SYNOPSIS
The term “stiff finger” refers to a reduction in the range of motion in the finger, and it is a condition that has many different causes and involves a number of different structures. Almost all injuries of the fingers and some diseases can cause finger stiffness. Hand surgeons often face difficulty treating stiff fingers that are affected by irreversible soft tissues fibrosis. Stiff fingers can be divided into flexion and extension deformities. They can also be sub-classified into four categories according to the involved tissues extending from the skin to the joint capsule. Prevention of stiff fingers by judicious mobilization of the joints is prudent to avoid more complicated treatment after established stiffness occurs. Static progressive and dynamic splints have been considered as effective non-operative interventions to treat stiff fingers. Most authors believe force of joint distraction and time duration of stretching are two important factors to consider while applying a splint or cast. We also introduce the concepts of capsulotomy and collateral ligament release and other soft tissue release of the MCP and PIP joint in this article. Future outcomes research is vital to assessing the effectiveness of these surgical procedures and guiding postoperative treatment recommendations.
Keywords: Stiffness, Finger, Contracture, Metacarpophalangeal joint, Proximal interphalangeal joint, Splint, Capsulotomy
INTRODUCTION
Motion of the finger requires bony stability, sensibility, muscle integrity, tendon gliding, and flexible joints. Full range of motion in the finger joints is the precondition of good function of the finger. The term “stiff finger” refers to a reduction in the range of motion in the finger. Almost all injuries of the fingers can cause finger stiffness, even when the joint is not directly involved in the initial injury. Furthermore, many diseases such as Dupuytren disease, 1 rheumatoid arthritis, 2, 3 gout, 4 and diabetes mellitus 5, 6 result in loss of motion of the finger. In addition, congenital stiffness of fingers without definite cause had been reported.7 Although the stiff finger has a similar clinical manifestation to joint contracture, different causative factors contribute to the stiffness. Both bone and soft tissue are what ultimately provide mechanical blocks to motion resulting in finger stiffness. For the purposes of this article, we will focus on the soft tissue etiology of the injury by reviewing the anatomy, classification, precautions, non-operative and operative intervention.
ANATOMY AND CLASSIFICATION
The anatomy of the metacarpophalangeal (MCP) joint and proximal interphalangeal (PIP) joint are complicated and intricate. The MCP and PIP joints share some structural similarities, but also have significant structural differences. 8
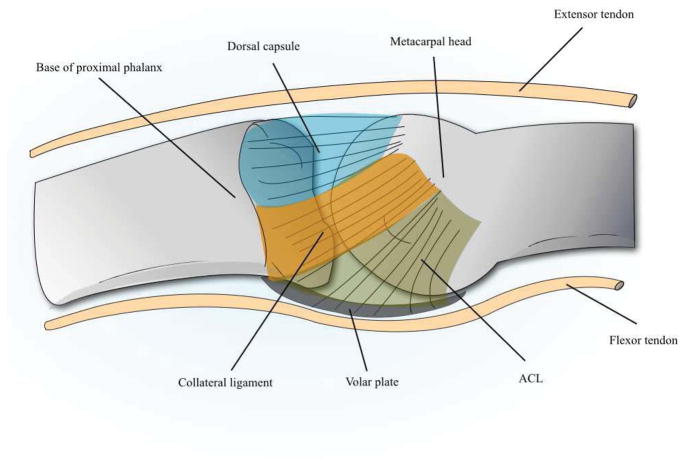
The base of the proximal phalanx and metacarpal head are the bony foundations of the MCP joint. The soft tissue boundaries of the joint are made up of the articular capsule and ligaments. The collateral ligaments originate from the tubercle of metacarpal head and run diagonally in a ladder-shape to the base of proximal phalanx. The length of collateral ligament changes as the joint flexes and extends.9 The bilateral accessory collateral ligaments (ACL) originate slightly proximal and volar to the collateral ligaments. The distal fibers of the ACL attach to the edge of volar plate and flexor sheath. The volar or palmar plate is a fibrocartilaginous structure that constitutes the base of the MCP joint (Figure 1). The extensor and flexor tendons, sagittal band, the lumbrical and interosseous muscles embrace the joint and these ligaments. The MCP joint is a condylar joint that has two axes of freedom including flexion/extension and radial/ulnar deviation. 10
Figure 1.
Anatomy of the MCP joint. The collateral ligaments arise from the metacarpal head to the base of proximal phalanx. Proximal and volar to the collateral ligament is the ACL (accessory collateral ligament). The volar plate is directly palmar to the joint.
