Abstract
Context:
The scope of ultrasound is emerging in medical science, particularly outside traditional areas of radiology practice.
Aims:
We designed this study to evaluate feasibility of bedside sonography as a tool for airway assessment and to describe sonographic anatomy of airway.
Settings and Design:
A prospective, clinical study.
Materials and Methods:
We included 100 adult, healthy volunteers of either sex to undergo airway imaging systemically starting from floor of the mouth to the sternal notch in anterior aspect of neck by sonography.
Results:
We could visualize mandible and hyoid bone as a bright hyperechoic structure with hypoechoic acoustic shadow underneath. Epiglottis, thyroid cartilage, cricoid cartilage, and tracheal rings appeared hypoechoic. Vocal cords were visualized through thyroid cartilage. Interface between air and mucosa lining the airway produced a bright hyperechoic linear appearance. Artifacts created by intraluminal air prevented visualization of posterior pharynx, posterior commissure, and posterior wall of trachea.
Conclusions:
Ultrasound is safe, quick, noninvasive, repeatable, and bedside tool to assess the airway and can provide real-time dynamic images relevant for several aspects of airway management.
Keywords: Airway, sonography, ultrasound
INTRODUCTION
Airway related morbidity and mortality is not uncommon. So, we require a clinical method having high index of sensitivity and specificity for airway assessment in current scenario.[1] The scope of ultrasound is emerging in medical science, particularly outside traditional areas of radiology practice. However, limited data exists on airway assessment[2,3] and management[4] by ultrasonography.
We designed this study with following aims:
To evaluate the feasibility of bedside ultrasonography as a tool to assess the airway from floor of the mouth to the sternal notch in anterior aspect of the neck,
To determine scanning technique, and
To describe sonographic anatomy of airway systemically.
MATERIALS AND METHODS
The prospective, clinical study was conducted in tertiary care hospital and teaching medical college after receiving institutional ethical approval and written informed consent. We included 100 adult, healthy volunteers of either sex to undergo airway imaging. We excluded the volunteers with morbid obesity, short neck, and abnormal airway. The volunteers were placed supine with head extended and neck flexed (‘sniffing’ position).[5,6] The single investigator in presence of all other investigators including one qualified radiologist performed sonographic examination of the volunteers systemically starting from floor of the mouth to the sternal notch in anterior aspect of neck. The probe operator was trained for emergency ultrasound and ultrasound-guided procedures by various workshop. We used curvilinear low frequency transducer (C60e/5-2 MHZ) for submandibular imaging and linear high frequency transducer (L38e/13-6 MHZ) for rest of airway imaging on a modern, portable ultrasound machine (Sonosite Micromaxx). The transducer was oriented sagittal, parasagittal, and transverse with respect to the neck of volunteers to visualize tongue, hyoid bone, thyrohyoid membrane, epiglottis, thyroid cartilage, vocal cords, cricoid cartilage, cricothyroid membrane, trachea, and other relevant anatomic structures of the upper airway[7,8,9] on sonography to evaluate the feasibility of ultrasound and to describe the scanning technique and sonographic anatomy of the airway.
In the descriptive statistical analysis, continuous variables were noted in terms of the mean and standard deviation and nominal variables were noted in terms of percentage.
RESULTS
We have examined 100 volunteers for airway imaging systemically from floor of the mouth to the sternal notch in anterior aspect of neck by ultrasound. The volunteers consisted 52 male and 48 female with a mean age of 26.13 ± 8.41 years and a mean body mass index of 23.15 ± 3.02. All of volunteers had a normal airway based on clinical methods of airway assessment.
Tongue and floor of the mouth
The tongue appeared like a curvilinear hyperechoic structure on transverse view in the submandibular region using a curvilinear transducer [Figure 1]. The mylohyoid, geniohyoid, and genioglossus muscles appeared like hypoechoic structures. The lingual septum appeared like a linear hyperechoic structure in the vertical midline. The palate could be visualized by keeping the tongue in close contact with palate.[5,6,7,8,9]
Figure 1.
