Abstract
Current therapies for Parkinson's disease (PD) offer symptomatic relief but do not provide a cure or slow the disease process. Treatments that could halt progression of the disease or help restore function to damaged neurons would be of substantial benefit. Calcitriol, the active metabolite of vitamin D, has been shown to have significant effects on the brain. These effects include upregulating trophic factor levels, and reducing the severity of some central nervous system lesions. While previous studies have shown that calcitriol can be neuroprotective in 6-hydroxydopamine (6-OHDA) rodent models of PD, the present experiments were designed to examine the ability of calcitriol to promote restoration of extracellular DA levels and tissue content of DA in animals previously lesioned with 6-OHDA. Male Fischer-344 rats were given a single injection of 12 µg 6-OHDA into the right striatum. Four weeks later the animals were administered vehicle or calcitriol (0.3 or 1.0 µg/kg, s.c.) once a day for eight consecutive days. Three weeks after the calcitriol treatments in vivo microdialysis experiments were conducted to measure potassium and amphetamine evoked overflow of DA from both the left and right striata. In control animals treated with 6-OHDA and vehicle there were significant reductions in both potassium and amphetamine evoked overflow of DA on the lesioned side of the brain compared to the contralateral side. In animals treated with 6-OHDA followed by calcitriol there was significantly greater potassium and amphetamine evoked overflow of DA from the lesioned striatum compared to that from the control animals. The calcitriol treatments also led to increases in postmortem tissue levels of DA in the striatum and substantia nigra. These results suggest that calcitriol may help promote recovery of dopaminergic functioning in injured nigrostriatal neurons.
Keywords: Striatum, Substantia Nigra, Dopamine, Calcitriol, 6-OHDA, GDNF
Introduction
Parkinson's disease (PD) is a debilitating neurodegenerative disorder that affects over one million people in the United States. The primary motor symptoms of PD, resting tremor, bradykinesia, rigidity and postural instability, are likely due in part to a progressive degeneration of substantia nigra dopamine (DA) neurons with a concomitant loss of DA in the striatum. Current therapies for PD offer symptomatic relief but do not provide a cure or slow the disease process. Thus, treatments that could halt progression of the disease or even restore function to damaged nigrostriatal DA neurons would be of substantial benefit.
Calcitriol (1,25-dihydroxyvitamin D3), the active metabolite of vitamin D3, has well documented roles in bone metabolism and calcium homeostasis and is currently used to treat several conditions including hypocalcemia and hypoparathyroidism. Calcitriol has also been shown to have several effects in the nervous system [1–3], including the modulation of trophic factors [4–7]. The receptor for calcitriol belongs to the steroid receptor superfamily and it is localized throughout the brain, including the striatum [8–10]. In addition, circulating calcitriol can cross the blood brain barrier to a limited extent [11, 12], and the brain itself may be able to synthesize calcitriol [10, 13]. Together these studies suggest that calcitriol has a role in central nervous system function.
One of the trophic factors that is regulated by calcitriol is glial cell line-derived neurotrophic factor (GDNF). Calcitriol has been shown to increase expression or release of GDNF in various cell lines [14–16] and in vivo administration has been shown to increase expression and protein levels of GDNF in the brain [17–20]. GDNF has potent effects on brain DA systems, and because of this it has been examined in several animal models of PD where it was shown to have neuroprotective or restorative effects [21–25]. The success of GDNF in animal models led to the clinical evaluation of exogenous GDNF in PD patients as a potential therapeutic agent. While there was some success in early open-label trials [26, 27], later results from a larger controlled trial were disappointing due to a lack of significant clinical benefits [28].
The 6-hydroxydopamine (6-OHDA) rodent model of PD has been used extensively for examining potential therapies for PD. Previous studies have demonstrated that calcitriol can partially protect against the histological, neurochemical and behavioral effects of 6-OHDA [19, 29–31], and one study has reported that calcitriol, when administered after a 6-OHDA lesion, led to an increase in tyrosine hydroxylase (TH) positive cells in the lesioned substantia nigra [19]. These studies suggest that calcitriol has positive benefits in models of dopaminergic dysfunction. However, the ability of calcitriol to promote or accelerate recovery from a dopaminergic lesion has not been extensively evaluated. The purpose of the present study was to examine the ability of calcitriol to promote restoration of extracellular DA levels and tissue content of DA in animals previously lesioned with 6-OHDA. In vivo microdialysis was used to evaluate basal extracellular levels of DA and its primary metabolites 3,4-dihydroxyphenylacetic acid (DOPAC) and homovanillic acid (HVA), and stimulus-evoked overflow of DA, from the striatum of rats treated with 6-OHDA and calcitriol (the term overflow in this paper refers to the increase in DA in the extracellular milieu following stimulation by local application of amphetamine or excess potassium). Following the microdialysis experiments the effects of calcitriol were further evaluated by analysis of postmortem tissue levels of DA in the striatum and substantia nigra. In a separate group of animals the effects of 6-OHDA and calcitriol on striatal and nigral GDNF levels were evaluated.
Materials and methods
Animals
Male Fischer-344 rats 4–5 months old were obtained from Harlan Laboratories (Indianapolis, IN). The animals were housed in pairs under a 12-hr light-dark cycle with food and water freely available. All animal use procedures were approved by the Animal Care and Use Committee at the University of Kentucky and were in strict accordance with National Institutes of Health guidelines. All efforts were made to minimize the number of animals used and to minimize their pain and discomfort.
6-OHDA Injections
Surgeries were performed using sterile procedures on animals anesthetized with isoflurane (2.0–2.5% as needed). The rats were positioned in a stereotaxic apparatus, the skull exposed, and a small hole drilled in the skull over the right striatum (1.0 mm anterior to bregma, 2.8 mm lateral from midline). A microliter syringe with a 26 gauge blunt tapered needle was used to inject 12 µg 6-OHDA (Sigma-Aldrich, St. Louis, MO) into the striatum 5.0 mm below the surface of the cortex. The 6-OHDA was injected in a total of 4 µl 0.9 % saline with 0.1% ascorbic acid (pH 5.5) at a rate of 0.5 µl/min. The needle was left in place for an additional 5 minutes following the injection before being withdrawn. Gelfoam was placed in the burr hole, the incision closed with wound clips, and the animals allowed to recover.
Calcitriol Treatment
Four weeks after the 6-OHDA injections the animals were injected once daily for eight consecutive days with calcitriol (0.3 or 1.0 µg/kg/day) or vehicle. All injections were administered subcutaneously. The calcitriol (Sigma Chemical Co., St. Louis, MO) was first dissolved in propylene glycol at a concentration of 100 µg/ml. For injections the calcitriol in propylene glycol was diluted into 0.9% saline so that the final volume given was 1 ml/kg of body weight. Vehicle treated animals were injected with propylene glycol diluted in 0.9% saline.
In Vivo Microdialysis
Microdialysis studies were conducted three weeks after the final calcitriol treatment. The animals were anesthetized with urethane (1.25–1.50 g/kg, i.p.) and positioned in a stereotaxic frame. Body temperature was maintained at 37°C with a heating pad coupled to a rectal thermometer. Microdialysis probes (CMA/11 probes, 3.0 mm length of dialysis membrane; CMA/Microdialysis, Acton, MA) were slowly lowered into both the left and right striata (0.0 mm anterior to bregma, 3.0 mm lateral from midline, tip of probe 6.3 mm below the surface of the brain). The probes were perfused at a rate of 1.2 µl/min with artificial cerebrospinal fluid containing 145 mM NaCl, 2.7 mM KCl, 1.2 mM CaCl2, 1.0 mM MgCl2, 0.2 mM ascorbic acid, and 2.0 mM NaH2PO4 (pH 7.4). Dialysate fractions were collected at 20-min intervals. Following a two-hour equilibration period and the collection of 3 baseline fractions, DA overflow was stimulated by increasing the potassium concentration in the perfusate to 100 mM (NaCl reduced to 47.7 mM) for a single 20-min fraction, and then two hours later by adding 100 µM d-amphetamine to the perfusate for a single 20-min fraction. Five final fractions with normal artificial cerebrospinal fluid were collected following the d-amphetamine stimulation. Dialysate samples were immediately frozen on dry ice and stored at −80°C until assayed for DA, DOPAC and HVA.