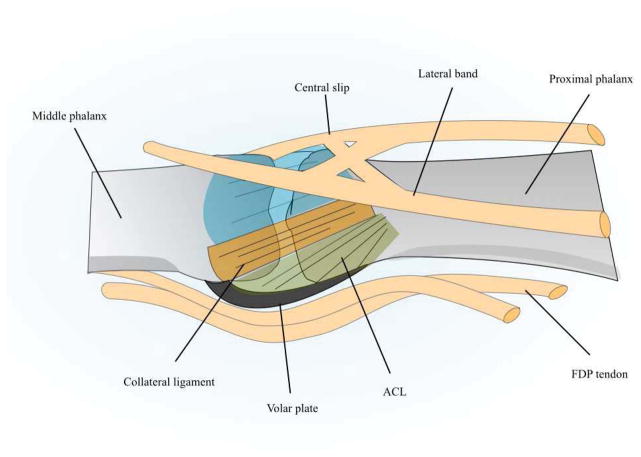
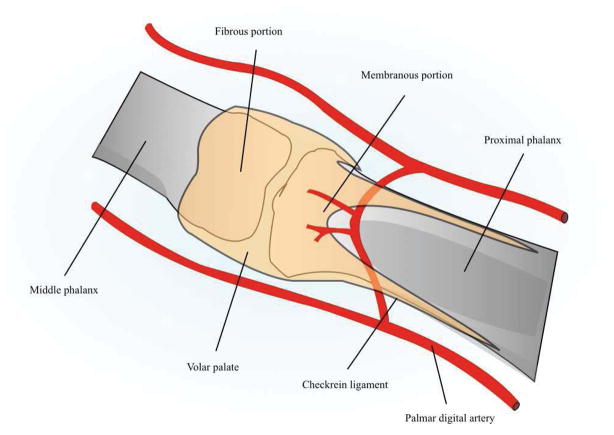
The head of the proximal phalanx and base of the middle phalanx constitute the bony structures of the PIP joint. The PIP joint is a simple hinge joint that can only move along the flexion/extension axis. 11 The origin and insertion of the collateral ligament, ACL and volar plate are similar to the MCP joint. The dorsal extensor apparatus, flexor tendons and their sheath embrace the joint (Figure 2). The tension in the collateral ligament changes very little as the PIP joint moves.12 Similar to the MCP joint, the volar plate of the PIP joint is composed of two portions: a fibrous and a membranous portion. The volar plates of PIP joints are thinner than at the MCP level for most fingers. 13 On each side of the volar plate, it is reinforced by a checkrein ligament that attaches onto the periosteum of the proximal phalanx (Figure 3). 14 The collateral ligaments and volar plate compose of a three-dimensional ligament-box complex that plays a major role in providing the stability of the PIP joint. 14
Figure 2.
Anatomy of the PIP joint. The collateral ligaments and volar plate of the PIP joint are similar to the MCP joint. The extensor apparatus and flexor tendons embrace the joint.
Figure 3.
Anatomy of volar plate of the PIP joint. The volar plate is composed of fibrous and membranous portion, and it is reinforced by two checkrein ligaments proximally.
The distal interphalangeal (DIP) joint is a hinge joint that is composed of the middle phalanx head and distal phalanx base. The DIP joint has flexion, extension and hyperextension motion. The capsule is reinforced by the collateral ligaments, volar plate, terminal extensor tendon and flexor digitorum profundus (FDP) tendon.
Stiff fingers can be categorized into flexion and extension deformities according to the fixed posture of the joint. Stiff finger deformities can also be classified into four categories according to the involved tissues: 1) Skin and fascia related problems. 2) Muscle and tendon injuries or lesions. 3) Capsule and ligament of joint contractures. 4) Damage of articular bone. We list the common causes in Table 1. It is important to note that some structures result in only one type of deformity, but others can initiate either flexion deformities or extension deformities in different conditions. For example, the collateral ligament contracture is a common reason for flexion contracture of the PIP joint, but rarely, the collateral ligament contracture may also cause an extension deformity.
TABLE 1.
Stiff finger classification
| Flexion Deformity | Extension Deformity | Operative Treatment | |
|---|---|---|---|
| Skin and fascia related problems | Skin scar or deficiency Dupuytren contracture |
Skin scar or deficiency | Scar release or skin graft Fasciectomy |
| Muscle and tendon injuries or lesions | Flexor tendon adhesion Retinacular ligament adhesion or tightness |
Extensor tendon adhesion Lateral band adhesion or tightness Intrinsic muscle contracture |
Tenolysis Adhesion release Intrinsic release |
| Capsule and ligament of joint contracture | Capsule contracture Collateral ligament and/or ACL contracture Palmar plate and/or checkrein ligament contracture |
Capsule contracture Collateral ligament contracture |
Capsulotomy Ligament release Palmar plate release and/or ligament excision |
| Damage of Articular bone | Bone block | Bone block | Arthrodesis/Arthroplasty/Joint replacement |
Information from the patient’s history may be used to discover the cause of joint stiffness. Examination of joint motion is also helpful for a surgeon to identify whether the musculotendinous structures are involved or the contracture is limited to the capsuloligamentous and articular structures. Decrease of active movement more than passive movement is more likely to be caused by a musculotendinous problem. However, when active and passive motion are limited to the same degree, joint contracture or bone block are likely causes. Knowledge of the specific patterns of joint deformities (e.g. boutonniere deformity, mallet deformity, swan-neck deformity) can also be helpful to identify the cause of the stiff finger. Nevertheless, it may be difficult to determine precisely which structures are involved in some complicated cases.
PRECAUTION
As discussed above, the stiff finger is a challenge to treat for many reasons. Notably, stiff fingers may occur in fingers that are not directly injured. For example, an avulsed index finger may result in a stiff small finger if the small finger is not considered during therapy.15 Prevention of a stiff finger is based on the principle of early joint motion. Therefore, treatment of original diseases and injuries of hands should reduce the duration of immobilization so that finger stiffness can be prevented. Minimizing bleeding, pain and edema can reduce the inflammation response after injury or operation, which in turn permits hand motion earlier and prevents finger stiffness from developing.
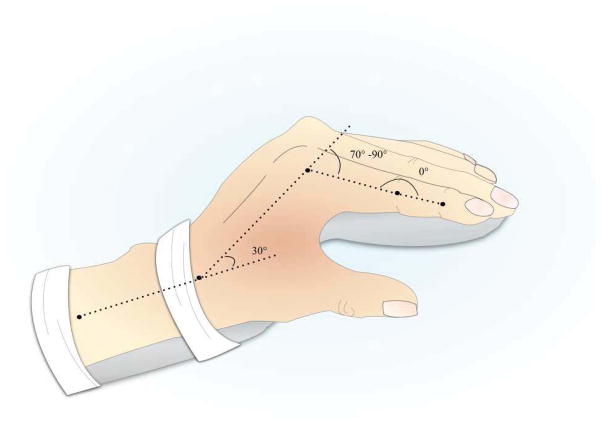
To thwart fingers stiffness, the recommended position of immobilization of the hand for any reason is the “safe position.” In the safe position, the wrist is in 30° of extension, the MCP joint is in 70° to 90° flexion position, and the PIP joint is in full extension (Figure 4). The opposed position of the MCP and PIP joints can make most portions of the collateral ligament of the MCP lengthened and the volar plate of the PIP joint straightened to minimize the contracture. Furthermore, the PIP joint should be immobilized in extension. This is because it is easier to restore flexion than extension after a PIP joint contracture.16
Figure 4.