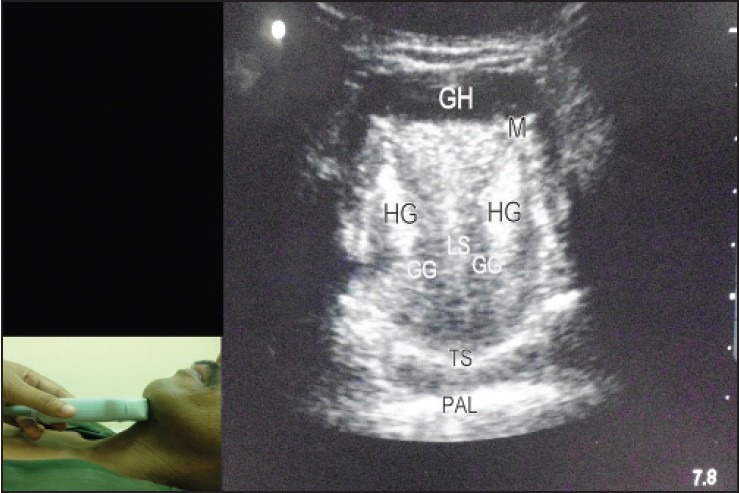
Submandibular transverse view using a curvilinear transducer. The scan shows genioglossus (GG), geniohyoid (GH), hyoglossus (HG), lingual septum (LS), mandible (M), tongue surface (TS), and palate (PAL)
On sagittal view, mylohyoid and geniohyoid appeared like a linear hypoechoic structure and genioglossus appeared like a hypoechoic, striated structure [Figure 2]. On extended submandibular sagittal view, one could also visualize hyoid bone, epiglottis, and pre-epiglottic space[5,6,7,8,9] [Figure 2].
Figure 2.
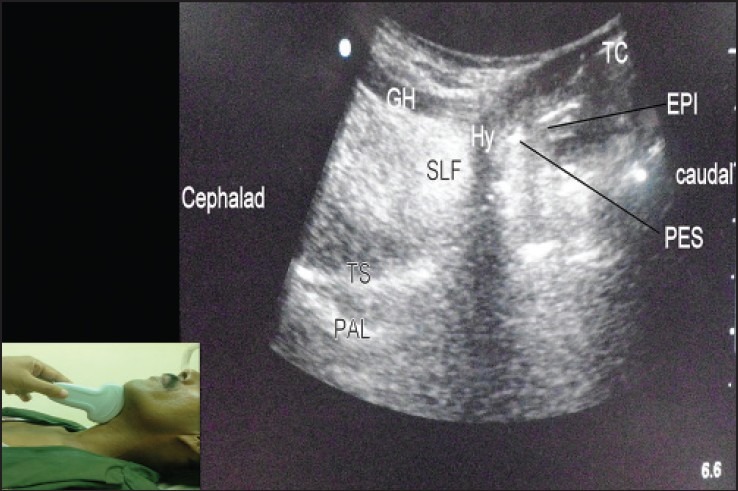
Submandibular sagittal view using a curvilinear transducer. The scan shows genioglossus (GG), geniohyoid (GH), hyoid bone (HY), sublingual fat (SLF), tongue surface (TS), epiglottis (EPI), preepiglottic space (PES), palate (PAL), and thyroid cartilage (TC)
Hyoid bone
On transverse view, hyoid bone appeared as a superficial, hyperechoic, inverted U-shaped, linear structure with posterior acoustic shadowing [Figure 3]. On sagittal view, it appeared as a narrow hyperechoic, curved structure casting an acoustic shadow[5,6,7,8,9] [Figure 4].
Figure 3.
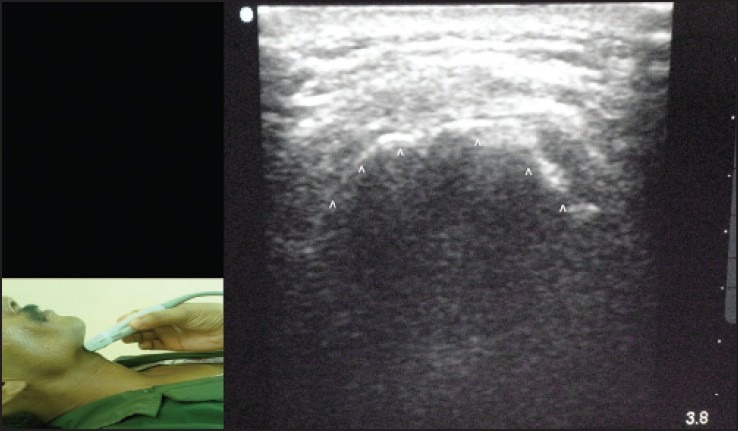
Transverse view of hyoid bone using a linear transducer. The scan shows hyoid bone (arrowheads) with posterior acoustic shadowing
Figure 4.
