Abstract
In response to the global rise in obesity, bariatric surgery has become increasingly more popular and successful. As a result, the demand for body contouring following massive weight loss is rapidly growing. Although bariatric procedures may produce impressive weight loss, people who achieve massive weight loss are often unhappy with the hanging folds of skin and subcutaneous tissue that remain. This review examines the nature of the post-bariatric deformity in each body region and briefly reviews common approaches to their treatment.
Keywords: Weight loss, Bariatric surgery, Body contour surgery
INTRODUCTION
As we enter the 21st century, a new health crisis has dawned upon affluent western societies, the plague of obesity. In the United States, the situation is particularly acute with recent estimates showing that nearly 65% of adult Americans (127 million) are over their ideal body weight, 30% (48 million) are obese [Body mass index (BMI) ≥ 30], and nearly 5% (9 million) are morbidly or severely obese (BMI ≥ 40)[1]. Further, the obesity epidemic has expanded globally, with approximately one-fifth of the one billion overweight or obese people in the world being Chinese[2]. Although the ultimate impact of mild obesity on survival has recently been challenged, there is no doubt that morbid or severe obesity is detrimental to both the physical and psychological well being of the afflicted patient[3,4]. Morbidly obese patients have often reached a point of no return in which they are too large and physically unable to exercise.
With some exceptions, the feed-forward cycle of weight gain in the morbidly obese can be interrupted only by physically restricting oral intake. This surgical subspecialty, known as bariatric surgery, has exploded in popularity in the last decade largely because of improved outcomes, enhanced patient safety and superior techniques and devices[5,6]. Although early bariatric procedures produced impressive weight loss, they also resulted in significant morbidity both initially because of wound healing problems and anastomotic leakage, and ultimately as a result of their malabsorptive effects[7]. Modern laparoscopic surgical approaches have minimized wound healing morbidity, while the improvement of more restrictive procedures, such as the minimally invasive LAP-Band®, have made weight loss surgery in morbidly obese patients a reliable and relatively safe procedure[8-12]. According to the most recent available data, approximately 170 000 bariatric surgeries were performed in the United States in 2005[13].
However, for the morbidly obese patient, the massive weight loss that follows successful bariatric surgery is only the first step in the process[14]. After massive weight loss, patients are left “deflated”. The excess skin that hangs from the torso, abdomen and extremities is not only extremely unsightly, but can be painful and susceptible to recurrent intertriginous infections[15,16]. In order for these patients to complete their transformation to a formerly morbidly obese patient, a plastic surgeon must address the deformities resulting from the massive weight loss[17].
This type of extreme body contouring has grown concomitantly with the popularity of bariatric surgery, with 55 927 procedures performed in 2004[18]. More than just excising excess skin and subcutaneous tissue, post-bariatric body contouring requires unique insights into the nature of the post-bariatric deformities[19]. In addition, there must be an appreciation of the fact that massive weight loss patients, because they are often relatively malnourished or anemic, constitute a distinct surgical cohort that must be carefully evaluated pre-operatively[20,21]. In the following sections, we will examine the nature of the post-bariatric deformity in each body region and briefly review common approaches to their treatment.
TORSO/ABDOMEN
In formulating a strategic approach to the massive weight loss patient, the abdomen is usually the first body territory addressed. The appropriate surgical intervention depends upon the amount and distribution of excess skin and subcutaneous tissue as well as the degree of abdominal wall laxity/integrity. In general, as the amount of weight loss increases, so does the aggressiveness of the surgical intervention.
For skin excess limited to the anterior abdomen, as might occur after moderate weight loss or pregnancy, a traditional abdominoplasty will suffice. In this procedure, the skin and subcutaneous tissue between the umbilicus and pubis is excised in an elliptical pattern, leaving a scar concealed within the underwear/bikini line[22]. Since there is usually an associated abdominal wall laxity, prior to closing the incision, the anterior abdominal fascia is plicated, with particular emphasis on re-creation of an appropriate waist in females[23] (Figure 1A-D).
Figure 1.
Typical frontal (A) and lateral (B) appearance of the anterior abdominal wall of a (non-weight loss) post-partum female. In addition to excess skin and subcutaneous tissue, there is significant laxity of the anterior abdominal wall of this 50-year-old female; C and D: Post-operative appearance several months after standard abdominoplasty.