Safe position of the hand. The wrist is in 30° of extension, the MCP joint is in 70° to 90° flexion position, and the PIP joint is in full extension.
NON-OPERATIVE INTERVENTION
The goals in treating the stiff finger are to provide patients with a pain-free, movable and stable joint. Non-operative interventions can be effective for most patients who have lost motion. In a large trial study, Weeks reported that 87% stiff joints responded sufficiently to exercise and dynamic splinting so that surgeries were not required. 17
Some authors believe that patients should accept a certain program of non-operative therapy before operative intervention is considered.11, 18–20 Curtis concluded that if the PIP joint passively flexes to 75 °, then patients should undergo physical therapy and splinting to achieve additional flexion rather than operative intervention.21
Non-operative treatment for stiff fingers includes exercise, joint mobilization, continuous passive motion, casting and splinting. Joint motion loss occurs because the ligaments and capsule of the stiff joint have shortened. Splints are applied to provide stress to stimulate the shortened soft tissues to “grow”, hence improving the passive range of motion.22, 23
Various splints are applied in treating hand disease and injuries, and some are designed to position the MCP or IP joints in their available end range position.24–29 These splints can be classified into static, serial static, static progressive or dynamic splints. Static progressive and dynamic splints have both been widely used in recent years. Dynamic splinting applies a passive constant force to maintain the stiff joint in a lengthened position using energy-storing or elastic materials.30 Static progressive splinting concentrates a force to the stiff joint in order to statically position at the maximal stretch, using inelastic components.31 Static progressive splints require adjustment of the inelastic components as the range of joint motion improves. Although these two types of splints are different in principle, the current literature suggests that both are effective to treat the stiff finger. 32, 33
Force of joint distraction and time duration of stretching are two important parameters in applying a splint or cast. Flowers introduced his guidelines about how to choose the splint parameters according to the level of joint stiffness.34 However, the objective recommended force ranges for splinting to a stiff finger remain unknown. The soft tissues of finger joints have visco-elastic behaviors, and excessive force will cause tissue inflammatory response. Overload will cause extreme discomfort, pain, and edema due to tissue tearing and dislocation. Consequently, the range of motion should be applied with a low load within tissue tolerance.35
Because force is limited to a low level, treatment may be improved by adjusting the time spent in the splint. Some authors agreed that improvement in passive range of motion of a stiff joint was proportional to the time spent in a splint. In 1994, Flowers and LaStayo studied the outcomes of fifteen patients with 20 PIP flexion contractures.36 Patients were randomly assigned to one of two groups. All subjects were originally placed in the casts with the finger positioned at target end-range. The researchers measured passive range of motion for group A at 6 days, and passive range of motion of Group B at 3 days. The results showed that the passive range of motion gained during 6 days was almost twice as much as in 3 days for all subjects. These results were supported by a study by Prosser who investigated the outcome of 20 patients with PIP flexion contracture treated with splinting. 32 Similar to Flower and LaStayo’s study, the statistical analysis showed that the time spent in a splint was also proportional to the final extension angle.
In 2003, Glasgow conducted a prospective study of patients with hand joint contractures.37 One group used splinting for less than 6 hours per day, and the other group used splint for 6 to 12 hours per day. Analysis showed a statistically significant motion gain for the group with the longer daily total end-range time. However, when comparing the effect of daily splint total end-range time of 6 to 12 hours with 12 to 16 hours, Glasgow found there was no significant difference in extension range of motion between these two groups. It was also noted that most patients have difficulty wearing splints more than 12 hours.38
To explore the long-term relationship between the duration of treatment using dynamic splints and contracture resolution in stiff PIP joints, Glasgow studied forty-one participants with the PIP joint contracture treated with a dynamic splint for 12 weeks. She drew a conclusion that the number of weeks of treatment is also significantly associated with the extent of contracture resolution. 16
OPERATIVE INTERVENTION
There is no evidence available for when conservative treatment should cease before considering operative intervention. However, it seems surgeons agree that surgery should be considered when a patient does not respond to a period of non-operative treatment. Surgeons and their patients should comprehend the following points before they decide to undergo surgery to improve the motion of a finger. First, treatment of the stiff finger must be comprehensive and operative intervention is only one of the stages in a long treatment process. The thought that the stiffness can be resolved by one surgery is not realistic. Second, although operative management can achieve improvement for stiff joints, the operation damages the structures of the finger at the same time. Therefore, a lack of preoperative evaluation, surgical technique, post-operative exercise and patient cooperation, may result in a poor outcome.