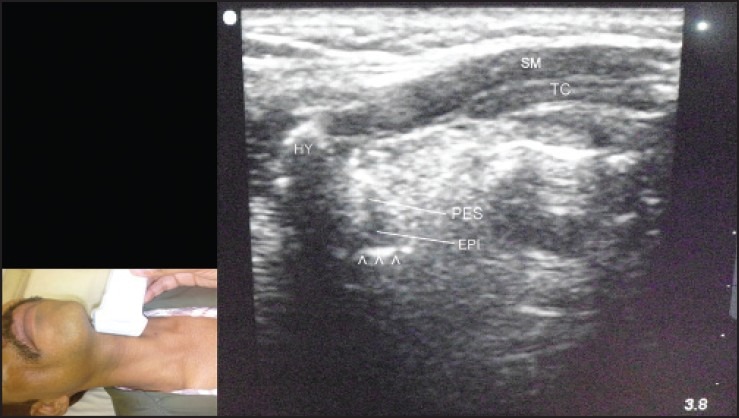
Left parasagittal view through thyrohyoid membrane using a linear transducer. The scan shows epiglottis (EPI), preepiglottic space (PES), hyoid bone (HY), strap muscles (SM), air-mucosal interface (arrowheads), and thyroid cartilage (TC)
Thyrohyoid membrane
It provided a window for visualization of epiglottis in both transverse [Figure 5] and parasagittal view [Figure 4] with linear transducer[5,6,7,8,9]. We could not identify the superior laryngeal nerves in almost all cases.
Figure 5.
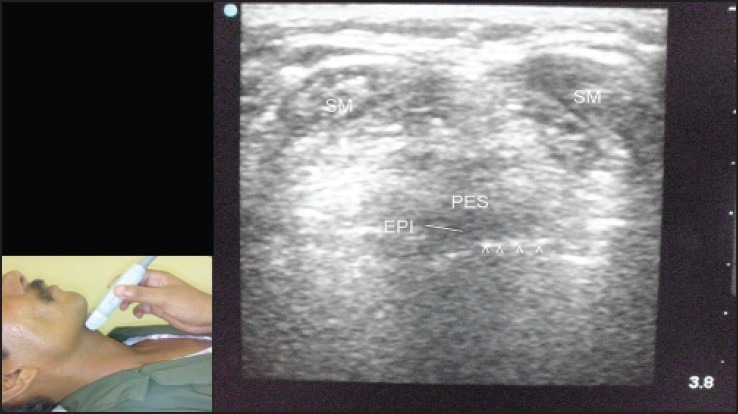
Transverse view through thyrohyoid membrane using a linear transducer. The scan shows epiglottis (EPI), preepiglottic space (PES), strap muscles (SM), air-mucosal interface (arrowheads)
Epiglottis
Epiglottis appeared as a hypoechoic curvilinear structure [Figures 4 and 5]. Tongue protrusion and swallowing movement facilitated the identification of epiglottis in real-time sonography. Epiglottis was surrounded by pre-epiglottic space anteriorly and by a bright linear air-mucosal interface posteriorly.[5,6,7,8,9] We could visualize epiglottis in 90% volunteers in transverse view and 70% of volunteers in parasagittal view [Figure 4].
Thyroid cartilage
Thyroid cartilage appeared as a linear hypoechoic structure on sagittal or parasagittal view [Figures 4 and 6]. On transverse view [Figure 7], it appeared as an inverted V-shaped hypoechoic structure.[5,6,7,8,9]
Figure 6.