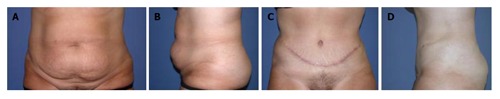
In some weight loss patients, the resulting abdominal pannus consisting of loose hanging skin and subcutaneous tissue can be the source of significant discomfort, recurrent infection and difficulty with personal hygiene[15]. A simple elliptical excision of the pannus, which can weigh 25 kg or more, can provide immediate relief of the aforementioned symptoms, with minimal morbidity[24]. In addition, a panniculectomy is often the only post weight loss surgery that may be covered by a third party payer[25] (Figure 2A-D).
Figure 2.

Typical frontal (A) and lateral (B) pre-operative appearance of a panniculectomy candidate; This 41-year-old patient is status post a 60-lb weight loss. In addition to the unsightly appearance, the hanging pannus can be the source of pain and recurrent infection. Removal of the pannus (in this case with umbilical translocation) even without plication of the underlying abdominal wall resulted in significant improvement in contour and relief of symptoms (C and D). The patient also underwent a concurrent bilateral mastopexy.
In most massive weight loss patients, however, the excess skin and subcutaneous tissue is not confined solely to the anterior abdomen[26,27]. In order to excise this “cone-like” circumferential excess, a circumferential excision or “belt lipectomy” is required[28,29]. The amount of tissue removed is tailored to the individual patient’s needs. An optimal excision will not only tighten and flatten the lower abdomen but will also give a beneficial lift to the buttocks, mons pubis and lateral thighs[29] (Figure 3A-D).
Figure 3.

A 34-year-old female status post 120-lb weight loss. Note the deflated, empty breasts and excess anterior abdominal skin and subcutaneous tissue anteriorly (A) and the excess skin and subcutaneous tissue posteriorly as well as the sagging buttocks (B); One month after circumferential abdominoplasty (and bilateral brachioplasty), there is significantly improved contour with re-creation of a feminine waistline (C); In addition, the buttocks have been lifted as a result of the circumferential excision (D). The patient is awaiting bilateral breast augmentation and bilateral medial thigh lift.
In some patients (usually those with the most significant excess), the circumferential excision alone is not sufficient to address the horizontal dimension of the excess tissue. In these patients, an anterior ellipse or fleur-de-lis pattern of excision is required[30,31]. For patients who have had previous “open” bariatric surgery (and therefore already have a vertical midline scar), the additional scar burden is minimal. Even for patients without a pre-existing midline scar, the trade-off for optimal abdominal contour is usually acceptable.
Massive weight loss patients undergoing abdominal contouring procedures often have associated abdominal hernias which are not always evident on pre-operative physical exam[32,33]. The surgeon should be prepared to repair these in the course of the abdominal contouring. General complications of abdominal contouring include skin necrosis, persistent paresthesias of the abdominal wall, seroma, infection and wound dehiscence[16,34-36]. Patients are encouraged to refrain from smoking for at least 3 wk prior to surgery, as tobacco use has been shown to significantly increase the morbidity of body contouring procedures[37].
UPPER TORSO/BREAST
Following massive weight loss, in both males and females, excess rolls (sometimes three or more per side) of skin and subcutaneous tissue remain. Because of firm underlying fascial attachments, though these may be improved somewhat by belt lipectomy[29,38], they can only be completely ablated by direct excision[26]. Usually, the deformity caused by these folds is significant enough that patients are willing to trade a horizontal scar across the upper back (hidden in the bra line in females). Furthermore, in women this excess tissue may be transferred anteriorly and used for autologous breast augmentation (see breast discussion below)[39,40].
The major deformity of the breast after massive weight loss in both men and women is ptosis or sagging of the breast which leaves the nipple areola complex (NAC) below its appropriate anatomic position. In males, the aim is to excise the excess skin and subcutaneous tissue while maintaining a flat breast profile[41]. Various patterns of excision exist to achieve this goal. In extreme cases where the NAC must be moved a long distance superiorly (more commonly in females), it can be removed and replaced as a full thickness skin graft[42]. Patients must be warned that this will cause the NAC to become insensate and may lead to de-pigmentation[43].
Although the NAC can be returned to its normal anatomic position by various means (at the level of the inframammary fold for women), a major challenge in female weight loss patients is recreation of breast fullness and projection. In most cases of massive weight loss, women are left with deflated empty “pancake” breasts. For female patients, the goal is to excise excess breast envelope skin while preserving as much volume as possible.