Tissue Collection and HPLC Analysis
After collecting the dialysate fractions the urethane-anesthetized animals were killed by decapitation and their brains rapidly removed and chilled in ice-cold saline. A coronal slice of brain 2 mm thick at the level of the dialysis probes was made with the aid of an ice-chilled brain mold (Rodent Brain Matrix, ASI Instruments, Warren, MI). The location of all dialysis probes was confirmed to be centered in the dorsal striatum at the level of, or just rostral to, the crossing of the anterior commissure. The site of the intrastriatal injection was also visible and was confirmed to be located in the dorsal striatum. The striatum was then dissected from each half of the slice. The substantia nigra was dissected from both sides of a 2 mm thick coronal slice through the midbrain. The tissue pieces were placed in preweighed vials, weighed, and frozen on dry ice. Samples were stored at −80°C until assayed for DA and metabolites by high performance liquid chromatography (HPLC) as previously described [32]. For dialysis samples, 20 µl of the dialysate was injected directly onto the column.
Striatal and Nigral GDNF Levels
Rats were given an injection of 12 µg 6-OHDA into the right striatum as described above. Four weeks later the rats were treated with calcitriol (0.3 or 1.0 µg/kg, s.c.) or vehicle once daily for eight consecutive days, and striatal and nigral tissue was harvested 2–3 hours after the last injection. GDNF levels were measured using either Promega Emax™ ImmunoAssay kits (two experimental runs) or an R&D Systems GDNF DuoSet ELISA kit (one experimental run). Tissue samples were prepared as described previously [30, 33], and ELISA’s were performed according to the instructions supplied with each kit.
Data Analysis
All dialysis probes were calibrated in vitro prior to use to determine acceptable probes (recovery of DA at least 12%). However, values were not corrected for in vitro recoveries as uncorrected values may be better correlated to true values [34]. Basal levels of DA and metabolites were defined as the average value in the three fractions preceding stimulation by excess potassium. Dialysis data were expressed as nM concentration of DA or metabolite in the dialysate and, for stimulus evoked overflow, as the total amount of DA in the dialysate above baseline following stimulation with potassium or amphetamine. Tissue levels of DA and metabolites were expressed as ng/g wet weight of tissue. For the GDNF assays, the two runs with the Promega Kits and the one run with the R&D kit each gave significantly different control values as defined by the average value of the left, non-lesioned side of the vehicle treated rats. Thus, to facilitate the combining of the data from the three experimental runs and statistical comparisons, all data were expressed as a percentage of the left side of the animals treated with vehicle. Results were analyzed statistically using mixed analyses of variance (ANOVA) followed by Newman-Keuls tests for post hoc comparisons.
Results
Dialysate Levels of DA and Metabolites
Basal extracellular dialysate levels of DA and metabolites are shown in Table 1. In the vehicle treated animals there was a significant decrease in basal levels of DA of 31% (p < 0.01) on the lesioned side of the brain compared to the contralateral side. In the calcitriol treated animals, while there was a tendency for reduced basal DA levels on the lesioned side, the decreases did not reach statistical significance. However, there were significant decreases in basal levels of both DOPAC and HVA on the lesioned side in vehicle as well as calcitriol treated rats. For the vehicle, 0.3 µg and 1.0 µg doses of calcitriol the respective decreases in DOPAC levels were 85%, 73% and 71% (p < 0.001 for all groups); and the respective decreases in HVA levels were 74%, 57% and 60% (p < 0.001 for all groups).
Table 1.
Basal dialysate levels of DA, DOPAC and HVA from the striatum of animals injected in the right striatum with 6-OHDA followed four weeks later with eight days of calcitriol treatment. Dialysis experiments were performed three weeks after the end of the calcitriol injections
| Calcitriol dose and side of brain |
Dialysate level (nM) | ||
|---|---|---|---|
| DA | DOPAC | HVA | |
| Vehicle | |||
| Left striatum | 5.03 ± 0.33 | 1654 ± 71 | 956 ± 34 |
| Right striatum | 3.44 ± 0.31 a | 253 ± 66 a | 253 ± 45 a |
| 0.3 µg/kg/day | |||
