Abstract
Purpose
While most studies of Duchenne muscular dystrophy (DMD) have focused on physical impairment, there is a need to explore how impairment impacts real life experiences in order to provide intervention strategies focused on participation. Objectives were: 1) to investigate the domains of participation in a sample of boys with Duchenne muscular dystrophy; 2) to compare a younger (<10 years) and older (≥10 years) group of boys with DMD with regard to participation; 3) to investigate strength and timed functional tests in a sample of boys with Duchenne muscular dystrophy; 4) to compare a younger (<10 years) and older (≥10 years) group of boys with DMD with regard to strength and timed functional tests; and 5) to explore associations between participation and strength and timed functional tests for our DMD cohorts.
Methods
This cross-sectional study included sixty boys with DMD (mean 9.3 years ±0.3). Boys completed strength testing, timed functional tests, the Children’s Assessment of Participation and Enjoyment and the ACTIVLIM. Independent samples t-tests were used to test for differences in all measures between our younger and older cohorts; Spearman’s (rank) correlation was used to assess relationships between participation and strength and time functional tests.
Results
Significant differences were found between our younger and older boys with DMD in the areas of recreational (p≤0.01), social (p≤0.001), and skill-based activities (p≤0.05), as well as with whom and where the activities were performed (p≤0.05 and 0.001, respectively). Older boys with DMD report lower levels of participation in these areas, as well as less engagement in activities with individuals other than family members and less participation outside of the home. Lower levels of strength and slower rates of functional performance correlate with participation in fewer physical activities for our younger cohort and fewer physical and social activities for our older cohort.
Conclusions
Strength and function relate to the variability and type of activities in which boys with DMD participate. A key finding is the significant decline in social activities and community-based engagement as the boys with DMD age. The ultimate goal of an intervention is for our children to be as actively engaged in life as they desire. This requires addressing participation when measuring outcomes in order to more fully understand limitations and provide appropriate strategies for continued participation for boys and their families.
Keywords: Duchenne muscular dystrophy, participation, strength outcomes, functional outcomes, social engagement
Duchenne muscular dystrophy (DMD) is an X-linked recessive disorder affecting upwards of 1 in 3500 live male births [1]. DMD is a severe, progressive disease that results in abnormal muscle function affecting early mobility and overall development. As the disease progresses, boys with DMD have increasing difficulties ambulating. They often demonstrate a waddling gait and toe walking, and the disease eventually results in a loss of ability to rise from the floor, climb stairs, and ambulate independently by the age of 13 years [2]. Death often occurs by the mid 20’s due to cardiopulmonary complications [3, 4]. Despite our understanding of the genetic basis and the functional mobility limitations intrinsic to DMD, our understanding of the impact of muscle impairment on children’s participation and social engagement is limited. The functional deterioration that occurs in DMD limits the boys’ participation in important age-related activities, which may have pronounced effects on their overall health and well-being [5].
Participation is a measureable outcome of health. This measure is defined by the International Classification of Functioning, Disability, and Health (ICF) [6] as direct engagement in a life situation. For children and youth, participation may include such activities as personal care, mobility, social relationships, education, recreation, and community life. Participation is increasingly becoming a key focus of rehabilitation programs for children through providing real-world experiences and limiting barriers to community involvement [7, 8]. Researchers have reported that children with physical disabilities engage in less varied activities than children without disabilities, most notably through less physical and social involvement [9]. Unfortunately, most studies of participation in children with disabilities have not included children with a progressive disease, such as DMD. Moreover, little is known about the participation levels of children with DMD and the various factors that may affect their participation.
While most clinical trials and natural history studies of DMD have focused on impairment measures such as strength and timed functional testing, there is a need to include a broader range of meaningful measures which are based on community participation in child focused activities. A child with DMD may demonstrate the clinical ability to walk 10 meters or climb 4 stairs in a timely manner (two commonly used clinical assessment measures for this patient population), but it is not clear that these measures are representative of actual participation in daily life activities for boys with DMD. Researchers and clinicians often infer activity limitations from pathophysiology or participation restrictions from functional limitations. However, a child’s ability to get around in school, dress himself, or play with friends is quite different from a timed clinical assessment of motor function [10]. The separate evaluation of each component and exploration of relations are essential to move forward in our understanding of the broader impact of the disease [10, 11]. Therefore, there is a need to quantify participation in boys with DMD and to examine how the changes in muscle strength and function affect participation, especially as the child ages and the disease progresses.
