Abstract
Aims:
To compare conventional magnetic resonance imaging (MRI) and direct magnetic resonance (MR) arthrography in the evaluation of triangular fibrocartilage complex (TFCC) and intrinsic wrist ligament tears.
Materials and Methods:
T1-weighted, fat suppressed (FS) proton density plus T2-weighted (FS PD/T2), 3D multiple-echo data image combination (MEDIC) sequences and direct MR arthrography were performed in 53 patients with wrist pain. Images were evaluated for the presence and location of TFCC, scapholunate ligament (SLL) and lunatotriquetral ligament (LTL) tears, and imaging findings were compared with operative findings in 16 patients who underwent arthroscopy or open surgery (gold standard).
Results:
Sixteen patients underwent arthroscopy/open surgery: 12 TFCC tears were detected arthroscopically out of which 9 were detected on FS PD/T2 sequence, 10 on MEDIC sequence, and all 12 were detected on MR arthrography. The sensitivities of FS PD/T2, MEDIC sequences, and MR arthrography in the detection of TFCC tears were 75%, 83.3%, and 100%, respectively. Out of the eight arthroscopically confirmed SLL tears, three tears were detected on FS PD/T2 sequence, five on MEDIC sequence, and all eight were visualized on MR arthrography. The sensitivities of FS PD/T2, MEDIC sequences, and MR arthrography in detecting SLL tears were 37.5%, 62.5%, and 100%, respectively. One arthroscopically confirmed LTL tear was diagnosed on FS PD/T2 sequence, three on MEDIC sequence, and all five arthroscopically confirmed LTL tears were detected with MR arthrography. The sensitivities of PD, MEDIC sequences, and MR arthrography in detecting LTL tears were 20%, 40%, and 100%, respectively.
Conclusions:
MR arthrography is the most sensitive and specific imaging modality for the evaluation of wrist ligament tears.
Keywords: TFCC, scapholunate ligament, lunatotriquetral ligament, MR arthrography, wrist ligament tear, wrist arthroscopy, TFCC tear
Introduction
Wrist ligaments maintain intimate contact between carpal bones, allow for a wide range of motion and maintain joint stability. Wrist ligaments are classified as extrinsic and intrinsic.[1] The extrinsic ligaments connect forearm bones or metacarpals with the carpus, whereas the intrinsic ligaments originate and insert within the carpus. The extrinsic ligaments include the radiocarpal, ulnocarpal/triangular fibrocartilage complex (TFCC), and dorsal ligaments.[1] The TFCC includes TFC disk proper, volar and dorsal radioulnar ligaments, ulnolunate ligament, ulnotriquetral ligament, ulnar collateral ligament, subsheath of extensor carpi ulnaris (ECU) tendon and meniscus homologue. Scapholunate ligament (SLL), lunatotriquetral ligament (LTL), deltoid/arcuate ligament, trapezium–trapezoid ligament, trapezoid–capitate ligament, and capitate–hamate ligament are the intrinsic ligaments. TFCC is the main stabilizer of the distal radioulnar joint (DRUJ), and SLL and LTL are the most important intrinsic ligaments.
Triangular fibrocartilage disk proper is attached by its base to the medial margin of distal radius and by its apex to the styloid process of ulna. It is biconcave in shape and articulates with distal ulna proximally and with proximal carpal row distally, primarily the triquetrum.[2,3] The SLL and LTL are delta or linear-shaped, and have thick dorsal and volar components and a thin central component.[4,5] Tears of the TFCC, SLL, and LTL are a common cause of wrist pain, instability, and limitation of joint movement.
A study by Hobby et al.[6] showed that MRI imaging of wrist changed the clinical diagnosis in 56% of patients and changed the management plan in 47% of patients. Reports of diagnostic accuracy of conventional magnetic resonance imaging (MRI) and magnetic resonance (MR) arthrography vary widely in literature.[7,8,9,10,11,12,13,14] Reported sensitivity of conventional MRI is 52-89% for detecting TFCC tears, 25-86% for SLL tears, and 31-89% for LTL tears.[8,9,13] For MR arthrography, different studies have shown sensitivity in the range of 90-100% for detecting TFCC tears, 52-86% for SLL tears, and 0-56% for LTL tears.[7]
We compared the diagnostic accuracy of conventional MRI sequences and direct MR arthrography in the detection of tears of the TFCC, SLL, and LTL, using arthroscopy/open surgery as the gold standard, and tried to develop the most appropriate MR imaging protocols for detection of these lesions.
Materials and Methods
Institute ethical clearance committee approval was obtained for the study. A total of 53 patients (age range 18-60 years; mean age 29.3 years) with clinical diagnosis of wrist pain and/or instability, and suspected of having wrist ligament tears were included in the study over a period of 2 years from April 2007 to May 2009. There were 35 male (66%) and 18 female (34%) patients in the study. Thirteen patients had a history of antecedent trauma; fractures were present in eight patients. Patients with history of localized bone or skin infections, clinical features suggestive of inflammatory arthritides, and neuropathies were excluded from the study. All patients were evaluated using plain radiographs (posteroanterior view, lateral view, and views in radial and ulnar deviation), conventional MRI, and MR arthrography. Patients with MRI findings suggestive of inflammatory arthritis, infection, neuropathy, etc., were excluded from the study. Arthroscopic correlation was obtained in 16 (30.2%) cases. MR arthrography was performed within 1 week following conventional MRI, and wrist arthroscopy was performed within 2 weeks of MR arthrography.