MCP Joint Extension Contracture
Weeks studied the effectiveness and merits of the dorsal and volar approaches for release of the MCP joint contracture. 39 In the study, forty-four percent of joints treated with the volar approach gained greater than 50 degrees of active and passive motion postoperatively. Only 16% in the dorsal approach gained greater than 50 degrees. He concluded that the volar approach compared favorably to the dorsal approach. Despite this finding, many authors still prefer a dorsal approach to the MCP joint because this approach is direct and provides adequate exposure of the joint. 40–42
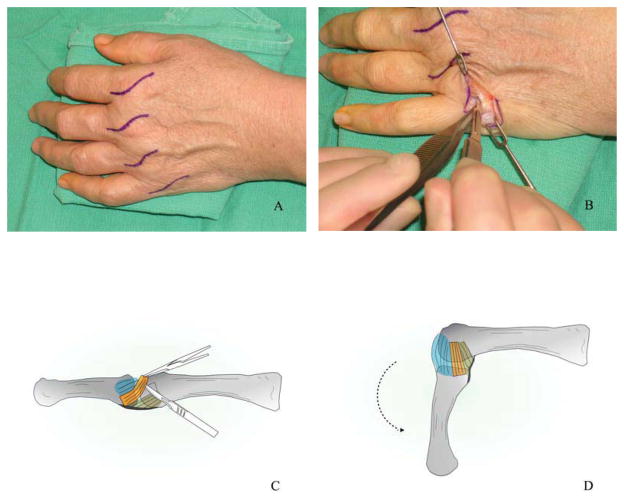
Our preferred procedure is similar to Buch40 and Shin’s41. We select a dorsal curvilinear incision over the MCP joint and a portion of the sagittal band is then incised on both sides of the extensor tendon to expose the MCP joint. After exposing the joint, the dorsal capsule excision or incision is performed. If it is not enough, we divide the dorsal collateral ligaments from the origin on the metacarpal head. MCP joint flexion during the operation can help to identify the tight collateral ligaments (Figure 5). If the joint cannot flex to 60 degrees, it shows that some part of the collateral ligaments still remains or the volar plate has adhered to the capsule. The adhesions between the volar plate and the capsule are usually released by an elevator. Finally, we test the passive motion or active motion of the joint to check if there are any structures that block the joint flexor. The patient is placed in a soft dressing after the operation, then aggressive active and passive range of motion exercises are begun.
Figure 5.
The MCP extension contracture release. (A) Dorsal curvilinear incisions over the MCP joint were made. (B) We excised the dorsal capsule of the joint. (C) If joint passive flexion was not enough after the dorsal capsule excised, we divided the collateral ligament from the origin on the metacarpal head. (D) The MCP joint flexion can help to identify the tight collateral ligament.
The patient can regain functional motion of the MCP joint after surgical release. 18, 40, 42 In a study conducted by Gould and his colleagues, 100 MCP joint capsulotomies were performed in 35 patients who had MCP joint extension contracture after conservative methods failed. 42 Alomost all patients could regain passive flexion of 90° at the operation table. Ultimately, the stiff MCP joints achieved an average gain of 21°of active motion and 29° of passive motion at follow-up after 3 to 32 months. In 1974, Buch carried out the MCP capsulotomy procedure in 27 hands with hyperextension deformity.40 The joints were mobilized at 5 to 7 days after surgery and kept in flexion position by splints at night. All fingers gained at least 30° of flexion at follow-up. In addition, Buch suggested early intensive physiotherapy was a key point in postoperative management.
PIP Joint Contracture
Flexion contracture
There are two approaches and several incisions to choose to release the PIP joint contracture. Brüser retrospectively reviewed 42 patients (45 fingers) with flexion contractures of the PIP joint who were treated with operative release. 43 He compared two patient groups after the PIP joint release with either mid-lateral or palmar approach using a Z or Y-V incision. The median arc of motion improved from 30° to 60° in the palmar incision group and from 40° to 90° in the mid-lateral incision group at 1.5 to 3-year postoperative review. Brüser discussed that better improvement in the mid-lateral incision group was because the mid-lateral incision enable early mobilization and dynamic splinting before wound healing.
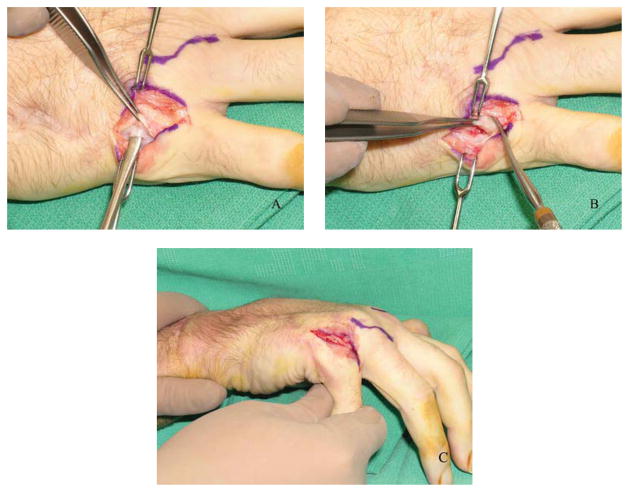
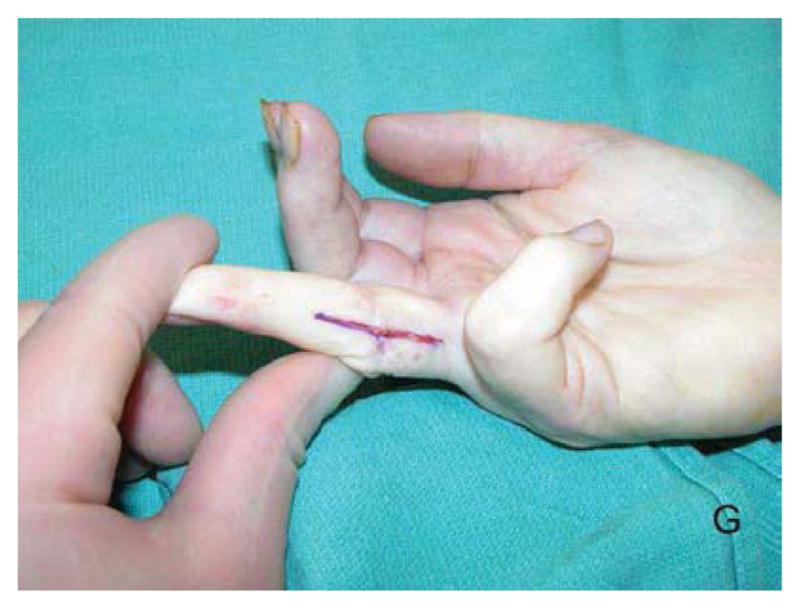
The anatomical structures that may be involved in flexion contractures include the collateral ligament, ACL, the volar plate, retinacular ligament and the flexor tendon. For this deformity, we carry out contracture release through a mid-axial incision on either or both sides of the finger. The neurovascular bundles with the skin flap are elevated and the A3 pulley is incised. The flexor tendon is then retracted volarly and a 15-blade is used to make an incision over the attachment of the volar plate at the head of the proximal phalanx. A portion of the volar collateral ligaments is incised. Then the volar plate is subperiosteally dissected to the joint space (Figure 6). The ACLs are released if required. Tenolysis should be performed if the joint is tethered by the flexor digitorum superficialis tendon. The patient should begin performing aggressive range of motion exercises within 48 hours after surgery.
