Abstract
The conventional modes of ventilation suffer many limitations. Although they are popularly used and are well-understood, often they fail to match the patient-based requirements. Over the years, many small modifications in ventilators have been incorporated to improve patient outcome. The ventilators of newer generation respond to patient's demands by additional feedback systems. In this review, we discuss the popular newer modes of ventilation that have been accepted in to clinical practice. Various intensive care units over the world have found these modes to improve patient ventilator synchrony, decrease ventilator days and improve patient safety. The various modes discusses in this review are: Dual control modes (volume assured pressure support, volume support), Adaptive support ventilation, proportional assist ventilation, mandatory minute ventilation, Bi-level airway pressure release ventilation, (BiPAP), neurally adjusted ventilatory assist and NeoGanesh. Their working principles with their advantages and clinical limitations are discussed in brief.
Keywords: Adaptive support ventilation, airway pressure release ventilation, dual control modes, mandatory minute ventilation, newer modes of ventilation, neurally adjusted ventilatory assist, NeoGanesh, proportional assist ventilation, volume-assured pressure support, volume support
INTRODUCTION
The conventional modes of ventilation suffer many limitations. Although they are popularly used and are well-understood, often they fail to match the patient based requirements. Over the years, many small modifications in ventilators have been incorporated to improve patient outcome. The ventilators of newer generation respond to patient's demands by additional feedback systems. In this review, we discuss the popular newer modes of ventilation that have been accepted in to clinical practice. Various intensive care units over the world have found these modes to improve patient ventilator synchrony, decrease ventilator days, and improve patient safety.
Key ideas in understanding mechanical ventilation
The basic understanding into mechanical aspects of ventilation comes from understanding the physics of flow and pressure involved. Before we elaborate the rationale for newer modes of ventilation understanding the key concepts in ventilation are critical. These modern modes are just alterations of interplay among these factors and thus innovate into newer advanced patient ventilator interactions.
The ability of ventilator to initiate, maintain, and terminate an assisted/artificial breath derives its basis from “Equation of motion.”[1,2] The equation of motion postulates that the pressure necessary to deliver a breath has two components; the pressure to overcome elastic recoil of the lungs and chest wall and the pressure to cause flow through the airways. The left hand side of the equation can be expanded to show that ventilating pressure may be made up of muscle pressure and/or airway pressure generated by the ventilator. The right hand side of the equation can be expanded to show that elastic recoil pressure is the product of elastance time's volume, while resistive pressure is the product of resistance and flow.[3]
P = Presistive + Pelastance
In a ventilators perspective, the same can be rewritten as shown in [Figure 1]:
Figure 1.
Ventilator pressure generation mechanics
In mathematical terms
P resistive is given by Volume (V) * Airway resistance (R)
P elastance is given by Volume (V) * Lung elastance (E)
Thus, the equation becomes
P = V*R + V*E
The various pressures involved in delivering volume to alveoli are illustrated in Figure 2.
Figure 2.
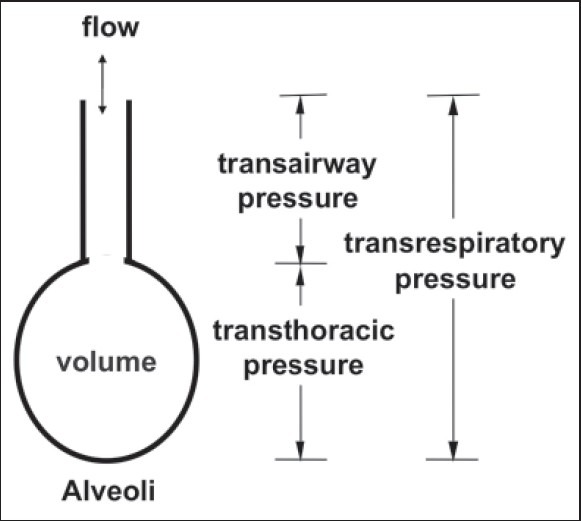
Alveolar diagram showing various pressures involved in inspiration/expiration. The same are either provided or overcome by the ventilator
The other aspect of modifications targets “the ventilatory variables”. These are as follows:
Trigger variable
This variable is what helps the ventilator to initiate a breath. In patient-initiated modes this forms a determinant of ventilator patient synchrony. The more sensitive is ventilator in sensing the lesser is likely to be patient work of initiation of breathing.[4] Trigger can further be by following:
Time (control modes),
Pressure
Flow,
Neural sensing
Trigger variable is the primary factor that divides all modes into the following:
Mandatory: Where ventilator initiates and controls phases of breathing
Spontaneous: Where patient initiates the breath and often interacts with ventilator to modify phase and cycle variables.