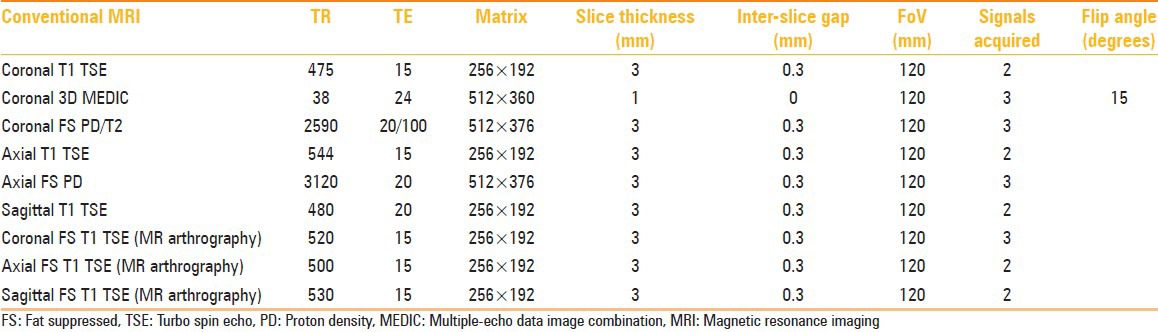
Conventional MRI
MRI examinations were performed on 1.5 Tesla (T) MR scanner (Sonata/Avanto; Siemens, Erlangen, Germany) using dedicated wrist coil. The patients were scanned in prone position with the wrist in neutral position and images were acquired in coronal, axial, and sagittal planes. The sequences used are listed in Table 1.
Table 1.
Parameters of MR sequences used
MR arthrography
Radiocarpal joint injection technique
Single-compartment radiocarpal joint arthrogram was performed under fluoroscopic guidance using 2-5 ml solution of 0.1 ml gadolinium diluted in 20 ml solution composed of 15 ml of normal saline and 5 ml of iodinated contrast (diatrizoate meglumine) (370 mg iodine/ml). If communication with midcarpal joint or DRUJ was noted, an additional 2-3 ml of contrast was injected. Patient was shifted to MR gantry within an hour of radiocarpal joint injection. The following sequences were performed [Table 1]: Coronal T1-weighted (T1W) fat-suppressed turbo spin echo, axial T1W fat-suppressed turbo spin echo, and sagittal T1W fat-suppressed turbo spin echo. Coronal is the most important plane for detecting wrist ligament tears. Therefore, to ensure similarity in the quality of sequences, parameters such as field of view, slice thickness, inter-slice gap, number of acquisitions, and averages were kept the same for coronal proton density (PD)/T2 and MR arthrography sequences. Similar parameters were used for multiple-echo data image combination (MEDIC) sequence, except slice thickness and inter-slice gap which were 1 mm and 0 mm, respectively, for MEDIC.
Image analysis
The images were analyzed by three experienced musculoskeletal radiologists (Radiologist 1 (SG) with 8 years of experience, Radiologist 2 (RS) with 20 years of experience, Radiologist 3 (DNS) with 22 years of experience) blinded to arthroscopic findings. All decisions were made by means of consensus. FS PD/T2, MEDIC, and MR arthrographic images were evaluated for the presence of TFCC/SLL/LTL tears and for the exact location of the tears. For purpose of interpretation, ligament tears were qualitatively assessed as being absent (0), possibly present (1), probably present (2), and definitely present (3) on conventional MRI sequences and on MR arthrogram. Confidence levels of 2 and 3 were taken as affirmative for the presence of ligament tears on all sequences, whereas confidence levels of 0 and 1 were taken as absence of a tear. For TFCC, a linear band of increased signal intensity on FS PD/T2 and MEDIC sequences was recorded as definite tear (3). On MR arthrogram, presence of a defect lined by contrast, or leakage of contrast from radiocarpal into distal radioulnar joint was recorded as definite tear (3). Distorted ligament morphology was classified as probable tear (2). Possible tear (1) was suggested when increased fluid was seen in DRUJ but ligaments appeared normal. Once diagnosed, we attempted to describe TFCC tears according to Palmer's classification, taking into account location of the tear and preceding history of trauma when available. However, patients usually do not remember the traumatic event that caused a TFCC tear (e.g., lifting a heavy weight), and present with waxing and waning chronic wrist pain. So, we described the location of tear, presence of any associated intrinsic ligament tears, presence of joint instability, and degenerative changes, if any, in every case.
For SLL and LTL, distinct areas of discontinuity within the ligament with increased signal intensity on coronal conventional (PD/T2 and/or MEDIC) or MR sequences, or complete absence of the ligament was recorded as definite tear (3). Distorted ligament morphology was recorded as probable tear (2). Fluid in midcarpal joint was classified as possible tear (1). On MR arthrogram, contrast outlining a defect in the ligament or contrast leakage from the radiocarpal joint into the midcarpal joint was also recorded as definite tear (3). Severe distortion of the ligament morphology (fraying, thinning, or irregularity) was considered as probable tear (2).
“On MR arthrography, it was possible to either completely exclude a ligament tear (no tear), or diagnose it with a high level of confidence (definite or probable tear).
Arthroscopy/surgery (gold standard)
Patients with normal MRI findings were not taken up for invasive surgical procedures. The indication for arthroscopy/open surgery in our study was detection of ligament tears on imaging and one of the following clinical scenarios: Persistent and debilitating symptoms despite a trial of conservative management, young patients who are actively involved in sports activities and wish to get the ligament tear repaired, patients presenting within 6 weeks of trauma with associated fractures. Arthroscopy/surgery was performed in 16 patients by one of the two fellowship-trained orthopedic surgeons (Orthopedic surgeon 1 (VS) with 10 years of experience and Orthopedic surgeon 2 (PK) with 30 years of experience). The findings recorded in arthroscopy were: presence of full-/partial-thickness ligament tears, exact location of these tears, chondromalacia, synovitis, and degenerative changes in the joint.