For most massive weight loss patients, satisfactory volume and projection can only be achieved with breast implants placed in combination with a breast lifting skin excision or mastopexy[19,32,39,44] (Figure 4A-D). The choice of implant used for breast augmentation is currently limited to saline-filled, silicone-shelled devices or (for surgeons involved in certain manufacturer study protocols) silicone-filled, silicone-shelled devices (since 1992 the Food and Drug Administration (FDA) has banned the routine use of silicone-filled implants in the United States, although they remain largely the implants of choice in Europe and the rest of the world and are available to a handful of surgeons in the United States who are part of ongoing clinical trials concerning their use).
Figure 4.
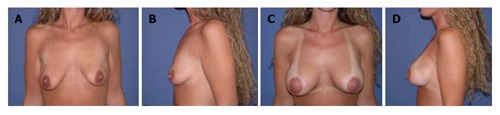
Pre-operative appearance of a 23-year-old post-partum female after 60 lb weight loss. The breasts are deflated and ptotic (A and B). Status post bilateral breast augmentation (with saline prostheses) and right sided circumareolar mastopexy (C and D). Note the improved projection, especially in the upper pole. Additionally, the pre-operative asymmetry has been corrected.
The most common complication of these devices (regardless of the implant filler material used) is capsular contracture, in which excessive fibrous scar tissue forms around the implant leading to firmness, distortion of the implant and pain[45,46]. Implant removal or revision of excessive scar tissue may be required in 15%-35% of cases[46,47]. Other known but less frequent complications of breast implants are infection, malposition and rupture[45]. Breast implants have not been shown to cause autoimmune disorders[48,49] or increase the risk of (delayed detection) of breast cancer, although special mammographic views may be required[50-52].
In some patients, autologous volume augmentation can be achieved by recruiting local folds of tissue that might be otherwise excised in the course of body contouring. Most commonly the excess folds of the upper lateral chest or back tissue are de-epithelialized and rotated anteriorly into the breast[39,40]. Other surgeons utilize excess tissue on the upper anterior abdomen from a “reverse abdominoplasty”. Common complications of breast lift with or without autologous augmentation are hematoma, infection, seroma and changes in NAC appearance and sensitivity (although many massive weight loss patients have little or no NAC sensitivity pre-operatively)[53-55]. In rare instances, the NAC may be partially or totally lost secondary to ischemic changes caused by surgery and patients should be fully informed pre-operatively[56] of this unfortunate possibility.
EXTREMITIES
Contour deformities of the extremities after massive weight loss can be quite significant. Large amounts of excess skin draped from the proximal half of the arm gives the appearance of a “bat wing”, while excess skin hanging from the thigh is unsightly and prevents patients from wearing bathing suits and shorts[19]. The unsightly appearance of their extremities will often prompt patients to wear long sleeves and pants at all times. To correct these deformities, the excess tissue must be directly excised. The pattern of excision used is similar for both the arms and the legs, since the deformity is essentially the same (a circumferential excess)[26,57,58].
For patients with a mild excess of tissue, the incision can usually be hidden in either the axilla (for a brachioplasty or arm lift)[59] or the groin (for a thigh lift)[60-62] using an elliptical pattern of excision perpendicular to the long axis of the extremity. This type of excision (“mini” brachioplasty or thigh lift) is usually insufficient to correct the amount of excess skin present in most massive weight loss patients[63].
For more significant deformities, an ellipse parallel to the longitudinal axis of the extremity is utilized, with or without the aforementioned perpendicular ellipse[58] (Figure 5A-D). Although this approach can provide remarkable improvement, brachioplasty scars are long and tend to hypertrophy[64,65]. Furthermore, contractures across the axilla may occur despite use of “z-plasty” designs. For brachioplasty, the longitudinal scar is best placed along the medial surface of the upper arm where it is not visible while the patient’s arms are at rest[32,66,67]. Similarly, for thigh lifts a scar is best placed medially along the thigh, although some surgeons advocate use of an anteriorly or laterally based excision[62,68,69]. Patients must be thoroughly counseled regarding the inevitable scars as well as other common complications, such as persistent edema, parasthesias and dysesthesias as well as delayed wound healing, particularly in the groin area[62].
Figure 5.
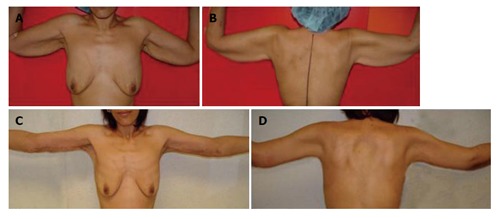
Typical appear-ance of upper extremity deformity after massive weight loss. Note the “bat-wing” appearance of the proximal arm (A and B); One month after brachioplasty, there is significant improvement in contour (C and D). The incision is designed to keep the resultant scar on the medial surface of the upper extremity so that it is hidden when the patient stands at rest with her arms at her side.