Limit variable
This is the maximal limit manually set for a phase of respiration; however, it does not cause switching of phase of breath. (i.e., maximal value to stop inspiration). This can be further
Time (control modes),
Pressure,
Flow,
Volumes
Cycle variable
This terminates the phase of respiration and causes the ventilator to switch from inspiration to expiration or vice versa. This can be time (commonest), flow, volume, or pressure.
Control variable
It can be understood from the equation of motion that the ventilator can control either the left side of the equation (i.e., airway pressure) or the right side (i.e., volume and flow). In volume control, [Figure 3] the ventilator controls flow indirectly controlling volume. Holding, inspiratory flow constant during inspiration causes volume and pressure to rise linearly. Inspiration ends (cycles off) when a preset tidal volume is met. In contrast in pressure control ventilation [Figure 4], airway pressure is held constant during inspiration. This causes inspiratory flow to fall exponentially from its peak value toward 0 as volume rises exponentially. Inspiration ends after a preset inspiratory time or after a preset inspiratory flow threshold (depending on cycle variable).
Figure 3.
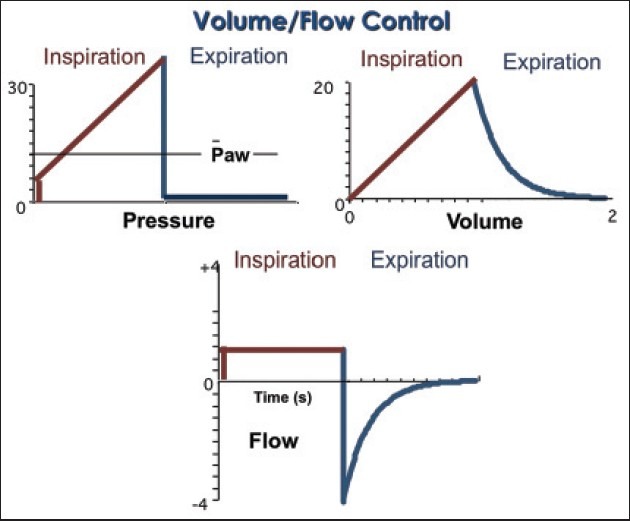
Ventilatory graphics in classical volume control mode
Figure 4.
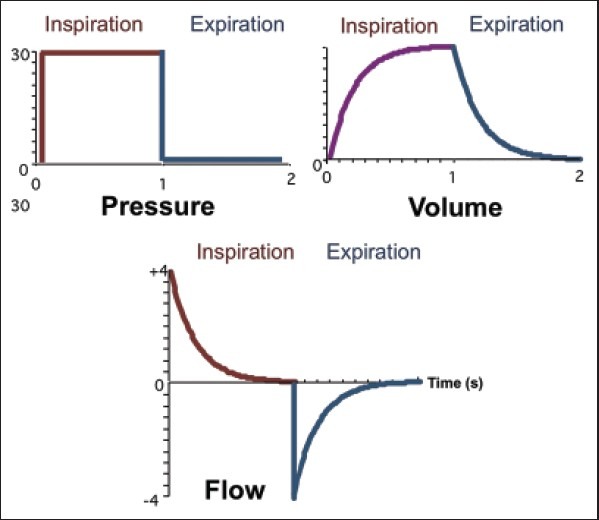
Ventilatory graphics in classical pressure control mode
This is the factor that the ventilator quantitatively modifies to deliver inspiratory volume to lungs.[5] This can be the following:
Volume/flow controlled,
Pressure control, and
Time controlled.
This is the mode that determines the primary labeled name of ventilatory mode, for example, volume-controlled or pressure-controlled ventilation.