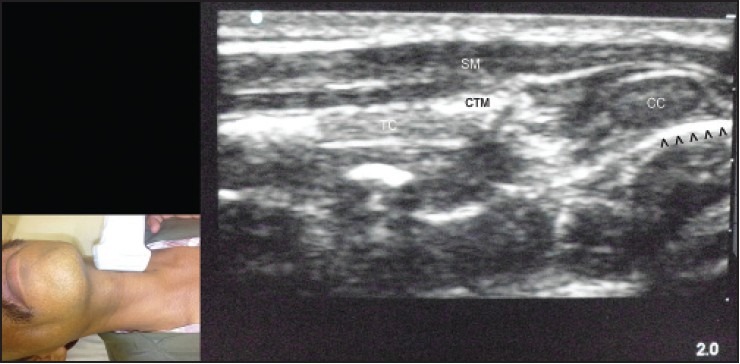
Left parasagittal view through cricothyroid membrane using a linear transducer. The scan shows cricothyroid membrane (CTM), cricoid cartilage (CC), thyroid cartilage (TC), strap muscles (SM), and air-mucosal interface (arrowheads)
Figure 7.
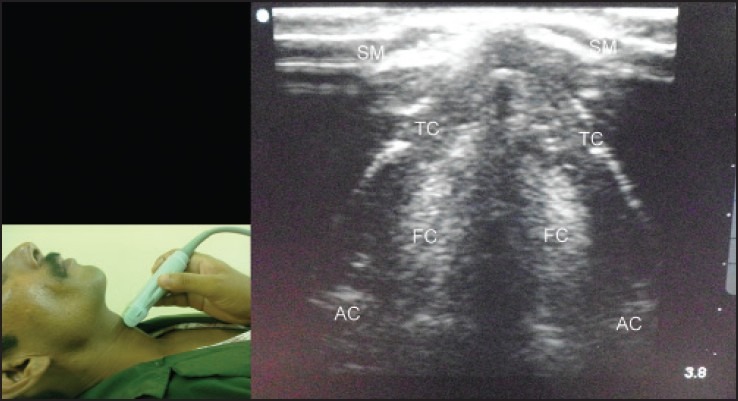
Transverse view at level of thyroid cartilage using a linear transducer. The scan shows false cords (FC), arytenoid cartilage (AC), thyroid cartilage (TC), and strap muscles (SM)
Vocal cords
We imaged vocal cords through thyroid cartilage window in a transverse view [Figures 7 and 8]. We could identify and distinguish the true and false vocal cords just by sliding the linear transducer in cephalocaudal direction over thyroid cartilage in all volunteers. True vocal cords appeared as two triangular hypoechoic structures (vocalis muscles), outlined by hyperechoic vocal ligaments. The false vocal cords lay parallel and cephalad to true vocal cords and appeared hyperechoic. False vocal cords remained relatively immobile during phonation.[5,6,7,8,9]
Figure 8.
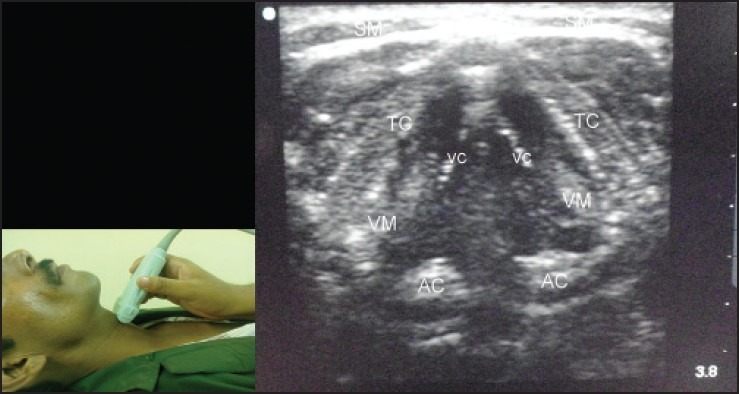
Transverse view at level of thyroid cartilage using a linear transducer. The scan shows vocal cords (VC), vocalis muscles (VM), arytenoid cartilage (AC), thyroid cartilage (TC), and strap muscles (SM)
Cricoid cartilage
Cricoid cartilage appeared as a round hypoechoic structure in parasagittal view [Figures 6 and 9] and as an arch-like structure in transverse view [Figure 10]. Posterior surface of it was delineated by a bright air mucosal interface and reverberation artifacts.[5,6,7,8,9]
Figure 9.