Figure 6.
The MCP joint extension contracture release in another patient. (A) We incised the portion of the sagittal band to expose the dorsal capsule. (B) The dorsal capsule was excised. (C) The MCP joint can be passive flexed to 90 degree after release.
Abbiati reported the results of 19 patients with chronic flexion contractures treated by surgical release, using a mid-lateral approach, involving incision of the collateral ligament, and excision of the volar plate and checkrein ligaments. 44 The patients had static and/or dynamic splints after surgical release. More than 50% of patients achieved complete extension of the finger without severe complications. Open release does not always provide a good result; on the contrary, some results are disappointing by this method. Ghidella retrospectively reviewed the results of surgical treatment of 49 PIP joint flexion contractures with a minimum follow-up period of 24 months. 45 The average improvement was 5.8° and 31% of the joints needed to have repeat release and salvage because of inadequate gain of motion or loss of motion.
Percutaneous ACL release is a less aggressive alternative method to treat the PIP joint flexion contracture. Stanley introduced this method in 1985. 46 He divided the ACL through two small incisions on the dorsal aspect of the joint by a blade. In 2009, Cerovac and Stanley reported an average of 34 months (range 4–120 months) follow-up results for this method in 30 joints.47 The range of PIP joint motion improved from 16.5° to 38.6° in 15 joints with osteoarthritis or immobilized joints, but the flexion deformity in 10 joints with rheumatoid arthritis deteriorated. Although percutaneous release alone can yield favorable outcomes, the authors agreed that the stiff joint that had no previous surgery and was initiated by capsuloligamentous disease is a good candidate for this method.
In recent years, external fixators have been used to correct flexion contracture of the PIP joint. 48–50 The metal frames are fixated to the proximal and middle phalanges. A constant distractive force is applied, which gradually straightens the joint contracture. In Houshian’s study, the fixators were removed at least one week after a 4 to 5-mm joint opening or full extension of the PIP joint was achieved. 48,49 In 2013, he reported the medium to long-term results using a mini-external fixator for chronic flexion deformity of the PIP joint from trauma. 49 He found that the mean gain in the active range of movement was 67° at a mean 54 months’ fellow-up without complications. He also compared the results from patients younger than 40 years to patients 40 years old or older, and found that there was no age-related difference in outcome. In Ghidella’s study, the patients older than 43 years who had open release of the PIP joints often achieved poor outcomes.45 Houshian believed this maybe because the open surgery caused more damage than the external fixator. 49
Extension contracture
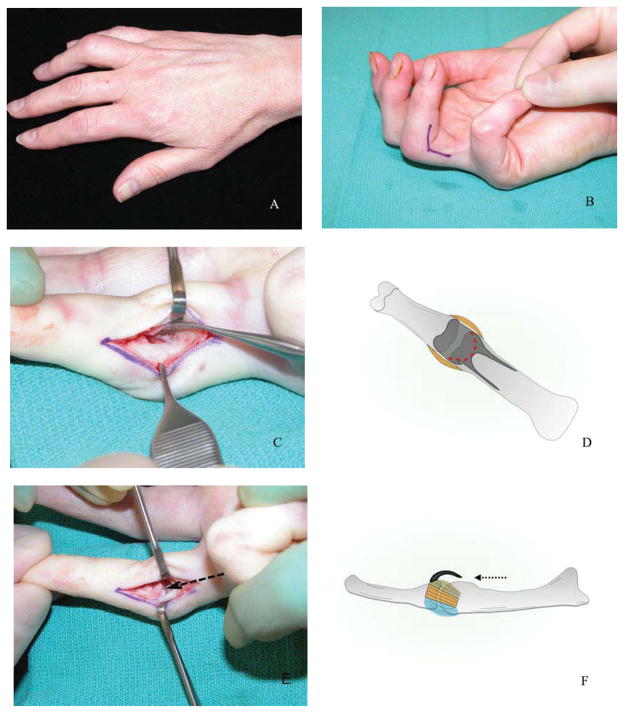
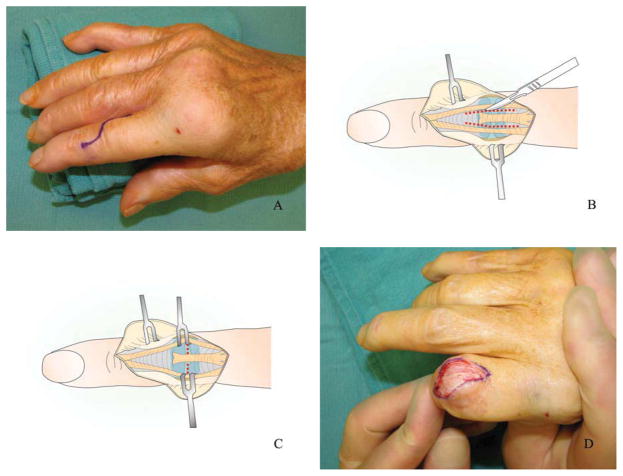
For the open surgical release of PIP extension contracture, a curvilinear incision over the dorsum of the PIP joint is performed. If there is extensor tendon adhesion to the skin or phalanx, tenolysis is performed first. The intervals between the central tendon and the lateral band are incised at the level of the PIP joint. The extensor tendon is then elevated and the central slip is preserved. The dorsal capsular incision or excision is made over the PIP joint including the collateral ligament dorsally (Figure 7). The whole collateral ligament is excised if the arc of flexion is not sufficient. Excising the whole collateral ligament will not affect the stability of the PIP joint. 51
Figure 7.
