Abstract
Osteoporosis is a global problem with an expected increase in f acture prevalence and public health burden as the world s population ages. Although excess mortality is well-described in those with low bone mineral density as well as those with recent hip and vertebral fractures, some uncertainty remains about whether this link is causal. Survival depends greatly on the fracture types, age, gender, and race. Deaths are predominately due to comorbidities, but may also be attributed to the fracture event itself, either directly or indirectly. The goal of osteoporosis care is prevention of fractures and ultimately reduction in morbidity and mortality. Until recently, there have been no data showing that osteoporosis treatment improves mortality, and even now the extent of these data are rather limited. Large observational cohort studies over considerable time are needed to determine whether improving osteoporosis quality of care will improve mortality rates.
Keywords: Osteoporosis, hip fractures, vertebral fractures, mortality, epidemiology
Introduction
Osteoporosis is a systemic skeletal disorder characterized by reduced bone strength predisposing to an increased risk of fracture. The clinical and public health importance of osteoporosis arises primarily from fragility fractures. Fragility fractures are one of the most common causes of disability and a major contributor to costs of medical care in all regions of the world (1). Clinical consequences of fracture include short and long-term morbidity characterized by pain, limitation of function, decreased health-related quality of life, and increased mortality. As fracture prevalence increases in tandem with increasing longevity of the population steoporosis is becoming an even more significant public health burden (2–7) The mortality risk of patients with osteoporosis is increased by approximately
1.5-fold for each standard deviation decrease in bone mineral density (BMD) (8–10). Survival estimates are dependent on fracture location and the completeness and duration of follow-up after fractures. Excess mortality in osteoporotic fractures occurs following fractures of the spine (radiographic and clinical fractures) (11–23) and particularly of the hip (17, 24–36). By contrast, there appears to be no excess mortality among patients who sustain a distal forearm, foot, or ankle fracture (12, 14, 17, 37). Although mortality rates are lower in younger elderly individuals who sustain fractures, people in this age group constitute a large proportion of the elderly population, and thus contribute substantially to the total number of excess deaths due to osteoporosis (13)
While osteoporosis-associated mortality is a well-recognized public health concern, the impact of other risk factors on mortality associated with osteoporosis remains unclear. Osteoporosis treatment has been shown to reduce the risk of subsequent fracture, but the impact on mortality has been minimally studied (38, 39). Understanding the possible relationship between mortality and osteoporosis fractures is needed to design strategies to improve quality of care in osteoporosis.
Mortality outcomes of osteoporosis have been analyzed in cohort studies and case-control observational study designs (often using linked hospital and death data). Many of these studies examine the observed mortality compared with the expected mortality of the (healthier) general population (13, 40, 41) of same sex and age; the difference between the observed and expected represents excess mortality. The cause of death is not always noted, and even if described, the contribution of fractures or falls may be underestimated since only the most proximate cause of death and not the inciting event is usually reported (42).
In cohort studies, the relationship between fracture (the exposure) and mortality (the outcome) is evaluated after adjusting for a variety of potentially confounding factors. Since people who fracture have generally poorer general health and physical function, earlier death may be a result of the patients poor health, greater number of pre-fracture comorbidities, and poor physical function. For some people, a fracture may be a sentinel event that leads to new diseases, difficulty with rehabilitation, progressive functional decline, loss of independence, and disability. Thus related health states, not directly caused by the fracture event itself, may be as important as the fracture in premature mortality. In order to delineate the quantum of excess mortality contributed by osteoporotic fractures and the tent to which mortality may be reduced through fracture prevention, control groups in these studies should ideally be subjects with health states as similar as possible to those of the study population. In addition to patient factors, the process of care, including surgery, rehabilitation, and post-care disposition, are crucial to quantify in order to determine which factors, if any, predispose to better post-fracture outcomes. This article reviews the recent clinical and epidemiological characteristics of mortality associated with osteoporotic hip and vertebral fractures worldwide.
Hip fractures and mortality
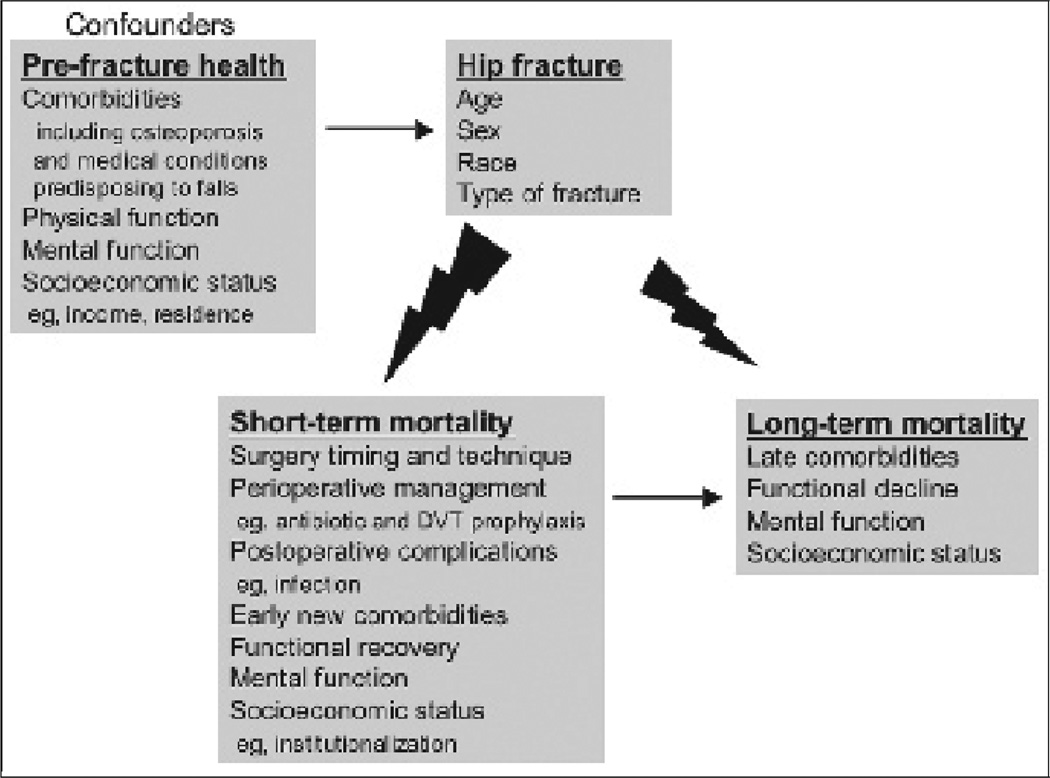
Hip fractures are the most serious of all osteoporotic fractures with extremely costly consequences. While mortality rate is undoubtedly high following hip fracture, there is still considerable controversy over the direct contribution of hip fractures to this excess mortality. Hip fracture may result in mortality either directly, indirectly, mediated through new or altered comorbidities, or as a result of pre-existing comorbidities that are simply associated with fracture risk. The first three circumstances represent causal (or partially causal) associations, whereas the latter would represent an example of a confounding factor (Fig. 1).
Fig. 1.
Predictors of mortality following osteoporotic hip fractures.
Mortality rates are highest during the firsr 6 months immediately after the fracture; lower, but still greater than in the general population, for up to 12 months post-fracture (25, 26, 34–36, 43–45); and appear to decrease with time thereafter. Mortality rates range from 10% to 45% in the first year (Table I). When and whether the mortality curves converge with those of the general population varies in different studies The majority of studies show persistently increased mortality rates (12, 17, 25, 26, 32, 35, 40, 43, 44, 46), while others suggest no long-term elevated mortality over time (34, 47) relative to that expected in older individuals. Differences across studies may be explained in part by variations in cohort characteristics (age, institutionalized, etc), health of the comparator groups, method of calculating excess mortality, and whether frailty before fracture has been taken into account adequately.
Table I.
