Abstract
Morel-Lavallée lesions are post-traumatic, closed degloving injuries occurring deep to subcutaneous plane due to disruption of capillaries resulting in an effusion containing hemolymph and necrotic fat. Magnetic resonance imaging (MRI) is the modality of choice in the evaluation of Morel-Lavallée lesion. Early diagnosis and management is essential as any delay in diagnosis or missed lesion will lead to the effusion becoming infected or leading to extensive skin necrosis.
Keywords: Closed degloving injury, magnetic resonance imaging, Morel-Lavallée lesions
Introduction
Morel-Lavallée lesion is a closed degloving soft tissue injury, as a result of abrupt separation of skin and subcutaneous tissue from the underlying fascia. This condition was first decribed by French physician Maurice Morel-Lavallée in the year 1853. MRI is the modality of choice for investigation of Morel-Lavallée lesion. Early diagnosis and management of the lesion is essential so as to prevent complications like infections or extensive skin necrosis.
Case Report
A 52 year old male was brought to casualty with alleged history of road traffic accident. He was found to have hemoglobin level of 5mg/dl and was given two pints of packed red blood cell (PRBC) transfusion and stabilized. On clinical examination, he had tenderness in the left side of abdomen, contusion marks, and a fluctuant swelling in left lateral wall of abdomen, extending upto left anterolateral thigh.
Ultrasound (USG) of the fluctuant swelling in the left thigh showed a large complex septated fluid collection in the deep subcutaneous plane with internal echoes extending upto the knee [Figure 1].
Figure 1.
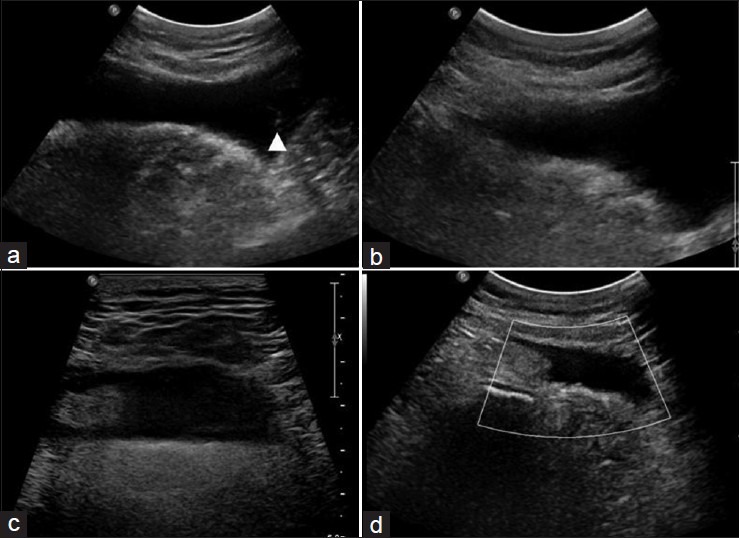
USG scan of fluctuant swelling in left anterolateral thigh showing, (a) large complex septated (arrow head) fluid collection within deep subcutaneous tissues; (b and c) fluid collection with internal echoes; (d) no evidence of vascularity
Computed tomography (CT) aortogram was done to rule out any vascular injury, which showed hypodense collection within the deep subcutaneous plane with strands of intralesional fat density suggestive of a Morel-Lavallée lesion [Figure 2].
Figure 2.
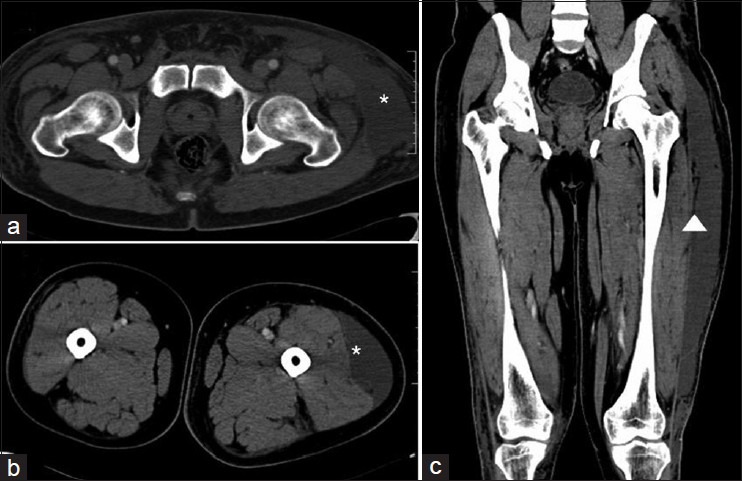
CT axial images (a and b) hypodense collection (asterisk) within deep subcutaneous tissues; Coronal image (c) streaks of fat density (arrow head) within subcutaneous collection
Magnetic resonance imaging (MRI) of left anterolateral thigh showed a well-defined crescentic collection extending along superficial fascia overlying the muscle plane, appearing hypointense with hyperintense (fat) strands on T1-weighted (T1W) images and hyperintense on T2-weighted (T2W) images [Figure 3].