Statistical analysis
Confidence levels of 2 and 3 (definite and probable tear) were taken as affirmative for the presence of tear. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated separately for FS PD/T2, MEDIC conventional MR sequences, and MR arthrography. In addition, kappa values were calculated for determining the strength of agreement between MR arthrography and arthroscopy in delineating the location of tears.
Results
The spectrum of findings seen in our study population is summarized in Table 2. A total of 24 (45.3%) TFCC tears, 13 (25.5%) SLL tears, and 11 (21.4%) LTL tears were diagnosed in 53 patients. Multiple findings were present in 23 patients. The findings were grouped under two categories: ligament affected (TFCC tear, SLL tear, and LTL tear), and the location of tear. MR arthrography helped to detect a total of 16 additional tears overall and 8 additional tears in patients who underwent surgery/arthroscopy, compared to conventional MRI. Detailed MRI findings listing the type and location of ligament tear in each of the 16 patients who underwent arthroscopic/surgical correlation are depicted in Table 3. The results of statistical analysis are summarized in Table 4. The indications and details of surgical procedures performed are provided in Table 5.
Table 2.
Radiologic findings in the study population*
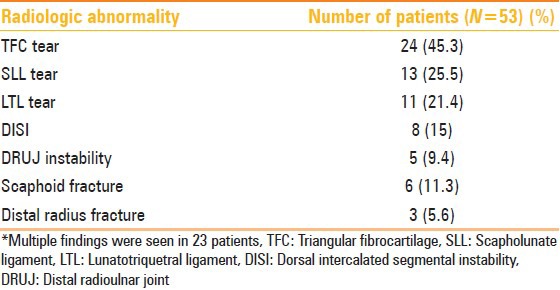
Table 3.
Detailed MRI and arthroscopic findings listing type and location of ligament tear in each of the 16 patients who underwent arthroscopic/surgical correlation
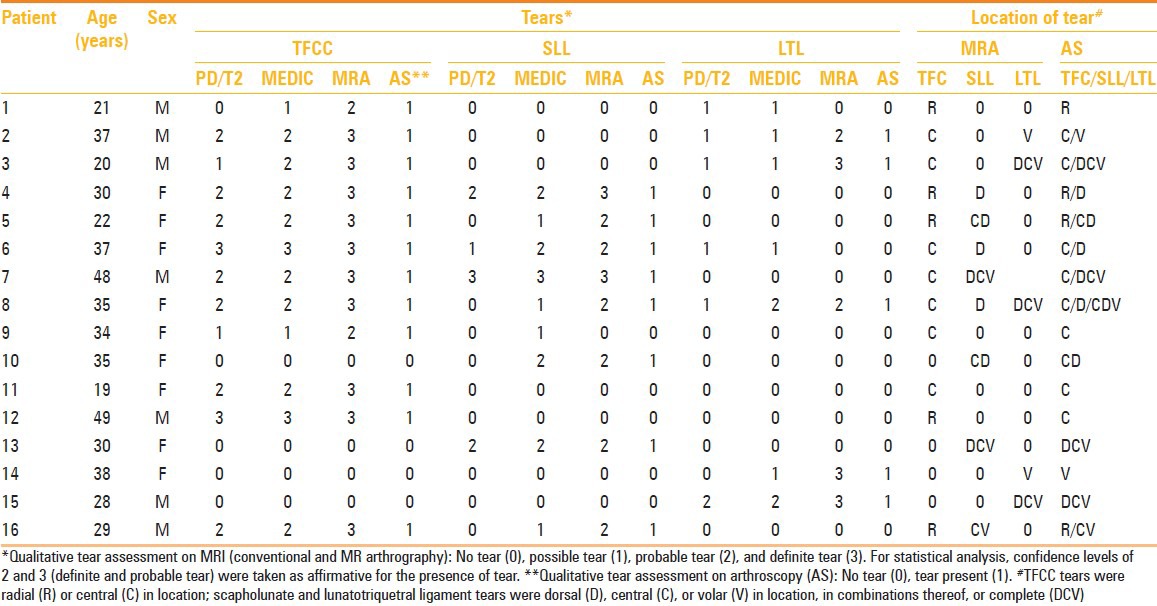
Table 4.
MR imaging findings versus arthroscopy findings
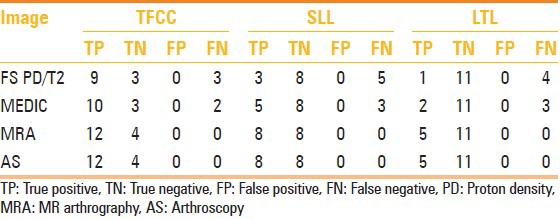
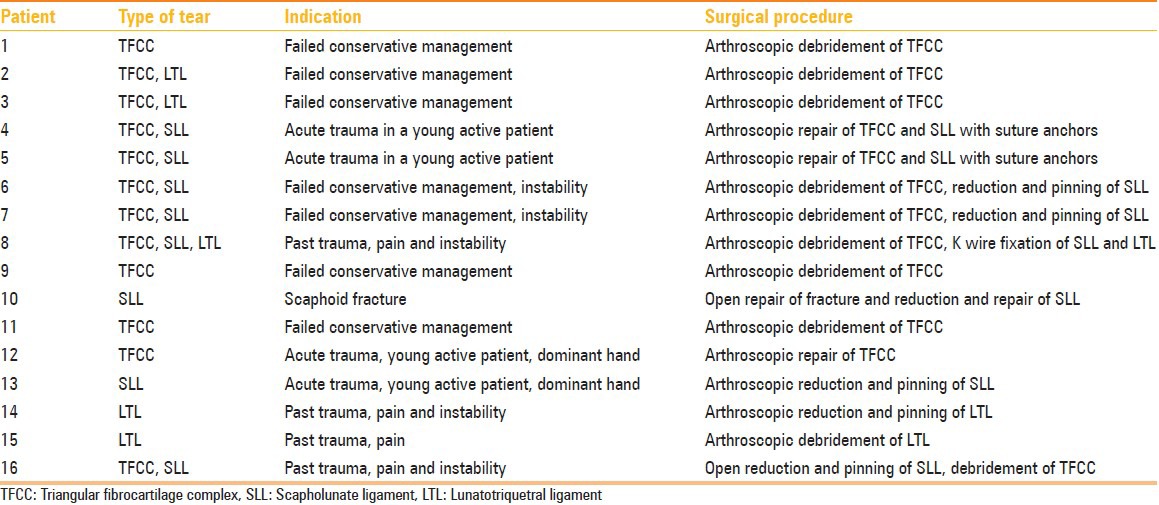
Table 5.