| Left striatum | 4.54 ± 0.65 | 1408 ± 109 | 874 ± 50 |
| Right striatum | 4.08 ± 0.47 | 387 ± 73 a | 373 ± 57 a |
| 1.0 µg/kg/day | |||
| Left striatum | 4.06 ± 0.26 | 1520 ± 85 | 888 ± 30 |
| Right striatum | 3.42 ± 0.32 | 435 ± 112 a | 355 ± 67 a |
Values are mean ± SEM from 8 animals per group
p < 0.05 vs. left striatum (mixed ANOVA with treatment group as a between factor and side of brain as a within factor; followed by Newman-Keuls post hoc comparisons)
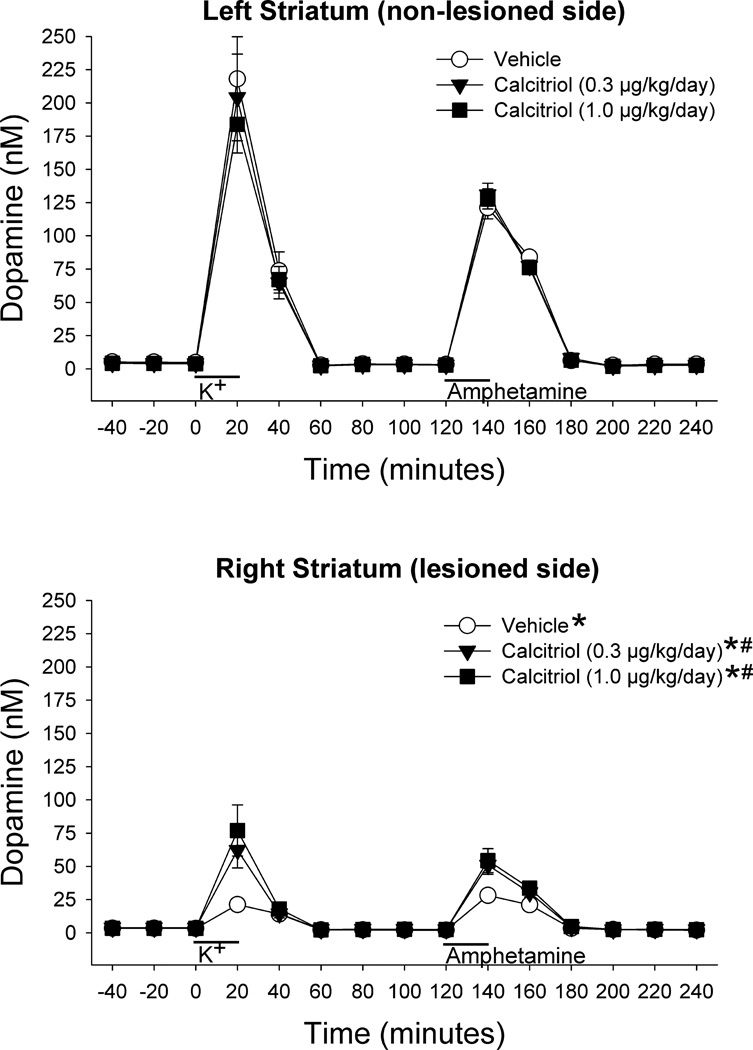
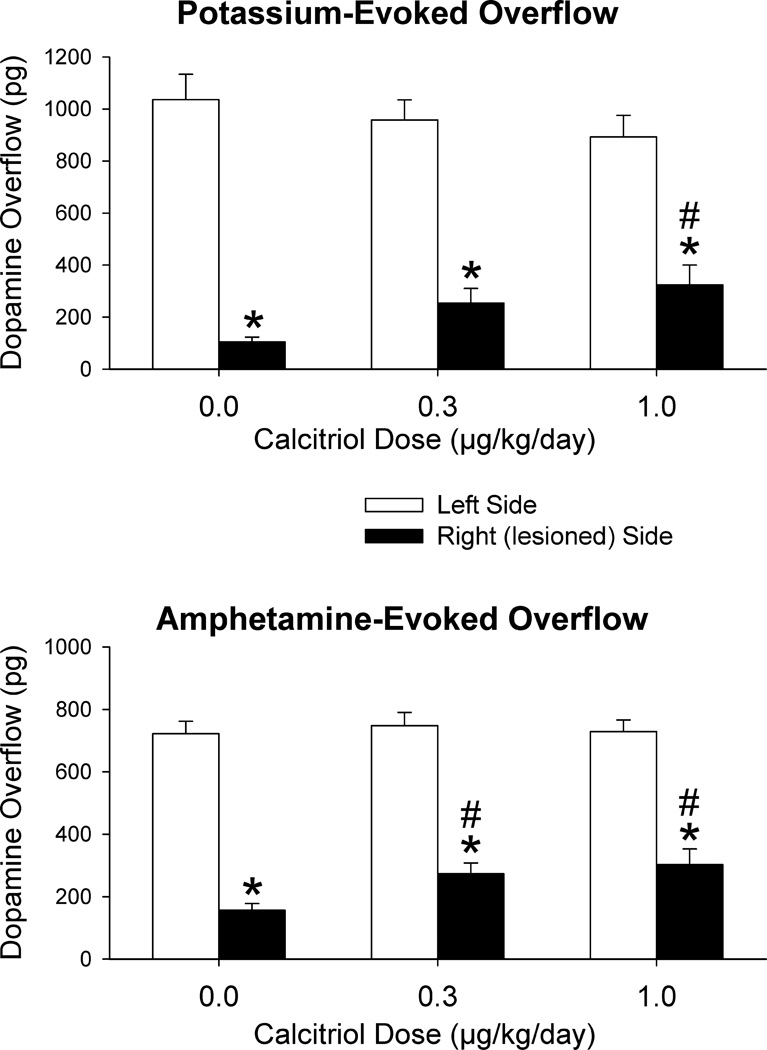
Figure 1 shows the time course data for DA levels from the in vivo microdialysis experiments. Within each group, overall DA levels on the lesioned side were lower than those from the contralateral side (p < 0.001 for all groups). In addition, on the lesioned side, DA levels from the groups treated with the 0.3 µg and 1.0 µg doses of calcitriol were greater than those from the vehicle treated group (p < 0.05 for both). In order to facilitate comparison of the stimulus evoked overflow of DA between the groups and sides of the brain the data were expressed as total amount of DA in the dialysate fractions above basal levels following stimulation by excess potassium or d-amphetamine (Fig. 2). In the vehicle treated rats, potassium evoked DA overflow was reduced on the lesioned side of the brain by 89% compared to the contralateral side (p < 0.001). In the calcitriol treated rats the decreases in potassium evoked DA overflow on the lesioned side were 73% in the 0.3 µg dose group and 63% in the 1.0 µg dose group (p < 0.001 for both groups). The potassium evoked overflow of DA on the lesioned side of the brain was significantly greater in the group treated with the 1.0 µg dose of calcitriol than in the vehicle treated group (p < 0.05). Amphetamine evoked DA overflow was reduced on the lesioned side of the brain by 78% in the vehicle treated rats (p < 0.001), and by 63% and 58%, respectively, in the groups treated with the 0.3 and 1.0 µg doses of calcitriol (p < 0.001 for both groups). In addition, the amphetamine evoked overflow of DA on the lesioned side of the brain was significantly greater in both calcitriol treated groups compared to the vehicle treated control group (p < 0.05 for both).
Fig. 1.
Dialysate levels of DA from the left and right striata of animals injected in the right striatum with 6-OHDA four weeks prior to treatment with vehicle or calcitriol. Microdialysis experiments were performed three weeks after the last vehicle or calcitriol injection. Excess potassium (100 mM) was included in the perfusate for 20-min starting at 0 min (horizontal bar above K+), and 100 µM amphetamine was included in the perfusate for 20-min starting at 120 min (horizontal bar above Amphetamine). Values shown are mean ± SEM from 8 animals per group. * p < 0.001 vs. left striatum, # p < 0.05 vs. right striatum of vehicle treated group (mixed ANOVA with side of brain and time of dialysis sample collection as within factors, and treatment group as a between factor; followed by Newman-Keuls post-hoc comparisons)
Fig. 2.
Potassium-evoked (top panel) and amphetamine-evoked (bottom panel) overflow of DA from the striatum of animals injected in the right striatum with 6-OHDA four weeks prior to treatment with vehicle (0.0 µg dose of calcitriol) or calcitriol. Microdialysis experiments were performed three weeks after the last vehicle or calcitriol injection. Values shown are mean ± SEM from 8 animals per group. * p < 0.05 vs. left side of same group, # p < 0.05 vs. right side of vehicle treated group (mixed ANOVA with side of brain as a within factor and treatment as a between factor; followed by Newman-Keuls post-hoc comparisons)
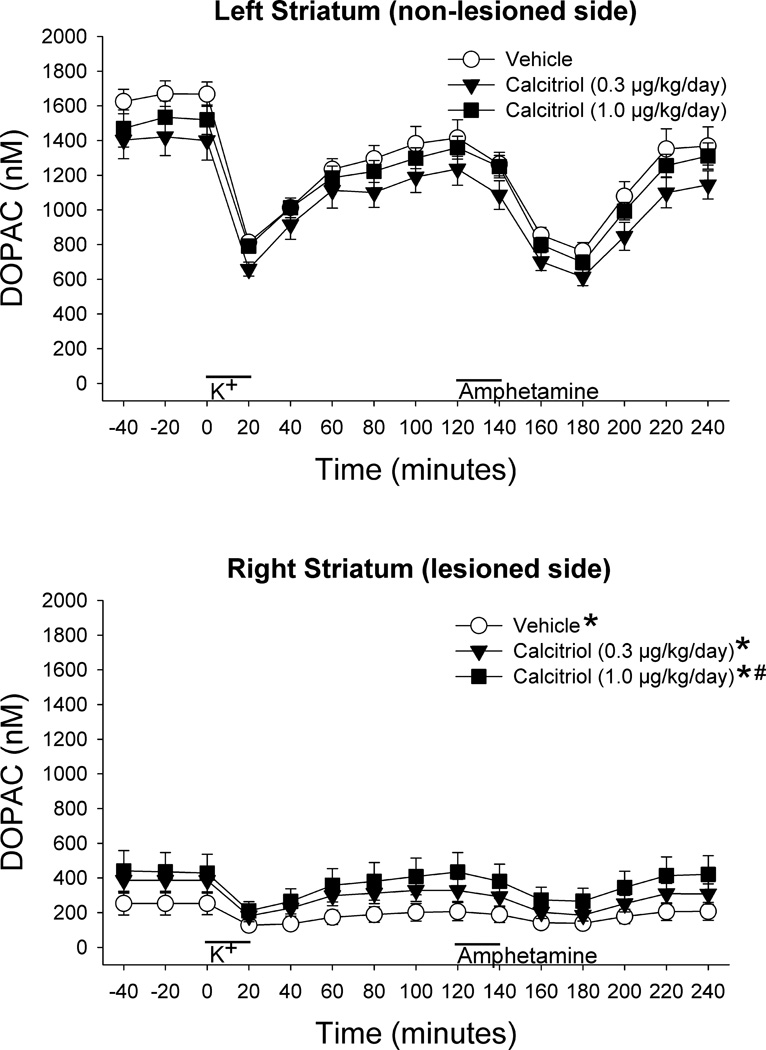
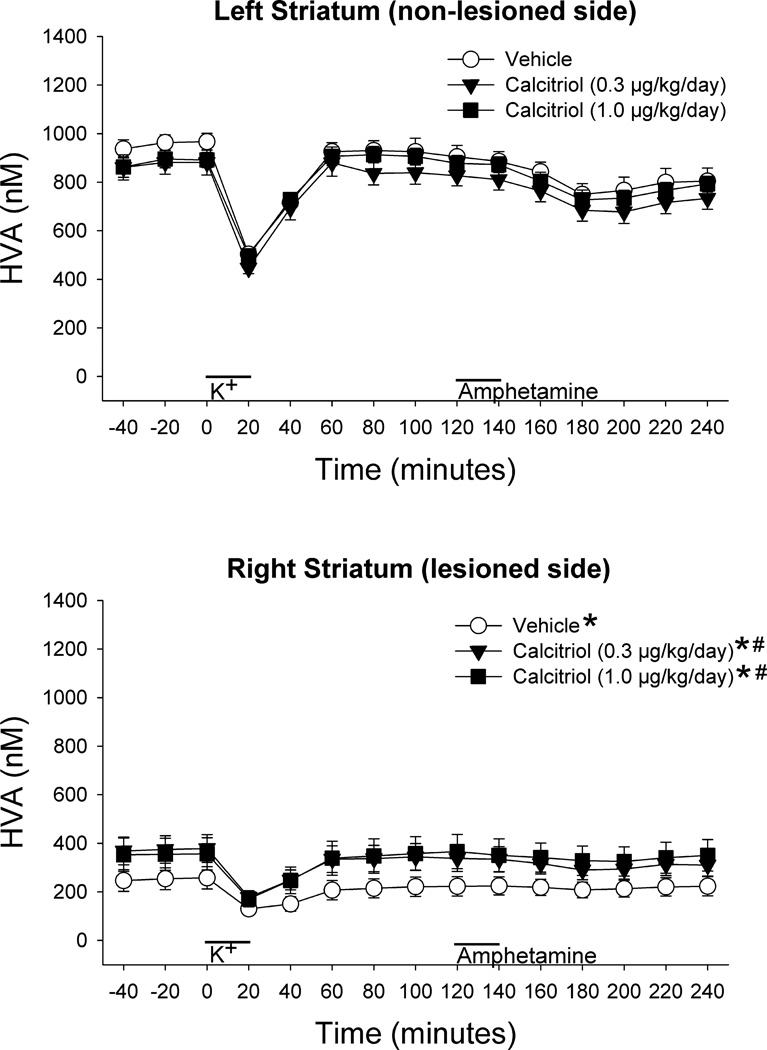
Figures 3 and 4 show the time course data from the in vivo microdialysis experiments for DOPAC and HVA. The 6-OHDA treatments led to reduced levels of both metabolites on the lesioned side of the brain compared to the contralateral side for all treatment groups (p < 0.001 for all groups). However, on the lesioned side, DOPAC levels were significantly greater in the animals treated with the 1.0 µg dose of calcitriol compared to the vehicle treated group (Fig. 3, p < 0.05), and HVA levels were significantly greater in the animals treated with both the 0.3 µg and 1.0 µg doses of calcitriol compared to the vehicle treated group (Fig. 4, p< 0.05 for both comparisons).
