ROC area by 4% compared with traditional risk factors combined with LVMI (Model 3). NT-proBNP indicates N-terminal–pro B type natriuretic peptide; LVMI, left ventricular mass index AUC, area under the curve.
Table 3. Reclassification of Heart Failure Risk With NT-proBNP.
| Model 3 Without NT-proBNP | Model 3 With NT-proBNP | |||
|---|---|---|---|---|
|
| ||||
| <6% Risk | 6–20% Risk | >20% Risk | Total no. | |
| Cases (n=75*) | ||||
| <6% risk | 29 (67.4%) | 14 (32.6%) | 0 | 43 |
| 6–20% risk | 4 (19.0%) | 15 (71.4%) | 2 (9.5%) | 21 |
| >20% risk | 0 | 2 (18.2%) | 9 (81.8%) | 11 |
| Total no. | 33 | 31 | 11 | 75 |
| Noncases (n=4065) | ||||
| <6% risk | 3740 (97.4%) | 97 (2.5%) | 2 (0.1%) | 3839 |
| 6–20% risk | 93 (47.2%) | 93 (47.2%) | 11 (5.6%) | 197 |
| >20% risk | 0 (0%) | 9 (31.0%) | 20 (69.0%) | 29 |
| Total no. | 3833 | 199 | 33 | 4065 |
| <3% Risk | 3–10% Risk | >10% Risk | Total no. | |
| Cases (n=75) | ||||
| <3% risk | 14 (51.9%) | 12 (44.4%) | 1 (3.7%) | 27 |
| 3–10% risk | 6 (20.7%) | 15 (51.7%) | 8 (27.6%) | 29 |
| >10% risk | 0 | 4 (21.1%) | 15 (78.9%) | 19 |
| Total no. | 20 | 31 | 24 | 75 |
| Noncases (n=4065) | ||||
| <3% risk | 3248 (95.4%) | 151 (4.4%) | 5 (0.1%) | 3404 |
| 3–10% risk | 263 (47.3%) | 254 (45.7%) | 39 (7.0%) | 556 |
| >10% risk | 7 (6.7%) | 39 (37.1%) | 59 (56.2%) | 105 |
| Total no. | 3518 | 444 | 103 | 4065 |
Model 3 included age, sex, ethnicity, systolic blood pressure, use of anti-hypertensive treatment, presence of diabetes mellitus, current smoking, LDL-cholesterol, HDL-cholesterol, statin use, glomerular filtration rate, and LV mass index. Sixteen cases moved upward and 6 cases downward; 110 controls upward and 102 controls downward with <6, 6–20, and >20% categories. The net classification improvement was estimated at 0.131 (P=0.036); 21 cases moved upward and 10 cases downward; 195 controls upward and 309 controls downward with <3%, 3–10%, >10% categories. The net classification improvement was estimated at 0.175 (P=0.019). NT-proBNP indicates N-terminal–pro B type natriuretic peptide.
Among 4163 participants who underwent both NT-proBNP and MRI, 76 cases of HF developed, and in 1 case risk probability could not be calculated in this model because of missing data for a few covariables.
Complementary Prognostic Value of NT-proBNP and the LV Mass Index
Although most cases of incident HF occurred among participants in the fourth quartile of NT-proBNP, some HF events developed among those in the 3 lower quartiles (n=26), which included most MESA participants (n=4199). In this group with lower values, the LV mass index had greater predictive power (HR per 1 SD increment = 2.04, 1.36–3.06, P=0.001) than NT-proBNP (HR per 1 SD increment = 1.46, 0.77–2.75, P=0.24 in model 3) before and after adjustment for all covariates included in the previous analyses (Appendix 2). In addition, among participants of both the highest quartile for NT-proBNP and for LV mass index, the HR for incident HF was 33.63 compared with participants in the lower quartiles for both variables after adjustment for Model 2 covariates (Table 4).
Table 4. Hazard Ratio (95% CI) of Incident Heart Failure According to Elevated LV Mass Index and NT-proBNP.
| NT-pro BNP in 4th Q | LVMIin 4th Q | Event no. /Sample Size (%) | HR | HR Adjusted |
|---|---|---|---|---|
| No | No | 8/2413 (0.3) | 1 (reference) | 1 (reference) |
| No | Yes | 11/769 (1.4) | 4.35 (1.75–10.80) | 3.28 (1.20–8.99) |
| Yes | No | 22/710 (3.1) | 9.59 (4.27–21.55) | 8.72 (3.50–21.70) |
| Yes | Yes | 35/271 (12.9) | 46.03 (21.34–99.29) | 33.63 (13.91–81.34) |
112.5 pg/mL and 86.8 g/m2 are cut off values of 4th quartile LVMI and NT-proBNP, respectively. NT-proBNP indicates N-terminal–pro B type natriuretic peptide; LV, left ventricle; HR, hazard ratio; LVMI, left ventricular mass index.