Studies on hip fractures (HFx) and mortality rates and ratios (past 5 years).
| Study (ref) | Location | Number of patients | Deaths in patients with HFx |
Relative risk compared with non-fractured (95% CI) |
Mortality rate by year after HF (% or per 100 person-years (95% CI)) |
Standardized mortality ratio (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| <1 year | 1 to <5 years | 5 years | <1 year | 1 to <5 years | 5 years | |||||
| Hindmarsh 2008 (28) | ||||||||||
| New South Wales, | 16836 HFx | |||||||||
| Australia | 65 –74 yo M | 18 | 1.2* | 1.3* | ||||||
| 65 –74 yo W | 10 | 1.1* | 1.1* | |||||||
| 85+ yo M | 35 | 1.6* | 1.8* | |||||||
| 85+ yo W | 20 | 1.3* | 1.4* | |||||||
| Paksima 2008 (32) | United States | 1050 HFx | 479 | 2.7 | 12.9 (1y) | 41.2 (5y) | 1.5 (1y) | 0.9 (5y) | ||
| (single hospital) | in-hospital | 18.5 (2y) | 75.3 (10y) | 1.1 (2y) | 0.6 (10y) | |||||
| 1.0 (3y) | ||||||||||
| Vestergaard 2007 (35) | Denmark | 169145 HFx | 121953 | 2.3 (2.2–2.3) | 28* | 2* | 1.3* | 1.2* | ||
| 524010 controls | a2.0 (1.9–2.0) | |||||||||
| Tosteson 2007 (34) | United States | 25178 | < 6 months | |||||||
| 730 incident HFx | 292 | b 11.6 (8.9–15.1) | 20 | |||||||
| c 6.3(4.8–8.2) | ||||||||||
| d 6.3 (4.8–8.2) | ||||||||||
| > 6 months | ||||||||||
| b 1.4 (1.2–1.6) | ||||||||||
| c 1.0 (0.9–1.2) | ||||||||||
| d1.0 (0.9–1.2) | ||||||||||
| Muraki 2006 (31) | Japan | 480 HFx | 3.5 | 11.5 (1 y) | 59* (5y) | |||||
| in-hospital | 82* (10y) | |||||||||
| Vidal 2006 (36) | Brazil | 606 post hip repair | 130 | /100 py | ||||||
| 95 (1mo) | 1.1 (7.9–1.5) | |||||||||
| 44 (1–3mo) | 5.1 (3.7–7.0) | |||||||||
| 11 (3mo–1y) | 1.4 (1.0–1.8) | |||||||||
| Pande 2006 (33) | United Kingdom | 100 M HFx | g 6.7 (3.4–13.4) | 25 (3mo) | 45 (1y) | |||||
| 100 controls | g6.2 (3.1–12.4) | 63 (2y) | ||||||||
| g 7.2 (3.5–14.7) | ||||||||||
| Karagiannis 2006 (29) | Greece | 499 HFx post surgery | IT: FN | IT: FN | ||||||
| (single hospital) | 17.9: 11.3 ns | 48.8: 34.7 (5y) | ||||||||
| 76: 58 (10y) | ||||||||||
| Farahmand 2005 (26) | Sweden | 2245 W HFx | 896 | 2.3 (2.0 2.5) | 4.3 (3mo) | 10.6 (1y) | 53 | |||
| 4035 W controls | f16 | |||||||||
| Franzo A, 2005 (27) | Italy | 6629 | 20.0 | 25.3 | ||||||
| Alegre-Lopez J, 2005 (24) | Spain | 218 | 49 | 65.3 (3mo) | 21 (1y) | |||||
| Johnell 2004 (47) | Malmö, Sweden | 1143 | 678 | 22.3 | ||||||
HFx: Hip fracture; M: men; W: women; ns: not significant; yo: years old; mo: months; y: year; /100 py: per hundred person-years; IT: intertrochanteric fracture; FN: femoral neck fracture;
derived from graph;
: adjusted for multiple covariates;
: adjusted for age, sex and race;
: adjusted for age, sex, race, functional status, comorbid conditions and socioeconomic variables;
: adjusted for age, sex, race, functional status, and comorbid conditions;
: previous serious hospitalization;
: without previous serious hospitalization;
: adjusted for age and quality of life measures.
In a recent Danish population-based cohort of all patients with hip fractures, the mortality rate was nearly 30% compared with age- and gender matched subjects from the general population. Mortality in patients was 19% greater than in the control subjects (relative survival = 0.81) in the first year after fracture. The major causes of death were factors associated with the accident leading to the fracture, accounting for 71% of all deaths within the first 30 days. Little of the excess mortality was attributed to pre-morbid conditions, with the exception of lower income. There was a small but constant 1.8% excess annual mortality for the subsequent 19 years. Therefore, over a period of 20 years, the long-term excess mortality contributed more than the short-term excess (35). In contrast, Tosteson et al. found no evidence of excess mortality beyond 6 months following hip fracture, despite adjustments for various pre-morbid conditions and function, in an elderly U.S. population that included persons who were institutionalized (34).
Risk factors associated with hip fracture mortality
Sex, age and race/ethnicity
Although the prevalence of hip fractures is higher in women, men have a higher risk of death than women after a hip fracture (28, 29, 32, 35, 41, 43, 48), but the gender-based difference is not significant after adjustment for age (17). The proportion of years of life lost was higher in men, even after considering higher mortality rates of males in the general population (41).
Intuitively, age is an independent predictor of mortality. However, some studies have shown an inverse relationship between age and excess risk of death. Older hip fracture patients have a much lower excess or relative risk of mortality than younger patients (i.e., age was an effect modifier) (26, 28, 35), since more older people in the general population die. In people with diseases, relative risk is almost always higher in younger subjects while absolute risk is higher in older subjects, as younger (control) people who do not have diseases are less likely to die.
Although understudied, there also appears to be a race/ethnicity disparity in mortality after hip fractures. Using a Medicare claims database, black women had higher mortality after a hip fracture than white women. The survival curves for black women and white women diverged during the first 9 months following hip fracture, thereafter remaining parallel. Men experienced the highest mortality, with nearly identical rates among blacks and whites. The observed race/ethnicity differences in fracture mortality were consistent despite stratification by age at time of hip fracture and by number of comorbid medical conditions (49). By contrast, early or late mortality following hip fracture was not affected by black versus non-black race/ethnicity in a subgroup analysis of a recent study of Medicare beneficiaries (34). However, unlike the earlier study (49), this study was not powered to study the sex-race interactions in early and late hip fracture mortality risks.
Type of fracture
Seemingly an unmodifiable risk factor, the type of hip fracture and consequently the type of surgical intervention result in differential survival (50). Intertrochanteric compared to femoral neck fractures led to significantly higher mortality risk at hospital discharge, at 1 year [relative risk (RR) 2.5; 95% confidence interval (CI) 1.3 – 5.1] (51), and up to10 years (RR 1.4; 95% CI 1.0 – 1.8) (29). The higher mortality rates with intertrochanteric fractures may be due to greater frailty before injury, older age, and more severe osteoporosis (52–55). This effect persisted after accounting for age and comorbid conditions; the functional outcomes among surviving patients was similar (51).
Perioperative factors and surgical complications
Postoperative complications of hip fractures such as infections and cardiovascular diseases are well-recognized causes of immediate mortality (32, 33, 35, 36, 56–58). Any major post-operative complication is associated with 90% increased mortality risk (32). Good surgical technique and minimization of operative delay (58–61) may minimize postoperative complications and improve early mortality outcomes, although studies are inconsistent (27, 62). In a meta-analysis, regional anesthesia appeared to reduce acute postoperative confusion but had no apparent effect on mortality (63). Appropriate perioperative management with antibiotics (64), blood transfusion (65), and prevention of deep venous thrombosis and pulmonary embolism (66, 67) also appear to improve mortality outcomes. In addition to these measures that reflect in-hospital quality of care, increase in hospital volume for hip fracture surgery has been associated with increased inmortality (27), although this finding is discordant with previous studies that either were small or did not adjust for confounding factors (68, 69).