Figure 3.
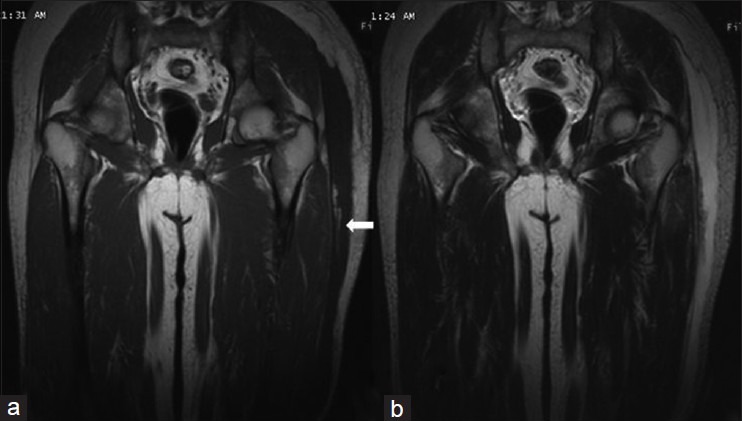
MR (a) Coronal T1W image showing, subcutaneous hypointense-fluid collection with fat density (arrow); (b) Coronal T2W image, showing hyperintense subcutaneous fluid collection
Patient was managed with percutaneous drainage and compression bandage. The lesion subsided at the time of discharge.
Discussion
Morel-Lavallée lesions are post-traumatic closed degloving soft tissue injuries where the skin and subcutaneous tissues are separated from fascia superficial to underlying muscle plane. Shear injury disrupts perforating vessels and lymphatics, thus creating a potential space filled with serosanguinous fluid, blood, and necrotic fat.
Morel-Lavallée effusions may be associated with pelvic, acetabular fractures or may also occur with blunt trauma in the absence of fracture. Morel-Lavallée lesions are most commonly seen in the trochanteric region and proximal thigh.[1,2] Clinically, Morel-Lavallée lesions usually present as an enlarging painful lesion within the anterolateral portion of affected thigh with soft tissue swelling and fluctuance. Other reported sites of involvement are the trunk, lumbar, prepatellar, and scapular regions.[3,4]
Perifascial plane gets filled up with blood, lymph, and debris due to disrupted capillaries. An inflammatory reaction results in the formation of a peripheral capsule, which may account for the perpetuation and occasional slow growth of the lesion.[1,2,4]
In an acute trauma, Morel-Lavallée lesions require surgical interventions so as to prevent infection.[2] However, these effusions may be initially missed or may take some time to develop, which can make clinical diagnosis difficult.[1,2] In longstanding cases, these lesions may subsequently enlarge and become painful, leading to misdiagnosis of soft tissue tumor.[1,2,4]
Imaging characteristics
USG features are based on the age of hematoma. The lesions appears as a focal anechoic to isoechoic complex collection located superficial to the muscle plane and deep to hypodermis. The mass may contain fat globules that appear as hyperechoic nodules along its wall.[4]
CT of a Morel-Lavallée lesion shows fluid-fluid level resulting from sedimentation of blood components and may or may not contain a capsule surrounding the lesion.
MRI is the preferred imaging modality of choice in the evaluation of Morel-Lavallée lesion. Signal characteristics of the lesion depend on chronicity and internal contents. The lesions are often homogeneously hypointense on T1W sequences and hyperintense on T2W sequences, and may resemble a simple fluid collection. The lesions may also appear homogeneously bright on both T1W and T2W sequences, which reflects a high internal concentration of methemoglobin.[5,6] The signal intensities on T1W and T2W images vary depending on the age of hematoma. Fat lobules may get entrapped within the lesion, and internal fluid-fluid levels may be present. A T1W, T2W hypointense peripheral ring representing hemosiderin and fibrous tissue may also be seen depending on the chronicity of the lesion.