The objectives of this study were: 1) to investigate the domains of participation in a sample of boys with Duchenne muscular dystrophy; 2) to compare a younger and older group of boys with DMD with regard to participation; 3) to investigate strength and timed functional tests in a sample of boys with Duchenne muscular dystrophy; 4) to compare a younger and older group of boys with DMD with regard to strength and timed functional tests; and 5) to explore associations between participation and strength and timed functional tests for our DMD cohorts.
METHODS
Between April 2009 and July 2013, sixty boys with DMD (confirmed by muscle biopsies and/or genetic testing) from various geographic locations and their parent(s) were approached to participate in this study. Recruitment resulted from boys with DMD who were currently enrolled in an NIH funded natural history study. Participants and their parent(s) were approached with information regarding our study and requested they contact the lead author if they were interested in participating. Subsequently, all sixty boys and their parent(s) contacted the lead author, met inclusion criteria and were enrolled; no refusals or dropouts occurred during the study period.
Boys with DMD ranged in age from 6 to 15 years (mean 9.3 ±0.29). Three boys with DMD who were non-ambulatory were included in this study; all others were ambulatory at the time of testing. To assess the effects of disease progression, the boys with DMD were divided into two age groups (i.e., less than 10 years and 10 years or older). The age of 10 years was selected because of the disease progression and the muscle and functional changes that reportedly occur for boys with DMD around this age [2,12]. The sponsoring university’s Institutional Review Board approved the study. Written, informed consent for the research and publication of results was obtained from the parent(s), and written assent was obtained from each participant. Following informed consent, the boys completed quadriceps and plantar-flexor strength testing, as well as three timed functional tests. Two paper/pencil self-report assessments of participation were completed with the assistance of their parent(s).
Instruments
Participation was measured by the Children’s Assessment of Participation and Enjoyment (CAPE) [13]. The CAPE is designed to examine how children and youth participate in 55 varied activities. Scores on the CAPE are divided into five dimensions: 1) Diversity, the number of activities performed overall, which is scored as a “yes” or “no” option; 2) Intensity, the frequency of performing the activity, which is scored on a 1–7 continuum from “once in the last 4 months” to “every day”; 3) With Whom the activity is performed, such as alone, with family or with friends; 4) Where the activity is performed, with such responses as “at home”, “at a relatives home”, “at a friends home”, or “in the community”; and 5) how much Enjoyment the child gets from the activity, with responses on a 5-point scale from “not at all” to “very much”. Additionally, all 55 activities are divided into the following domains: physical, recreational, social, skill-based, and self-improvement. Domain scores are derived from intensity scores (frequency reports) of how often each activity is engaged in, with scores of 0=lowest participation to 7=highest participation. Physical activities include such items as playing team sports and using playground equipment. Recreational activities include reading and playing video/computer games. Social activities include visiting friends and going to the movies. Skill-based activities incorporate such activities as playing a musical instrument and participating in a community organization. Activities that are considered self-improvement include going to the public library and doing homework. King et al [14] previously established reliability and validity of the CAPE in a longitudinal study involving 427 children with a variety of physical disabilities.
The ACTIVLIM questionnaire was used to measure participation in activities of daily living. The ACTIVLIM is a Rasch developed measurement for individuals with neuromuscular disorders that explores difficulties in performing ADLs, such as bathing, toileting and dressing. Each activity is scored as easy, difficult or impossible to achieve. Scores range from 0–36 with the highest score indicting more independence in completing daily activities. The questionnaire presents with excellent psychometric qualities, including reliability, construct validity, reproducibility, linearity and unidimensionality [10].
Isometric peak torque of the knee extensors (quadriceps) and plantar-flexors of the right leg was measured using an isokinetic dynamometer (Biodex System 3 Pro, Biodex Medical Systems, Inc.). Five trials were performed, and the highest torque value (i.e. peak torque) was used for further analysis. Reliability of the strength testing methods has been previously established [15]. Three functional tasks that were timed using a stopwatch included the time to walk or run 10 meters (10m Walk/Run), rise from the floor (Supine Up), and ascend four stairs (4 Stairs) [16]. Subjects were asked to perform each task three times as fast as they could and the fastest time was recorded for analysis.