Comorbidities and functional status
The severity of comorbidities, measured using the American Society of Anesthesiologists grading system, is an important predictor of mortality after a hip fracture (32, 40, 58, 70, 71). The more dependent the patient is in ambulatory status, activities of daily living (ADL), and instrumental ADL prior to hip fracture, the higher the mortality risk (32–34). Poor isometric knee extension strength may be a measure of frailty and old age but also has been shown to predict increased mortality independently after the fracture (72).
A substantially increased mortality risk after hip fracture was observed among subjects with more than 5 hospitalizations since availability of electronic inpatient records (26). Previous serious hospitalization as a surrogate for poor pre-fracture health did not increase the relative risk of demise. However, when calculated in absolute terms, previous serious hospitalization increased the attributable 5-year mortality risk from 9% to 26% (26). The relative attributable mortality risk of hip fracture was higher for women than men, increased with age, and was markedly lower when hazard ratios were adjusted for health status in another study (34). It is complex, however, to compare these figures due to the different methodologies and assumptions used in different studies.
Socioeconomic factors
In a large Danish case-control study, the excess mortality of hip fractures changed only slightly upon adjustment forpre-morbid conditions, except for income, suggesting the importance of socio-economic factors on better out- (35). Institutionalized patients suffer higher mortality after hip fracture (33, 73). Although elderly people with hip fractures reported living alone more frequently and were less likely to be health maintenance organization members, these and other socioeconomic factors had no association with on mortality in another study (34).
Osteoporosis interventions to reduce mortality
It remains unclear whether prevention of fractures using anti-osteoporotic therapies may extend life expectancy, and to what extent. In a recent randomized controlled trial of secondary fracture prevention (39), there was a 28% reduction of mortality after 16 months in the zoledronic acid group compared to the placebo group, in addition to prevention of recurrent symptomatic fractures. Mortality outcome was not one of the pre-specified study endpoints, and this unexpected finding has not been explained. Extremely large population cohort studies are needed to establish whether prevention of a secondary hip fracture will improve longevity. After a hip fracture has occurred, implementation of evidence-based clinical pathways appears to reduce postoperative morbidity, but may not affect mortality (74, 75). However, co-management of hip fracture patients by orthopedic surgeons and geriatricians may potentially improve outcomes (76, 77). In summary, reducing the number of hip fractures and optimizing immediate post-fracture medical care may reduce mortality, particularly if the focus is on reducing comorbidities such as infection and cardiovascular complications immediately following this very serious yet common late-life event. Further studies are required to identify other factors in the process of care that are associated with better outcomes
Vertebral fractures and mortality
Vertebral fractures are the most frequent complication of osteoporosis (14, 78). The lifetime risk of a clinically diagnosed vertebral fracture after the age of 50 is estimated to be 9% in men and 15% in women (79). However, only one-third of cases are clinically diagnosed and an even smaller proportion of patients are admitted to hospital (18, 80, 81). Compared to hip fractures, it is thus more even more challenging to analyze the mortality burden of vertebral fractures.
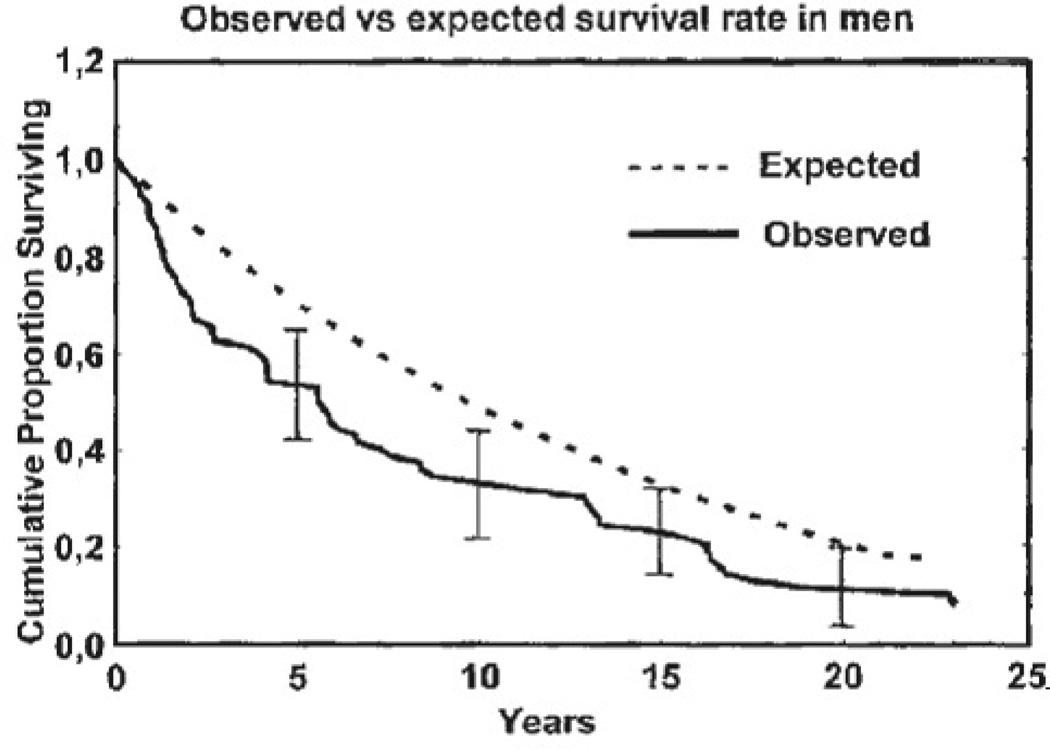
Many studies have indicated an increase in mortality risk after vertebral fracture (11–14, 16, 18, 20, 21, 23, 82,83). Excess mortality varies substantially after a clinical vertebral fracture, with 1-year rates ranging considerably from 1.9 to 42% (Table III). Increased mortality risk appears lower than that for hip fractures (13), although one study, the Study of Osteoporotic Fractures, indicated higher mortality risk following vertebral fracture (RR = 8.6) compared to hip (RR = 6.7) (although the CIs overlapped) (12). As with hip fractures, mortality risk is most marked within the first year after fracture (12– 14, 20, 82), but an increased mortality risk greater than that of the general population extends for up to 5–22 years (14, 82). In one of the longest cohort studies, with 22 years of post-fracture follow-up, the post-vertebral fracture survival curves of men and women were similar in general. The greatest divergence of survival curves from the age-expected norms occurred during the first 3 years in men (Fig. 2) but later (near the tenth year) in women (data not shown), compared to the general population. After the first decade, the curves converged towards expected mortality rates in both sexes. Despite this, mortality was significantly higher in those experiencing vertebral fractures than in the comparator group over the entire 22-year follow-up period (82).
Table III.
Studies on vertebral fractures (VF) and mortality rates and ratios.