Indications and surgical procedures performed in 16 patients
Detection of TFCC tears
Triangular Fibrocartilage Complex tears were diagnosed in 24 (45.3%) patients. Twelve full-thickness TFC tears were found in 16 patients who underwent arthroscopy/open surgery, out of which 9 tears were detected on FS PD/T2 sequence, 10 on MEDIC sequence, and all 12 were detected on MR arthrography; statistical analysis was performed for these 16 patients [Figures 1–5]. We did not encounter any partial-thickness tears in our study. FS PD/T2 sequence showed a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 75%, 100%, 90%, 50%, and 75%, respectively, for the detection of TFC tears, while MEDIC sequence showed a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 83.3%, 100%, 90.9%, 60%, and 81.25%, respectively. The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of MR arthrography were 100%, 100%, 100%, 100%, and 100%, respectively.
Figure 1.

TFC tear in a 21 year old male with wrist pain of 1 year duration. Coronal FS T1W arthrogram image shows a central TFC tear (arrow)
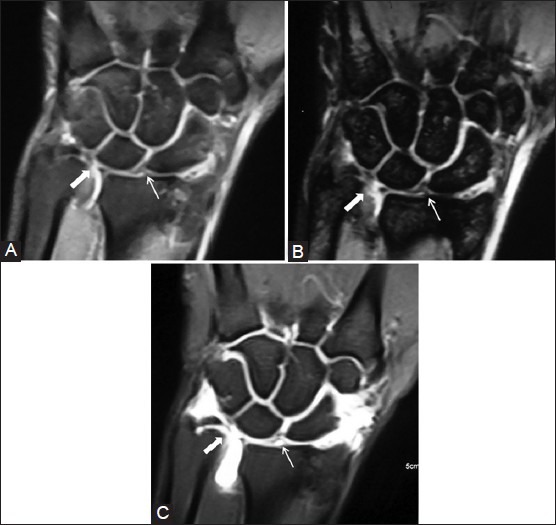
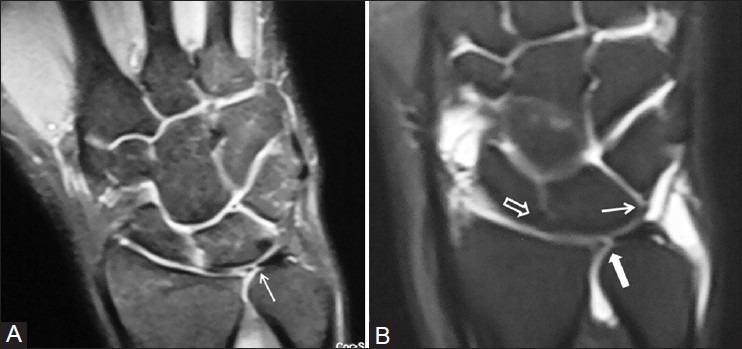
Figure 5 (A-B).
Scapholunate and lunatotriquetral ligament tears in a 30 year old woman with wrist pain since 1 year. A defect is seen in the scapholunate ligament (bold arrow); TFC and the lunatotriquetral ligament (thin arrow) are apparently intact on coronal MEDIC image (A). However, coronal MR arthrogram image (B) shows a radial tear of TFC (open arrow) and a tear of the lunate attachment of lunatotriquetral ligament (thin arrow), with contrast extending into the gap and reaching into the midcarpal joint; scapholunate ligament tear is also well visualized (bold arrow). All the tears were confirmed on arthroscopy
According to location, TFC tears were classified as radial, central, and ulnar. There were 14 (41.7%) central tears and 10 radial tears; no ulnar-sided tears were found in our study. The strength of agreement between MR arthrography and arthroscopy for delineating the location of tear was good (κ = 0.999), and the correlation between MR arthrography and arthroscopy was significant (P = 0.0003).
Detection of SLL tears
Scapholunate ligament tears were diagnosed in 13 (25.5%) patients. Eight SLL tears were found in 16 patients who underwent arthroscopy/open surgery and statistical analysis was done for these patients [Figures 2, 3, and 5]. All eight tears were detected on MR arthrography, five tears were detected on MEDIC, and only three tears were picked up on FS PD/T2 sequence. FS PD/T2 sequence showed a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 37.5%, 100%, 100%, 61.5%, and 68.8%, respectively, for detecting SLL tears. MEDIC sequence showed a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 62.5%, 100%, 100%, 72.7%, and 81.3%, respectively, and MR arthrography showed a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 100%, 100%, 100%, 100%, and 100%, respectively. It was possible to make a diagnosis of SLL tear with a high confidence level (probable/definite tear) in all the patients on MR arthrogram.