Statistical Analysis
Descriptive statistics reporting the mean and standard error of the mean (±) were used to present demographics, self-report of participation, and clinical assessments of strength and function for our cohort of boys with DMD (N=60). To assess the effects of disease progression, our boys with DMD were divided into two age groups (i.e., less than 10 years and 10 years or older). We used independent samples t-tests, with equal variances not assumed, to determine the nature of the differences in demographics, participation, strength and function between the groups. To assess the relationships between participation and clinical assessments, we used Spearman’s (rank) correlation. We used this nonparametric estimator to address the censoring on the timed and strength-related tasks. Censored data points are those whose measured properties are not known precisely, but are known to lie above or below some limiting sensitivity. For example, the boys who were unable to complete the tasks were assigned a ranking with either a slower time for functional tasks or weaker strength than those who completed the tasks. This ensured that the boys who did not complete the tasks were ranked as having less functional ability and/or strength than those able to complete the task(s). Although we had three boys with DMD who were non-ambulatory, they were able to complete the two reports of participation and all strength testing measures. In addition to these three non-ambulatory boys, one boy with DMD was unable to complete the 10m Walk/Run, and six boys were unable to complete the Supine Up test. Inability to complete these tests was based on the child being physically unable to accomplish the task. Each of these unknown data points was censored in our data.
RESULTS
Demographics
All demographic variables of age, height, body weight, and body mass index (BMI) are significantly different (p≤0.001) between our younger (<10 years) and older boys with DMD (table 1).
Table 1.
Demographic variables and comparisons between younger and older boys with DMD.
| DMD < 10 (n=35) | DMD ≥ 10 (n=25)*** | |
|---|---|---|
| Age (years) | 7.5 ±0.25 | 11.08 ±0.29 |
| Height (cm) | 118.4 ±2.5 | 136.7 ±2.90 |
| Weight (kg) | 24.1 ±0.92 | 42.0 ±1.23 |
| Body Mass Index (kg/m2) | 17.1 ±0.37 | 22.1 ±0.40 |
Means ± standard error of the means presented.
All significant at p≤0.001.
Comparison of self-report of participation
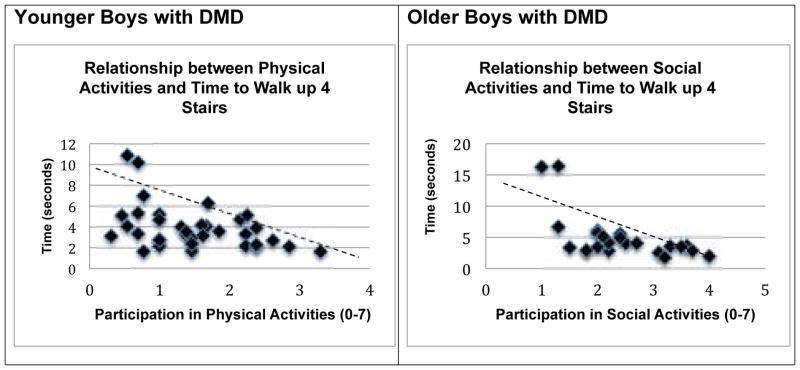
Report of daily participation (CAPE) in physical, recreational, social, self-improvement and skill-based activities, as well as who the activities were performed with, where the activities were performed, and how much they enjoyed the activities is presented for our compete sample of DMD participants (table 2). Participation scores were compared between our younger and older DMD cohorts using independent samples t-tests, with equal variances not assumed. Significant differences were found between our younger (n=35) and older boys (n=25) with DMD in the areas of recreational (p≤0.01), social (p≤0.001), and skill-based activities (p≤0.05), as well as with whom and where the activities were performed (p≤0.05 and 0.001, respectively). Older boys with DMD report lower levels of participation in these areas, as well as less engagement in activities with individuals other than family members and less participation outside of the home (figure 1).
Table 2.