Fig. 3.
Dialysate levels of DOPAC from the left and right striata of animals injected in the right striatum with 6-OHDA four weeks prior to treatment with vehicle or calcitriol. Microdialysis experiments were performed three weeks after the last vehicle or calcitriol injection. Excess potassium (100 mM) was included in the perfusate for 20-min starting at 0 min (horizontal bar above K+), and 100 µM amphetamine was included in the perfusate for 20-min starting at 120 min (horizontal bar above Amphetamine). Values shown are mean ± SEM from 8 animals per group. * p < 0.001 vs. left striatum, # p < 0.05 vs. right striatum of vehicle treated group (mixed ANOVA with side of brain and time of dialysis sample collection as within factors, and treatment group as a between factor; followed by Newman-Keuls post-hoc comparisons)
Fig. 4.
Dialysate levels of HVA from the left and right striata of animals injected in the right striatum with 6-OHDA four weeks prior to treatment with vehicle or calcitriol. Microdialysis experiments were performed three weeks after the last vehicle or calcitriol injection. Excess potassium (100 mM) was included in the perfusate for 20-min starting at 0 min (horizontal bar above K+), and 100 µM amphetamine was included in the perfusate for 20-min starting at 120 min (horizontal bar above Amphetamine). Values shown are mean ± SEM from 8 animals per group. * p < 0.001 vs. left striatum, # p < 0.05 vs. right striatum of vehicle treated group (mixed ANOVA with side of brain and time of dialysis sample collection as within factors, and treatment group as a between factor; followed by Newman-Keuls post-hoc comparisons)
Tissue Levels of DA and Metabolites
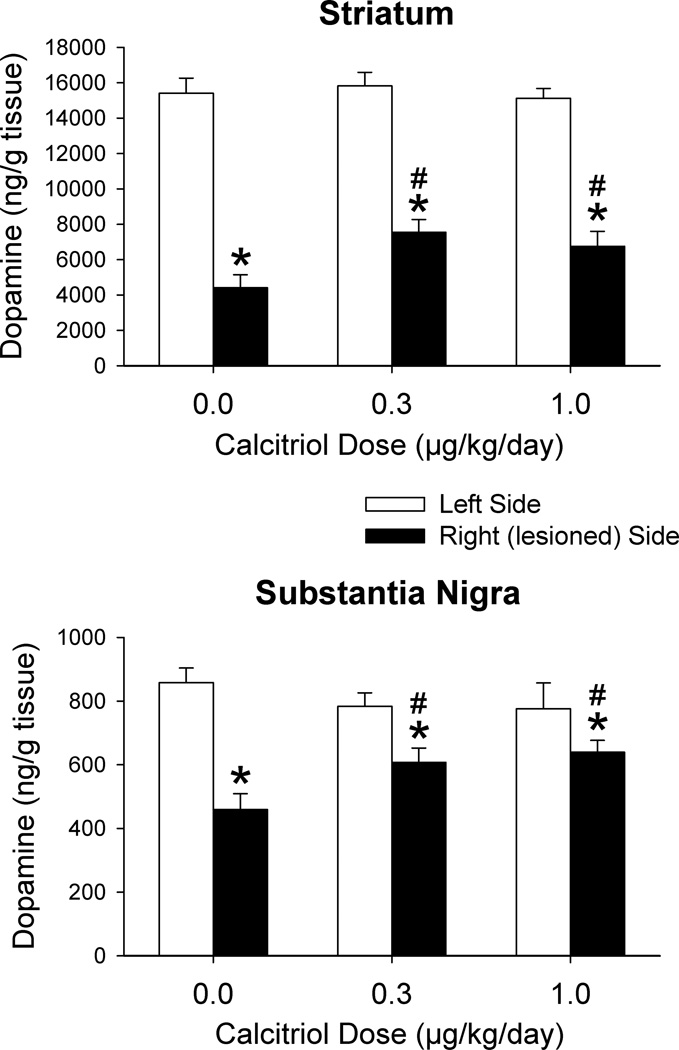
The intrastriatal injection of 6-OHDA and the systemic injections of calcitriol affected postmortem levels of DA in both the striatum and substantia nigra (Fig. 5). In the 6-OHDA and vehicle treated rats striatal DA levels were decreased by 71% on the lesioned side compared to the contralateral side (p < 0.001). In the 6-OHDA and calcitriol treated rats striatal DA levels were decreased by 52% (0.3 µg dose of calcitriol) and 55% (1.0 µg dose of calcitriol) on the lesioned side compared to the contralateral side (p < 0.001 for both doses). The decrease in DA levels in both the calcitriol treated groups was significantly less than the decrease in the vehicle treated animals (p < 0.05 for both). Similar effects were found in the substantia nigra. In the 6-OHDA and vehicle treated rats nigral DA levels were decreased by 47% on the lesioned side compared to the contralateral side (p < 0.001). However, in the 6-OHDA and calcitriol treated rats nigral DA levels were decreased by 23% and 18% in the 0.3 µg and 1.0 µg dose groups, respectively, on the lesioned side compared to the contralateral side (p < 0.05 for both doses). The decrease in DA levels in both calcitriol treated groups was significantly less than the decrease in the vehicle treated animals (p < 0.05 for both).
Fig. 5.
Postmortem tissue levels of DA from the striatum and substantia nigra of animals injected in the right striatum with 6-OHDA four weeks prior to treatment with vehicle (0.0 µg dose of calcitriol) or calcitriol. Tissue was harvested three weeks after the last vehicle or calcitriol injection. Values shown are mean ± SEM from 8 animals per group. * p < 0.05 vs. left side of same group, # p < 0.05 vs. right side of vehicle treated group (mixed ANOVA with side of brain as a within factor and treatment group as a between factor; followed by Newman-Keuls post-hoc comparisons)
Postmortem tissue levels of DOPAC and HVA are shown in Table 2. In the 6-OHDA and vehicle treated animals striatal DOPAC and HVA levels were decreased by 69% and 66%, respectively, on the lesioned side compared to the contralateral side (p < 0.001 for both). While both striatal DOPAC and HVA levels tended to be higher on the lesioned side of the calcitriol treated groups the differences were not statistically significant from the vehicle treated group. A similar effect was found for DOPAC levels in the substantia nigra. In the vehicle treated animals there was a 51% decrease in nigral DOPAC levels on the lesioned side (p < 0.001), and, although the decreases tended to be less in the calcitriol treated groups, the decreases were not statistically different from the vehicle treated group. However, while nigral HVA levels were reduced by 44% on the lesioned side in the vehicle treated group (p < 0.001), they were not significantly reduced on the lesioned side of either the 0.3 µg dose group (−7%) or the 1.0 µg dose group (−8%). In addition, nigral tissue levels of HVA were greater on the lesioned side of both of the calcitriol treated groups compared to the lesioned side of the vehicle treated control animals (p < 0.01 for both).