| Study | Location | Number of patients | Deaths in patients with VF |
Relative risk of death compared with non-fractured (95% CI) |
Mortality rate by year after VF (% or per 100 person-years) (95% CI) |
Standardized mortality ratio (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| <1 year | 1 to <5 years | 5 years | <1 year | 1 to <5 years | 5 years | ||||||
| Clinical VF | |||||||||||
| Lau 2008 (85) | United States | 97142 VF | 39707 | j1.8 (1.8–1.9) | 46.1 (3y) | 69.1 (5y) | |||||
| 428956 controls | 89.5 (7y) | ||||||||||
| Bouza 2007 (11) | Spain | 7100 | 246 | 3.5 | |||||||
| Osteoporotic VF | in-hospital | in-hospital | |||||||||
| By ICD-9 code | |||||||||||
| Kanis 2004 (20) | Sweden | 16051 (40358 py) | M1597 | /100py | /100py | /100py | |||||
| By ICD-9 codes | W4065 | ||||||||||
| M 50 yo | 3.2 (2.8–3.7) | 1.8 (1.6–2.0) | 13.2 | 7.3 | |||||||
| M 80 yo | 15.9 (15.2–16.5) | 8.8 (8.4–9.2) | 2.2 | 1.2 | |||||||
| W 50 yo | 1.9 (1.4–2.7) | 1.6 (1.1–2.2) | 12.5 | 10.2 | |||||||
| W 80 yo | 12.9 (11.3–14.9) | 10.9 (9.2–12.1) | 15* (5y) | 2.9 | 2.4 | ||||||
| 20* (8y) | |||||||||||
| Cauley 2000 (12) | United States | 6459 W | b8.6 (4.5–16.7) | 100py | |||||||
| (FIT) | 2027 prevalent VF | 6.8 | |||||||||
| 119 incident VF | 11 | ||||||||||
| Center 1999 (13) | Dubbo, | 4312 subjects | /100py | /100py | /100py | Incident | Prevalent | ||||
| Australia | 76 W incident VF | 16 | 13.5 | 1.6 | 1.1 | 6 (1 4– 8) | 8 (1 6 2 1) | ||||
| 38 M incident VF | 17 | 42 | 4.8 | 1.4 | 8 (1 6 2 0) | 3 7 (3 4 3 9) | |||||
| 1.7 (1.5–1.8) | |||||||||||
| 2.4 (2.2–2.6) | |||||||||||
| Cooper 1993 (14) | Rochester, | 335 incident VF | 76 | 39 (5y) | 1.2 (1.1–1.4) | ||||||
| Minnesota | |||||||||||
| United States | |||||||||||
| Radiographic morphometric VF | |||||||||||
| Trone 2007 (22) | United States | 1580 subjects | 1 VF: 1.1 (0.8–1.4) | 41 (8y) | 1.5 (p<0.001) | ||||||
| 178 prevalent VF | 73 | ||||||||||
| 2 VF | |||||||||||
| 1.6 (1.0–2.4) | |||||||||||
| Hasserius 2005 (82) | Sweden | 257 prevalent | 64M, 166W M: not verifiable | /100py | |||||||
| (EVOS) | clinical VF | W: 2.8 (1.0–7.9) | 11.2 | 1.5* | |||||||
| 23 incident VF | Incident VF | 9.5 | 1.5* | ||||||||
| (over 1st 12y) | (22y) | (22y) | |||||||||
| Naves 2003 (21) | Spain | 308 M | 65M | M not increased | 7* (5y) | 1.3* (5y) | |||||
| Part of EVOS | 316 W | 37W | W: d 2.2(1.1–4.6) | 6* (5y) | 2.2* (5y) | ||||||
| 147 prevalent VF | f 2.0 (1.0–4.1) | 25* (8y) | 1.6* (8y) | ||||||||
| 11 incident VF | Post all VF | 22* (8y) | 3.1* (8y) | ||||||||
| Kado 2003 (19) | United States | 7233 | 1.3 (1.1 1.6) | g 27* (8y) | |||||||
| (part of SOF) | 1414 prevalent VF | h 35* (8y) | |||||||||
| 389 incident VF | 1.1 (0.9–1.3) | ||||||||||
| Incident VF | |||||||||||
| Jalava 2003 (16) | Finland | 677 | Prevalent VF: 4.4 | /100py | |||||||
| 352 prevalent VF | 31 | (1.9–10.6); | 59 yo: 2.1 | ||||||||
| 2.4 (0.9–6.2) | 69 yo: 3.2 | ||||||||||
| 118 incident VF | 7 | ||||||||||
| Incident VF | |||||||||||
| No increase | |||||||||||
| Ensrud 2000 (23) | United States | 6459 W | 1.6 (1.1–2.3) | ||||||||
| (FIT) | 2027 | 1 prevalent VF | 1.5 (1.1–2.2) | ||||||||
| Kado 1999 (18) | United States | 9575 W | 1.2 (1.1–1.4) | i2.3, 2.5, 2, 9, | |||||||
| (SOF) | 1915 with 1 | 3.2, 4.4 | |||||||||
| prevalent VF | /100py | ||||||||||
| (8y) | |||||||||||
| Ismail 1998 (15) | Europe | 6480 subjects | M 1.3(0.9–2.0); | M 1.4* (1y) | |||||||
| (EPOS) | 438 M prevalent VF | a 1.2 (0.7–1.8) | M 2.4* (4y) | ||||||||
| 429 W prevalent VF | W1.9 (1.0–3.4); | W1.1* (1y) | |||||||||
| a 1.6 (0.9–3.0) | W2.6* (4y) | ||||||||||
VF: vertebral fracture; M: men; W: women; yo: years-old; 95% CI: 95% Confidence Interval; ; EVOS: European Vertebral Osteoporosis Study; FIT: Fracture Intervention Trial (alendronate. placebo); SOF: Study of Osteoporotic Fractures; EPOS: European Prospective Osteoporosis Study;
derived from graph;
: adjusted for multiple covariates ;
adjusted for age, study group and treatment assignment;
: by any radiographic criteria;
: McCloskey-Kanis radiographic criterion;
: Genant Grade II radiograghic criterion;
: no prevalent and 1 incident VF; prevalent and 1 incident VF;
: for 1, 2, 3, 4, 5 prevalent VF respectively;
: adjusted for comorbidity; yo: years old; mo: months; y: years; /100 py: per hundred person-years.
Fig. 2.
Kaplan-Meier survival curve during a 22-year follow-up period after a clinically diagnosed vertebral fracture in men compared with the expected survival curve in the entire male Malmö population at risk. Ninety-five percent confidence intervals are shown at 5, 10, 15, and 20 years after the fracture event (82) [Reprinted with permission from Hasserius R, Karlsson MK, Jonsson B, Redlund- Johnell I, Johnell O. Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly--a 12- and 22-year follow-up of 257 patients. Calcif Tissue Int. 2005; 76(4): 235-42.]
Mortality patterns with vertebral fractures
Although the absolute risk of mortality associated with vertebral fracture increases with age (11, 13, 20), the age-matched relative risk of death is higher in younger individuals and decreases with age (13, 20). In a study where low- and high-energy-related vertebral fracture were not distinguished, younger patients died more commonly from high trauma injuries or from secondary causes of osteoporosis (20). Similar to hip fracture studies, most (11, 13, 16) but not all vertebral fracture studies (20, 21) describe a higher mortality in men compared to women Standardized mortality ratios (SMRs) were increased for incident and prevalent clinical vertebral fractures (13). Women with undiagnosed but vertebral fractures also had increased mortality risk in at least one study (18), contradicting the notion that subclinical fractures are less serious The risk of death increased with number and severity of prevalent vertebral fractures (18, 22, 23).
Other risk factors for mortality with vertebral fractures
Similar to analyses of mortality after hip fractures, reduced survival is difficult to attribute directly to vertebral fracture, since mortality is also a result of underlying comorbidities and/or complications of prolonged hospital stays (84). Frailty and health-behaviors as well as the extent of comorbidities explain a significant proportion of the excess mortality risk (11, 15, 16, 18, (Table IV). In a study based on hospital discharge ICD-9 codes, 26% of in hospital deaths was attributable to the fracture itself since this subgroup of patients had no identifiable comorbidity (11). In another study of nationwide hospitalizations for vertebral fractures in persons 50 years and older in Sweden, and based on assumptions that mortality in the first year was attributable to vertebral fracture, up to 28% of all deaths were attributed to vertebral fractures (20).
Table IV.