SUCTION-ASSISTED LIPECTOMY (LIPOSUCTION, SAL)
Although some patients may experience an evenly distributed massive weight loss resulting in a relatively thin layer of subcutaneous tissue throughout their body, for most patient this is not the case. In order to address these recalcitrant adipose deposits which are common in the upper abdomen, back, flanks, arms and legs, plastic surgeons utilize suction-assisted lipectomy (SAL), more commonly known as liposuction[70]. Liposuction is not for weight loss, although as much as 6-8 liters or more of fat may be removed safely in a single session[71]. Liposuction is used to “sculpt” areas of the body that need further refinement in their contour. SAL, like most procedures, is effective and safe when performed by a board certified plastic surgeon in an appropriately monitored setting. Although SAL alone is commonly performed as an ambulatory procedure, when more than 5 liters of lipoaspirate is removed in one session, the procedure is considered “large volume” liposuction and overnight monitoring is required[71]. SAL may be used concurrently with any of the above mentioned contouring procedures, or may be used afterwards to fine tune the results. Although not very painful, liposuction can prolong swelling and edema when used in conjunction with other body contouring procedures. A less frequent complication of SAL is persistent seroma. Transient paresthesias and bruising may also occur after SAL[72].
SEQUENCE OF SURGERY
Body contouring after massive weight loss is a significant undertaking on the part of both the surgeon and the patient. As stated earlier, many of these patients are chronically malnourished which predisposes them to increased surgical morbidity[21,73]. The surgery itself is laborious and sometimes involves considerable blood loss. For these reasons, most surgeons stage the procedures[19]. Usually the abdomen and torso are treated first and, in less severe cases, may be combined with brachioplasty, thigh lift and or breast lift. The number of procedures performed at one time depends upon the health of the patient and the number of surgeons available. In centers where a “total body lift” is performed, two teams operating simultaneously are mandatory to limit time under anesthesia, although such procedures may still take eight or more hours[39].
As mentioned previously, special consideration must be given to the massive weight loss patient, since they are often relatively malnourished and even anemic secondary to their weight loss. Although severe complications such as pulmonary embolism or even death are relatively rare (0.02% or less)[74], minor complications such as seroma, infection or delayed wound healing are common with some surgeons reporting a greater than 70% total complication rate, especially in refractory smokers[16]. However, most patients will gladly trade these minor complications for the significant improvements in their body contour and by direct extension, their self image and confidence.
MOLECULAR ADVANCES IN WEIGHT LOSS
Few drugs remain approved for weight loss. The dearth of pharmaceutical solutions is not for a lack of effort on the part of medical researches, but rather the complex nature of obesity. Most promising advances in weight loss technology surround the hormones leptin and ghrelin, and the peptide known as PYY. These molecules all help regulate mechanisms of obesity. Currently, pharmaceutical companies are developing a variety of compounds to modulate the effects of these compounds.
CONCLUSION
Body contouring after bariatric surgery is currently the fastest growing field within plastic surgery[75]. At the same time, body contouring after massive weight loss continues to evolve as surgeons refine patient selection, technique, and improve safety. However, the surge in weight loss-related surgeries has resulted in ethical questions, such as who should be treated, which operation is best, and who should be performing the surgeries. For these reasons, national consortiums have been founded to develop consensus responses to some of these questions. Meanwhile, though post-bariatric surgery is associated with a greater frequency of complications than “traditional” body contouring, the major transformation imparted by these procedures results in a high degree of patient satisfaction.
Footnotes
S- Editor Liu Y L- Editor Kumar M E- Editor Bai SH
References
- 1.American Obesity Association. Obesity in the U.S. Available from: http: //www.obesity.org/subs/fastfacts/obesity_US.shtml.