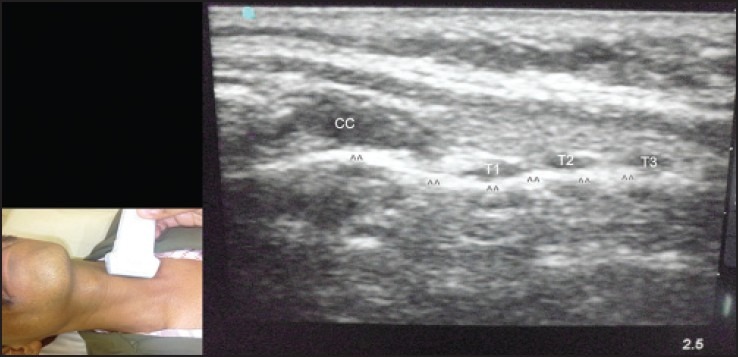
Left parasagittal view over trachea using a linear transducer. The scan shows cricoid cartilage (CC), tracheal rings (T1, T2, and T3), and air-mucosal interface (arrowheads)
Figure 10.
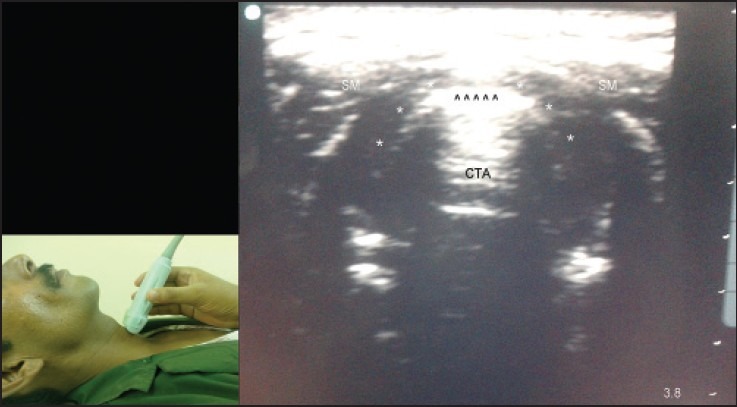
Transverse view at level of cricoid cartilage using a linear transducer. The scan shows cricoid cartilage (asterisks), air-mucosal interface (arrowheads), comet tail artifacts (CTA), and strap muscles (SM)
Cricothyroid membrane
Cricothyroid membrane appeared as a hyperechoic band between the thyroid and cricoid cartilages in sagittal as well as parasagittal view [Figure 6]. It could provide a window to visualize vocal cords but least suitable.[5,6,7,8,9]
Trachea and adjacent structures
Trachea, thyroid gland, and esophagus could be visualized in transverse view at the level of suprasternal notch [Figures 11 and 12]. Tracheal rings appeared hypoechoic structures in sonography. On transverse view, they appeared as an inverted U-shaped hypoechoic structure, delineated posteriorly by a linear hyperechoic air-mucosal interface and reverberation artifact. They looked like ‘strings of beads’ in parasagittal view [Figure 9]. Thyroid gland was very well-visualized just anterolateral to trachea as homogenous and hyperechoic, compared to adjacent soft tissues. Esophagus lay posterolateral to trachea and could be distinguish from trachea by peristaltic movement of esophageal lumen during swallowing in real-time sonography.[8,9]
Figure 11.
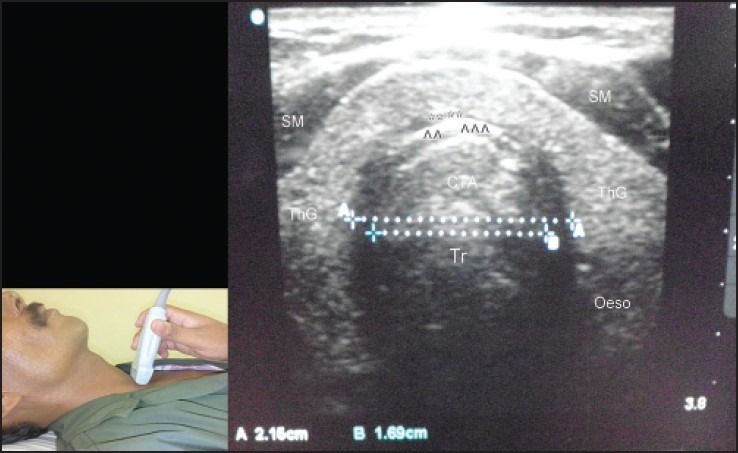
Transverse view at the level of suprasternal notch using a linear transducer in midline. The scan shows trachea (Tr), esophagus (Oeso), thyroid gland (ThG), strap muscles (SM), comet tail artifacts (CTA), and air mucosal interface (arrowheads)
Figure 12.