Report of Participation (CAPE) for boys with DMD (N=60).
| CHILDREN’S ASSESSMENT OF PARTICIPATION AND ENJOYMENT | |||||||
|---|---|---|---|---|---|---|---|
| ACTIVITY DOMAINS | ACTIVITY DIMENSIONS | ||||||
| Physical | Recreational | Social | Skill- Based | Self- Improvement | With Whom | Where | Enjoyment |
| 1.38 ±0.09 | 4.63 ±0.14 | 2.98 ±0.10 | 1.09 ±0.08 | 3.04 ±0.09 | 2.49 ±0.06 | 2.57 ±0.05 | 4.03 ±0.06 |
Score 0=lowest participation to 7=highest participation. Means ± standard error of the means presented.
Figure 1.
Children’s Assessment of Participation and Enjoyment (CAPE) report of scores in participation for younger (n=35) and older (n=25) boys with DMD. Score 0=lowest participation to 7=highest participation. Means ± standard error of the mean presented.
*p≤0.05; **p≤0.01; ***p≤0.001.
Report of independence in completing a variety of activities of daily living, as measured through the ACTIVLIM, was compared using independent samples t-tests, with equal variances not assumed. Scores ranged from 15 (dependent) to 36 (independent), with a mean of 29.4 ±0.68. No significant differences were observed between our two DMD cohorts.
Comparison of clinical assessments
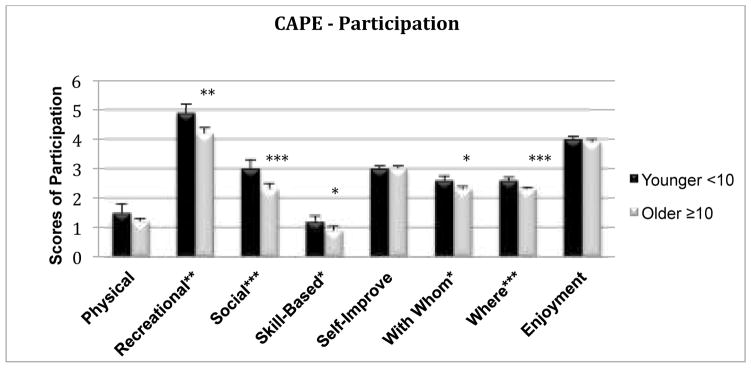
Significant differences in strength of the lower leg muscles (plantar-flexor peak torque) were observed between our two DMD cohorts (p≤0.05). When examining timed functional tests (figure 2), older boys with DMD scored significantly slower in the 10m Walk/Run and the Supine Up than their younger cohort (p≤0.05); no other significant timed functional differences were observed between these two groups.
Figure 2.
Timed functional tests measured in seconds: Time to walk or run 10-meters (10m walk/run), time to rise from the floor (SupineUp), and time to walk up 4 stairs (4 Stairs). Includes censored data. Means ± standard error of the mean presented. * p<0.05.
Relationships between participation and clinical assessments
Spearman’s rho correlation coefficients were calculated to determine relationships between participation and clinical assessments of strength and function in our two groups of boys with DMD. In our full cohort of boys (N=60), moderate negative correlations between report of participation in physical activities (CAPE) and all timed functional tests (10m Walk/Run r=−0.35, p≤0.01; Supine Up r=−0.42, p≤0.001; 4 Stairs r=−0.44, p≤0.001) were observed. A positive correlation was found between participation in physical activities and strength in the upper leg muscles (quadriceps peak torque) (p<0.01; r= 0.32).
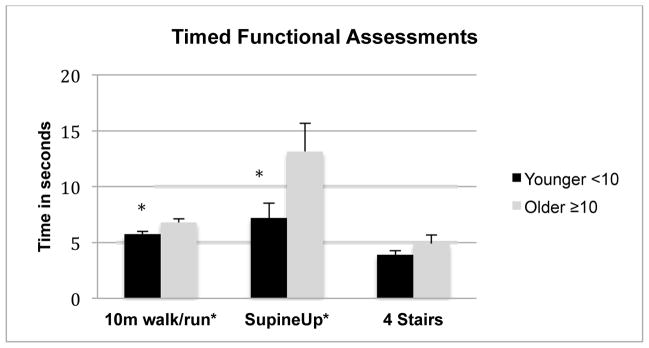
Relationships with participation and clinical assessments appear to change as the boys age and the disease progresses. For our younger cohort of boys with DMD, participation in physical activities was negatively correlated with timed functional tasks of 10m Walk/Run (r=−0.34), Supine Up (r=−0.39) and 4 stairs (r=−0.40) (all p≤0.05). For our older boys with DMD, a negative relationship with participation in physical activities and the time to walk up 4 stairs was observed (r=−0.44, p≤0.05), as well as with participation in social activities and the time to walk up 4 stairs (r=−0.46, p≤0.05) (figure 3).