Factors related to mortality following vertebral fracture (relative risk ratio (95% CI)).
| Study: | Kado 1999 (18) | Kado 2003 (19) | Jalava 2003 (16) | Bouza 2007 (11) | Trone 2007 (22) |
|---|---|---|---|---|---|
| Sociodemographic and fall risk factors | |||||
| Men | 3.0 (1.0–8.8) | 1.5 (1.2–2.0) | 1.8 (1.3–2.5) | ||
| Age | 1.6 (1.5–1.6) | 1.6 (1.5–1.7) | a2.0 (1.3–2.8) | 1.6 (1.5–1.7) | |
| Vertebral fracture | 1.2 (1–1.3) | I: 1.1 (0.9–1.3) | 2.4 (0.9–6.2) | 1.1 (0.8, 1.4) | |
| P: 1.2 (1.0–1.3) | |||||
| Body mass index | 0.9 (0.9–1) | ||||
| Total body fat | 0.8 (0.8–0.9) | ||||
| % Weight change | 0.8 (0.8–0.9) | ||||
| Current smoking | 2.0 (1.8–2.3) | 1.3 (1.2–1.4) | 1.6 (1.1–2.3) | ||
| Comorbidities | |||||
| Diabetes mellitus | 1.8 (1.8–2.1) | 1.9 (1.6–2.3) | |||
| Hypertension | 1.4 (1.2–1.5) | ||||
| Health status | 1.6 (1.5–1.9) | 0.7 (0.6–0.8) | |||
| Serum ESR | 1.0 (1.0–1.1) | ||||
| Alcohol | 0.6 (0.3–1.2) | 1.0 (0.9–1.0) | |||
| Pulse > 80/min | 1.3 (1.1–1.5) | ||||
| Charlson Index 0 | |||||
| 1–2 | 2.1 (1.5–3.0) | ||||
| 3–4 | 5.0 (3.0–8.1) | ||||
| >4 | 8.5 (5.1–14.1) | ||||
| Physical Function | |||||
| Physical activity | 0.9 (0.8–0.9) | 1.0 (0.9–1.0) | 0.6 (0.5–0.8) | ||
| Inability to rise from chair | 1.5 (1.3–1.7) | ||||
| Difficulty standing on feet for 2 hours | 1.1 (1.0–1.2) | ||||
95% CI: 95% Confidence Interval; I: incident vertebral fracture; P: prevalent vertebral fracture;
age>80; ESR: erythrocyte sedimentation rate.
Prevalent versus incident vertebral fractures
Various studies have attempted to assess the mortality risk of prevalent versus incident clinical (11–14, 20) and radio- graphic vertebral fractures (16, 19, 82) (Table III). Prevalent vertebral fractures differ from incident spine fractures in that they may have occurred many years prior to study entry and have a different prognosis for mortality. After adjusting for age, poor health, and other known predictors, including sex, body mass index, calcium, estrogen or thiazide use, thyroid medication, alcohol intake, exercise, current smoking, physical function, etc., prevalent vertebral fractures were an independent risk factor for mortality in some (18, 19, 22, 23), but not all studies (15, 16). One study found that women with two or more prevalent fractures had increased risk of all-cause mortality which was not seen in women with a single prevalent radiographic vertebral fracture (22). The authors indicated that a single vertebral fracture detected by quantitative vertebral height and area assessment (radiographic vertebral morphometry) cannot always distinguish between a congenital anomaly and a fracture, but two or more morphometric fractures are more likely to be osteoporotic fractures (22).Mortality risk appears higher in people with incident morphometric vertebral fractures compared to those who do not have incident vertebral fractures (19). However, after adjustment for 12 covariates, including age, low bone density, prevalent vertebral fractures, weight loss, inability to rise from a chair, and difficulty standing for more than 2 hours, the association between incident vertebral fractures and mortality was not significant. This finding suggests that incident vertebral fractures do not directly cause death. Women who had experienced both a prevalent and incident vertebral fracture had the highest mortality, but there was no significant interaction between prevalent and incident vertebral fracture status. In other words, stratifying by prevalent vertebral fracture status did not affect the multivariable results. While it is possible that frailty can be both a cause and effect of vertebral fractures, the authors suggested that vertebral fractures, physical function decline, and weight loss may all be proxy markers of an accelerated aging process rather than independent contributors to mortality (19).
Proximate causes of death after vertebral fracture
In the Study of Osteoporotic Fractures (18), women with severe vertebral deformities had an increased risk of death due to pulmonary causes such as chronic obstructive pulmonary disease and pneumonia, even after adjusting for long term glucocorticoid and tobacco use. Severe kyphosis is strongly associated with pulmonary deaths, possibly due to restrictive lung disease and reduced respiratory reserves. Several studies report a greater rate of cancer mortality in women with vertebral fractures compared to those without fractures (14, 18), even after excluding the possibility of metastatic disease to the spine (18). In the Malmö population with vertebral fractures, cancer was significantly increased compared with the female, age- matched population at risk (82). In another study, however, there was no increased mortality risk in people with a history of vertebral fractures compared to the other patients (22), although the cause of death was unknown in 26% of the deceased. Differential classification of causes of death and the overall small number of deaths complicate meaningful comparisons across studies.
In summary, increased mortality rates have been observed after vertebral fractures, although the independent effect of the fracture on this outcome compared to the effect of comorbidities remains somewhat controversial. If a direct independent association between vertebral fracture and mortality exists, the pathophysiology of how vertebral fractures may lead to increased mortality remains unknown. While vertebral fractures may account partly for excess mortality, the underlying comorbidities and poor health status influence considerably the risk for vertebral fractures. This may be due either directly to the pathogenesis or by selection bias through increased medical surveillance of a sicker population with a higher risk of mortality. Beyond preventing future morbidity, it appears logical to manage post-vertebral fracture patients aggressively to potentially reduce the risk of death.
Conclusion
Hip and vertebral fragility fractures are associated with significantly increased mortality rates. No single factor predicts excess risk of death, and no proven solution to improving fracture survival in osteoporosis in all populations has been identified. The independent role of fractures versus other confounding factors, including functional status, comorbidities, capacity for independent living, etc., in increased mortality rates is uncertain. Aggressive treatment of osteoporosis, especially in patients who have already suffered from a fracture event, reduces morbidity and may translate into longer-term survival. Future research should help to better characterize critical predictors of mortality and to design cost-effective interventions with the goal to reduce short- and long-term morbidity and mortality in patients at greatest risk.
Table II.
Factors related to mortality following hip fracture (relative risk ratio (95% CI)) (Variables refer to those before fracture unless otherwise stated).