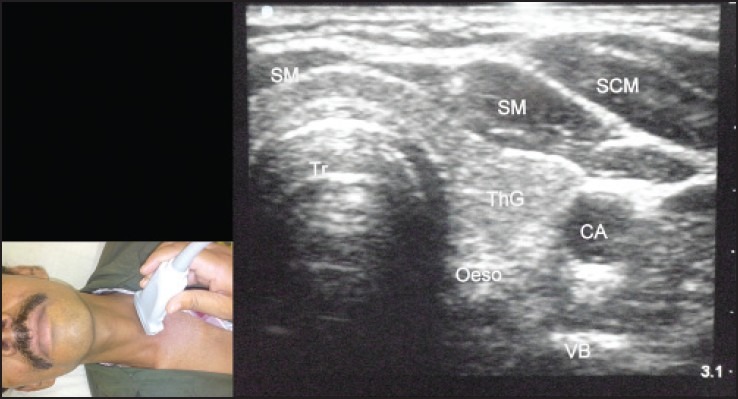
Transverse view at the level of suprasternal notch using a linear transducer in left lateral side. The scan shows trachea (Tr), esophagus (Oeso), thyroid gland (ThG), strap muscles (SM), carotid artery (CA), vertebral body of cervical vertebra (VB), and sternocleidomastoid muscle (SCM)
DISCUSSION
We could successfully visualize all of the relevant anatomic structures of the airway with transcutaneous scanning approach on modern portable ultrasound unit and were able to describe the scanning technique along with sonographic anatomy.
Airway structures are filled with air. Because of high acoustic impedance, air does not transmit ultrasound signals properly and produces poor ultrasound image. Hence, we can view partial to complete anterior and lateral wall of airway structures, but cannot view posterior wall. In present study, air prevented visualization of palatal surface in the most of volunteers in transverse and parasagittal view in submandibular region. We could visualize palatal surface by asking volunteers to keep their tongue in contact with palate. Epiglottis is suspended in air. So, visualization of entire epiglottis is difficult. As intraluminal air and acoustic shadowing of hyoid bone obscured the visualization of epiglottis,[2,5] we could visualize epiglottis in 90% volunteers in transverse view and 70% of volunteers in parasagittal view. Calcification of thyroid cartilage prevents visualization of vocal cords especially in male and old age people.[10] We could visualize vocal cords through thyroid cartilage in all volunteers may be, because volunteers were younger.
In present study, a single probe operator performed sonography to decrease the experience related bias. We have used a modern portable ultrasound machine as it allows bedside sonography for airway assessment in elective as well as emergency condition. However, it needs to be validated in future. Our clinical experience indicates that resolution is not an issue as far as airway assessment is concerned with a modern ultrasound machine.
Sonography of airway structures like epiglottis,[11,12,13] cricothyroid membrane,[14] vocal cords,[15,16,17] trachea,[18] etc. were studied separately by many authors but only few2,3 studied for the purpose of airway assessment.
Singh et al.,[2] carried out similar study on 24 healthy volunteers with a larger cart-based sonography machine and found that sonography can provide anatomical information of airway. They could visualize all the airway structures among all volunteers in their feasibility study except epiglottis. They could not visualize epiglottis in 29% (seven of 24) of volunteers in parasagittal plane because of acoustic shadowing by hyoid bone.
Prasad et al.,[3] found that sonography could visualize all of the structures as reliable as computed tomography. Both modalities agreed well for infrahyoid parameters than suprahyoid parameters as later may be affected by head extension.
Recently, intraoral sublingual technique[19,20] has also been described. Ultrasound has been evaluated in identifying laryngeal abnormalities[21,22] and laryngeal traumas.[23] Ultrasound has been used for an identification of endotracheal tube placement[24,25] and Ryle's tube[26] placement. The ultrasound has potential to guide surgical airways such as percutaneous dilatational tracheostomy[27] and cricothyrotomy[28] and to predict difficult laryngoscopy[29] and post-extubation stridor.[30]
Further work is also necessary to validate the study in children, old-aged, morbid obesity, patients with short neck and patients with abnormal airway. Larger, randomized studies are required to compare ultrasound with established imaging technique like computed tomography and magnetic resonance imaging for airway assessment. Further studies are also required to compare ultrasound with other gold standard technique for airway assessment like direct laryngoscopy and bronchoscopy.