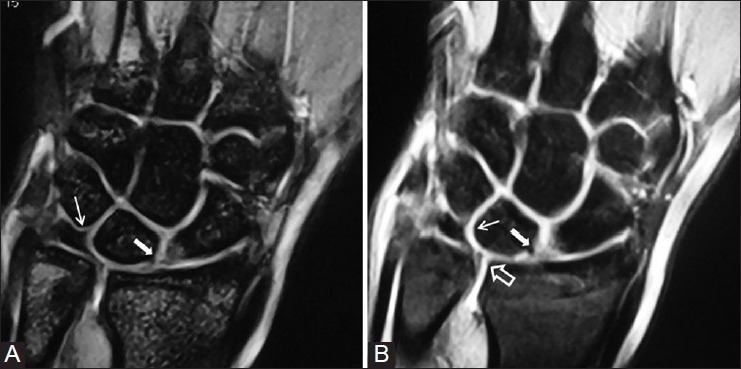
Figure 2.
TFC and scapholunate ligament tear in a 38 year old man with wrist pain of 6 months duration after trauma: Coronal 3D MEDIC image shows complete disruption of the scapholunate ligament (thick arrow). Central tear of the TFC is also present (thin arrow)
Figure 3 (A-C).
TFC and scapholunate ligament tears in a 35 year old man. Coronal PD (A) and MEDIC (B) images show a central TFC tear (bold arrow) with fluid in distal radioulnar joint, but the scapholunate ligament appears intact (arrow). However, MR arthrogram (C) clearly depicts a scapholunate ligament tear with contrast extending into the midcarpal joint through the gap between scaphoid and lunate. The frayed, coapted ends of the torn scapholunate ligament have now separated; lunatotriquetral ligament is intact
According to location, SLL tears were classified as volar, membranous, dorsal, volar plus membranous, dorsal plus membranous, and complete on coronal and axial MR arthrography images. Five volar segment tears, three dorsal segment tears, two tears involving both the central and dorsal segments, one tear involving both the central and dorsal segments, and two complete tears of SLL were seen on MR arthrography. The strength of agreement between MR arthrography and arthroscopy for delineating the location of tear was good (κ = 0.999), and the correlation between MR arthrography and arthroscopy was significant (P = 0.001).
Detection of LTL tears
Lunatotriquetral ligament tears were diagnosed in 11 (21.4%) patients. Five LTL tears were found in 16 patients who underwent arthroscopy with or without open surgery [Figure 5] and statistical analysis was done for these patients. MR arthrography detected all five tears, two tears were diagnosed on MEDIC, and only one tear was visualized on FS PD/T2 sequence [Figures 4 and 5]. FS PD/T2 sequence showed a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 20%, 100%, 100%, 73.3%, and 75%, respectively, for detecting LTL tears. MEDIC sequence had a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 40%, 100%, 100%, 72.7%, and 81.3%, respectively, and MR arthrography had a sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 100%, 100%, 100%, 100%, and 100%, respectively.
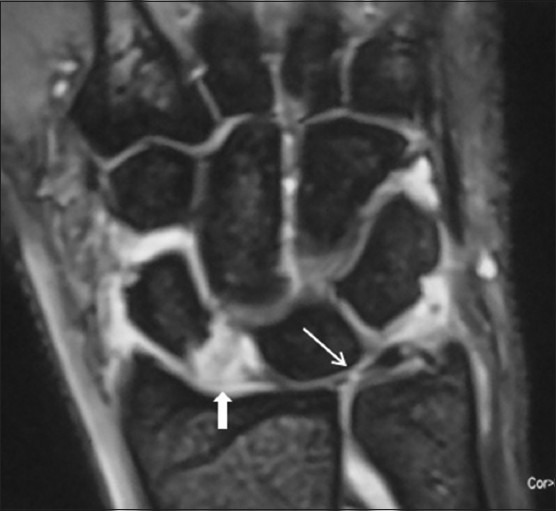
Figure 4 (A and B).
TFC and lunatotriquetral ligament tears in a 28 year old male patient. Coronal PD image (A) shows a central TFC tear (arrow) with doubtful tears of scapholunate and lunatotriquetral ligaments. Apart from the TFC tear (bold arrow), a defect in the lunatotriquetral ligament is outlined by gadolinium in coronal MR arthrogram image (B) with contrast extending into the midcarpal joint (arrow); the scapholunate ligament is confirmed to be intact (open arrow). Both the tears were arthroscopically confirmed
According to location, LTL tears were classified as volar, membranous, dorsal, volar plus membranous, membranous plus dorsal, and complete on coronal and axial MR arthrography images. Two volar segment tears, one dorsal segment tear, one tear involving both the central and volar segments, and three complete LTL tears were seen on MR arthrography. The strength of agreement between MR arthrography and arthroscopy for delineating the location of tear was moderate (κ = 0.6667), and the correlation between MR arthrography and arthroscopy was significant (P = 0.0206). A diagnosis of ligament tear was made with a high confidence level (probable/definite tear) in all the patients on MR arthrogram.