Figure 3.
Correlation between participation in physical activities (CAPE) and time to walk up 4 stairs for younger boys with DMD (r=−0.40, p ≤0.05). Correlation between participation in social activities (CAPE) and time to walk up 4 stairs for older boys with DMD (r= −0.46; p≤0.05). Does not include censored data. Dashed line (trend) provided for visual purposes only.
DISCUSSION
Our study is one of the first to report participation in real life activities for younger and older boys with DMD and to investigate the relationships between participation and traditional clinical measures. Findings from this study assist in our understanding of how impairments at the body structure and function level may relate to actual participation in life activities.
Overall report of participation for our boys with DMD demonstrates low levels of engagement in physical activities. Physical activities included playing team and non-team sports, doing martial arts and gardening. Based on our understanding of the muscle weakness and mobility difficulties in boys with DMD, this is not a surprising finding. Our boys also report very low levels of participation in skill-based activities, which focused mainly on activities that require taking lessons in order to learn new skills. Skill-based activities included swimming lessons, dancing lessons, art and music lessons. Past research on the CAPE has shown that both boys and girls with physical limitations report lower levels of engagement in skill-based activities than recreational, social or self-improvement type activities [17]. Our boys with DMD reported moderate engagement in recreational, social and self-improvement activities. Examples of recreational activities included doing puzzles, playing board games and playing with computer or video games. Report of participation in recreational activities was the highest for our group, with more than 96% engaging in video or computer games at least weekly. Unfortunately, the playing of computer/video games was typically done at home and alone, although there was anecdotal report of boys playing computer games with friends who were remote. Boys with DMD participated in self-improvement activities at approximately the same intensity as social activities. Social activities focused on being with others through visiting, going to a party or going to the movies. Self-improvement activities included reading, doing homework and doing a household chore. We also explored the CAPE activity dimensions of where the child does the activity, with whom they do the activity, and how much they enjoy the activity. Boys with DMD appear to engage in most activities with their family or with a relative, and engage more often within their own homes or relative’s home than a friend’s house or in the community. Importantly, even though overall participation in activities and community engagement was limited, most boys reported high levels of enjoyment in the activities they did engage in.
An objective of this investigation was to compare a younger and older group of boys with DMD with regard to participation. We observed that participation in activities that were physical in nature, as well as self-improvement activities, such as doing homework, was comparable between our younger boys with DMD (<10 years) and our older cohort (≥10 years). In contrast, participation in activities that were recreational, social, and skill-based in nature was significantly lower for our older boys with DMD. An additional crucial finding was the substantial decline in community-based participation for our older cohort. It appears that as boys with DMD age, additional social isolation occurs, as their time spent with friends or engaging in the community decreases significantly.
Our study group also participated in clinical assessments of strength and timed functional tasks. In comparison, results support past research that has shown that boys with DMD demonstrate greater muscle weakness and are significantly slower in performing timed functional tests than unaffected controls, even at a young age [16]. When comparing our two cohorts, a significant difference in plantar-flexor (PF) strength was observed, with younger boys presenting with higher levels of PF peak torque than our older boys. Plantar flexor strength is important for trunk support and forward progression during propulsion for normal walking and running. Research has demonstrated the decline in walking and running ability for boys with DMD as they age [18–19]. This decline was also observed in our study, as younger boys with DMD were significantly quicker to complete the timed test of 10 meter walk/run than their older cohort. In addition, older boys with DMD were considerably slower in their ability to rise from the floor (Supine Up). In fact, nine of our boys (3 non-ambulatory) were unable to complete this timed activity. Supine Up has been observed to be one of the first clinically-based tasks that boys with DMD lose the ability to accomplish [18].