The PIP joint flexion contracture release. (A) The PIP joint flexion contraction of the ring finger. (B) A mid-lateral incision was made on the ulnar border of the ring finger. (C) The A3 pulley was incised and we retracted the flexor tendon to explore the PIP joint. (D) An incision in periosteal attachments of the volar plate was performed. (E,F) The volar plate (arrow) was subperiosteally dissected to the joint space. (G) A passive extension of the finger was able to bring the finger in a full-extended posture.
One cause of the PIP joint extension deformity is adhesion between the lateral bands and dorsal capsule or the central band. In 1968, Egawa and his colleagues first introduced a technique of lateral band release to correct post-traumatic extension contracture of the PIP joint.52 The parallel incisions 5 mm in width are made on the extensor apparatus between the lateral bands and the central band over the PIP joint to release the adhesion (Figure 8). The joints are allowed to flex actively postoperatively, and aggressive flexion exercises are performed at 2 weeks following release. Inoue in 1991 reported the outcome of this technique in 10 patients with post-traumatic extension contracture of the PIP joint. 53 At 6 to 36 months postoperatively, the patients gained an average of 56.2° of flexion motion and lost an average of 8.7° of extension. He believed the lateral band release should be considered first to treat the PIP joint extension contracture caused by extensor tendon adhesion or the interosseous muscle contracture. (Figure 8)
Figure 8.
The PIP joint extension contracture release. (A) A curvilinear incision was made over the dorsal PIP joint. (B, C) The lateral band was released and then the dorsal capsule was incised. (D) The PIP joint was able to flex to about 90 degree after release.
DIP joint Contracture
Stiffness or contracture of the DIP joint has less of an impact on the motion of the finger. It is seldom required to treat a simple joint contracture in extension. DIP joint contracture resulting from a swan neck or boutonniere deformity must be treated as a part of these deformities. A long time deformity fixed in flexion position due to chronic mallet deformities or chronic rupture of the lateral extensor can be managed by arthrodesis.
Summary
The term “stiff finger” refers to a reduction in the range of motion in the finger, and it is a condition that has many different causes and involves a number of different structures. Almost all injuries of the fingers and some diseases can cause finger stiffness. Hand surgeons often face difficulty treating stiff fingers that are affected by irreversible soft tissues fibrosis. Stiff fingers can be divided into flexion and extension deformities. They can also be sub-classified into four categories according to the involved tissues extending from the skin to the joint capsule. Prevention of stiff fingers by judicious mobilization of the joints is prudent to avoid more complicated treatment after established stiffness occurs. Static progressive and dynamic splints have been considered as effective non-operative interventions to treat stiff fingers. Most authors believe force of joint distraction and time duration of stretching are two important factors to consider while applying a splint or cast. We also introduce the concepts of capsulotomy and collateral ligament release and other soft tissue release of the MCP and PIP joint in this article. Future outcomes research is vital to assessing the effectiveness of these surgical procedures and guiding postoperative treatment recommendations.
KEY POINTS.
The stiff finger is a challenge to treat because it has many different causes and involves a number of different structures. It is important to prevent this injury.
Static progressive and dynamic splints have been proven effective as non-operative interventions to treat the stiff finger.
Operative intervention can be considered when a patient does not respond to a period of non-operative treatment.