| Study | Paksima Lopez 2008 (32) |
Vestergaard 2007 (35) |
Muraki 2006 (31) |
Karagiannis 2006 (29) |
Farahmand 2005 (26) |
Franzo 2005 (27) |
Alegre- 2005 (24) |
|||
|---|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic and fall risk factors | ||||||||||
| Men | 1.4 (1.2–1.7) | 1.3 (1.3–1.4) | 1.4 (1.1–2.0) | 1.8 (1.3–2.4) | 1.7 (1.2–2.0) | 2.4 (2.1 2.8) | 2.4 (1.0–6.0) | |||
| Age | 1.0 (1.0–1.1) | 2.8 (2.8–2.9) | 1.0 (1.0–1.0) | 1.09 (1.1–1.1) | 1.1 (1.1–1.1) | d8.4 (2.5–28.0) | d 2.3 (1.3–3.9) | 1.6 (1.5 1.7) | 1.2 (0.3 4.2) | |
| b 6.3 (6.2–6.4) | 3.7 (2.2–6.3) | 1.5 (1.1–2.1) | (80y) | |||||||
| 12.7 (12.5–12.9) | f2.1 (1.5–2.8) | f 1.6 (1.3–2.1) | ||||||||
| Body mass index | <22 | 1.9 (1.4–2.6) | ||||||||
| 22–25 | 1.6 (1.2–2.2) | |||||||||
| >25 | 1.5 (1.1–2.1) | |||||||||
| Smoking | g1.6 (1.2–2.0) | |||||||||
| h2.0 (1.4–3.0) | ||||||||||
| i1.9 (1.3–2.7) | ||||||||||
| Use of hormone replacement therapy | 1.7 (1.4 2.1) | |||||||||
| (never) | ||||||||||
| 1.7 (1.2 2.4) | ||||||||||
| (ever) | ||||||||||
| Living single | 1.1 (1.1–1.1) | 1.5 (0.4–5.6) | ||||||||
| Income | 1.5 (1.5–1.6) | |||||||||
| Institutionalized at discharge | ns | 2.9 (1.0–8.4) | ||||||||
| Comorbidities and Physical Function | ||||||||||
| Charlson Index | 0 | Referent | 2.2 (2.0 2.4) | 0.6 (0.1 3.5) | ||||||
| 1–2 | 1.8(1.8–1.8) | (Charlson | (Comorbidity 1) | |||||||
| 3–4 | 2.7 (2.6–2.7) | (Charlson | (Comorbidity 1) | |||||||
| >4 | 4.1 (4.0–4.2) | index 1) | ||||||||
| High ASA score at fracture | 1.5 (1.2–1.8) | |||||||||
| Without previous hospitalization | 1.7 (1.4–2.2) | |||||||||
| With previous hospitalization | 1.7 (1.3–2.2) | |||||||||
| No. of hospitalization before | 1.4 (0.9–2.2) | |||||||||
| index date | 1 | |||||||||
| 2–5 | 1.6 (1.1 (2.4) | |||||||||
| >5 | 3.4 (1.5–7.8) | |||||||||
| Diabetes mellitus | 1.5 (1.1–2.0) | |||||||||
| COPD | 1.3 (0.9–1.7) | 1.0 (0.6–2.0) | ||||||||
| Heart failure | 1.4 (1.0–1.9) | 1.1 (0.8–1.7) | 1.9 (1.3–2.7) | 1.7 (1.2–2.3) | ||||||
| Cancer | 19 (12–31) | |||||||||
| Alcoholism | 2.2 (1.7–2.9) | 1.7 (1.7–1.8) | j 1.7 (1.3 (2.2) | |||||||
| Gastrectomy/colectomy | 2.2 (1.4–3.5) | |||||||||
| Ambulatory status | 1.3 (1.0–1.6) | n 1.7 (1.0–2.6) | l 1.4 (1.1–1.8) | 4.4 (1.3–14.4) | ||||||
| (assistive device) | o 1.7 (1.2–2.3) | 2.1 (1.6–2.8) | (limited function) | |||||||
| p 1.8 (1.1–2.9) | ||||||||||
| Mental Function | 7.0 (1.7–28) | |||||||||
| Poor mental status | (dementia) | |||||||||
| Delirium | 0.6 (0.2 1.5) | |||||||||
| Surgical and perioperative factors | ||||||||||
| High surgical volume | 1.2 (1.1 1. 3) | |||||||||
| IT fracture | 1.5 (1.1–1.9) | 1.3 (0.9–1.9)* | 1.4 (1.0–1.8)* | 2.4 (2.0–2.6) | Referent | |||||
| FN fracture | Referent | Referent | Referent | 2.2 (1.9–2.6) | 0.6 (0.3 1.3) | |||||
| Time to surgery 2 days | 1.1 (1.0 1.2) | |||||||||
| Year of fracture | 0.9 (0.9 1.0) | |||||||||
| Major postoperative | 1.9 (1.4–2.6) | 2.0 (1.1–3.6) | ||||||||
| complication | (pneumonia) | |||||||||
| Number of operations | 1 | 2.8 (2.1 3.7) | ||||||||
95% CI: 95% Confidence Interval; ASA, American Society of Anesthesiologists; COPD: chronic obstructive pulmonary disease; y: years; ns: not significant; IT: intertrochanteric fracture; FN: femoral neck fracture;
: 65–74 years old;
: 75–84 years old;
: 85 years old with <65 years old as reference;
: <70 years old;
: 70–75 years old;
: 76 years old;
: never smoked;
: former smoker;
: current smoker;
: no alcohol;
: yes alcohol;
: leisure physical activity <1 h/week;
: leisure physical activity 1 h/week;
: walk with walker;
: walk with support;
: non-ambulatory.
Acknowledgments
Dr. J.R. Curtis has received consultancy fees from Roche, UCB, Procter’ Gamble; is a member of Speakers’ Bureau on behalf of Novartis, Procter’ Gamble, Lilly, Roche, and Merck; has received research support from Novartis, Amgen, Merck, Procter’ Gamble, Lilly and Roche; and honoraria from Novartis, UCB, Amgen, Procter’ Gamble, Lilly and Roche.
Dr. K.G. Saag has received consultancy fees from Merck, Lilly, Amgen, Novartis, Roche, UCB, Procter’ Gamble; is a member of Speakers’ Bureau on behalf of Merck and Novartis has received research support from Lilly, Novartis, Amgen, Roche, and Sanofi-Aventis; and honoraria from Novartis, UCB, Amgen, Procter’ Gamble, Lilly and Roche. Dr. G.G.
Footnotes
Conflict of interest: Teng has declared no competing interests
References
- 1.Cauley JA, Wampler NS, Barnhart JM, et al. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008 doi: 10.1007/s00198-008-0634-y. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma S, Fraser M, Lovell F, Reece A, Mclellan AR. Characteristics of males over 50 years who present with a fracture: epidemiology and underlying risk factors. J Bone Joint Surg Br. 2008;90:72–77. doi: 10.1302/0301-620X.90B1.18773. [DOI] [PubMed] [Google Scholar]
- 3.Lippuner K, Golder M, Greiner R. Epidemiology and direct medical costs of osteoporotic fractures in men and women in Switzerland. Osteoporos Int. 2005;16(Suppl. 2):S8–S17. doi: 10.1007/s00198-004-1696-0. [DOI] [PubMed] [Google Scholar]
- 4.Johnell O, Kanis JA, Jonsson B, Oden A, Johansson H, De laet C. The burden of hospitalised fractures in Sweden. Osteoporos Int. 2005;16:222–228. doi: 10.1007/s00198-004-1686-2. [DOI] [PubMed] [Google Scholar]
- 5.Bone Health and Osteoporosis. A Report of the Surgeon General. [Last accessed 30 Dec 2007];2004 http://www.surgeongeneral.gov/library/bonehealth/Executive_Summary.html. [PubMed]
- 6.The American Academy of Orthopaedic Surgeons (AAOS) and the National Osteoporosis Foundation. Joint Position Statement. [accessed 30 Dec 2007];1999 http://www.aaos.org/about/papers/position/1113.asp. [Google Scholar]
- 7.International Osteoporosis Foundation Annual Report. International Osteoporosis Foundation. [Last accessed 30 Dec 2007];1999 www.iofbonehealth.org/download/osteofound/filemanager/publications/pdf/report_1999.pdf. [Google Scholar]
- 8.Browner WS, Seeley DG, Vogt TM, Cummings SR. Non-trauma mortality in elderly women with low bone mineral density. Study of Osteoporotic Fractures Research Group. Lancet. 1991;338:355–358. doi: 10.1016/0140-6736(91)90489-c. [DOI] [PubMed] [Google Scholar]
- 9.Johansson C, Black D, Johnell O, Oden A, Mellstrom D. Bone mineral density is a predictor of survival. Calcif Tissue Int. 1998;63:190–196. doi: 10.1007/s002239900513. [DOI] [PubMed] [Google Scholar]
- 10.Kado DM, Browner WS, Blackwell T, Gore R, Cummings SR. Rate of bone loss is associated with mortality in older women: a prospective study. J Bone Miner Res. 2000;15:1974–1980. doi: 10.1359/jbmr.2000.15.10.1974. [DOI] [PubMed] [Google Scholar]
- 11.Bouza C, Lopez T, Palma M, Amate JM. Hospitalised osteoporotic vertebral fractures in Spain: analysis of the national hospital discharge registry. Osteoporos Int. 2007;18:649–657. doi: 10.1007/s00198-006-0292-x. [DOI] [PubMed] [Google Scholar]
- 12.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–561. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 13.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 14.Cooper C, Atkinson EJ, Jacobsen SJ, O’fallon WM, Melton LJ., 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–1005. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 15.Ismail AA, O’neill TW, Cooper C, et al. Mortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 1998;8:291–297. doi: 10.1007/s001980050067. [DOI] [PubMed] [Google Scholar]