Discussion
The accuracy of history and clinical examination in diagnosing and localizing wrist ligament tears is very poor. We need to arrive at a proper diagnosis before we discuss the treatment options available to a patient suspected of having a ligament tear. Furthermore, the orthopedic surgeons need a road map before they take up patients for invasive surgical procedures. Direct MR arthrography is a simple procedure that combines the advantages of standard MRI and conventional arthrography by achieving joint distension. This improves detectability of small intra-articular abnormalities. According to the appropriateness criteria laid down by the American College of Radiology (ACR Appropriateness Criteria), direct MR arthrography is an appropriate imaging modality if wrist ligament tears are suspected and radiographs are normal or non-specific, especially in patients with ulnar-sided wrist pain.[15] It has the highest accuracy for diagnosing abnormalities of the TFCC and intrinsic ligaments. The ACR guidelines further state that direct MR arthrography is more sensitive than conventional MRI performed at 3T MRI for intrinsic ligament (SLL and LTL) tears, and that 3T MRI can be used as an alternative for detecting TFCC tears when direct MR arthrography is not available.[15,16]
The treatment of wrist ligament injuries aims at relieving pain, restoring stability, and maintaining mobility of the wrist. The natural course of wrist ligament tears is progressive restriction of motion and debility, especially with TFCC and SLL tears. Earlier intervention leads to better results, and hence, timely diagnosis and management of wrist ligament tears is necessary to preserve wrist function. The actual management decision takes into account a number of patient-specific factors (age, activity level of the patient, whether the involved hand is dominant or non-dominant), as well as factors related to the injury (time elapsed since injury, traumatic or degenerative tear, associated fractures, type of ligament involved, location of tear).
Palmer[17] classified TFCC lesions into those resulting from an isolated traumatic event (class I) and those resulting from recurrent insults with insidious degeneration (class II). The central 80-85% of TFC is avascular and has no potential for healing, whereas the peripheral 15-20% of the articular disk and volar and dorsal radioulnar ligaments are well vascularized and capable of healing.[3,18,19] Hence, class IA (central tears) and ID (peripheral radial tears) lesions are treated by debridement, whereas class IB and IC lesions (peripheral and ulnar in location) are sutured. Class II injuries constitute the spectrum of ulnocarpal abutment syndrome,[7] which is due to an ulna longer than radius, resulting in excessive load bearing through the ulnar carpus, causing central degenerative tears in the TFCC. These tears are addressed by debridement; positive ulnar variance can be corrected by surgical procedures such as corrective osteotomies and wafer procedure.
Scapholunate ligament and LTL injuries have been described in association with scaphoid fracture, perilunate dislocation, and a number of other patterns of wrist instability. Tears of the thick volar and dorsal portions of these ligaments can cause instability of the scapholunate joint, and untreated SLL injuries can produce a common form of osteoarthritis of the wrist – scapholunate advanced collapse (SLAC) – with debilitating restriction of motion.[18] Therefore, orthopedic surgeons are always concerned about the integrity of the SLL and try to surgically repair SLL tears whenever possible.
A broad outline of the protocol followed at our institute for management of wrist ligament injuries is depicted in Figure 6. As previously mentioned, only patients with MRI evidence of a ligament tear and fulfilling certain clinical criteria were taken up for surgical procedures. Patient with normal MRI findings were not taken up for surgery to avoid unnecessary invasive procedures. Many patients with chronic ligament tears responded well to conservative management (analgesics, immobilization with a supportive cast). Arthroscopic debridement resulted in symptomatic improvement in patients who did not respond to conservative measures [Figure 4]. Ligament repair using arthroscopic or open surgical techniques (using bone anchoring sutures, pinning with K-wires) was performed in patients who presented with fractures or SLL tears [Figure 2]. Surgical repair restored full range of motion and provided pain relief as well in these patients. Reconstructive procedures for chronic injury are not performed at our institute.
Figure 6.
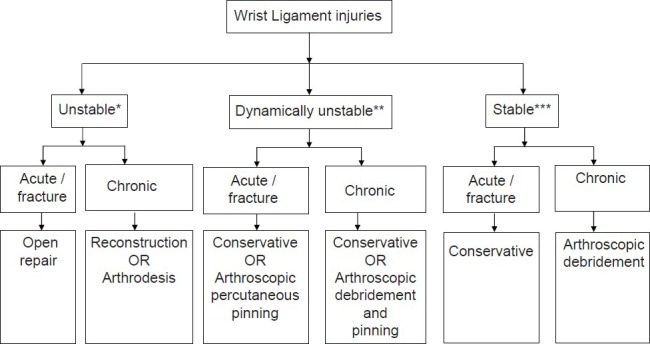
Flowchart depicting treatment algorithm for wrist ligament injuries at our institute (stability of injuries is assessed on clinical examination, radiographs, and MRI; *unstable injury = visible deformity on radiographs; **dynamically unstable injury = instability elicited by stress views or fluoroscopy; ***stable injury = ligamentous injury without instability/deformity on stress views or at rest)
We attempted to standardize the technique for MRI imaging of wrist because different studies in the literature have used different sequence protocols. T1-weighted and FS PD/T2-weighted images were helpful in assessing marrow signal abnormalities as seen in ulnocarpal abutment syndrome, fractures, and avascular necrosis of bone. MEDIC sequence exquisitely depicted the ligament morphology on non-enhanced MRI. MR arthrography consistently picked up more tears, and it either completely excluded the possibility of a tear or provided a higher diagnostic confidence level (“probable”/“definite” tear) in cases diagnosed with a low confidence (“possible tears”) on FS PD/T2 or MEDIC sequence.
The current literature recommends acquiring FS PD/T2-weighted or MEDIC images in coronal plane to evaluate ligament pathology.[9,11,20] We recommend that MEDIC sequence acquired at 1 mm slice thickness should form an integral part of MR protocol for evaluation of wrist. MEDIC is a T2 weighted gradient-echo sequence optimized for orthopedic imaging - the joint fluid is hyperintense and the images produced have an “arthrographic quality.” MEDIC sequence combines multiple echoes with a high receiver bandwidth, in contrast to other gradient sequences which use a single low-bandwidth echo. Hence, MEDIC achieves a higher signal-to-noise ratio, and eliminates susceptibility gradients and chemical shifts which cause image degradation in other gradient sequences. Although FS PD/T2 sequences achieve similar signal intensities, MEDIC is still preferable over them because it attains more superior differentiation between fluid and cartilage signal. T1W axial images were acquired in all patients to assess DRUJ instability. Additional axial FS PD/T2-weighted images were acquired in patients with suspected SLL and LTL tears to evaluate individual components of the torn ligament (volar, central, and dorsal). These were not acquired in all patients due to time constraints. Sagittal T1W images displayed the static alignment of the carpal bones.