Capsulotomy, collateral ligament and volar plate releases are the basic surgical techniques to treat MCP and PIP joint contracture.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Davis TR. Surgical treatment of primary Dupuytren’s contractures of the fingers in the UK: surgeons’ preferences and research priorities. J Hand Surg Eur Vol. 2013;38:83–5. doi: 10.1177/1753193412467170. [DOI] [PubMed] [Google Scholar]
- 2.Scott FA, Boswick JA., Jr Palmar arthroplasty for the treatment of the stiff swan-neck deformity. J Hand Surg Am. 1983;8:267–72. doi: 10.1016/s0363-5023(83)80156-7. [DOI] [PubMed] [Google Scholar]
- 3.Rizio L, Belsky MR. Finger deformities in rheumatoid arthritis. Hand Clin. 1996;12:531–40. [PubMed] [Google Scholar]
- 4.Hernández-Cortés P, Caba M, Gómez-Sánchez R, et al. Digital flexion contracture and severe carpal tunnel syndrome due to tophaceus infiltration of wrist flexor tendon: first manifestation of gout. Orthopedics. 2011;34:e797–9. doi: 10.3928/01477447-20110922-36. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbloom AL. Limitation of finger joint mobility in diabetes mellitus. J Diabet Complications. 1989;3:77–87. doi: 10.1016/0891-6632(89)90016-0. [DOI] [PubMed] [Google Scholar]
- 6.Abate M, Schiavone C, Salini V, et al. Management of limited joint mobility in diabetic patients. Diabetes Metab Syndr Obes. 2013;6:197–207. doi: 10.2147/DMSO.S33943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsujii M, Hirata H, Matsumoto M, et al. Surgical treatment for a congenitally stiff metacarpophalangeal joint of the small finger: report of four cases. J Hand Surg Am. 2006;31:1189–92. doi: 10.1016/j.jhsa.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Kuczynski K. The proximal interphalangeal joint. Anatomy and causes of stiffness in the fingers. J Bone Joint Surg Br. 1968;50:656–63. [PubMed] [Google Scholar]
- 9.Minami A, An KN, Cooney WP, 3rd, et al. Ligamentous structures of the metacarpophalangeal joint: a quantitative anatomic study. J Orthop Res. 1984;1:361–8. doi: 10.1002/jor.1100010404. [DOI] [PubMed] [Google Scholar]
- 10.Schultz RJ, Storace A, Krishnamurthy S. Metacarpophalangeal joint motion and the role of the collateral ligaments. Int Orthop. 1987;11:149–55. doi: 10.1007/BF00266701. [DOI] [PubMed] [Google Scholar]
- 11.Harrison DH. The stiff proximal interphalangeal joint. Hand. 1977;9:102–8. doi: 10.1016/s0072-968x(77)80002-8. [DOI] [PubMed] [Google Scholar]
- 12.Loubert PV, Masterson TJ, Schroeder MS, et al. Proximity of collateral ligament origin to the axis of rotation of the proximal interphalangeal joint of the finger. J Orthop Sports Phys Ther. 2007;37:179–85. doi: 10.2519/jospt.2007.2476. [DOI] [PubMed] [Google Scholar]
- 13.Kömürcü M, Kirici Y, Korkmaz C, et al. Morphometric analysis of metacarpophalangeal and proximal interphalangeal palmar plates. Clin Anat. 2008;21:433–8. doi: 10.1002/ca.20631. [DOI] [PubMed] [Google Scholar]
- 14.Lee SW, Ng ZY, Fogg QA. Three-dimensional analysis of the palmar plate and collateral ligaments at the proximal interphalangeal joint. J Hand Surg Eur Vol. 2014;39:391–7. doi: 10.1177/1753193413492288. [DOI] [PubMed] [Google Scholar]
- 15.Merritt WH. Written on behalf of the stiff finger. J Hand Ther. 1998;11:74–9. doi: 10.1016/s0894-1130(98)80003-3. [DOI] [PubMed] [Google Scholar]
- 16.Glasgow C, Fleming J, Tooth LR, et al. The Long-term relationship between duration of treatment and contracture resolution using dynamic orthotic devices for the stiff proximal interphalangeal joint: a prospective cohort study. J Hand Ther. 2012;25:38–46. doi: 10.1016/j.jht.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Weeks PM, Wray RC, Jr, Kuxhaus M. The results of non-operative management of stiff joints in the hand. Plast Reconstr Surg. 1978;61:58–63. doi: 10.1097/00006534-197801000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Young VL, Wray RC, Jr, Weeks PM. The surgical management of stiff joints in the hand. Plast Reconstr Surg. 1978;62:835–41. doi: 10.1097/00006534-197812000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Tang JB. The stiff hand. In: Gu YD, Wang SH, Si D, editors. Operative hand surgery. 2. Beijing: People’s Medical Publishing House; 2010. pp. 564–73. [Google Scholar]
- 20.Houshian S, Jing SS, Chikkamuniyappa C, et al. Management of posttraumatic proximal interphalangeal joint contracture. J Hand Surg Am. 2013;38:1651–8. doi: 10.1016/j.jhsa.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Curtis RM. Management of the stiff proximal interphalangeal joint. Hand. 1969;1:32–37. [Google Scholar]
- 22.Brand PW. Mechanical factors in joint stiffness and tissue growth. J Hand Ther. 1995;8:91–6. doi: 10.1016/s0894-1130(12)80305-x. [DOI] [PubMed] [Google Scholar]
- 23.Flowers KR. Reflections on mobilizing the stiff hand. J Hand Ther. 2010;23:402–3. doi: 10.1016/j.jht.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 24.Callahan AD, McEntee P. Splinting proximal interphalangeal joint flexion contractures: a new design. Am J Occup Ther. 1986;40:408–13. doi: 10.5014/ajot.40.6.408. [DOI] [PubMed] [Google Scholar]
- 25.Wu SH. A belly gutter splint for proximal interphalangeal joint flexion contracture. Am J Occup Ther. 1991;45:839–43. doi: 10.5014/ajot.45.9.839. [DOI] [PubMed] [Google Scholar]
- 26.Schwartz DA, Janssen RG. Static progressive splint for composite flexion. J Hand Ther. 2005;18:447–9. doi: 10.1197/j.jht.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 27.Boccolari P, Tocco S. Alternative splinting approach for proximal interphalangeal joint flexion contractures: no-profile static-progressive splinting and cylinder splint combo. J Hand Ther. 2009;22:288–93. doi: 10.1016/j.jht.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 28.Wang J, Erlandsson G, Rui Yj, et al. Composite flexion splint for the stiff hand. J Hand Ther. 2011;24:66–8. doi: 10.1016/j.jht.2010.09.068. [DOI] [PubMed] [Google Scholar]