ACKNOWLEDGEMENT
The authors would like to thank the volunteers for their cooperation and Dr Digish Vaghela (Associate Professor, Department of Radiology) for kind help.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gupta S, Sharma KR, Jain D. Airway assessment: Predictors of difficult airway. Indian J Anaesth. 2005;49:257–62. [Google Scholar]
- 2.Singh M, Chin KJ, Chan VW, Wong DT, Prasad GA, Yu E. Use of sonography for airway assessment: An observational study. J Ultrasound Med. 2010;29:79–85. doi: 10.7863/jum.2010.29.1.79. [DOI] [PubMed] [Google Scholar]
- 3.Prasad A, Yu E, Wong DT, Karkhanis R, Gullane P, Chan VW. Comparison of sonography and computed tomography as imaging tools for assessment of airway structures. J Ultrasound Med. 2011;30:965–72. doi: 10.7863/jum.2011.30.7.965. [DOI] [PubMed] [Google Scholar]
- 4.Kristensen MS. Ultrasonography in the management of the airway. Acta Anaesthesiol Scand. 2011;55:1155–73. doi: 10.1111/j.1399-6576.2011.02518.x. [DOI] [PubMed] [Google Scholar]
- 5.Kundra P, Mishra SK, Ramesh A. Ultrasound of the airway. Indian J Anaesth. 2011;55:456–62. doi: 10.4103/0019-5049.89868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta PK, Gupta K, Dwivedi AD, Jain Manish. Potential role of ultrasound in anaesthesia and intensive care. Anesth Essays Res. 2011;5:11–9. doi: 10.4103/0259-1162.84172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loveday E. The larynx. In: Ahuja AT, Evans RM, editors. Practical Head and Neck Ultrasound. 1st ed. London: Greenwich medical media limited; 2000. pp. 105–17. [Google Scholar]
- 8.Iro H, Bozzato A, Zenk J, editors. Atlas of Head and Neck Ultrasound. New York: Thieme medical publishers; 2013. [Google Scholar]
- 9.Ahuja AT. The thyroid and parathyroids. In: Ahuja AT, Evans RM, editors. Practical Head and Neck Ultrasound. 1st ed. London: Greenwich medical media limited; 2000. pp. 35–9. [Google Scholar]
- 10.Wang CP, Chen TC, Yang TL, Chen CN, Lin CF, Lou PJ, et al. Transcutaneous ultrasound for evaluation of vocal fold movement in patients with thyroid disease. Eur J Radiol. 2012;81:e288–91. doi: 10.1016/j.ejrad.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 11.Werner SL, Jones RA, Emerman CL. Sonographic assessment of the epiglottis. Acad Emerg Med. 2004;11:1358–60. doi: 10.1197/j.aem.2004.05.033. [DOI] [PubMed] [Google Scholar]
- 12.Hung TY, Li S, Chen PS, Wu LT, Yang YJ, Tseng LM, et al. Bedside ultrasonography as a safe and effective tool to diagnose acute epiglottitis. Am J Emerg Med. 2011;29:359.e1–3. doi: 10.1016/j.ajem.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Ko DR, Chung YE, Park I, Lee HJ, Park JW, You JS, et al. Use of bedside sonography for diagnosing acute epiglottitis in the emergency department: A preliminary study. J Ultrasound Med. 2012;31:19–22. doi: 10.7863/jum.2012.31.1.19. [DOI] [PubMed] [Google Scholar]
- 14.Nicholls SE, Sweeney TW, Ferre RM, Strout TD. Bedside sonography by emergency physicians for the rapid identification of landmarks relevant to cricothyrotomy. Am J Emerg Med. 2008;26:852–6. doi: 10.1016/j.ajem.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 15.Desai AA, Pandya VK, Bhalani DB, Desai S, Parikh BD. Value of ultrasonography in laryngeal and laryngopharyngeal cancers. Indian J Otolaryngol Head Neck Surg. 2004;56:191–5. doi: 10.1007/BF02974348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sirikci A, Karatas E, Durucu C, Baglam T, Bayazit Y, Ozkur A, et al. Noninvasive assessment of benign lesions of vocal folds by means of ultrasonography. Ann Otol Rhinol Laryngol. 2007;116:827–31. doi: 10.1177/000348940711601106. [DOI] [PubMed] [Google Scholar]