We chose direct MR arthrography over indirect MR arthrography because firstly, this technique fully distends the joint cavity and outlines ligament defects, and secondly, it can depict the precise location of the ligamentous defect. We performed fluoroscopy-guided single-compartment arthrography of the radiocarpal joint. The three-compartment arthrogram (DRUJ, radiocarpal and midcarpal joint injection) was considered the standard technique to evaluate the integrity of TFCC and interosseous ligaments by earlier authors.[21,22] However, subsequent authors described a false-negative rate of only 2% for complete perforations and 10% for complete and partial perforations together for single-compartment arthrograms of the radiocarpal joint.[1,23] We achieved a technical success rate of 100% for radiocarpal joint injection, and apart from mild pain lasting a few hours, no other complication was encountered. Diagnostic quality images were obtained in all patients. We acquired FS T1W sequences in coronal, sagittal, and axial planes. TFCC tears were best assessed on coronal and sagittal images, whereas SLL and LTL tears were assessed on coronal and axial images.
All the components of TFC complex were consistently visualized on non-enhanced MRI as well as MR arthrography. The volar and dorsal radioulnar ligaments, the ulnolunate and ulnotriquetral ligaments, and the ulnar collateral a ligament were best depicted on MEDIC sequence and MR arthrography. The SLL and LTL were consistently visualized on non-enhanced MRI as well as MR arthrography, but the individual components of these ligaments were best evaluated by axial images on MR arthrography.
Zlatkin et al.[12] reported a sensitivity of 89%, specificity of 92%, and an accuracy of 90% for non-enhanced MRI for evaluation of TFCC tears, when compared with arthroscopy and arthrotomy. These values were 86%, 100%, and 95%, respectively, for SLL tears, and 50%, 80%, and 100%, respectively, for LTL tears. They did not include MR arthrography in their study. Schweitzer et al.[13] found an average sensitivity of 52%, specificity of 91%, and accuracy of 77% for MRI imaging in the evaluation of TFCC tears, with arthroscopy as the standard. For SLL injuries, the sensitivity, specificity, and accuracy were 25%, 56%, and 64%, respectively, whereas the same values for LTL tears were 31%, 90%, and 78%, respectively. They did not separately compare unenhanced MRI and MR arthrography with arthroscopy. Scheck et al.[14] reported average sensitivities, specificities, and accuracies of 80%, 60%, and 70%, respectively, on non-enhanced MRI imaging and 90%, 100%, and 95%, respectively, on MR arthrography for diagnosis of full-thickness TFC tears, using wrist arthroscopy as the standard of reference. They found sensitivity and specificity values of 52% and 34%, respectively, for non-enhanced MRI and 90% and 87%, respectively, for MR arthrography in detecting SLL tears, and sensitivity and specificity of 89% and 64%, respectively, with conventional MRI and 100% and 90%, respectively, with MR arthrography for diagnosing LTL tears.
None of these studies evaluated the individual diagnostic performance of each MR sequence. In our study, MR arthrography had a sensitivity of 100% in the detection of TFC, SLL, and LTL tears, which is better than that reported in earlier studies, and these results are similar to those reported by Scheck et al.[14] Conventional MRI sequences were less sensitive in the detection of ligament tears, but were as specific as MR arthrography, and these results are similar to those obtained by Zlatkin et al.12
Earlier studies did not assess the accuracy of MRI in determining the exact location of the tear. We attempted to delineate the exact location of tears on coronal and axial MR arthrography images, and found that the strength of agreement between MRI and arthroscopy for delineating the location of TFCC and SLL tears was good (κ = 0.999), whereas the strength of agreement between MRI and arthroscopy for delineating the location of lunatotriquetral tears was moderate (κ = 0.6667).
Limitations
The sample size in our study was small. There was an inherent bias as no control group of asymptomatic subjects was included. Also, an inter-slice gap of 10% (0.3 mm) was used in acquiring FS PD/T2 and MR arthrography sequences. This was because of limited time available on the MRI scanner at our institute. A single injection into the radiocarpal compartment was employed. Some non-communicating tears, therefore, may have been missed. Arthroscopic/surgical correlation could be obtained for a small number of patients in our study. This was because the orthopedic surgeons at our institute performed arthroscopy only when the imaging findings were positive and certain clinical criteria were fulfilled.