- 2.Wu Y. Overweight and obesity in China. BMJ. 2006;333:362–363. doi: 10.1136/bmj.333.7564.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 4.Buddeberg-Fischer B, Klaghofer R, Krug L, Buddeberg C, Müller MK, Schoeb O, Weber M. Physical and psychosocial outcome in morbidly obese patients with and without bariatric surgery: a 4 1/2-year follow-up. Obes Surg. 2006;16:321–330. doi: 10.1381/096089206776116471. [DOI] [PubMed] [Google Scholar]
- 5.Benotti PN, Wood GC, Rodriguez H, Carnevale N, Liriano E. Perioperative outcomes and risk factors in gastric surgery for morbid obesity: a 9-year experience. Surgery. 2006;139:340–346. doi: 10.1016/j.surg.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Trus TL, Pope GD, Finlayson SR. National trends in utilization and outcomes of bariatric surgery. Surg Endosc. 2005;19:616–620. doi: 10.1007/s00464-004-8827-8. [DOI] [PubMed] [Google Scholar]
- 7.Requarth JA, Burchard KW, Colacchio TA, Stukel TA, Mott LA, Greenberg ER, Weismann RE. Long-term morbidity following jejunoileal bypass. The continuing potential need for surgical reversal. Arch Surg. 1995;130:318–325. doi: 10.1001/archsurg.1995.01430030088018. [DOI] [PubMed] [Google Scholar]
- 8.Belachew M, Legrand MJ, Defechereux TH, Burtheret MP, Jacquet N. Laparoscopic adjustable silicone gastric banding in the treatment of morbid obesity. A preliminary report. Surg Endosc. 1994;8:1354–1356. doi: 10.1007/BF00188302. [DOI] [PubMed] [Google Scholar]
- 9.Chua TY, Mendiola RM. Laparoscopic Vertical Banded Gastroplasty: The Milwaukee Experience. Obes Surg. 1995;5:77–80. doi: 10.1381/096089295765558222. [DOI] [PubMed] [Google Scholar]
- 10.Wittgrove AC, Clark GW, Schubert KR. Laparoscopic Gastric Bypass, Roux-en-Y: Technique and Results in 75 Patients With 3-30 Months Follow-up. Obes Surg. 1996;6:500–504. doi: 10.1381/096089296765556412. [DOI] [PubMed] [Google Scholar]
- 11.van Dielen FM, Soeters PB, de Brauw LM, Greve JW. Laparoscopic adjustable gastric banding versus open vertical banded gastroplasty: a prospective randomized trial. Obes Surg. 2005;15:1292–1298. doi: 10.1381/096089205774512456. [DOI] [PubMed] [Google Scholar]
- 12.Provost DA. Laparoscopic adjustable gastric banding: an attractive option. Surg Clin North Am. 2005;85:789–805, vii. doi: 10.1016/j.suc.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 13.American Society of Bariatric Surgeons. Medicare expands coverage for lifesaving obesity surgery. Available from: http: //www.asbs.org/html/about/ncd_release.html.
- 14.Shons AR. Plastic reconstruction after bypass surgery and massive weight loss. Surg Clin North Am. 1979;59:1139–1152. doi: 10.1016/s0039-6109(16)41992-4. [DOI] [PubMed] [Google Scholar]
- 15.Acarturk TO, Wachtman G, Heil B, Landecker A, Courcoulas AP, Manders EK. Panniculectomy as an adjuvant to bariatric surgery. Ann Plast Surg. 2004;53:360–366; discussion 367. doi: 10.1097/01.sap.0000135139.33683.2f. [DOI] [PubMed] [Google Scholar]
- 16.Nemerofsky RB, Oliak DA, Capella JF. Body lift: an account of 200 consecutive cases in the massive weight loss patient. Plast Reconstr Surg. 2006;117:414–430. doi: 10.1097/01.prs.0000197524.18233.bb. [DOI] [PubMed] [Google Scholar]
- 17.Chandawarkar RY. Body contouring following massive weight loss resulting from bariatric surgery. Adv Psychosom Med. 2006;27:61–72. doi: 10.1159/000090964. [DOI] [PubMed] [Google Scholar]
- 18.American Society of Plastic Surgery. Body contouring after massive weight loss. Available from: http: //plasticsurgery.org/public_education/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=16766.