Table 2.
Tissue levels of DOPAC and HVA from the striatum and substantia nigra of animals injected in the right striatum with 6-OHDA followed four weeks later with eight days of calcitriol treatment. Tissue was harvested three weeks after the end of the calcitriol injections
| Calcitriol dose and side of brain |
Tissue content (ng/g wet weight) | |||
|---|---|---|---|---|
| Striatum | Substantia Nigra | |||
| DOPAC | HVA | DOPAC | HVA | |
| Vehicle | ||||
| Left side | 2324 ± 131 | 1505 ± 73 | 145 ± 12 | 78 ± 5 |
| Right side | 727 ± 153 a | 519 ± 93 a | 71 ± 10 a | 44 ± 5 a |
| 0.3 µg/kg/day | ||||
| Left side | 2239 ± 97 | 1419 ± 57 | 137 ± 12 | 75 ± 3 |
| Right side | 1025 ± 78 a | 699 ± 43 a | 100 ± 7 a | 70 ± 3 b |
| 1.0 µg/kg/day | ||||
| Left side | 2243 ± 91 | 1614 ± 68 | 151 ± 14 | 83 ± 6 |
| Right side | 902 ± 107 a | 700 ± 83 a | 98 ± 13 a | 76 ± 8 b |
Values are mean ± SEM from 8 animals per group
p < 0.01 vs. left side of same group,
p < 0.01 vs. right side of vehicle treated group (mixed ANOVA with treatment group as a between factor and side of brain as a within factor; followed by Newman-Keuls post hoc comparisons)
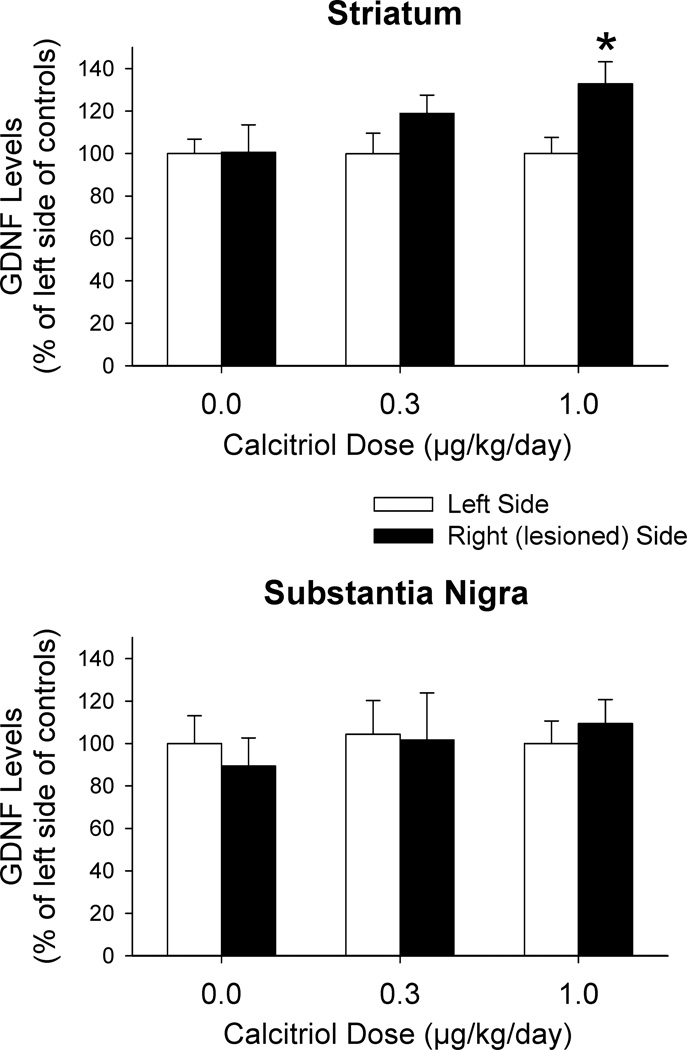
Tissue Levels of GDNF
In a separate group of animals, rats were given an injection of 12 µg 6-OHDA into the right striatum as described above and four weeks later the rats were treated with calcitriol or vehicle once daily for eight consecutive days. Tissue was harvested on the last day of calcitriol or vehicle treatment for measurement of GDNF levels. The overall control levels of GDNF on the non-lesioned side of the vehicle treated rats were 7.16 ± 1.72 ng/g tissue in the striatum, and 11.65 ± 3.91 ng/g tissue in the substantia nigra (n = 12 each). Because of the relatively large variance (due to the differing results with the three GDNF assay kits), the data were expressed as a percentage of the non-lesioned side of the animals treated with vehicle in order to facilitate statistical comparisons. In the striatum a mixed ANOVA (side of brain as a within factor and treatment as a between factor) identified a main effect of side of brain. While there was a trend for GDNF levels to be greater on the lesioned side of the brain in the calcitriol treated animals (Fig. 6), the differences did not reach significance using a Newman-Keuls post hoc comparison (however, the less conservative Fisher’s Least Significant Difference (LSD) test did indicate a significant increase in GDNF levels on the lesioned side of the animals treated with the 1.0 µg dose of calcitriol). In the substantia nigra there were no significant differences in GDNF levels between sides of brain or between doses of calcitriol.
Fig. 6.
Tissue levels of GDNF from the striatum and substantia nigra of animals injected in the right striatum with 6-OHDA four weeks prior to eight days of treatment with vehicle (0.0 µg dose of calcitriol) or calcitriol. Tissue was harvested 2–3 hours after the last injection of vehicle or calcitriol. Data from all groups are expressed as a percentage of the left side of the animals treated with vehicle (0.0 µg dose of calcitriol). Values shown are mean ± SEM from 12 animals per group. * p < 0.05 vs. left side of all groups and right side of vehicle treated group (mixed ANOVA with side of brain as a within factor and treatment group as a between factor; followed by Fisher’s LSD post-hoc comparisons)
Discussion
The goal of the present study was to examine the ability of calcitriol to help promote recovery of DA release and content in the nigrostriatal system of rats previously treated with the neurotoxin 6-OHDA. The calcitriol treatments led to increases in potassium and amphetamine evoked overflow of striatal DA, and to increases in striatal and nigral tissue levels of DA, on the lesioned side of the brain. Although these calcitriol-induced increases were only partial, these results support that calcitriol may be able to help in promoting the restoration of dopaminergic functioning in injured nigrostriatal DA neurons.
Two doses of calcitriol were examined in this study (0.3 and 1.0 µg/kg/day). For the most part the effects were similar; however, the larger dose did produce a greater or significant effect in a few parameters (for instance, potassium evoked DA overflow and striatal GDNF levels). While we did not examine higher doses of calcitriol, it is not likely that larger doses would have substantially greater effects. We did not examine higher doses in this study because we have previously examined a higher dose (3.0 µg/kg/day) in normal rats and found that while the effects on DA overflow and content were very similar to the 1.0 µg/kg/day dose [17], rats treated with the 3.0 µg dose lost a substantial amount of body weight over the eight days of treatment (which did not occur with the 0.3 or 1.0 µg/kg/day doses). Thus, higher doses may produce adverse side effects, which may be due in part to hypercalcemia [20, 35].
The eight days of calcitriol injections and the three week time period from the last injection to the microdialysis experiments were based on previously published studies. Seven or eight days of calcitriol has been shown to have significant effects of the nigrostriatal DA system of normal and lesioned animals [17–19, 31], and seven or eight days of calcitriol has been shown to upregulate GDNF expression and protein levels in the brain [17–20, 30]. Thus, we treated the animals with calcitriol for eight days. The three week interval from the last calcitriol injection to the microdialysis experiments was chosen as it is a time point when significant changes in stimulus evoked DA overflow and content have been demonstrated in normal rats following calcitriol treatment [17]. In addition, as it is possible that the effects of calcitriol on DA neurons may be due in part to augmented GDNF levels, the three week time period has also been shown to lead to changes in stimulus evoked DA overflow and content in animals following GDNF injection [36–38].