PROBLEMS WITH CONVENTIONAL MODES OF VENTILATION
In critical care settings, all the parameters of equation of motion change with time. A ventilator setting appropriate for one point of time may not be optimal with patient deterioration or improvement.[6] These ventilators only deliver the set parameters and take no feedback from patient variables. Thus, all the classical volume/pressure control modes are “Open Loop” (the feedback loop is absent). The newer modes target to make alterations with the changing lung and take feedback from patient parameters, thus completing the feedback loop and are “Closed loop” type.[7,8] The control, cycle, or the limit variables undergo self-adjustment and these variables are no longer limited to single parameter determinant but if the threshold of one component is reached they shift to the other alternate set parameter. This has lead to name “Dual control” ventilation.[9,10] These adjustments can occur in a single initiated breath or in subsequent breaths and thus form the basis of classification of these modes. Various newer modes available in market are shown in Table 1.
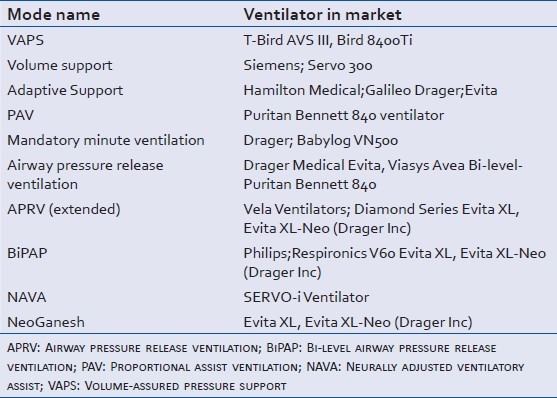
Table 1.
Ventilator modes and Modes and available ventilatorsavailable market ventilators
Dual control within a breath
The control variable can change its nature (from pressure to volume or vice versa) within a single breath if the desired ventilation requirements are not met.[9]
The listed mode under this subtype is
Volume-assured pressure support (VAPS): This is a modification into pressure control mode. It makes the ventilator to switch from pressure control mode to volume control if a minimum set tidal volume is not achieved.[11] [Figure 5] The operator adjustable mechanical parameters are as in conventional pressure control mode-Pressure limit, peak flow rate, ventilator rate, and positive end-expiratory pressure (PEEP). Additionally, a minimum desired “Minimum tidal volume” is also defined. In patients where the lung compliance decreases this mode provides safety against increasing blood CO2 levels by maintaining minimal minute ventilation. It is tricky to understand the rationale behind the optimal setting in this mode. One must understand if the set pressure limit is too high it will not only cause unwanted barotrauma to lung but also would generate higher volume than minimal set tidal volume, thus negating the volume guarantee. Set flow rates must not be very low; in situations where minimal volume is not met it would cause a delayed switch from pressure control to volume control and would lead to unwanted prolongation of inspiratory time. Evidence in favor of this mode has shown that it leads to decreased work of breathing and lower intrinsic PEEP.[12,13]
Figure 5.
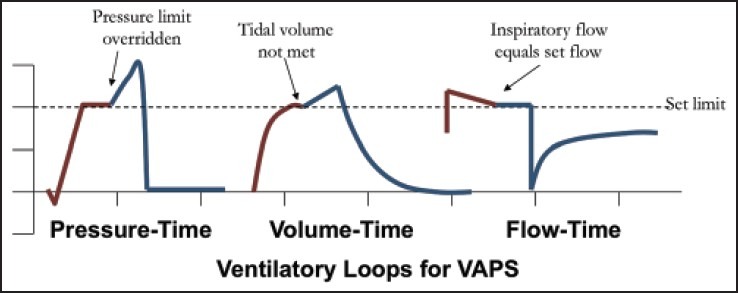
Ventilatory graphics in VAPS (Volume assured pressure support mode) mode
Dual control in subsequent breaths
The ventilator takes feedback from output parameters of initial breaths and makes automatic adjustments to set targets in the subsequent breaths. The mode listed under this subcategory is
Pressure limited flow cycled ventilation (aka volume support): It is a modification of pressure support mode where the support pressure is automatically adjusted by the ventilator to meet the minimal set tidal volume.[14] [Figure 6] The ventilator in initial breaths measures the delivered tidal volume and if the minimal volume set is higher than this, it automatically steps up the pressure support in the next breaths.[15] This mode achieves the advantages of pressure support assuring an adequate tidal volume despite changes in lung compliance. The respiratory therapist sets respiratory rate, minimal tidal volume and PEEP. Volume support is a useful mode for weaning as once the patient begins to achieve a desired tidal volume it automatically decreases the pressure support, thus gradually loading the respiratory muscles to take on work of breathing. Like the pressure support mode patient controls the I:E (Inspiratory time: Expiratory time) and the total inspiratory time, this improves the ventilator-patient synchrony. The basic caution prior to use of this mode is that patient must have spontaneous breathing activity else the ventilator will automatically shift to backup mode. Also if the set tidal volume is too large, the ventilator will raise the pressure support to achieve it and lead to problems like barotrauma, hemodynamic compromise, and intrinsic PEEP. If the set volume is too low, it may lead to inadequate pressure support and thus increased respiratory rate leading to increased work of breathing[16]
Figure 6.