- 19.Examination of the massive weight loss patient and staging considerations. Plast Reconstr Surg. 2006;117:22S–30S; discussion 82S-83S. doi: 10.1097/01.prs.0000196301.37309.a3. [DOI] [PubMed] [Google Scholar]
- 20.Song AY, Jean RD, Hurwitz DJ, Fernstrom MH, Scott JA, Rubin JP. A classification of contour deformities after bariatric weight loss: the Pittsburgh Rating Scale. Plast Reconstr Surg. 2005;116:1535–1544; discussion 1535-144;. doi: 10.1097/01.prs.0000182606.92069.13. [DOI] [PubMed] [Google Scholar]
- 21.Safety considerations and avoiding complications in the massive weight loss patient. Plast Reconstr Surg. 2006;117:74S–81S; discussion 82S-83S. doi: 10.1097/01.prs.0000196303.53181.8f. [DOI] [PubMed] [Google Scholar]
- 22.Pitanguy I. Abdominal lipectomy. Clin Plast Surg. 1975;2:401–410. [PubMed] [Google Scholar]
- 23.Matarasso A. Abdominolipoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg. 1991;15:111–121. doi: 10.1007/BF02273843. [DOI] [PubMed] [Google Scholar]
- 24.Fotopoulos L, Kehagias I, Kalfarentzos F. Dermolipectomies following weight loss after surgery for morbid obesity. Obes Surg. 2000;10:451–459. doi: 10.1381/096089200321593959. [DOI] [PubMed] [Google Scholar]
- 25.Gallagher S. Panniculectomy, documentation, reimbursement, and the WOC nurse. J Wound Ostomy Continence Nurs. 2003;30:72–77. doi: 10.1067/mjw.2003.23. [DOI] [PubMed] [Google Scholar]
- 26.Lockwood T. The role of excisional lifting in body contour surgery. Clin Plast Surg. 1996;23:695–712. [PubMed] [Google Scholar]
- 27.Carwell GR, Horton CE Sr. Circumferential torsoplasty. Ann Plast Surg. 1997;38:213–216. doi: 10.1097/00000637-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Gonzales-Ulloa M. Belt lipectomy. Br J Plast Surg. 1960;13:179–186. doi: 10.1016/s0007-1226(60)80035-5. [DOI] [PubMed] [Google Scholar]
- 29.Aly AS, Cram AE, Chao M, Pang J, McKeon M. Belt lipectomy for circumferential truncal excess: the University of Iowa experience. Plast Reconstr Surg. 2003;111:398–413. doi: 10.1097/01.PRS.0000037873.49035.2A. [DOI] [PubMed] [Google Scholar]
- 30.Dellon AL. Fleur-de-lis abdominoplasty. Aesthetic Plast Surg. 1985;9:27–32. doi: 10.1007/BF01570680. [DOI] [PubMed] [Google Scholar]
- 31.Duff CG, Aslam S, Griffiths RW. Fleur-de-Lys abdominoplasty--a consecutive case series. Br J Plast Surg. 2003;56:557–566. doi: 10.1016/s0007-1226(03)00174-7. [DOI] [PubMed] [Google Scholar]
- 32.Taylor J, Shermak M. Body contouring following massive weight loss. Obes Surg. 2004;14:1080–1085. doi: 10.1381/0960892041975578. [DOI] [PubMed] [Google Scholar]
- 33.Shermak MA. Hernia repair and abdominoplasty in gastric bypass patients. Plast Reconstr Surg. 2006;117:1145–1150; discussion 1151-1152;. doi: 10.1097/01.prs.0000204587.10550.21. [DOI] [PubMed] [Google Scholar]
- 34.Vastine VL, Morgan RF, Williams GS, Gampper TJ, Drake DB, Knox LK, Lin KY. Wound complications of abdominoplasty in obese patients. Ann Plast Surg. 1999;42:34–39. doi: 10.1097/00000637-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Pitanguy I. Evaluation of body contouring surgery today: a 30-year perspective. Plast Reconstr Surg. 2000;105:1499–1514; discussion 1515-1516. [PubMed] [Google Scholar]
- 36.Aly AS, Cram AE, Heddens C. Truncal body contouring surgery in the massive weight loss patient. Clin Plast Surg. 2004;31:611–624, vii. doi: 10.1016/j.cps.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 37.Manassa EH, Hertl CH, Olbrisch RR. Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plast Reconstr Surg. 2003;111:2082–2087; discussion 2088-2089;. doi: 10.1097/01.PRS.0000057144.62727.C8. [DOI] [PubMed] [Google Scholar]
- 38.Lockwood T. Lower body lift with superficial fascial system suspension. Plast Reconstr Surg. 1993;92:1112–1122; discussion 1123-1125;. [PubMed] [Google Scholar]