Both doses of calcitriol led to partial recovery of striatal and nigral DA levels. While the role of striatal DA in behavior, including parkinsonian signs, has been well established, there is growing evidence for the importance of nigral DA in regulating motor performance [39–42]. Thus, the ability of calcitriol to partially restore nigral DA levels, as well as striatal DA, is an important component of the potential restorative effects of calcitriol.
The mechanism by which calcitriol promotes recovery of dopaminergic release and content remains to be determined. Previous reports have shown that calcitriol administration can lead to upregulation of endogenous GDNF levels in the striatum and substantia nigra [17–19] and to increases in expression or release of GDNF in various cell lines [14–16]. GDNF has been shown to have both neuroprotective and restorative effects in animal models of PD [21–25], including increased DA levels [43, 44] and TH positive cell number and fiber density [44,45] in animals previously lesioned with 6-OHDA. Calcitriol-induced upregulation of GDNF could therefore be a possible mechanism for the effects reported in this study. However, the effects we observed on GDNF levels were minor: a 32% increase in striatal GDNF levels on the lesioned side in animals treated with the higher dose of calcitriol, and no difference between the lesioned and non-lesioned sides in the substantia nigra. Thus, while calcitriol-induced increases in GDNF could play a role in the observed increases in evoked overflow and tissue content of DA, other yet unidentified mechanisms may also be involved with producing the present results. For example, calcitriol has been shown to regulate several other trophic factors [4–7] and the p75 neurotrophin receptor [46]. Modulation of these pathways could affect neuronal cell function. Calcitriol also increases expression of the TH gene in vitro [47]. If a similar effect occurs in vivo this could lead to increased stores and release of DA. In addition, calcitriol and vitamin D have numerous others effects in the brain, such as reducing the production of free radicals or upregulating free radical scavenging systems [48–51], modulating neuro-immunological function [1, 3, 52] and regulating neuronal calcium signaling [53, 54], all of which could alter the functional status of neurons. Thus, there are numerous possibilities that could play a role in the present results, and further studies will be needed to determine the complete mechanism.
An unexpected finding in this study was the lack of calcitriol-induced increases in extracellular DA levels and DA content, and GDNF levels, on the non-lesioned control side of the brain. We have previously reported increases in stimulus evoked DA overflow and tissue DA content in normal animals following calcitriol treatment [17]. In addition, we [17] and others [18] have reported increases in GDNF levels in normal rats following calcitriol administration. The reasons for the discrepancies between the current study and previous studies are not clear. The main difference in the current study is that the animals were lesioned with 6-OHDA prior to the calcitriol treatments. It is possible that homeostatic mechanisms are in play to try and maintain the balance between the two sides of the brain; however, additional studies will be necessary in order to explain the different findings between studies.
While the present study was designed to examine potential restorative effects of calcitriol in animals previously lesioned with 6-OHDA, several previous studies have examined the protective effects of calcitriol against dopaminergic toxins. Wang et al. [31] treated rats with calcitriol (1 µg/kg/day) for eight days and administered a unilateral 6-OHDA lesion of the medial forebrain bundle on the seventh day of treatment. They found that calcitriol treated rats had greater locomotor activity than saline treated rats, and that nigral levels of DA and metabolites were not significantly reduced on the lesioned side of the calcitriol and 6-OHDA treated rats. Smith et al. [30] reported that continuous daily treatment with calcitriol (1.0 µg/kg/day) starting seven days prior to an interventricular injection of 6-OHDA partially protected against 6-OHDA induced reductions in potassium and amphetamine evoked overflow of DA and tissue content of DA in the striatum. Kim et al. [29] found that pretreatment with calcitriol (1.0 µg/kg/day) for seven days before injecting 6-OHDA into the medial forebrain bundle of rats, or intraperitoneal injections of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) in mice, significantly attenuated toxin-induced loss of TH positive neurons in the substantia nigra. Sanchez et al. [19] reported that 7 days of calcitriol (1.0 µg/kg/day) prior to a medial forebrain bundle 6-OHDA lesion reduced 6-OHDA-induced decreases in striatal TH protein levels and nigral TH positive cell number. There are many mechanisms for how compounds may help protect against neurotoxins, such as by upregulating trophic factors, or by directly or indirectly interfering with the toxin’s mechanism of action. However, as DA cells are continually lost over time in PD, the ability of compounds such as calcitriol to protect against dopaminergic toxins in animal models is important in understanding how to prevent further loss or damage to DA cells.
Along with the current results that suggest that calcitriol may be able to help promote the recovery of dopaminergic functioning in injured nigrostriatal DA neurons, Sanchez et al. [19] also examined the potential restorative effects of calcitriol. They found that 7 days of calcitriol (1.0 µg/kg/day) starting 21 days after a medial forebrain bundle 6-OHDA lesion helped restore striatal TH protein levels and increased the number of TH positive cells in the substantia nigra on the lesioned side compared to the lesioned side of control animals. In addition, several studies have linked vitamin D insufficiency or variations in the vitamin D receptor with an increased risk of developing PD [55–57], and a recent clinical study has demonstrated positive effects of vitamin D supplementation in PD patients [58]. Taken together, the animal and clinical studies suggest that vitamin D and calcitriol may have positive effects on dopaminergic neurons and warrant further investigation of the effects of calcitriol on DA systems.
Acknowledgments
This study was supported in part by United States Public Health Service Grants NS60924 and NS75871.
Footnotes
None of the authors have a conflict of interest of any type in association with this work.
References
- 1.Fernandes de Abreu DA, Eyles D, Feron F. Vitamin D, a neuro-immunomodulator: implications for neurodegenerative and autoimmune diseases. Psychoneuroendocrinology. 2009;34S:S265–S277. doi: 10.1016/j.psyneuen.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 2.Garcion E, Wion-Barbot N, Montero-Menei CN, Berger F, Wion D. New clues about vitamin D functions in the nervous system. Trends Endocrinol Metab. 2002;13:100–105. doi: 10.1016/s1043-2760(01)00547-1. [DOI] [PubMed] [Google Scholar]
- 3.Kesby JP, Eyles DW, Burne THJ, McGrath JJ. The effects of vitamin D on brain development and adult brain function. Mol Cell Endocrinol. 2011;347:121–127. doi: 10.1016/j.mce.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 4.Neveu I, Naveilhan P, Baudet C, Brachet P, Metsis M. 1,25-Dihydroxyvitamin D3 regulates NT-3, NT-4 but not BDNF mRNA in astrocytes. NeuroReport. 1994;6:124–126. doi: 10.1097/00001756-199412300-00032. [DOI] [PubMed] [Google Scholar]