- 29.Harte D, Porter-Armstrong A. Managing the stiff hand: dual orthosis innovation. J Hand Ther. 2012;25:342–4. doi: 10.1016/j.jht.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Glasgow C, Tooth LR, Fleming J, et al. Dynamic splinting for the stiff hand after trauma: predictors of contracture resolution. J Hand Ther. 2011;24:195–205. doi: 10.1016/j.jht.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 31.Schultz-Johnson K. Static progressive splinting. J Hand Ther. 2002;15:163–78. doi: 10.1053/hanthe.2002.v15.015016. [DOI] [PubMed] [Google Scholar]
- 32.Prosser R. Splinting in the management of proximal interphalangeal joint flexion contracture. J Hand Ther. 1996;9:378–86. doi: 10.1016/s0894-1130(96)80045-7. [DOI] [PubMed] [Google Scholar]
- 33.Michlovitz SL, Harris BA, Watkins MP. Therapy interventions for improving joint range of motion: A systematic review. J Hand Ther. 17:118–31. doi: 10.1197/j.jht.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 34.Flowers KR. A proposed decision hierarchy for splinting the stiff joint, with an emphasis on force application parameters. J Hand Ther. 2002;15:158–62. doi: 10.1053/hanthe.2002.v15.015015. [DOI] [PubMed] [Google Scholar]
- 35.Fess EE, McCollum M. The influence of splinting on healing tissues. J Hand Ther. 1998;11:157–61. doi: 10.1016/s0894-1130(98)80014-8. [DOI] [PubMed] [Google Scholar]
- 36.Flowers KR, LaStayo PC. Effect of total end range time on improving passive range of motion. J Hand Ther. 1994;7:150–7. doi: 10.1016/s0894-1130(12)80056-1. [DOI] [PubMed] [Google Scholar]
- 37.Glasgow C, Wilton J, Tooth L, et al. Optimal daily total end range time for contracture: resolution in hand splinting. J Hand Ther. 2003;16:207–18. doi: 10.1016/s0894-1130(03)00036-x. [DOI] [PubMed] [Google Scholar]
- 38.Glasgow C, Fleming J, Tooth LR, et al. Randomized controlled trial of daily total end range time (TERT) for Capener splinting of the stiff proximal interphalangeal joint. Am J Occup Ther. 2012;66:243–8. doi: 10.5014/ajot.2012.002816. [DOI] [PubMed] [Google Scholar]
- 39.Weeks PM, Young VL, Wray RC, Jr, et al. Operative mobilization of stiff metacarpophalangeal joints: dorsal versus volar approach. Ann Plast Surg. 1980;5:178–85. doi: 10.1097/00000637-198009000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Buch VI. Clinical and functional assessment of the hand after metacarpophalangeal capsulotomy. Plast Reconstr Surg. 1974;53:452–7. doi: 10.1097/00006534-197404000-00013. [DOI] [PubMed] [Google Scholar]
- 41.Shin AY, Amadio PC. The stiff finger. In: Wolfe SW, Hotchkiss RN, Pederson WC, et al., editors. Green’s operative hand surgery. 6. Philadelphia: Elsevier/Churchil Livingstone; 2011. pp. 355–89. [Google Scholar]
- 42.Gould JS, Nicholson BG. Capsulectomy of the metacarpophalangeal and proximal interphalangeal joints. J Hand Surg Am. 1979;4:482–6. doi: 10.1016/s0363-5023(79)80048-9. [DOI] [PubMed] [Google Scholar]
- 43.Brüser P, Poss T, Larkin G. Results of proximal interphalangeal joint release for flexion contractures: midlateral versus palmar incision. J Hand Surg Am. 1999;24:288–94. doi: 10.1053/jhsu.1999.0288. [DOI] [PubMed] [Google Scholar]
- 44.Abbiati G, Delaria G, Saporiti E, et al. The treatment of chronic flexion contractures of the proximal interphalangeal joint. J Hand Surg Br. 1995;20:385–9. doi: 10.1016/s0266-7681(05)80099-3. [DOI] [PubMed] [Google Scholar]
- 45.Ghidella SD, Segalman KA, Murphey MS. Long-term results of surgical management of proximal interphalangeal joint contracture. J Hand Surg Am. 2002;27:799–805. doi: 10.1053/jhsu.2002.35303. [DOI] [PubMed] [Google Scholar]
- 46.Stanley JK, Jones WA, Lynch MC. Percutaneous accessory collateral ligament release in the treatment of proximal interphalangeal joint flexion contracture. J Hand Surg Br. 1986;11:360–3. doi: 10.1016/0266-7681(86)90158-0. [DOI] [PubMed] [Google Scholar]
- 47.Cerovac S, Stanley J. Outcome review on the percutaneous release of the proximal interphalangeal joint accessory collateral ligaments. Orthop Rev (Pavia) 2009;1:e19. doi: 10.4081/or.2009.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Houshian S, Chikkamuniyappa C, Schroeder H. Gradual joint distraction of post-traumatic flexion contracture of the proximal interphalangeal joint by a mini-external fixator. J Bone Joint Surg Br. 2007;89:206–9. doi: 10.1302/0301-620X.89B2.18448. [DOI] [PubMed] [Google Scholar]
- 49.Houshian S, Jing SS, Kazemian GH, et al. Distraction for Proximal interphalangeal Joint Contractures: Long-Term Results. J Hand Surg Am. 2013;38:1951–6. doi: 10.1016/j.jhsa.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 50.Houshian S, Chikkamuniyappa C. Distraction correction of chronic flexion contractures of PIP joint: comparison between two distraction rates. J Hand Surg Am. 2007;32:651–6. doi: 10.1016/j.jhsa.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 51.Diao E, Eaton RG. Total collateral ligament excision for contractures of the proximal interphalangeal joint. J Hand Surg Am. 1993;18:395–402. doi: 10.1016/0363-5023(93)90081-D. [DOI] [PubMed] [Google Scholar]
- 52.Egawa T, Doi T, Iwasaki N, et al. Lateral band release for post-traumatic extension contracture of the PIP joint. Seikeigeka (Orthop Surg) 1968;19:1076–8. [Google Scholar]
- 53.Inoue G. Lateral band release for post-traumatic extension contracture of the proximal interphalangeal joint. Arch Orthop Trauma Surg. 1991;110:298–300. doi: 10.1007/BF00443462. [DOI] [PubMed] [Google Scholar]