Conclusion
Diagnosis and localization of wrist ligament injuries is important to preserve the mobility and stability of wrist and hand, especially as arthroscopic and surgical techniques for wrist ligament repair become more developed. Direct MR arthrography should be an integral part of the imaging protocol when wrist ligament injuries are suspected, as this modality achieves the highest level of diagnostic confidence and also accurately delineates the location of the tear.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Stoller David W. 3rd ed. Philadelphia, USA: Lippincott William and Wilkins; 2006. Magnetic Resonance Imaging in Orthopaedics and Sports Medicine; pp. 1627–847. [Google Scholar]
- 2.Green DP. 6th ed. USA: Elsevier; 2010. Green's Operative Hand Surgery; pp. 429–745. [Google Scholar]
- 3.Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist: anatomy and function. J Hand Surg. 1981;6:153–62. doi: 10.1016/s0363-5023(81)80170-0. [DOI] [PubMed] [Google Scholar]
- 4.Smith DK. Scapholunate interosseous ligament of the wrist: MR appearances in asymptomatic volunteers and arthrographically normal wrists. Radiology. 1994;192:217–21. doi: 10.1148/radiology.192.1.8208941. [DOI] [PubMed] [Google Scholar]
- 5.Smith DK, Snearly WN. Lunotriquetralinterosseous ligament of the wrist: MR appearances in asymptomatic volunteers and arthrographically normal wrists. Radiology. 1994;191:199–202. doi: 10.1148/radiology.191.1.8134570. [DOI] [PubMed] [Google Scholar]
- 6.Hobby JL, Dixon AK, Bearcroft PW, Tom BD, Lomas DJ, Rushton N, et al. MR imaging of the wrist: Effect on clinical diagnosis and patient care. Radiology. 2001;220:589–93. doi: 10.1148/radiol.2203001429. [DOI] [PubMed] [Google Scholar]
- 7.Cerezal L, Abascal F, Garcia-Valtuille R, del Pinal Wrist arthrography: How, why, when. Radiol Clin North Am. 2005;43:709–31. doi: 10.1016/j.rcl.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Zlatkin MB, Chao PC, Osterman AL, Schnall MD, Dalinka MK, Kressel HY. Chronic wrist pain: evaluation with high resolution MR imaging. Radiology. 1989;173:723–9. doi: 10.1148/radiology.173.3.2813777. [DOI] [PubMed] [Google Scholar]
- 9.Schweitzer ME, Brahme SK, Hodler J, Hanker GJ, Lynch TP, Flannigan BD, et al. Chronic wrist pain: spine-echo and short term inversion recovery MR imaging and conventional and MR arthrography. Radiology. 1992;182:205–11. doi: 10.1148/radiology.182.1.1727283. [DOI] [PubMed] [Google Scholar]
- 10.Scheck RJ, Romagnolo A, Hierner R, Pfluger T, Wilhelm K, Hahn K. The carpal ligaments in MR arthrography of wrist: Correlation with standard MRI and wrist arthroscopy. J Magn Reson Imaging. 1999;9:468–74. doi: 10.1002/(sici)1522-2586(199903)9:3<468::aid-jmri16>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 11.Haims AH, Schweitzer ME, Morrison WB, Deely D, Lange R, Osterman AL, et al. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol. 2002;178:419–22. doi: 10.2214/ajr.178.2.1780419. [DOI] [PubMed] [Google Scholar]
- 12.Scheck RJ, Kubitzek C, Hierner R, Szeimies U, Pfluger T, Wilhelm K, et al. The scapholunate interosseous ligament in MR arthrography of the wrist: correlation with non-enhanced MRI and wrist arthroscopy. Skeletal Radiol. 1997;26:263–71. doi: 10.1007/s002560050233. [DOI] [PubMed] [Google Scholar]
- 13.Zanetti M, Bräm J, Hodler J. Triangular fibrocartilage and intercarpal ligaments of the wrist: Does MR arthrography improve standard MR imaging? J Magn Reson Imaging. 1997;7:590–4. doi: 10.1002/jmri.1880070322. [DOI] [PubMed] [Google Scholar]
- 14.Oneson SR, Timins ME, Scales LM, Erickson SJ, Chamoy L. MR imaging diagnosis of triangular fibrocartilage pathology with arthroscopic correlation. Am J Roentgenol. 1997;168:1513–8. doi: 10.2214/ajr.168.6.9168716. [DOI] [PubMed] [Google Scholar]
- 15.ACR Appropriateness Criteria®. Overview. Rubin: American College of Radiology; 2012. Electronic copies: Available in Portable Document Format (PDF) from the American College of Radiology (ACR) Web site [Google Scholar]
- 16.Magee T. Comparison of 3T MRI and arthroscopy of intrinsic wrist ligament and TFCC tears. AJR Am J Roentgenol. 2009;192:80–5. doi: 10.2214/AJR.08.1089. [DOI] [PubMed] [Google Scholar]
- 17.Palmer AK. Triangular fibrocartilage complex lesions: A classification. J Hand Surg Am. 1989;14:594–605. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 18.Morris PJ, Wood WC. 2nd ed. New York, USA: Oxford University Press; 2000. Oxford's Textbook of Surgery; pp. 2068–3078. [Google Scholar]
- 19.Thiru-Pathi RG, Ferlic DC, Clayton MC, McLure DC. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg. 1986;20B:178–84. doi: 10.1016/s0363-5023(86)80065-x. [DOI] [PubMed] [Google Scholar]
- 20.Cerezal L, Abascal F, Garcia-Valtuille R, del Pinal F. Imaging findings in ulnar-sided wrist impaction syndromes. RadioGraphics. 2002;22:105–21. doi: 10.1148/radiographics.22.1.g02ja01105. [DOI] [PubMed] [Google Scholar]
- 21.Levinsohn ME, Rosen DI, Palmer AK. Wrist arthrography: Value of the three-compartment injection method. Radiology. 1991;179:231–9. doi: 10.1148/radiology.179.1.2006283. [DOI] [PubMed] [Google Scholar]
- 22.Linkous MD, Gilula LA. Wrist arthrography today. Radiol Clin North Am. 1998;36:651–72. doi: 10.1016/s0033-8389(05)70054-3. [DOI] [PubMed] [Google Scholar]
- 23.Manaster BJ. The clinical efficacy of triple-injection wrist arthrography. Radiology. 1991;178:267–70. doi: 10.1148/radiology.178.1.1984317. [DOI] [PubMed] [Google Scholar]