- 39.Hurwitz DJ. Single-staged total body lift after massive weight loss. Ann Plast Surg. 2004;52:435–441; discussion 441. doi: 10.1097/01.sap.0000123361.14654.a5. [DOI] [PubMed] [Google Scholar]
- 40.Van Landuyt K, Hamdi M, Blondeel P, Monstrey S. Autologous breast augmentation by pedicled perforator flaps. Ann Plast Surg. 2004;53:322–327. doi: 10.1097/01.sap.0000125500.27599.a0. [DOI] [PubMed] [Google Scholar]
- 41.Eriksson S. Male reduction mammaplasty after vertical banded gastroplasty. Obes Surg. 1999;9:499–501. doi: 10.1381/096089299765552819. [DOI] [PubMed] [Google Scholar]
- 42.Tashkandi M, Al-Qattan MM, Hassanain JM, Hawary MB, Sultan M. The surgical management of high-grade gynecomastia. Ann Plast Surg. 2004;53:17–20; discussion 21. doi: 10.1097/01.sap.0000112347.30612.f4. [DOI] [PubMed] [Google Scholar]
- 43.Greuse M, Hamdi M, DeMey A. Breast sensitivity after vertical mammaplasty. Plast Reconstr Surg. 2001;107:970–976. doi: 10.1097/00006534-200104010-00011. [DOI] [PubMed] [Google Scholar]
- 44.Rhomberg M, Pulzl P, Piza-Katzer H. Single-stage abdominoplasty and mastopexy after weight loss following gastric banding. Obes Surg. 2003;13:418–423. doi: 10.1381/096089203765887769. [DOI] [PubMed] [Google Scholar]
- 45.Gabriel SE, Woods JE, O'Fallon WM, Beard CM, Kurland LT, Melton LJ 3rd. Complications leading to surgery after breast implantation. N Engl J Med. 1997;336:677–682. doi: 10.1056/NEJM199703063361001. [DOI] [PubMed] [Google Scholar]
- 46.Handel N, Cordray T, Gutierrez J, Jensen JA. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006;117:757–767; discussion 768-772. doi: 10.1097/01.prs.0000201457.00772.1d. [DOI] [PubMed] [Google Scholar]
- 47.Federal Drug Administration. FDA Breast Implant Consumer Handbook - 2004. Available from: http: //www.fda.gov/cdrh/breastimplants/handbook2004/localcomplications.html.
- 48.Bar-Meir E, Eherenfeld M, Shoenfeld Y. Silicone gel breast implants and connective tissue disease--a comprehensive review. Autoimmunity. 2003;36:193–197. doi: 10.1080/08916931000148818. [DOI] [PubMed] [Google Scholar]
- 49.Janowsky EC, Kupper LL, Hulka BS. Meta-analyses of the relation between silicone breast implants and the risk of connective-tissue diseases. N Engl J Med. 2000;342:781–790. doi: 10.1056/NEJM200003163421105. [DOI] [PubMed] [Google Scholar]
- 50.Hoshaw SJ, Klein PJ, Clark BD, Cook RR, Perkins LL. Breast implants and cancer: causation, delayed detection, and survival. Plast Reconstr Surg. 2001;107:1393–1407. doi: 10.1097/00006534-200105000-00012. [DOI] [PubMed] [Google Scholar]
- 51.Brisson J, Holowaty EJ, Villeneuve PJ, Xie L, Ugnat AM, Latulippe L, Mao Y. Cancer incidence in a cohort of Ontario and Quebec women having bilateral breast augmentation. Int J Cancer. 2006;118:2854–2862. doi: 10.1002/ijc.21711. [DOI] [PubMed] [Google Scholar]
- 52.Friis S, Holmich LR, McLaughlin JK, Kjoller K, Fryzek JP, Henriksen TF, Olsen JH. Cancer risk among Danish women with cosmetic breast implants. Int J Cancer. 2006;118:998–1003. doi: 10.1002/ijc.21433. [DOI] [PubMed] [Google Scholar]
- 53.Henriksen TF, Holmich LR, Friis S, McLaughlin JK, Fryzek JP, Pernille Hoyer A, Kjoller K, Olsen JH. The Danish Registry for Plastic Surgery of the Breast: establishment of a nationwide registry for prospective follow-up, quality assessment, and investigation of breast surgery. Plast Reconstr Surg. 2003;111:2182–189; discussion 2190-2191. doi: 10.1097/01.PRS.0000060111.19272.8D. [DOI] [PubMed] [Google Scholar]
- 54.Baran CN, Peker F, Ortak T, Sensoz O, Baran NK. Unsatisfactory results of periareolar mastopexy with or without augmentation and reduction mammoplasty: enlarged areola with flattened nipple. Aesthetic Plast Surg. 2001;25:286–289. doi: 10.1007/s002660010138. [DOI] [PubMed] [Google Scholar]
- 55.Bostwick J. Plastic and reconstructive breast surgery. 2nd ed. St. Louis, Mo. Quality Medical Pub; 2000. [Google Scholar]