An important aim of this study was to investigate possible associations between daily real-life participation and traditional clinical assessments of strength and timed functional tests for our cohorts. Although there is an assumption that physical limitations and disability resulting from DMD have pronounced effects on the boys’ participation choices and activity level [20,21], participation is rarely measured and little is known about its actual link to clinically-based assessments. In our large cohort of boys, correlational analyses suggest that boys who possess lower levels of strength (quadriceps muscles) participate less in physically-based activities such as swimming or bicycling. In addition, all timed functional tests had a negative correlation with participation in physical activities. Hence, as boys with DMD require more time to complete certain tasks such as walking up a few stairs or getting up off the floor, they participate less in physical activities that require them to utilize their lower extremities such as climbing playground equipment or playing sports.
For this objective, we also separately analyzed our two groups (younger (n=35) and older (n=25)) in order to observe relationships between participation and clinical assessments, which may change as the boys age. When exploring relationships with timed functional tests, moderate negative correlations between participation in physical activities and all timed functional tests were observed in our younger boys with DMD. Consequently, even for our youngest children with DMD, physical limitations are often evident and lead to a decrease in active engagement. Active engagement is important for both developmental and social growth. What we don’t know is whether these boys are choosing not to participate in physical activities because they are unable to keep up with their peers, or because of social or environmental barriers, which preclude them from participation. This is an important question and worthy of further inquiry.
Interestingly, for our older cohort (≥10 years), the increase in the amount of time required to walk up stairs was significantly related to a decrease in both participation in physical activities, as well as social activities. At approximately 10–12 years of age, physical changes are most dramatic for boys with DMD and may therefore have the most substantial impact on their social activities [5]. This decrease in social engagement comes at a time when boys are often strengthening friendships, and building confidence and self-esteem through competitive physical sports. Obstacles to participation and environmental limitations may further compound the sense of difference and lead to boys with DMD being left out of activities that simple modifications may provide access to. Choices for these boys are often limited. Therapeutic interventions that provide opportunities to develop “team spirit”, self-discipline and social connections may help to raise self-esteem and reduce social isolation for these boys. Continued ability to participate in activities (engaging in sports or as a spectator of sports) provides the opportunity to engage with one’s peer group and socialize with others who have the same interests [22]. Sports and physical activities can be enjoyed on many different levels. Determining ways to include children with DMD allows them to continue to foster social interactions, share experiences and maintain connections with their peers, all developmentally important skills.
The proper monitoring of disease progression in boys with DMD is essential for health maintenance and preventive care [23]. The neuromuscular assessments utilized in this study are psychometrically robust measures, which have traditionally been used to monitor change in physical status and response to treatment interventions in boys with DMD [16,24–25]. Traditional assessments of disease progression, such as muscle strength and timed testing, are one means to detect therapeutic changes. The Food and Drug Administration of the United States (FDA) has challenged the research community to demonstrate how changes in strength and function actually correlate with “life altering events” [26]. The FDA emphasized a need for surrogate measures that predict clinically meaningful outcomes, such as the link described between the time to walk/run and time to transition to a wheelchair [26]. Participation’s relationship with these clinical measures may provide information concerning what boys with DMD are able to accomplish in their natural environment and the real life impact of disease progression.
Based on our findings, we are assuming that our boys with DMD may be making decisions about participation based on their strength and functional abilities. It would be important to compare these results to an unaffected cohort to determine if this assumption remains true and are their choices clearly related to growing up with a neuromuscular disorder. Although we had a large sample of boys with DMD, it would be important to utilize a more diverse group of boys with DMD to examine how participation can be affected in boys who are ambulatory, boys as they transition to a wheelchair, and boys who have been non-ambulatory for a longer period of time. As our study was a cross-sectional research design, another focus for future research would be to longitudinally examine how an individual’s choice of participation changes across time.
CONCLUSION
Traditional clinical assessments of neuromuscular function provide important information that can be analyzed to show progression of pathological muscle weakness over time. Physical limitations are an important aspect of DMD and timely assessment and monitoring are necessary, but the results may have little meaning for the child with DMD and his parents. The ability to move beyond medical settings and assess and monitor a child’s daily activities through participation measures may provide information for therapeutic interventions. It’s important that we acknowledge the value of outcomes that explore the more distal elements of the diagnosis, such as participation. Although participation in activities may involve factors that are less related to traditional health care (personal choices, motivation, familial factors), the ultimate goal of an intervention is for our children to be as actively engaged in life as they desire. Rehabilitation specialists have a role as advocates for social and community engagement for children with physical limitations. This requires that families are provided with information on community-based opportunities, and the strategies and environmental modifications available to allow their children to participate. This also requires addressing participation when measuring outcomes [27].