- 16.Jalava T, Sarna S, Pylkkanen L, et al. Association between vertebral fracture and increased mortality in osteoporotic patients. J Bone Miner Res. 2003;18:1254–1260. doi: 10.1359/jbmr.2003.18.7.1254. [DOI] [PubMed] [Google Scholar]
- 17.Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42. doi: 10.1007/s00198-003-1490-4. [DOI] [PubMed] [Google Scholar]
- 18.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 19.Kado DM, Duong T, Stone KL, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14:589–594. doi: 10.1007/s00198-003-1412-5. [DOI] [PubMed] [Google Scholar]
- 20.Kanis JA, Oden A, Johnell O, De laet C, Jonsson B. Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int. 2004;15:108–112. doi: 10.1007/s00198-003-1516-y. [DOI] [PubMed] [Google Scholar]
- 21.Naves M, Diaz-lopez JB, Gomez C, Rod-Riguez-Rebollar A, Rodriguez-Garcia M, Cannata-Andia JB. The effect of vertebral fracture as a risk factor for osteoporotic fracture and mortality in a Spanish population. Osteoporos Int. 2003;14:520–524. doi: 10.1007/s00198-003-1405-4. [DOI] [PubMed] [Google Scholar]
- 22.Trone DW, Kritz-Silverstein D, Von Muhlen DG, Wingard DL, Barrett-Con-Nor E. Is radiographic vertebral fracture a risk factor for mortality? Am J Epidemiol. 2007;166:1191–1197. doi: 10.1093/aje/kwm206. [DOI] [PubMed] [Google Scholar]
- 23.Ensrud KE, Thompson DE, Cauley JA. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc. 2000;48:241–249. doi: 10.1111/j.1532-5415.2000.tb02641.x. [DOI] [PubMed] [Google Scholar]
- 24.Alegre-Lopez J, Cordero-Guevara J, Alonso-Valdivielso JL, Fernandez-Melon J. Factors associated with mortality and functional disability after hip fracture: an inception cohort study. Osteoporos Int. 2005;16:729–736. doi: 10.1007/s00198-004-1740-0. [DOI] [PubMed] [Google Scholar]
- 25.Empana JP, Dargent-Molina P, Breart G. Effect of hip fracture on mortality in elderly women: the EPIDOS prospective study. J Am Geriatr Soc. 2004;52:685–690. doi: 10.1111/j.1532-5415.2004.52203.x. [DOI] [PubMed] [Google Scholar]
- 26.Farahmand BY, Michaelsson K, Ahl-Bom A, Ljunghall S, Baron JA. Survival after hip fracture. Osteoporos Int. 2005;16:1583–1590. doi: 10.1007/s00198-005-2024-z. [DOI] [PubMed] [Google Scholar]
- 27.Franzo A, Francescutti C, Simon G. Risk factors correlated with post-operative mortality for hip fracture surgery in the elderly: a population-based approach. Eur J Epidemiol. 2005;20:985–991. doi: 10.1007/s10654-005-4280-9. [DOI] [PubMed] [Google Scholar]
- 28.Hindmarsh DM, Hayen A, Finch CF, Close JC. Relative survival after hospitalisation for hip fracture in older people in New South Wales, Australia. Osteoporos Int. 2008 doi: 10.1007/s00198-008-0641-z. [DOI] [PubMed] [Google Scholar]
- 29.Karagiannis A, Papakitsou E, Dretakis K, et al. Mortality rates of patients with a hip fracture in a southwestern district of Greece: ten-year follow-up with reference to the type of fracture. Calcif Tissue Int. 2006;78:72–77. doi: 10.1007/s00223-005-0169-6. [DOI] [PubMed] [Google Scholar]
- 30.Lee AY, Chua BS, Howe TS. One-year outcome of hip fracture patients admitted to a Singapore hospital: quality of life post-treatment. Singapore Med J. 2007;48:996–999. [PubMed] [Google Scholar]
- 31.Muraki S, Yamamoto S, Ishibashi H, Nakamura K. Factors associated with mortality following hip fracture in Japan. J Bone Miner Metab. 2006;24:100–104. doi: 10.1007/s00774-005-0654-z. [DOI] [PubMed] [Google Scholar]
- 32.Paksima N, Koval KJ, Aharanoff G, et al. Predictors of mortality after hip fracture: a 10-year prospective study. Bull NYU Hosp Jt Dis. 2008;66:111–117. [PubMed] [Google Scholar]
- 33.Pande I, Scott DL, O’neill TW, Pritch-Ard C, Woolf AD, Davis MJ. Quality of life, morbidity, and mortality after low trauma hip fracture in men. Ann Rheum Dis. 2006;65:87–92. doi: 10.1136/ard.2004.034611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tosteson AN, Gottlieb DJ, Radley DC, Fisher ES, Melton LJ., 3rd Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18:1463–1472. doi: 10.1007/s00198-007-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vestergaard P, Rejnmark L, Mosekil-de L. Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int. 2007;18:1583–1593. doi: 10.1007/s00198-007-0403-3. [DOI] [PubMed] [Google Scholar]
- 36.Vidal EI, Coeli CM, Pinheiro RS, Camar-go KR, Jr, et al. Mortality within 1 year after hip fracture surgical repair in the elderly according to postoperative period: a probabilistic record linkage study in Brazil. Osteoporos Int. 2006;17:1569–1576. doi: 10.1007/s00198-006-0173-3. [DOI] [PubMed] [Google Scholar]
- 37.Browner WS, Pressman AR, Nevitt MC, Cummings SR. Mortality following fractures in older women. The study of osteoporotic fractures. Arch Intern Med. 1996;156:1521–1525. [PubMed] [Google Scholar]
- 38.Steinbuch M, D‘agostino RB, Mandel JS, et al. Assessment of mortality in patients enrolled in a risedronate clinical trial program: a retrospective cohort study. Regul Toxicol Pharmacol. 2002;35:320–326. doi: 10.1006/rtph.2002.1550. [DOI] [PubMed] [Google Scholar]
- 39.Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid in reducing clinical fracture and mortality after hip fracture. N Engl J Med. 2007;357 doi: 10.1056/NEJMoa074941. nihpa40967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richmond J, Aharonoff GB, Zucker-man JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17:53–56. doi: 10.1097/00005131-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Trombetti A, Herrmann F, Hoffmeyer P, Schurch MA, Bonjour JP, Rizzoli R. Survival and potential years of life lost after hip fracture in men and age-matched women. Osteoporos Int. 2002;13:731–737. doi: 10.1007/s001980200100. [DOI] [PubMed] [Google Scholar]
- 42.Calder SJ, Anderson GH, Gregg PJ. Certification of cause of death in patients dying soon after proximal femoral fracture. BMJ. 1996;312:1515. doi: 10.1136/bmj.312.7045.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10:73–78. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 44.Kanis JA, Oden A, Johnell O, De laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003;32:468–473. doi: 10.1016/s8756-3282(03)00061-9. [DOI] [PubMed] [Google Scholar]
- 45.Todd CJ, Palmer C, Camilleri-Ferran-Te C, et al. Differences in mortality after fracture of hip. BMJ. 1995;311:1025. doi: 10.1136/bmj.311.7011.1025b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897–902. doi: 10.1007/s00198-004-1627-0. [DOI] [PubMed] [Google Scholar]
- 47.Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health. 1997;87:398–403. doi: 10.2105/ajph.87.3.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fransen M, Woodward M, Norton R, Robinson E, Butler M, Campbell AJ. Excess mortality or institutionalization after hip fracture: men are at greater risk than. J Am Geriatr Soc. 2002;50:685–690. doi: 10.1046/j.1532-5415.2002.50163.x. [DOI] [PubMed] [Google Scholar]
- 49.Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82:1147–1150. doi: 10.2105/ajph.82.8.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marottoli RA, Berkman LF, Leo-Sum-Mers L, Cooney LM., Jr Predictors of mortality and institutionalization after hip fracture: the New Haven EPESE cohort. Established Populations for Epidemiologic Studies of the Elderly. Am J Public Health. 1994;84:1807–1812. doi: 10.2105/ajph.84.11.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haentjens P, Autier P, Barette M, Venken K, Vanderschueren D, Boonen S. Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone. 2007;41:958–964. doi: 10.1016/j.bone.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 52.Baudoin C, Fardellone P, Sebert JL. Effect of sex and age on the ratio of cervical to trochanteric hip fracture. A meta-analysis of 16 reports on 36,451 cases. Acta Orthop Scand. 1993;64:647–653. doi: 10.3109/17453679308994590. [DOI] [PubMed] [Google Scholar]
