Abstract
Chlorfenapyr has been used worldwide for agricultural pest control since 1995. Despite its widespread use, acute human poisoning data are insufficient; only a small number of fatalities from chlorfenapyr poisoning have been reported. The signs and symptoms of chlorfenapyr toxicity include nausea, vomiting, fever, rhabdomyolysis, among others. In addition, central nervous system effects in association with delayed toxicity have also been observed. Here, we detail a fatality resulting from delayed chlorfenapyr toxicity following the ingestion of a small amount of pesticide.
Keywords: Chlorfenapyr, insecticide, poisoning
INTRODUCTION
Chlorfenapyr [4-bromo-2-(4-chlorophenyl)-1-(ethoxymethyl)-5-(trifluoromethyl)-1H-pyrrole-3-carbonitrile] is a pesticide in the pyrrole family. It has been used against insects in agricultural environments for over 15 years. It is a pro-insecticide that forms CL 303268 that uncouples oxidative phosphorylation within the mitochondria. Consequently, chlorfenapyr inhibits adenosine triphosphate (ATP) production, causing cellular death and the death of the target organism.[1] Chlorfenapyr has not been studied extensively, but its toxicity to humans is very high. Some fatal cases of chlorfenapyr poisoning by oral ingestion have been reported in the medical literature.[2,3,4,5,6] However, fatality case from small amount of chlorfenapyr ingestion has not been reported. Here, we present a fatal case caused by delayed chlorfenapyr toxicity, even though only a small amount was ingested.
CASE REPORT
A 41-year-old woman was transferred from a rural hospital to our emergency department for further evaluation and management, following pesticide poisoning. She had ingested a mouthful (estimated 20 mL) of pesticide during a suicide attempt approximately 2 weeks earlier. However, she showed no symptoms immediately after ingesting the pesticide; therefore, she continued in her daily activities. After 2 weeks, she developed nausea and general weakness. She was immediately admitted to a rural hospital. Despite treatment, her symptoms worsened. By the time she was referred to our hospital, she was drowsy and had mild fever. She had no history of chronic disease, alcohol, or drug abuse. She denied coingesting other toxic substances; however, she did not remember the pesticide class or trade name.
Upon examination, her vital signs were as follows: Blood pressure, 98/50 mm Hg; heart rate, 86/min; respiratory rate, 17/min; and body temperature, 37.6°C. She exhibited a slight drowsiness, and her Glasgow Coma Scale (GCS) rating was 14. There were no abnormalities in her initial electrocardiogram, blood gas analysis, or chest radiograph. Her hemoglobin (Hb) was 11.7 g/dL, her white blood cell (WBC) count was 6830/mm3, and a platelet count of 198000/mm3. Her renal function and serum electrolyte tests were normal, but other laboratory results showed high levels of serum creatinine kinase (CK) (3081 IU/L) and serum aspartate aminotransferase (AST) (130 IU/L).
The emergency department managed this patient by providing supportive care, including intravenous fluid hydration and urine alkalinization. We were able to exclude the possibility of central nervous system (CNS) infection, because we had already performed brain computed tomography (CT) and a lumbar puncture. The brain CT scan showed diffuse cerebral swelling with low density lesions in the white matter throughout the brain [Figure 1]. However, the patient's cerebrospinal fluid (CSF) pressure was normal and the lumbar puncture was unremarkable.
Figure 1.
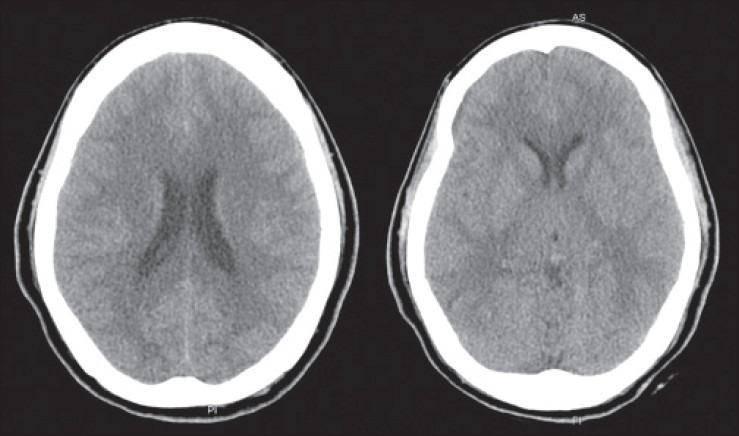
A brain computed tomography scan shows diffuse cerebral swelling with low-density lesions in the white matter throughout the brain
On the following morning, 20 h after admission, the patient suddenly exhibited a high fever, diaphoresis, and an altered mental state. Her vital signs were as follows: Blood pressure, 150/90 mm Hg; heart rate, 98/min; respiratory rate, 28/min; and body temperature, 40.7°C. She became comatose, and her GCS was 3. A tracheal intubation was performed and a mechanical ventilator was applied to maintain her airway and support ventilation. Following these measures, we investigated her brain CT follow-up scan for sudden mental changes and her chest/abdomen CT scan for a high fever. The follow-up brain CT scan showed no significant change and we could not find any infection foci in the chest/abdominal CT scan. Soon afterward, she showed signs of sudden cardiac arrest. Advanced cardiac life support was performed for 30 min, but she finally expired, approximately 2 weeks after ingesting a small amount of chlorfenapyr.