Acknowledgments
The authors would like to thank the children and families who gave their time to participate in this study. We would also like to acknowledge Dr. Michael Daniels for his statistical support.
Footnotes
Declaration of Interests
The project described was supported by Award Number K01HD064778 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National institutes of Health. Additional funding for recruitment and participant support was provided through Parent Project Muscular Dystrophy, the Muscular Dystrophy Association, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases, and National Institute of Neurological Disorders and Stroke (PI, K. Vandenborne – R01AR056973). All authors report no further declarations of interest.
Contributor Information
Roxanna M. Bendixen, Department of Occupational Therapy, University of Pittsburgh.
Donovan J. Lott, Department of Physical Therapy, University of Florida.
Claudia Senesac, Department of Physical Therapy, University of Florida.
Sunita Mathur, Department of Physical Therapy, University of Toronto.
Krista Vandenborne, Department of Physical Therapy, College of Public Health & Health Professions, University of Florida.
References
- 1.Deconinck N, Dan B. Pathophysiology of duchenne muscular dystrophy: Current hypotheses. Pediatric Neurology. 2007;36:1–7. doi: 10.1016/j.pediatrneurol.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 2.Emery A, Muntoni F. Duchenne muscular dystrophy. 3. Oxford: Oxford University Press; 2003. [Google Scholar]
- 3.Wren TAL, Bluml S, Tseng-Ong L, Gilsanz V. Three-point technique of fat quantification of muscle tissue as a marker of disease progression in Duchenne muscular dystrophy: Preliminary study. American Journal of Roentgenology. 2008;190:W8–W12. doi: 10.2214/AJR.07.2732. [DOI] [PubMed] [Google Scholar]
- 4.Bogdanovich S, Perkins KJ, Krag TOB, Khurana TS. Therapeutics for Duchenne muscular dystrophy: current approaches and future directions. Journal of Molecular Medicine-Jmm. 2004;82:102–15. doi: 10.1007/s00109-003-0484-1. [DOI] [PubMed] [Google Scholar]
- 5.Bendixen RM, Senesac C, Lott DJ, Vandenborne K. Participation and quality of life in children with Duchenne muscular dystrophy using the International Classification of Functioning, Disability, and Health. Health and Quality of Life Outcomes. 2012;10 doi: 10.1186/1477-7525-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) International Classification of Functioning, Disability and Health. Geneva, Switzerland: WHO; 2001. [Google Scholar]
- 7.King G, Law M, Hanna S, et al. Predictors of the leisure and recreation participation of children with physical disabilities: A structural equation modeling analysis. Child Health Care. 2006;35:209–34. [Google Scholar]
- 8.Whiteneck G, Dijkers MP. Difficult to Measure Constructs: Conceptual and Methodological Issues Concerning Participation and Environmental Factors. Archives of Physical Medicine and Rehabilitation. 2009;90:S22–S35. doi: 10.1016/j.apmr.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Coster W, Bedell G, Law M, et al. Psychometric evaluation of the Participation and Environment Measure for Children and Youth. Developmental Medicine and Child Neurology. 2011;53:1030–7. doi: 10.1111/j.1469-8749.2011.04094.x. [DOI] [PubMed] [Google Scholar]
- 10.Vandervelde L, Van den Bergh PYK, Goemans N, Thonnard JL. ACTIVLIM: A Rasch-built measure of activity limitations in children and adults with neuromuscular disorders. Neuromuscular Disorders. 2007;17:459–69. doi: 10.1016/j.nmd.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Bostrom K, Ahlstrom G. Living with a chronic deteriorating disease: the trajectory with muscular dystrophy over ten years. Disability and Rehabilitation. 2004;26:1388–98. doi: 10.1080/0963-8280400000898. [DOI] [PubMed] [Google Scholar]