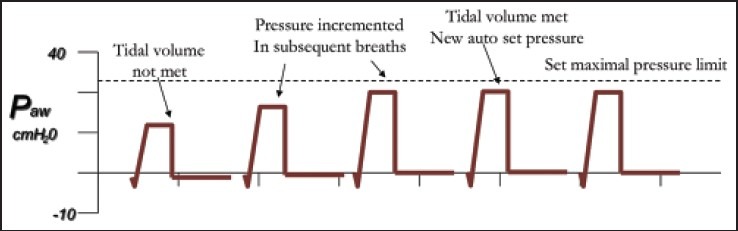
Ventilatory graphics in volume support mode
It must be realized from above description that VAPS and volume support not only differ in the method of their parameter adjustment but also VAPS is an entirely controlled mode, whereas the volume support is a spontaneous patient-initiated mode.
OTHER NEWER CLOSED LOOP MODES
Adaptive support ventilation
This is a unique mode that sets minimal work of breathing as its end point to achieve desired minute ventilation. The control variable is “pressure” and is capable of delivering both pressure control or pressure support breaths. The operating principle is based on pressure controlled synchronized intermittent mandatory ventilation with automatic adjustments to set pressure level and respiratory rate on the basis of measured lung mechanics in the previous breaths.[17] The set parameters are the ideal body weight, minimum minute ventilation, PEEP, and trigger sensitivity. The target ventilation (tidal volume and respiratory rate) corresponds to the best combination from energy standpoint estimated by automatic measurements of lung compliance and resistance. The ventilator continuously optimizes I:E ratio to avoid any auto-PEEP. The indications for the use of this mode cover wide range of clinical conditions. It can be used as partial to full support mode Acute respiratory distress syndrome (ARDS), asthma, and weaning.[18,19] Patients with rapid changes in lung physical parameters like compliance (ARDS) and resistance (asthma) are benefited, as these parameters are main determinants unlike any other mode. The major limitation if this mode is inability to recognize dead space ventilation or shunts to make adjustments to ventilation.[17] In clinical conditions where lung physical parameters remain unchanged (pulmonary embolism), the mode fails to adapt to patients requirements. Auto-PEEP may become problem in chronic obstructive pulmonary disease (COPD) patients needing longer expiratory times which are currently unaccounted in current protocols of automatic adjustments.
Proportional assist ventilation (PAV)
PAV is a promising newer mode with advantage of improving ventilator patient synchrony. It is a form of synchronized partial ventilator assistance with a unique feature that ventilator assists in proportion to patients instantaneous effort.[20] In other words, it amplifies patient's ventilatory effort giving patient freedom to adopt his own breathing pattern. PAV unloads respiratory muscles and unaltered respiratory pattern allows synchrony between ventilator and patient's neural ventilator drive. The therapist sets the percentage of assistance to be delivered and other parameters are adjusted automatically by patients “air hunger.” As the ventilator on take on only a part of breathing work this mode is unlikely to cause respiratory muscle atrophy in chronically ventilated patients. Parameters like I:E ration and inspiratory time are completely patient controlled and further add to successful patient synchronization. The potential disadvantage noted it that if the patient worsens or improves, the proportion of assistance may needed to be reset according to newer clinical situation.[21] This has, however, has been addressed in newer modification of “PAV+” mode, which is capable of sensing patient lung mechanical properties and adjusting accordingly.[22] Other advantages of PAV include low airway pressures, optimal weaning, and decreased work of breathing.[23] A technical important aspect of PAV is that there should be minimal air leak in the system; this would cause the ventilator to overassist or cause auto cycling[24] (a positive back pressure wont build up during inspiration and ventilator would presume inspiration is going on). PAV has been used in early/late ARDS, hypercapnic respiratory failure, and weaning. Recent trials with noninvasive PAV have also shown promising results for the above indications.