- 56.Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas DA. Reduction mammaplasty with the inferior pedicle technique: early and late complications in 371 patients. Br J Plast Surg. 1996;49:442–446. doi: 10.1016/s0007-1226(96)90027-2. [DOI] [PubMed] [Google Scholar]
- 57.Regnault P. Brachioplasty, axilloplasty, and pre-axilloplasty. Aesthetic Plast Surg. 1983;7:31–36. doi: 10.1007/BF01570533. [DOI] [PubMed] [Google Scholar]
- 58.Pitanguy I. Dermolipectomy of the Abdominal Wall, Thighs and Buttocks and Upper Extremity. In: Converse JM, ed , editors. Reconstructive Plastic Surgery. 2nd ed. Philadelphia: W.B. Saunders & Co; 1977. [Google Scholar]
- 59.Abramson DL. Minibrachioplasty: minimizing scars while maximizing results. Plast Reconstr Surg. 2004;114:1631–1634; discussion 1635-1637. doi: 10.1097/01.prs.0000139296.80079.1a. [DOI] [PubMed] [Google Scholar]
- 60.Schultz RC, Feinberg LA. Medial thigh lift. Ann Plast Surg. 1979;2:404–410. doi: 10.1097/00000637-197905000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Lockwood TE. Fascial anchoring technique in medial thigh lifts. Plast Reconstr Surg. 1988;82:299–304. doi: 10.1097/00006534-198808000-00015. [DOI] [PubMed] [Google Scholar]
- 62.Le Louarn C, Pascal JF. The concentric medial thigh lift. Aesthetic Plast Surg. 2004;28:20–23. doi: 10.1007/s00266-003-3095-x. [DOI] [PubMed] [Google Scholar]
- 63.Pianguy I. Correction of lipodystrophy of the lateral thoracic aspect and inner side of the arm and elbow dermosenescence. Clin Plast Surg. 1975;2:477–483. [PubMed] [Google Scholar]
- 64.Hurwitz DJ, Holland SW. The L brachioplasty: an innovative approach to correct excess tissue of the upper arm, axilla, and lateral chest. Plast Reconstr Surg. 2006;117:403–411; discussion 412-413. doi: 10.1097/01.prs.0000200800.81548.37. [DOI] [PubMed] [Google Scholar]
- 65.Pascal JF, Le Louarn C. Brachioplasty. Aesthetic Plast Surg. 2005;29:423–429; discussion 430. doi: 10.1007/s00266-005-0058-4. [DOI] [PubMed] [Google Scholar]
- 66.Chandawarkar RY, Lewis JM. 'Fish-incision' brachioplasty. J Plast Reconstr Aesthet Surg. 2006;59:521–525. doi: 10.1016/j.bjps.2005.04.035. [DOI] [PubMed] [Google Scholar]
- 67.Lockwood T. Brachioplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96:912–920. doi: 10.1097/00006534-199509001-00022. [DOI] [PubMed] [Google Scholar]
- 68.Lewis JR Jr. The thigh lift. J Int Coll Surg. 1957;27:330–334. [PubMed] [Google Scholar]
- 69.Hurwitz DJ, Rubin JP, Risin M, Sajjadian A, Sereika S. Correcting the saddlebag deformity in the massive weight loss patient. Plast Reconstr Surg. 2004;114:1313–1325. doi: 10.1097/01.prs.0000135862.83833.5f. [DOI] [PubMed] [Google Scholar]
- 70.Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72:591–597. doi: 10.1097/00006534-198311000-00001. [DOI] [PubMed] [Google Scholar]
- 71.Commons GW, Halperin B, Chang CC. Large-volume liposuction: a review of 631 consecutive cases over 12 years. Plast Reconstr Surg. 2001;108:1753–1763; discussion 1764-1767. doi: 10.1097/00006534-200111000-00050. [DOI] [PubMed] [Google Scholar]
- 72.Illouz YG. Liposuction's complications. Ann Chir Plast Esthet. 2004;49:614–629. doi: 10.1016/j.anplas.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 73.Deitel M. Surgery for the morbidly obese patient. Philadelphia: Lea & Febiger; 1989. [Google Scholar]
- 74.Rohrich RJ. Mastering shape and form in cosmetic surgery: the annual meeting of the american society for aesthetic plastic surgery. Plast Reconstr Surg. 2001;108:741–742. doi: 10.1097/00006534-200109010-00021. [DOI] [PubMed] [Google Scholar]
- 75.Rubin JP. Plastic surgery after massive weight loss. Contemporary Surgery. 2005;61:599–603. Available from: http: //www.syneture.com/imageServer.aspx?contentID=8132&contenttype=application/pdf. [Google Scholar]