- 5.Saporito MS, Brown ER, Hartpence KC, Wilcox HM, Vaught JL, Carswell S. Chronic 1,25-dihydroxyvitamin D3-mediated induction of nerve growth factor mRNA and protein in L929 fibroblasts and in adult rat brain. Brain Res. 1994;633:189–196. doi: 10.1016/0006-8993(94)91539-3. [DOI] [PubMed] [Google Scholar]
- 6.Veenstra TD, Londowski JM, Windebank AJ, Brimijoin S, Kumar R. Effects of 1,25-dihydroxyvitamin D3 on growth of mouse neuroblastoma cells. Dev Brain Res. 1997;99:53–60. doi: 10.1016/s0165-3806(96)00196-4. [DOI] [PubMed] [Google Scholar]
- 7.Veenstra TD, Windebank AJ, Kumar R. 1,25-Dihydroxyvitamin D3 regulates expression of N-myc, c-myc, protein kinase C, transforming growth factor-β2 in neuroblastoma cells. Biochem Biophys Res Commun. 1997;235:15–18. doi: 10.1006/bbrc.1997.6718. [DOI] [PubMed] [Google Scholar]
- 8.Stumpf WE, O’Brien LP. 1,25(OH)2 vitamin D3 sites of action in the brain. An autoradiographic study. Histochemistry. 1987;87:393–406. doi: 10.1007/BF00496810. [DOI] [PubMed] [Google Scholar]
- 9.Prufer K, Veenstra TD, Jirikowski GF, Kumar R. Distribution of 1,25-dihydroxyvitamin D3 receptor immunoreactivity in rat brain and spinal cord. J Chem Neuroanat. 1999;16:135–145. doi: 10.1016/s0891-0618(99)00002-2. [DOI] [PubMed] [Google Scholar]
- 10.Eyles DW, Smith S, Kinobe R, Hewison M, McGrath JJ. Distribution of the vitamin D receptor and 1α-hydroxylase in human brain. J Clin Neuroanat. 2005;29:21–30. doi: 10.1016/j.jchemneu.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Gascon-Barre M, Huet PM. Apparent [3H]1,25-dihydroxyvitamin D3 uptake by canine and rodent brain. Am J Physiol. 1983;244:E266–E271. doi: 10.1152/ajpendo.1983.244.3.E266. [DOI] [PubMed] [Google Scholar]
- 12.Pardridge WM, Sakiyama R, Coty WA. Restricted transport of vitamin D and A derivatives through the rat blood-brain barrier. J Neurochem. 1985;44:1138–1141. doi: 10.1111/j.1471-4159.1985.tb08735.x. [DOI] [PubMed] [Google Scholar]
- 13.Neveu I, Naveilhan P, Menaa C, Wion D, Brachet P, Garabedian M. Synthesis of 1,25-dihydroxyvitamin D3 by rat brain macrophages in vitro. J Neurosci Res. 1994;38:214–220. doi: 10.1002/jnr.490380212. [DOI] [PubMed] [Google Scholar]
- 14.Naveilhan P, Neveu I, Wion D, Brachet P. 1,25-Dihydroxyvitamin D3, an inducer of glial cell line-derived neurotrophic factor. NeuroReport. 1996;7:2171–2175. doi: 10.1097/00001756-199609020-00023. [DOI] [PubMed] [Google Scholar]
- 15.Orme RP, Bhangal MS, Fricker RA. Calcitriol imparts neuroprotection in vitro to midbrain dopaminergic neurons by upregulating GDNF expression. PLoS ONE. 2013;8(4):e62040. doi: 10.1371/journal.pone.0062040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verity AN, Wyatt TL, Lee W, Hajos B, Baecker PA, Eglen RM, Johnson RM. Differential regulation of glial cell line-derived neurotrophic factor (GDNF) expression in human neuroblastoma and glioblastoma cell lines. J Neurosci Res. 1999;55:187–197. doi: 10.1002/(SICI)1097-4547(19990115)55:2<187::AID-JNR6>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 17.Cass WA, Peters LE, Fletcher AM, Yurek DM. Evoked dopamine overflow is augmented in the striatum of calcitriol treated rats. Neurochem Int. 2012;60:186–191. doi: 10.1016/j.neuint.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanchez B, Lopez-Martin E, Segura C, Labandeira-Garcia JL, Perez-Fernandez R. 1,25-Dihydroxyvitamin D3 increases striatal GDNF mRNA and protein expression in adult rats. Mol Brain Res. 2002;108:143–146. doi: 10.1016/s0169-328x(02)00545-4. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez B, Relova JL, Gallego R, Ben-Batalla I, Perez-Fernandez R. 1,25-Dihydroxyvitamin D3 administration to 6-hydroxydopamine-lesioned rats increases glial cell line-derived neurotrophic factor and partially restores tyrosine hydroxylase expression in substantia nigra and striatum. J Neurosci Res. 2009;87:723–732. doi: 10.1002/jnr.21878. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Chiang Y-H, Su T-P, Hayashi T, Morales M, Hoffer BJ, Lin S-Z. Vitamin D3 attenuates cortical infarction induced by middle cerebral artery ligation in rats. Neuropharmacology. 2000;39:873–880. doi: 10.1016/s0028-3908(99)00255-5. [DOI] [PubMed] [Google Scholar]
- 21.Bjorklund A, Kirik D, Rosenblad C, Georgievska B, Lundberg C, Mandel RJ. Towards a neuroprotective gene therapy for Parkinson’s disease: use of adenovirus, AAV and lentivirus vectors for gene transfer of GDNF to the nigrostriatal system in the rat Parkinson model. Brain Res. 2000;886:82–98. doi: 10.1016/s0006-8993(00)02915-2. [DOI] [PubMed] [Google Scholar]
- 22.Cass WA, Kearns CM, Gash DM. Protective and regenerative properties of GDNF in the central nervous system. In: Mattson MP, editor. Neuroprotective Signal Transduction. Totowa, NJ: Humana Press; 1998. pp. 145–161. [Google Scholar]
- 23.Gash DM, Zhang Z, Gerhardt GA. Neuroprotective and neurorestorative properties of GDNF. Ann Neurol. 1998;44(suppl. 1):S121–S125. doi: 10.1002/ana.410440718. [DOI] [PubMed] [Google Scholar]
- 24.Grondin R, Zhang Z, Yi A, Cass WA, Maswood N, Andersen AH, Elsberry DD, Klein MC, Gerhardt GA, Gash DM. Chronic, controlled GDNF infusion promotes structural and functional recovery in advanced parkinsonian monkeys. Brain. 2002;125:2191–2201. doi: 10.1093/brain/awf234. [DOI] [PubMed] [Google Scholar]
- 25.Kordower JH, Emborg ME, Bloch J, Ma SY, Chu Y, Leventhal L, McBride J, Chen E-Y, Palfi S, Roitberg BZ, Brown WD, Holden JE, Pyzalski R, Taylor MD, Carvey P, Ling Z, Trono D, Hantraye P, Deglon N, Aebisher P. Neurodegeneration prevented by lentiviral vector delivery of GDNF in primate models of Parkinson’s disease. Science. 2000;290:767–773. doi: 10.1126/science.290.5492.767. [DOI] [PubMed] [Google Scholar]
- 26.Gill SS, Patel NK, Hotton GR, O'Sullivan K, McCarter R, Bunnage M, Brooks DJ, Svendsen CN, Heywood P. Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease. Nature Med. 2003;9:589–595. doi: 10.1038/nm850. [DOI] [PubMed] [Google Scholar]
- 27.Slevin JT, Gerhardt GA, Smith CD, Gash DM, Kryscio R, Young B. Improvement of bilateral motor functions in patients with Parkinson disease through the unilateral intraputaminal infusion of glial cell line-derived neurotrophic factor. J Neurosurg. 2005;102:216–222. doi: 10.3171/jns.2005.102.2.0216. [DOI] [PubMed] [Google Scholar]
- 28.Lang AE, Gill S, Patel NK, Lozano A, Nutt JG, Penn R, Brooks DJ, Hotton G, Moro E, Heywood P, Brodsky MA, Burchiel K, Kelly P, Dalvi A, Scott B, Stacy M, Turner D, Wooten VGF, Elias WJ, Laws ER, Dhawan V, Stoessl AJ, Matcham J, Coffey RJ, Traub M. Randomized controlled trial of intraputamenal glial cell line-derived neurotrophic factor infusion in Parkinson disease. Ann Neurol. 2006;59:459–466. doi: 10.1002/ana.20737. [DOI] [PubMed] [Google Scholar]
- 29.Kim J-S, Ryu S-Y, Yun I, Kim W-J, Lee K-S, Park J-W, Kim Y-I. 1α,25-Dihydroxyvitamin D3 protects dopaminergic neurons in rodent models of Parkinson’s disease through inhibition of microglial activation. J Clin Neurol. 2006;2:252–257. doi: 10.3988/jcn.2006.2.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith MP, Fletcher-Turner A, Yurek DM, Cass WA. Calcitriol protection against dopamine loss induced by intracerebroventricular administration of 6-hydroxydopamine. Neurochem Res. 2006;31:533–539. doi: 10.1007/s11064-006-9048-4. [DOI] [PubMed] [Google Scholar]