Mandatory minute ventilation (MMV)
It is a modification of pressure support ventilation. The ventilator takes feedback to alter both respiratory rate and the level of pressure support to achieve set minimum minute ventilation. The operator sets minimum minute ventilation required adjudging the present patient clinical state. These values often fall in 70%-90% of current minute volume. If the patient fails to achieve the set value, the ventilator provides the deficit. MMV forms a reliable weaning mode,[25] as the set value can be gradually decreased loading the respiratory muscles. In patients with apneic episodes or central drive pathologies, MMV sets safety by providing a set value ventilation as mandatory ventilation.[26] The ventilatory setting of MMV need extreme caution, if the set value is significantly lower than current minute ventilation, this may lead to increased work of breathing by the patient and in reverse situation this can lead to complete unloading of respiratory muscles causing possibility of muscle atrophy. A maximal respiratory rate set too high can cause significant increase in ventilator frequency during ventilator automatic adjustment leading to “rapid shallow” breathing.
BI-LEVEL VENTILATION MODES
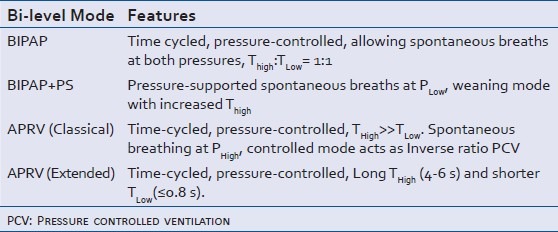
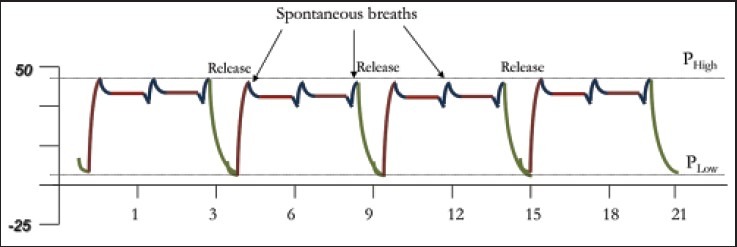
Bi-levels are innovative ventilator modes that allow patients spontaneous breathing during any phase of ventilator cycle. The ventilator cycles between two set pressures: P-High and P-Low (high pressure and low pressure, respectively). The likelihood of ventilator-patient asynchrony is minimal due to the fact that the patient can breathe irrespective of ventilator cycle and these breaths can be aided by the ventilator. Maintaining high pressure prevents alveolar collapse and aids in recruitment. The low-pressure phase prevents any barotrauma, air trapping, and hemodynamic compromise. The various modifications to Bi-level ventilator modes[27] are represented in Table 2.
Table 2.
(Bi-level modes and their modifications)
Airway pressure release ventilation (APRV)
APRV is a bi-level mode representing another open-lung ventilation strategy. It provides two levels of continuous positive airway pressure (CPAP) with an inverse I:E ratio of 2:1 or more. [Figure 7].[28] The rationale of using prolonged high-pressure phase is to prevent alveolar collapse and maintain recruitment. The release phase (expiratory phase) brings down mean airway pressure and plays significant role in maintaining normocarbia. The mode has dual functionality; in presence of spontaneous breathing the patient can breathe in any phase of respiratory cycle with supported breaths thus bringing down needs of sedation. In absence of spontaneous breathing activity, the bi-level pressure acts as time-cycled inverse ratio ventilation.[29] The tidal volume generated mainly depends upon respiratory compliance and difference between the two CPAP levels. The therapist sets Phigh,(high pressure in CPAP) Plow,(low pressure in CPAP) Thigh(time for Phigh)and Tlow (Time for Plow). Initial Phigh should be set to plateau pressure or the upper inflection point and Plow should be set at lower inflection point on volume-pressure curve. APRV should be used with caution in hypovolemic as increased intrathoracic pressure further lower venous return. APRV should be avoided in patients with obstructive lung diseases as it can cause air trapping or rupture of bullae in COPD. APRV has been shown to improve oxygenation in patients with ARDS simultaneously decreasing need of sedation or paralysis.[30]
Figure 7.