- 12.Chamberlain J, Rando T. Duchenne muscular dystrophy: Advances in therapeutics. New York: Taylor & Francis Group; 2006. [Google Scholar]
- 13.King G, Law M, King S, et al. Children’s Assessment of Participation and Enjoyment (CAPE) and Preferences for Activities of Children (PAC) San Antonio: TX: Harcourt Assessment, Inc; 2004. [Google Scholar]
- 14.King G, Law M, King S, Rosenbaum P, Kertoy MK, Young NL. A conceptual model of the factors affecting the recreation and leisure participation of children with disabilities. Phys Occup Ther Pediatr. 2003;23:63–90. [PubMed] [Google Scholar]
- 15.Mathur S, Lott DJ, Senesac C, et al. Age-related differences in lower-limb muscle cross-sectional area and torque production in boys with Duchenne muscular dystrophy. Archives of Physical Medicine and Rehabilitation. 2010;91:1051–8. doi: 10.1016/j.apmr.2010.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McDonald CM, Abresch RT, Carter GT, et al. Profiles of neuromuscular diseases. Duchenne muscular dystrophy. Am J Phys Med Rehabil. 1995;74:S70–92. doi: 10.1097/00002060-199509001-00003. [DOI] [PubMed] [Google Scholar]
- 17.King GA, Law M, King S, Hurley P, Hanna M, Kertoy M, et al. Measuring children’s participation in recreation and leisure activities: construct validation of the CAPE and PAC. Child: Care, Health and Development. 2006;33(1):28–39. doi: 10.1111/j.1365-2214.2006.00613.x. [DOI] [PubMed] [Google Scholar]
- 18.Beenakker EA, Maurits NM, Fock JM, Brouwer OF, van der Hoeven JH. Functional ability and muscle force in healthy children and ambulant Duchenne muscular dystrophy patients. European Journal of Paediatric Neurology. 2005;9:387–393. doi: 10.1016/j.ejpn.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Lerario A, Bonfiglio S, Sormani M, Tettamanti A, Marktel S, Napolitano S, et al. Quantitative muscle strength assessment in duchenne muscular dystrophy: Longitudinal study and correlation with functional measures. BMC Neurology. 2012;12:91–98. doi: 10.1186/1471-2377-12-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newacheck PW, Halfon N. Prevalence and impact of disabling chronic conditions in childhood. American Journal of Public Health. 1998;88:610–7. doi: 10.2105/ajph.88.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Law M, King G, King S, et al. Patterns of participation in recreational and leisure activities among children with complex physical disabilities. Developmental Medicine and Child Neurology. 2006;48:337–342. doi: 10.1017/S0012162206000740. [DOI] [PubMed] [Google Scholar]
- 22.Chawla JC. ABC of Sports Medicine - Sport for people with disability. British Medical Journal. 1994;308:1500–4. doi: 10.1136/bmj.308.6942.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bushby K, Finkel R, Birnkrant DJ, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and pharmacological and psychosocial management. Lancet Neurology. 2010;9:77–93. doi: 10.1016/S1474-4422(09)70271-6. [DOI] [PubMed] [Google Scholar]
- 24.Brooke MH, Griggs RC, Mendell JR, Fenichel GM, Shumate JB, Pellegrino RJ. Clinical-Trial in Duchenne Dystrophy. 1. The Design of the Protocol. Muscle & Nerve. 1981;4:186–97. doi: 10.1002/mus.880040304. [DOI] [PubMed] [Google Scholar]
- 25.Scott E, Mawson SJ. Measurement in Duchenne muscular dystrophy: considerations in the development of a neuromuscular assessment tool. Developmental Medicine and Child Neurology. 2006;48:540–4. doi: 10.1017/S0012162206001137. [DOI] [PubMed] [Google Scholar]
- 26.Mendell JR, Csimma C, McDonald CM, et al. Challenges in drug development for muscle disease: a stakeholders’ meeting. Muscle & Nerve. 2007;35:8–16. doi: 10.1002/mus.20686. [DOI] [PubMed] [Google Scholar]
- 27.Bendixen RM, Kreider CM. Review of Occupational Therapy Research in the Practice Area of Children and Youth. American Journal of Occupational Therapy. 2011;65:351–9. doi: 10.5014/ajot.2011.000976. [DOI] [PMC free article] [PubMed] [Google Scholar]