DISCUSSION
The symptoms and signs of chlorfenapyr toxicity include nausea, vomiting, fever, diaphoresis, tachypnea, rhabdomyolysis, and mental state changes.[2,4,5,6] Tharaknath et al., reported that a similar fatality presented delayed adverse neurological effects ten days after chlorfenapyr ingestion and Kwon et al., reported symptoms approximately 2 weeks after chlorfenapyr ingestion.[5,6] In both cases, the patients presented brain and spinal cord magnetic resonance imaging (MRIs) demonstrating the demyelination of the CNS. This delayed toxicity was also observed in our case; however, we could not conduct a brain MRI because of institutional circumstances. We assume that chlorfenapyr poisoning has a latent period related to the formation of the active toxic product from this pro-insecticide.
In our case, the patient complained of diaphoresis and fever, as in other cases. However, we could not uncover the exact information about the agent she ingested. Therefore, only a symptomatic treatment was performed. After the patient died, her husband found the pesticide bottle and informed us.
We had prescribed antipyretics, such as nonsteroidal anti-inflammatory drugs and acetaminophen, to control a high fever, but the fever could not be controlled. An uncontrolled high fever is thought to be responsible for chlorfenapyr poisoning fatalities. Thermoregulation is conducted by hypothalamic regulation of the sympathetic nervous system and by mitochondrial oxidative phosphorylation. Nonshivering thermogenesis occurs in brown adipose tissue and it primarily uncouples oxidative phosphorylation through the activity of a group of mitochondrial proteins known as uncoupling proteins.[7] Chlorfenapyr seems to affect the inhibition and uncoupling of oxidative phosphorylation in the mitochondria.[1] Because of this uncoupled system, ATP production from glucose is lacking, and this deficiency can cause severe damage to the skeletal muscle, retina, and other parts of the nervous system with high-energy requirements.[8,9]
The fatality rate from chlorfenapyr poisoning is quite high. Endo et al.,[2] reported that 8 patients out of 24 chlorfenapyr poisoning cases died. Three fatal chlorfenapyr poisoning cases were recently reported in South Korea and India.[4,5,6] In addition to toxicity from oral ingestion, there was one case of death from chlorfenapyr vapor exposure.[3] Because of these findings, we believe that chlorfenapyr is highly toxic to humans, and the use of chlorfenapyr may need to be restricted in the same way that paraquat is controlled.
CONCLUSIONS
We have described a fatal chlorfenapyr poisoning case that included a latent period accompanying delayed toxicity, even though only a mouthful of chlorfenapyr was ingested. Based on this observation, patients with chlorfenapyr poisoning should be carefully observed for several weeks after ingestion, even when small amounts of chlorfenapyr are ingested and no toxic symptoms are present.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Raghavendra K, Barik TK, Sharma P, Bhatt RM, Srivastava HC, Sreehari U, et al. Chlorfenapyr: A new insecticide with novel mode of action can control pyrethroid resistant malaria vectors. Malar J. 2011;10:16. doi: 10.1186/1475-2875-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Endo Y, Tachibana S, Hirano J, Kuroki Y, Ohashi N, Yoshioka T, et al. Acute chlorfenapyr poisoning. Chudoku Kenkyu. 2004;17:89–93. [PubMed] [Google Scholar]
- 3.Hoshiko M, Naito S, Koga M, Mori M, Hara K, Ishitake T. Case report of acute death on the 7th day due to exposure to the vapor of the insecticide chlorfenapyr. Chudoku Kenkyu. 2007;20:131–6. [PubMed] [Google Scholar]
- 4.Choi UT, Kang GH, Jang YS, Ahn HC, Seo JY, Sohn YD. Fatality from acute chlorfenapyr poisoning. Clin Toxicol (Phila) 2010;48:458–9. doi: 10.3109/15563651003750074. [DOI] [PubMed] [Google Scholar]
- 5.Kwon JS, Han HJ, Kim JY, Park JH. A case of chlorfenapyr intoxication with central nervous system involvement. J Clin Toxicol. 2012;2:147. [Google Scholar]
- 6.Tharaknath VR, Prabhakar YV, Kumar KS, Babu NK. Clinical and radiological findings in chlorfenapyr poisoning. Ann Indian Acad Neurol. 2013;16:252–4. doi: 10.4103/0972-2327.112486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rusyniak DE, Sprague JE. Toxin-induced hyperthermic syndromes. Med Clin North Am. 2005;89:1277–96. doi: 10.1016/j.mcna.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Holt IJ, Harding AE, Morgan-Hughes JA. Deletions of muscle mitochondrial DNA in patients with mitochondrial myopathies. Nature. 1988;331:717–9. doi: 10.1038/331717a0. [DOI] [PubMed] [Google Scholar]
- 9.Walker UA, Collins S, Byrne E. Respiratory chain encephalomyopathies: A diagnostic classification. Eur Neurol. 1996;36:260–7. doi: 10.1159/000117269. [DOI] [PubMed] [Google Scholar]