Ventilatory graphics in airway pressure release ventilation
Neurally adjusted ventilatory assist (NAVA)
NAVA is a closed loop mode that delivers breath proportional to patient's inspiratory effort. Unlike all other modes available that use pressure, flow or volume sensing to initiate a breath, NAVA uses diaphragmatic electromyogram to detect inspiratory effort of patient.[31] An esophageal catheter with electrodes placed at the level of diaphragm is used to record time of initiation and strength of contraction. This mode over scores all other modes in synchronization of patients efforts to ventilator by having least possible delay among the two. Like PAV, NAVA assists in accordance to measured strength of diaphragmatic contractions and most of parameters like inspiratory time, I:E ratio are patient controlled. Leaks in the circuit can cause false initiation of breaths in conventional modes leading to severe ventilator asynchrony; NAVA, however, is completely unaffected by this phenomena as breath initiation is completely independent of physical properties of the circuit.[32] In other modes auto-PEEP increases work of ventilator initiation in COPD and asthma, this does not effect ventilatory cycle in NAVA and thus overall work of breathing decreases in these patients. Setting up a NAVA ventilator is straightforward and gain over diaphragmatic electrographic potential is the only single input required. A practical limitation with NAVA is placement of esophageal catheter with electrodes and its validity of longer duration of ventilation.[33]
NeoGanesh (Smartcare)
It is closed loop modification of pressure support ventilation with integrated artificial intelligence. The system mimics clinical approach of adjusting ventilator assistance depending on patient's respiratory pattern and literature based weaning protocols. This mode is based on three fundamental principles: 1. Adapt pressure support to patient's current clinical situation, 2. In case of stability the ventilator tends to wean of pressure support, and 3. Initiate spontaneous breathing trials as per prerecorded clinical guidelines. Ventilator takes feedback from monitored respiratory rate, tidal volume, and end-tidal CO2. Once the patient remains stable on a setting, it tries to gradually wean off to maintain optimal respiratory variables, which are predefined as “Patient comfort zone.” Trials have shown that it not only reduces weaning failures but also significantly hastens weaning duration.[34]
CONCLUSION
The newer modes by the use of ventilatory physics improve patient ventilator synchrony and assist in weaning. These modes have become sensitive to patient ventilation requirements and demands. However, long-term studies are needed to prove their efficacy. Classical modes are used in most intensive care setups; however, understanding these newer modes may help to chart out patient-based ventilatory strategies and improve outcomes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lucangelo U, Bernabè F, Blanch L. Lung mechanics at the bedside: Make it simple. Curr Opin Crit Care. 2007;13:64–72. doi: 10.1097/MCC.0b013e32801162df. [DOI] [PubMed] [Google Scholar]
- 2.Lucangelo U, Bernabé F, Blanch L. Respiratory mechanics derived from signals in the ventilator circuit. Respir Care. 2005;50:55–65. [PubMed] [Google Scholar]
- 3.Chatburn RL. Understanding mechanical ventilators. Expert Rev Respir Med. 2010;4:809–19. doi: 10.1586/ers.10.66. [DOI] [PubMed] [Google Scholar]
- 4.Sassoon CS. Mechanical ventilator design and function: The trigger variable. Respir Care. 1992;37:1056–69. [PubMed] [Google Scholar]