Cox regression analysis and the results after adjustment of the covariates in Model 2.
Discussion
The main finding of this study is that plasma NT-proBNP predicts incident HF in asymptomatic individuals over and above established HF risk factors and LV hypertrophy assessed as the LV mass index, as well as interim myocardial infarction. This relationship was upheld in men and women and among individuals of different ethnicities. These findings suggest that higher NT-proBNP is not only a mediator for other risk factors, but may also function as an independent predictor of incident HF. Indeed, we demonstrate that NT-proBNP levels are predictive of incident HF using C-statistics as well as discrimination and reclassification analyses,13,14 which are currently considered as the standard methods for evaluation of novel prognostic markers of cardiovascular risk.14,15 To confirm the additive role of NT-proBNP, we also assessed NRI using different risk categories (<3%, 3–10%, >10%; <6%, 6–20%, >20%) and also category-less NRI.16 In these additional analyses, significant discrimination was demonstrated after adding NT-proBNP to the predictive models. These results support the concept that NT-proBNP measurements could be included as part of the evaluation of patients suspected to be in the earliest states of HF (stage B).17
Another potentially important result from this analysis is the finding that NT-proBNP values differed by ethnicity. We previously demonstrated that incident HF18 and baseline LV function19 were related to ethnicity in MESA, whereas similar relationships have been demonstrated in other studies.20 This raises the possibility of ethnic differences in the physiologic biomarker response to increased myocardial stress, which represents the underlying cause of NT-proBNP production and release, and could be related to genetic factors or exposure to unmeasured environmental confounders. However, regardless of the different ethnic distributions of NT-proBNP, this study demonstrated that this biomarker reliably predicted HF in <3 (Non-Hispanic whites, African-Americans, and Hispanics) of the 4 ethnic groups evaluated (among Chinese the power to test the hypothesis was limited). These results support the generalizability of our findings to at least these 3 ethnicities.3
Although NT-proBNP has consistently been shown to be associated with clinically overt HF, there is controversy as to whether higher NT-proBNP can predict HF among asymptomatic individuals with lower levels of NT-proBNP or within the normal reference range.3,6 In this study, 77% of the incident HF cases occurred among those in the top fourth quartile of NT-proBNP (>112.5 pg/mL) for this population. Therefore, further risk stratification is needed for individuals with lower levels of NT-proBNP, because most individuals in an asymptomatic population fall into such category. Indeed, in the subgroup with NT-proBNP below the fourth quartile, NT-proBNP was a weaker predictor of incident HF than the LV mass index. This could be explained by a threshold effect for biomarker release which may not be reached until the heart has exhausted its ability to carry out hypertrophy and remodeling to maintain wall stress at low levels. Conversely, it could also be secondary to NT-proBNP gene polymorphism,6,21–24 genetic predisposition, or the possibility that HF in individuals with low baseline levels of NT-proBNP have a different pathogenesis. In this subpopulation, increased LV mass, which reflects compensatory remodeling in response to ventricular overload, was a better predictor of HF, and provided additive prognostic information to NT-proBNP. Finally, by combining the LV mass index with NT-proBNP, the overall predictive power was remarkably increased for both the lower and the higher NT-proBNP subgroups, suggesting mutually additive prognostic power between the imaging and biochemical markers. Therefore, although both NT-proBNP and LV mass reflect responses to increased LV wall stress, their contribution to prognostication might be mutually independent and complementary. Further studies are necessary to confirm these findings.
This study has limitations that deserve discussion. First, the subgroup analyses, used to determine the predictors for HF among MESA participants with lower NT-proBNP levels, might have the well-known limitations of subgroup analysis in general.25 Second, it is unclear whether the complementary risk prediction of NT-proBNP and structural LV indices is secondary to measurement error as opposed to biological complementarity. Finally, the number of incident HF events limited our ability to assess the effect of interactions fully.
In conclusion, NT-proBNP provides additional predictive information for the future development of HF, over and above traditional risk factors and the LV mass index in a multiethnic asymptomatic population without baseline history of heart disease.
Supplementary Material
Supplemental Appendix 1. For the computation of NRI, three categorization approaches were applied to the predicted probabilities of HF within 6 years: (a) “<6%, 6 to 20%, and >20%”, (b) “<3%, 3 to 10%, and >10%”, and (c) category-less;1 due to uncertainty about cutpoints for risk categories for HF. We compared the change of the predicted probabilities of HF within 6 years based on the risk categories given in (a) and (b) and the category-less approach (c). Based on the estimated risk categories and the predicted probabilities of HF within 6 years, calculated NRI and IDI values, their corresponding standard errors (SE), and the p-values for testing the null hypotheses of having zero NRI and IDI values were computed using Equations 3 through 15 from previous work by Pencina et al.2
Supplemental Appendix 2. Effects of Interaction between NT-proBNP and other covariates in cox regression for incident HF.