- 17.Bryson PC, Leight WD, Zdanski CJ, Drake AF, Rose AS. High-resolution ultrasound in the evaluation of pediatric recurrent respiratory papillomatosis. Arch Otolaryngol Head Neck Surg. 2009;135:250–3. doi: 10.1001/archoto.2008.544. [DOI] [PubMed] [Google Scholar]
- 18.Hatfield A, Bodenham A. Portable ultrasonic scanning of the anterior neck before percutaneous dilatational tracheostomy. Anaesthesia. 1999;54:660–3. doi: 10.1046/j.1365-2044.1999.00859.x. [DOI] [PubMed] [Google Scholar]
- 19.Tsui BC, Hui CM. Sublingual airway ultrasound imaging. Can J Anaesth. 2008;55:790–1. doi: 10.1007/BF03016357. [DOI] [PubMed] [Google Scholar]
- 20.Tsui BC, Hui CM. Challenges in sublingual airway ultrasound interpretation. Can J Anaesth. 2009;56:393–4. doi: 10.1007/s12630-009-9077-y. [DOI] [PubMed] [Google Scholar]
- 21.Loveday EJ. Ultrasound of the larynx. Imaging. 2003;15:109–14. [Google Scholar]
- 22.Bisetti MS, Segala F, Zappia F, Albera R, Ottaviani F, Schindler A. Non-invasive assessment of benign vocal folds lesions in children by means of ultrasonography. Int J Pediatr Otorhinolaryngol. 2009;73:1160–2. doi: 10.1016/j.ijporl.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 23.Jakubowska A, Zawadzka-Gıos L, Brzewski M. Usefulness of ultrasound examination in larynx traumas in children. Pol J Radiol. 2011;76:7–12. [PMC free article] [PubMed] [Google Scholar]
- 24.Marciniak B, Fayoux P, Hébrard A, Krivosic-Horber R, Engelhardt T, Bissonnette B. Airway management in children: Ultrasonography assessment of tracheal intubation in real time? Anesth Analg. 2009;108:461–5. doi: 10.1213/ane.0b013e31819240f5. [DOI] [PubMed] [Google Scholar]
- 25.Muslu B, Sert H, Kaya A, Demircioglu RI, Gözdemir M, Usta B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30:671–6. doi: 10.7863/jum.2011.30.5.671. [DOI] [PubMed] [Google Scholar]
- 26.Kim HM, So BH, Jeong WJ, Choi SM, Park KN. The effectiveness of ultrasonography in verifying the placement of a nasogastric tube in patients with low consciousness at an emergency center. Scand J Trauma Resusc Emerg Med. 2012;20:38. doi: 10.1186/1757-7241-20-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guinot PG, Zogheib E, Petiot S, Marienne JP, Guerin AM, Monet P, et al. Ultrasound-guided percutaneous tracheostomy in critically ill obese patients. Crit Care. 2012;16:R40. doi: 10.1186/cc11233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curtis K, Ahern M, Dawson M, Mallin M. Ultrasound-guided, Bougie-assisted cricothyroidotomy: A description of a novel technique in cadaveric models. Acad Emerg Med. 2012;19:876–9. doi: 10.1111/j.1553-2712.2012.01391.x. [DOI] [PubMed] [Google Scholar]
- 29.Adhikari S, Zeger W, Schmier C, Crum T, Craven A, Frrokaj I, et al. Pilot study to determine the utility of point-of-care ultrasound in the assessment of difficult laryngoscopy. Acad Emerg Med. 2011;18:754–8. doi: 10.1111/j.1553-2712.2011.01099.x. [DOI] [PubMed] [Google Scholar]
- 30.Ding LW, Wang HC, Wu HD, Chang CJ, Yang PC. Laryngeal ultrasound: A useful method in predicting post-extubation stridor. A pilot study. Eur Respir J. 2006;27:384–9. doi: 10.1183/09031936.06.00029605. [DOI] [PubMed] [Google Scholar]