- 5.Mireles-Cabodevila E, Diaz-Guzman E, Heresi GA, Chatburn RL. Alternative modes of mechanical ventilation: A review for the hospitalist. Cleve Clin J Med. 2009;76:417–30. doi: 10.3949/ccjm.76a.08043. [DOI] [PubMed] [Google Scholar]
- 6.Mireles-Cabodevila E, Hatipoglu U, Chatburn RL. A rational framework for selecting modes of ventilation. Respir Care. 2013;58:348–66. doi: 10.4187/respcare.01839. [DOI] [PubMed] [Google Scholar]
- 7.Chatburn RL, Mireles-Cabodevila E. Closed-loop control of mechanical ventilation: Description and classification of targeting schemes. Respir Care. 2011;56:85–102. doi: 10.4187/respcare.00967. [DOI] [PubMed] [Google Scholar]
- 8.Branson RD, Johannigman JA, Campbell RS, Davis K., Jr Closed-loop mechanical ventilation. Respir Care. 2002;47:427–51. [PubMed] [Google Scholar]
- 9.Branson RD, Davis K., Jr Dual control modes: Combining volume and pressure breaths. Respir Care Clin N Am. 2001;7:397–408, viii. doi: 10.1016/s1078-5337(05)70041-1. [DOI] [PubMed] [Google Scholar]
- 10.Tehrani F, Rogers M, Lo T, Malinowski T, Afuwape S, Lum M, et al. A dual closed-loop control system for mechanical ventilation. J Clin Monit Comput. 2004;18:111–29. doi: 10.1023/b:jocm.0000032744.99885.38. [DOI] [PubMed] [Google Scholar]
- 11.Amato MB, Barbas CS, Bonassa J, Saldiva PH, Zin WA, De Carvalho CR. Volume-assured pressure support ventilation (VAPSV). A new approach for reducing muscle workload during acute respiratory failure. CHEST. 1992;102:1225–34. doi: 10.1378/chest.102.4.1225. [DOI] [PubMed] [Google Scholar]
- 12.Oscroft NS, Smith IE. A bench test to confirm the core features of volume-assured non-invasive ventilation. Respirology. 2010;15:361–4. doi: 10.1111/j.1440-1843.2009.01691.x. [DOI] [PubMed] [Google Scholar]
- 13.Okuda M, Kashio M, Tanaka N, Fujii T, Okuda Y. Positive outcome of average volume-assured pressure support mode of a Respironics V60 Ventilator in acute exacerbation of chronic obstructive pulmonary disease: A case report. J Med Case Rep. 2012;6:284. doi: 10.1186/1752-1947-6-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sottiaux TM. Patient-ventilator interactions during volume-support ventilation: Asynchrony and tidal volume instability - a report of three cases. Respir Care. 2001;46:255–62. [PubMed] [Google Scholar]
- 15.McGough EK, Banner MJ, Boysen PG. Pressure support and flow-cycled, assisted mechanical ventilation in acute lung injury. Chest. 1990;98:458–62. doi: 10.1378/chest.98.2.458. [DOI] [PubMed] [Google Scholar]
- 16.Donn SM, Sinha SK. Newer modes of mechanical ventilation for the neonate. Curr Opin Pediatr. 2001;13:99–103. doi: 10.1097/00008480-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Brunner JX, Iotti GA. Adaptive Support Ventilation (ASV) Minerva Anestesiol. 2002;68:365–8. [PubMed] [Google Scholar]
- 18.Sulemanji D, Marchese A, Garbarini P, Wysocki M, Kacmarek RM. Adaptive support ventilation: An appropriate mechanical ventilation strategy for acute respiratory distress syndrome? Anesthesiology. 2009;111:863–70. doi: 10.1097/ALN.0b013e3181b55f8f. [DOI] [PubMed] [Google Scholar]
- 19.Dongelmans DA, Veelo DP, Paulus F, de Mol BA, Korevaar JC, Kudoga A, et al. Weaning automation with adaptive support ventilation: A randomized controlled trial in cardiothoracic surgery patients. Anesth Analg. 2009;108:565–71. doi: 10.1213/ane.0b013e318190c49f. [DOI] [PubMed] [Google Scholar]