Supplemental Appendix 3. Cox regression analysis for incident HF in lower NT-proBNP (<112.5 pg/mL, n=4169) population with Model 3 covariates.
Clinical Perspective.
In this study of asymptomatic subjects from the Multi-Ethnic Study of Atherosclerosis, a total of 5597 multiethnic participants without clinically apparent cardiovascular disease underwent baseline measurement of N-terminal–pro B type natriuretic peptide, and were followed for 5.5±1.1 years. Higher plasma N-terminal–pro B type natriuretic peptideat baseline was associated with an increase in the risk of future incident heart failure even after adjustment for traditional risk factors, left ventricular mass index and interim myocardial infarction. This relationship held in men and women and among individuals of different ethnic groups. N-terminal–pro B type natriuretic peptideprovided additive prognostic value beyond both traditional risk factors and left ventricular mass index (measured by cardiac magnetic resonance imaging, the most accurate methodology currently available to assess left ventricular remodeling and hypertrophy) for predicting incident heart failure. We conclude that N-terminal–pro B type natriuretic peptideprovides additional predictive information for the future development of heart failure, over and above traditional risk factors and the left ventricular mass index, in a multiethnic asymptomatic population without baseline history of heart disease. These data may have implications for screening strategies.
Acknowledgments
Sources of Funding: This study was supported by the National Heart, Lung, and Blood Institute grant (R01-HL66075-01), the Multi-Ethnic Study of Atherosclerosis study contracts (N01-HC-95162, N01-HC-95168, and N01-HC-95169), and Roche Diagnostics.
Footnotes
The online-only Data Supplement is available at http://circheartfailure.ahajournals.org/lookup/suppl/doi:10.1161/CIRCHEARTFAILURE.112.968701/-/DC1.
Disclosures: None.
References
- 1.Mann DL. Mechanisms and models in heart failure: a combinatorial approach. Circulation. 1999;100:999–1008. doi: 10.1161/01.cir.100.9.999. [DOI] [PubMed] [Google Scholar]
- 2.Doust JA, Pietrzak E, Dobson A, Glasziou P. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. BMJ. 2005;330:625. doi: 10.1136/bmj.330.7492.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Omland T, Wolf PA, Vasan RS. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350:655–663. doi: 10.1056/NEJMoa031994. [DOI] [PubMed] [Google Scholar]
- 4.Kistorp C, Raymond I, Pedersen F, Gustafsson F, Faber J, Hildebrandt P. N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. JAMA. 2005;293:1609–1616. doi: 10.1001/jama.293.13.1609. [DOI] [PubMed] [Google Scholar]
- 5.Daniels LB, Bhalla V, Clopton P, Hollander JE, Guss D, McCullough PA, Nowak R, Green G, Saltzberg M, Ellison SR, Bhalla MA, Jesse R, Maisel A. B-type natriuretic peptide (BNP) levels and ethnic disparities in perceived severity of heart failure: results from the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT) multicenter study of BNP levels and emergency department decision making in patients presenting with shortness of breath. J Card Fail. 2006;12:281–285. doi: 10.1016/j.cardfail.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 6.McKie PM, Cataliotti A, Lahr BD, Martin FL, Redfeld MM, Bailey KR, Rodeheffer RJ, Burnett JC., Jr The prognostic value of N-terminal pro-B-type natriuretic peptide for death and cardiovascular events in healthy normal and stage A/B heart failure subjects. J Am Coll Cardiol. 2010;55:2140–2147. doi: 10.1016/j.jacc.2010.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bluemke DA, Kronmal RA, Lima JA, Liu K, Olson J, Burke GL, Folsom AR. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–2155. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Simone G, Gottdiener JS, Chinali M, Maurer MS. Left ventricular mass predicts heart failure not related to previous myocardial infarction: the Cardiovascular Health Study. Eur Heart J. 2008;29:741–747. doi: 10.1093/eurheartj/ehm605. [DOI] [PubMed] [Google Scholar]