- 53.Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res. 2004;425:64–71. doi: 10.1097/01.blo.0000132406.37763.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Duboeuf F, Hans D, Schott AM, et al. Different morphometric and densitometric parameters predict cervical and trochanteric hip fracture: the EPIDOS Study. J Bone Miner Res. 1997;12:1895–1902. doi: 10.1359/jbmr.1997.12.11.1895. [DOI] [PubMed] [Google Scholar]
- 55.Pulkkinen P, Partanen J, Jalovaara P, Jamsa T. Combination of bone mineral density and upper femur geometry improves the prediction of hip fracture. Osteoporos Int. 2004;15:274–280. doi: 10.1007/s00198-003-1556-3. [DOI] [PubMed] [Google Scholar]
- 56.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. Bmj. 2005;331:1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003;18:2231–2237. doi: 10.1359/jbmr.2003.18.12.2231. [DOI] [PubMed] [Google Scholar]
- 58.Clague JE, Craddock E, Andrew G, Horan MA, Pendleton N. Predictors of outcome following hip fracture. Admission time predicts length of stay and in-hospital mortality. Injury. 2002;33:1–6. doi: 10.1016/s0020-1383(01)00142-5. [DOI] [PubMed] [Google Scholar]
- 59.Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006;332:947–951. doi: 10.1136/bmj.38790.468519.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Radcliff TA, Henderson WG, Stoner TJ, Khuri SF, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90:34–42. doi: 10.2106/JBJS.G.00065. [DOI] [PubMed] [Google Scholar]
- 61.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–154. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 62.Grimes JP, Gregory PM, Noveck H, But-Ler MS, Carson JL. The effects of time- to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112:702–709. doi: 10.1016/s0002-9343(02)01119-1. [DOI] [PubMed] [Google Scholar]
- 63.Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2004:CD000521. doi: 10.1002/14651858.CD000521.pub2. [DOI] [PubMed] [Google Scholar]
- 64.Southwell-Keely JP, Russo RR, March L, Cumming R, Cameron I, Brnabic AJ. Antibiotic prophylaxis in hip fracture surgery: a metaanalysis. Clin Orthop Relat Res. 2004;419:179–184. doi: 10.1097/00003086-200402000-00029. [DOI] [PubMed] [Google Scholar]
- 65.Halm EA, Wang JJ, Boockvar K, et al. Effects of blood transfusion on clinical and functional outcomes in patients with hip fracture. Transfusion. 2003;43:1358–1365. doi: 10.1046/j.1537-2995.2003.00527.x. [DOI] [PubMed] [Google Scholar]
- 66.Handoll HH, Farrar MJ, Mcbirnie J, Tytherleigh-Strong G, Milne AA, Gillespie WJ. Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database Syst Rev. 2002:CD000305. doi: 10.1002/14651858.CD000305. [DOI] [PubMed] [Google Scholar]
- 67.Grion AM, Gallo U, Bano F, et al. Difference in mortality after hip fracture is associated with postdischarge prescription of anti- thrombotic prophylaxis: a case-control study. Clin Appl Thromb Hemost. 2002;8:143–146. doi: 10.1177/107602960200800210. [DOI] [PubMed] [Google Scholar]
- 68.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 69.Hughes RG, Garnick DW, Luft HS, Mcphee SJ, Hunt SS. Hospital volume and patient outcomes. The case of hip fracture patients. Med Care. 1988;26:1057–1067. doi: 10.1097/00005650-198811000-00004. [DOI] [PubMed] [Google Scholar]
- 70.Ishida Y, Kawai S, Taguchi T. Factors affecting ambulatory status and survival of patients 90 years and older with hip fractures. Clin Orthop Relat Res. 2005;(436):208–215. doi: 10.1097/01.blo.0000159156.40002.30. [DOI] [PubMed] [Google Scholar]
- 71.Michel JP, Klopfenstein C, Hoffmeyer P, Stern R, Grab B. Hip fracture surgery: is the pre-operative American Society of Anesthesiologists (ASA) score a predictor of functional outcome? Aging Clin Exp Res. 2002;14:389–394. doi: 10.1007/BF03324467. [DOI] [PubMed] [Google Scholar]
- 72.Rantanen T, Sakari-Rantala R, Heik-Kinen E. Muscle strength before and mortality after a bone fracture in older people. Scand J Med Sci Sports. 2002;12:296–300. doi: 10.1034/j.1600-0838.2002.102100.x. [DOI] [PubMed] [Google Scholar]
- 73.Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50:1644–1650. doi: 10.1046/j.1532-5415.2002.50455.x. [DOI] [PubMed] [Google Scholar]
- 74.Beaupre LA, Cinats JG, Senthilselvan A, et al. Reduced morbidity for elderly patients with a hip fracture after implementation of a perioperative evidence-based clinical pathway. Qual Saf Health Care. 2006;15:375–379. doi: 10.1136/qshc.2005.017095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.March LM, Cameron ID, Cumming RG, et al. Mortality and morbidity after hip fracture: can evidence based clinical pathways make a difference? J Rheumatol. 2000;27:2227–2231. [PubMed] [Google Scholar]
- 76.Friedman SM, Mendelson DA, Kates SL, Mccann RM. Geriatric Co-Management of Proximal Femur Fractures: Total Quality Management and Protocol-Driven Care Result in Better Outcomes for a Frail Patient Population. J Am Geriatr Soc. 2008 doi: 10.1111/j.1532-5415.2008.01770.x. [DOI] [PubMed] [Google Scholar]
- 77.Adunsky A, Arad M, Levi R, Blankstein A, Zeilig G, Mizrachi E. Five-year experience with the ‘Sheba’ model of comprehensive orthogeriatric care for elderly hip fracture patients. Disabil Rehabil. 2005;27:1123–1127. doi: 10.1080/09638280500056030. [DOI] [PubMed] [Google Scholar]
- 78.Melton LJ, 3rd, Thamer M, Ray NF, et al. Fractures attributable to osteoporosis: report from the National Osteoporosis Foundation. J Bone Miner Res. 1997;12:16–23. doi: 10.1359/jbmr.1997.12.1.16. [DOI] [PubMed] [Google Scholar]
- 79.Kanis JA, Johnell O, Oden A, et al. Long- term risk of osteoporotic fracture in Malmö. Osteoporos Int. 2000;11:669–674. doi: 10.1007/s001980070064. [DOI] [PubMed] [Google Scholar]
- 80.Cooper C, Atkinson EJ, O’fallon WM, Melton LJ., 3rd Incidence of clinically diagnosed vertebral fractures: a population- based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res. 1992;7:221–227. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 81.Gehlbach SH, Bigelow C, Heimis-Dottir M, May S, Walker M, Kirkwood JR. Recognition of vertebral fracture in a clinical setting. Osteoporos Int. 2000;11:577–582. doi: 10.1007/s001980070078. [DOI] [PubMed] [Google Scholar]
- 82.Hasserius R, Karlsson MK, Jonsson B, Redlund-Johnell I, Johnell O. Long- term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly--a 12- and 22-year follow-up of 257 patients. Calcif Tissue Int. 2005;76:235–242. doi: 10.1007/s00223-004-2222-2. [DOI] [PubMed] [Google Scholar]
- 83.Ismail AA, Pye SR, Cockerill WC, et al. Incidence of limb fracture across Europe: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 2002;13:565–571. doi: 10.1007/s001980200074. [DOI] [PubMed] [Google Scholar]
- 84.Papaioannou A, Adachi JD, Parkinson W, Stephenson G, Bedard M. Lengthy hospitalization associated with vertebral fractures despite control for comorbid conditions. Osteoporos Int. 2001;12:870–874. doi: 10.1007/s001980170039. [DOI] [PubMed] [Google Scholar]
- 85.Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008;90:1479–1486. doi: 10.2106/JBJS.G.00675. [DOI] [PubMed] [Google Scholar]