- 20.Ambrosino N, Rossi A. Proportional assist ventilation (PAV): A significant advance or a futile struggle between logic and practice? Thorax. 2002;57:272–6. doi: 10.1136/thorax.57.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vitacca M. New things are not always better: Proportional assist ventilation vs. pressure support ventilation. Intensive Care Med. 2003;29:1038–40. doi: 10.1007/s00134-003-1707-1. [DOI] [PubMed] [Google Scholar]
- 22.Xirouchaki N, Kondili E, Vaporidi K, Xirouchakis G, Klimathianaki M, Gavriilidis G, et al. Proportional assist ventilation with load-adjustable gain factors in critically ill patients: Comparison with pressure support. Intensive Care Med. 2008;34:2026–34. doi: 10.1007/s00134-008-1209-2. [DOI] [PubMed] [Google Scholar]
- 23.Kleinsasser A, Von Goedecke A, Hoermann C, Maier S, Schaefer A, Keller C, et al. Proportional assist ventilation reduces the work of breathing during exercise at moderate altitude. High Alt Med Biol. 2004;5:420–8. doi: 10.1089/ham.2004.5.420. [DOI] [PubMed] [Google Scholar]
- 24.Du HL, Ohtsuji M, Shigeta M, Chao DC, Sasaki K, Usuda Y, et al. Expiratory asynchrony in proportional assist ventilation. Am J Respir Crit Care Med. 2002;165:972–7. doi: 10.1164/ajrccm.165.7.2103049. [DOI] [PubMed] [Google Scholar]
- 25.Guthrie SO, Lynn C, Lafleur BJ, Donn SM, Walsh WF. A crossover analysis of mandatory minute ventilation compared to synchronized intermittent mandatory ventilation in neonates. J Perinatol. 2005;25:643–6. doi: 10.1038/sj.jp.7211371. [DOI] [PubMed] [Google Scholar]
- 26.Burns KE, Lellouche F, Lessard MR. Automating the weaning process with advanced closed-loop systems. Intensive Care Med. 2008;34:1757–65. doi: 10.1007/s00134-008-1154-0. [DOI] [PubMed] [Google Scholar]
- 27.Rose L, Ed A. Advanced modes of mechanical ventilation: Implications for practice. AACN Adv Crit Care. 2006;17:145–58. [PubMed] [Google Scholar]
- 28.Daoud EG. Airway pressure release ventilation. Ann Thorac Med. 2007;2:176–9. doi: 10.4103/1817-1737.36556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoshida T, Rinka H, Kaji A, Yoshimoto A, Arimoto H, Miyaichi T, et al. The impact of spontaneous ventilation on distribution of lung aeration in patients with acute respiratory distress syndrome: Airway pressure release ventilation versus pressure support ventilation. Anesth Analg. 2009;109:1892–900. doi: 10.1213/ANE.0b013e3181bbd918. [DOI] [PubMed] [Google Scholar]
- 30.Modrykamien A, Chatburn RL, Ashton RW. Airway pressure release ventilation: An alternative mode of mechanical ventilation in acute respiratory distress syndrome. Cleve Clin J Med. 2011;78:101–10. doi: 10.3949/ccjm.78a.10032. [DOI] [PubMed] [Google Scholar]
- 31.Terzi N, Piquilloud L, Rozé H, Mercat A, Lofaso F, Delisle S, et al. Clinical review: Update on neurally adjusted ventilatory assist-report of a round-table conference. Crit Care. 2012;16:225. doi: 10.1186/cc11297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verbrugghe W, Jorens PG. Neurally adjusted ventilatory assist: A ventilation tool or a ventilation toy? Respir Care. 2011;56:327–35. doi: 10.4187/respcare.00775. [DOI] [PubMed] [Google Scholar]
- 33.Biban P, Serra A, Polese G, Soffiati M, Santuz P. Neurally adjusted ventilatory assist: A new approach to mechanically ventilated infants. J Matern Fetal Neonatal Med. 2010;23(Suppl 3):38–40. doi: 10.3109/14767058.2010.510018. [DOI] [PubMed] [Google Scholar]
- 34.Lellouche F, Brochard L. Advanced closed loops during mechanical ventilation (PAV, NAVA, ASV, SmartCare) Best Pract Res Clin Anaesthesiol. 2009;23:81–93. doi: 10.1016/j.bpa.2008.08.001. [DOI] [PubMed] [Google Scholar]