- 9.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 10.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 11.Daniels LB, Laughlin GA, Clopton P, Maisel AS, Barrett-Connor E. Minimally elevated cardiac troponin T and elevated N-terminal pro-B-type natriuretic peptide predict mortality in older adults: results from the Rancho Bernardo Study. J Am Coll Cardiol. 2008;52:450–459. doi: 10.1016/j.jacc.2008.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain A, McClelland RL, Polak JF, Shea S, Burke GL, Bild DE, Watson KE, Budoff MJ, Liu K, Post WS, Folsom AR, Lima JA, Bluemke DA. Cardiovascular imaging for assessing cardiovascular risk in asymptomatic men versus women: the multiethnic study of atherosclerosis (MESA) Circ Cardiovasc Imaging. 2011;4:8–15. doi: 10.1161/CIRCIMAGING.110.959403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. doi: 10.1002/sim.2929. discussion 207. [DOI] [PubMed] [Google Scholar]
- 14.Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkind MS, Go AS, Harrell FE, Jr, Hong Y, Howard BV, Howard VJ, Hsue PY, Kramer CM, McConnell JP, Normand SL, O'Donnell CJ, Smith SC, Jr, Wilson PW. American Heart Association Expert Panel on Subclinical Atherosclerotic Diseases and Emerging Risk Factors and the Stroke Council. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–2416. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ioannidis JP, Tzoulaki I. What makes a good predictor?: the evidence applied to coronary artery calcium score. JAMA. 2010;303:1646–1647. doi: 10.1001/jama.2010.503. [DOI] [PubMed] [Google Scholar]
- 16.Pencina MJ, D'Agostino RB, Vasan RS. Statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med. 2010;48:1703–1711. doi: 10.1515/CCLM.2010.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:e391–e479. doi: 10.1161/CIRCULATIONAHA.109.192065. [DOI] [PubMed] [Google Scholar]
- 18.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, Burke GL, Lima JA. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernandes VR, Cheng S, Cheng YJ, Rosen B, Agarwal S, McClelland RL, Bluemke DA, Lima JA. Racial and ethnic differences in subclinical myocardial function: the Multi-Ethnic Study of Atherosclerosis. Heart. 2011;97:405–410. doi: 10.1136/hrt.2010.209452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tokola H, Hautala N, Marttila M, Magga J, Pikkarainen S, Kerkelä R, Vuolteenaho O, Ruskoaho H. Mechanical load-induced alterations in B-type natriuretic peptide gene expression. Can J Physiol Pharmacol. 2001;79:646–653. [PubMed] [Google Scholar]
- 22.Rame JE, Tam SW, McNamara D, Worcel M, Sabolinski ML, Wu AH, Dries DL. Dysfunctional corin i555(p568) allele is associated with impaired brain natriuretic peptide processing and adverse outcomes in blacks with systolic heart failure: results from the Genetic Risk Assessment in Heart Failure substudy. Circ Heart Fail. 2009;2:541–548. doi: 10.1161/CIRCHEARTFAILURE.109.866822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Costello-Boerrigter LC, Boerrigter G, Ameenuddin S, Mahoney DW, Slusser JP, Heublein DM, Redfeld MM, Rodeheffer RJ, Olson TM, Burnett JC. B-type natriuretic peptide single nucleotide polymorphism rs198389 impacts test characteristics of common assays (abstr) Circulation. 2009;120(Suppl):S777. doi: 10.4065/mcp.2010.0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meirhaeghe A, Sandhu MS, McCarthy MI, de Groote P, Cottel D, Arveiler D, Ferrières J, Groves CJ, Hattersley AT, Hitman GA, Walker M, Wareham NJ, Amouyel P. Association between the T-381C polymorphism of the brain natriuretic peptide gene and risk of type 2 diabetes in human populations. Hum Mol Genet. 2007;16:1343–1350. doi: 10.1093/hmg/ddm084. [DOI] [PubMed] [Google Scholar]
- 25.Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in medicine–reporting of subgroup analyses in clinical trials. N Engl J Med. 2007;357:2189–2194. doi: 10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Appendix 1. For the computation of NRI, three categorization approaches were applied to the predicted probabilities of HF within 6 years: (a) “<6%, 6 to 20%, and >20%”, (b) “<3%, 3 to 10%, and >10%”, and (c) category-less;1 due to uncertainty about cutpoints for risk categories for HF. We compared the change of the predicted probabilities of HF within 6 years based on the risk categories given in (a) and (b) and the category-less approach (c). Based on the estimated risk categories and the predicted probabilities of HF within 6 years, calculated NRI and IDI values, their corresponding standard errors (SE), and the p-values for testing the null hypotheses of having zero NRI and IDI values were computed using Equations 3 through 15 from previous work by Pencina et al.2
Supplemental Appendix 2. Effects of Interaction between NT-proBNP and other covariates in cox regression for incident HF.
Supplemental Appendix 3. Cox regression analysis for incident HF in lower NT-proBNP (<112.5 pg/mL, n=4169) population with Model 3 covariates.