- 31.Wang J-Y, Wu J-N, Cherng T-L, Hoffer BJ, Chen H-H, Borlongan CV, Wang Y. Vitamin D3 attenuates 6-hydroxydopmaine-induced neurotoxicity in rats. Brain Res. 2001;904:67–75. doi: 10.1016/s0006-8993(01)02450-7. [DOI] [PubMed] [Google Scholar]
- 32.Cass WA, Harned ME, Peters LE, Nath A, Maragos WF. HIV-1 Protein Tat Potentiation of Methamphetamine-Induced Decreases in Evoked Overflow of Dopamine in the Striatum of the Rat. Brain Res. 2003;984:133–142. doi: 10.1016/s0006-8993(03)03122-6. [DOI] [PubMed] [Google Scholar]
- 33.Yurek DM, Fletcher-Turner A. Differential expression of GDNF, BDNF, and NT-3 in the aging nigrostriatal system following a neurotoxic lesion. Brain Res. 2001;891:228–235. doi: 10.1016/s0006-8993(00)03217-0. [DOI] [PubMed] [Google Scholar]
- 34.Glick SD, Dong N, Keller RW, Jr, Carlson JN. Estimating extracellular concentrations of dopamine and 3,4-dihydroxyphenylacetic acid in nucleus accumbens and striatum using microdialysis: relationships between in vitro and in vivo recoveries. J Neurochem. 1994;62:2017–2021. doi: 10.1046/j.1471-4159.1994.62052017.x. [DOI] [PubMed] [Google Scholar]
- 35.Chavhan SG, Brar RS, Banga HS, Sandhu HS, Sodhi S, Gadhave PD, Kothule VR, Kammon AM. Clinicopathological studies on vitamin D3 toxicity and therapeutic evaluation of aloe vera in rats. Toxicol Int. 2011;18:35–43. doi: 10.4103/0971-6580.75851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cass WA, Peters LE. Neurturin effects on nigrostriatal dopamine release and content: comparison with GDNF. Neurochem Res. 2010;35:727–734. doi: 10.1007/s11064-010-0128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hebert MA, Van Horne CG, Hoffer BJ, Gerhardt GA. Functional effects of GDNF in normal rat striatum: presynaptic studies using in vivo electrochemistry and microdialysis. J Pharmacol Exp Ther. 1996;279:1181–1190. [PubMed] [Google Scholar]
- 38.Hebert MA, Gerhardt GA. Behavioral and neurochemical effects of intranigral administration of glial cell line-derived neurotrophic factor on aged Fischer 344 rats. J Pharmacol Exp Ther. 1997;282:760–768. [PubMed] [Google Scholar]
- 39.Robertson GS, Robertson HA. Evidence that L-dopa-induced rotational behavior is dependent on both striatal and nigral mechanisms. J Neurosci. 1989;9:3326–3331. doi: 10.1523/JNEUROSCI.09-09-03326.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gerhardt GA, Cass WA, Yi A, Zhang Z, Gash DM. Changes in somatodendritic but not terminal dopamine regulation in aged rhesus monkeys. J Neurochem. 2002;80:168–177. doi: 10.1046/j.0022-3042.2001.00684.x. [DOI] [PubMed] [Google Scholar]
- 41.Andersson DR, Nissbrandt H, Bergquist F. Partial depletion of dopamine in substantia nigra impairs motor performance without altering striatal dopamine neurotransmission. Eur J Neurosci. 2006;24:617–624. doi: 10.1111/j.1460-9568.2006.04953.x. [DOI] [PubMed] [Google Scholar]
- 42.Salvatore MF, Pruett BS, Spann SL, Dempsey C. Aging reveals a role for nigral tyrosine hydroxylase ser31 phosphorylation in locomotor activity generation. PLoS ONE. 2009;4(12):e8466. doi: 10.1371/journal.pone.0008466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bowenkamp KE, Lapchak PA, Hoffer BJ, Miller PJ, Bickford PC. Intracerebroventricular glial cell line-derived neurotrophic factor improves motor function and supports nigrostriatal dopamine neurons in bilaterally 6-hydroxydopamine lesioned rats. Exp Neurol. 1997;145:104–117. doi: 10.1006/exnr.1997.6436. [DOI] [PubMed] [Google Scholar]
- 44.Zheng J-S, Tang L-L, Zheng S-S, Zhan R-Y, Zhou Y-Q, Goudreau J, Kaufman D, Chen AF. Delayed gene therapy of glial cell line-derived neurotrophic factor is efficacious in a rat model of Parkinson’s disease. Mol Brain Res. 2005;134:155–161. doi: 10.1016/j.molbrainres.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 45.Aoi M, Date I, Tomita S, Ohmoto T. The effect of intrastriatal single injection of GDNF on the nigrostriatal dopaminergic system in hemiparkinsonian rats: behavioral and histological studies using two different dosages. Neurosci Res. 2000;36:319–325. doi: 10.1016/s0168-0102(00)00097-3. [DOI] [PubMed] [Google Scholar]
- 46.Naveilhan P, Neveu I, Baudet C, Funakoshi H, Wion D, Brachet P, Metsis M. 1,25-Dihydroxyvitamin D3 regulates the expression of the low-affinity neurotrophin receptor. Mol Brain Res. 1996;41:259–268. doi: 10.1016/0169-328x(96)00103-9. [DOI] [PubMed] [Google Scholar]
- 47.Puchacz E, Stumpf WE, Stachowiak EK, Stachowiak MK. Vitamin D increases expression of the tyrosine hydroxylase gene in adrenal medullary cells. Mol Brain Res. 1996;36:193–196. doi: 10.1016/0169-328x(95)00314-i. [DOI] [PubMed] [Google Scholar]
- 48.Garcion E, Sindji L, Montero-Menei C, Andre C, Brachet P, Darcy F. Expression of inducible nitric oxide synthase during rat brain inflammation: regulation by 1,25-dihydroxyvitamin D3. Glia. 1998;22:282–294. [PubMed] [Google Scholar]
- 49.Garcion E, Sindji L, Leblondel G, Brachet P, Darcy F. 1,25-Dihydroxyvitamin D3 regulates the synthesis of γ-glutamyl transpeptidase and glutathione levels in rat primary astrocytes. J Neurochem. 1999;73:859–866. doi: 10.1046/j.1471-4159.1999.0730859.x. [DOI] [PubMed] [Google Scholar]
- 50.Shinpo K, Kikuchi S, Sasaki H, Moriwaka F, Tashiro K. Effect of 1,25-dihydroxyvitamin D3 on cultured mesencephalic dopaminergic neurons to the combined toxicity caused by L-buthionine sulfoximine and 1-methyl-4-phenylpyridine. J Neurosci Res. 2000;62:374–382. doi: 10.1002/1097-4547(20001101)62:3<374::AID-JNR7>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 51.Ibi M, Sawada H, Nakanishi M, Kume T, Katsuki H, Kaneko S, Shimohama S, Akaike A. Protective effects of 1α,25-(OH)2D3 against the neurotoxicity of glutamate and reactive oxygen species in mesencephalic culture. Neuropharmacology. 2001;40:761–771. doi: 10.1016/s0028-3908(01)00009-0. [DOI] [PubMed] [Google Scholar]
- 52.Harms LR, Burne THJ, Eyles DW, McGrath JJ. Vitamin D and the brain. Best Pract Res Clin Endocinol Metab. 2011;25:657–669. doi: 10.1016/j.beem.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 53.de Viragh PA, Haglid KG, Celio MR. Parvalbumin increases in the caudate putamen of rats with vitamin D hypervitaminosis. Proc Natl Acad Sci USA. 1989;86:3887–3890. doi: 10.1073/pnas.86.10.3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brewer LD, Porter NM, Kerr DS, Landfield PW, Thibault O. Chronic 1α,25-(OH)2vitamin D3 treatment reduces Ca2+-mediated hippocampal biomarkers of aging. Cell Calcium. 2006;40:277–286. doi: 10.1016/j.ceca.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 55.Newmark HL, Newmark J. Vitamin D and Parkinson disease – a hypothesis. Mov Disord. 2007;22:461–468. doi: 10.1002/mds.21317. [DOI] [PubMed] [Google Scholar]
- 56.Evatt ML, DeLong MR, Khazai N, Rosen A, Triche S, Tangpricha V. Prevalence of vitamin D insufficiency in patients with Parkinson disease and Alzheimer disease. Arch Neurol. 2008;65:1348–1352. doi: 10.1001/archneur.65.10.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Butler MW, Burt A, Edwards TL, Zuchner S, Scott WK, Martin ER, Vance JM, Wang L. Vitamin D receptor gene as a candidate gene for Parkinson disease. Ann Hum Genet. 2011;75:201–210. doi: 10.1111/j.1469-1809.2010.00631.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Suzuki M, Yoshioka M, Hashimoto M, Murakami M, Noya M, Takahashi D, Urashima M. Randomized, double-blind, placebo-controlled trial of vitamin D supplementation in Parkinson disease. Am J Clin Nutr. 2013;97:1004–1013. doi: 10.3945/ajcn.112.051664. [DOI] [PubMed] [Google Scholar]