Post-contrast images may show patchy enhancement both internal and peripheral to the lesion, consistent with an organizing hematoma.
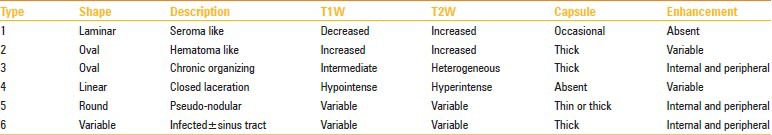
Classification of Morel-Lavallée lesion
Mellado and Bencardino proposed a classification based on the shape of lesion, signal characteristics, enhancement, and the presence or absence of a capsule.[7] Six types of lesions were described:
The differential diagnosis of the Morel-Lavallée lesion includes post-traumatic injuries like fat necrosis, coagulopathy-related hematoma, and rarely, post-traumatic early-stage myositis ossificans with diffuse subcutaneous edema. As the Morel-Lavallée lesion can clinically and radiographically simulate a malignant tumor, careful evaluation for a prior history of trauma can be very useful in suggesting the correct diagnosis.
Treatment
Once the lesion is identified, the hematoma should be evacuated and necrotic material removed. Neglected lesions can become infected[8,9] and progression of lesion may lead to extensive skin necrosis. Conservative treatment with compression can be utilized for small acute lesions without a definite capsule.[10] Presence of a capsule would render conservative or percutaneous treatment unsuccessful, thus leading to recurrence if not managed surgically.[11] Percutaneous drainage and sclerodesis using talc and doxycycline have been reported to be effective.[12]
Conclusion
Morel-Lavallée lesions are post-traumatic, closed degloving injuries occurring in the subcutaneous plane superficial to the muscle plane due to disruption of capillaries resulting in an effusion containing hemolymph and necrotic fat. MRI is the modality of choice in the evaluation of Morel-Lavallée lesion. Early diagnosis and management is essential. Presence of a capsule indicates the choice of surgery over conservative management of the lesion.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Letournel E, Judet R. 2nd ed. Berlin, Germany: Springer-Verlag; 1993. Fractures of the acetabulum. [Google Scholar]
- 2.Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: The Morel-Lavallée lesion. J Trauma. 1997;42:1046–51. doi: 10.1097/00005373-199706000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Kottmeier SA, Wilson SC, Born CT, Hanks GA, Iannacone WM, Delong WG. Surgical management of soft tissue lesions associated with pelvic ring injury. Clin Orthop Relat Res. 1996;329:46–53. doi: 10.1097/00003086-199608000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Parra JA, Fernandez MA, Encinas B, Rico M. Morel-Lavallée effusions in the thigh. Skeletal Radiol. 1997;26:239–41. doi: 10.1007/s002560050228. [DOI] [PubMed] [Google Scholar]
- 5.Rubin JI, Gomori JM, Grossman RI, Gefter WB, Kressel HY. High-field MR imaging of extracranial hematomas. AJR Am J Roentgenol. 1987;148:813–7. doi: 10.2214/ajr.148.4.813. [DOI] [PubMed] [Google Scholar]
- 6.Bush CH. The magnetic resonance imaging of musculoskeletal hemorrhage. Skeletal Radiol. 2000;29:1–9. doi: 10.1007/s002560050001. [DOI] [PubMed] [Google Scholar]
- 7.Mallado JM, Bencardino JT. Morel-Lavellee lesion: Review with Emphasis on MR imaging. Magn Reson Imaging Clin N Am. 2005;13:775–82. doi: 10.1016/j.mric.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Mellado JM, Perez del Palomar L, Diz L, Ramos A, Sauri A. Long standing Morel-Lavallée lesions of the trochanteric region and proximal thigh: MRI features in five patients. AJR Am J Roentgenol. 2004;182:1289–94. doi: 10.2214/ajr.182.5.1821289. [DOI] [PubMed] [Google Scholar]
- 9.Hudson DA, Knottenbelt JD, Krige JE. Closed degloving injuries: Results following conservative surgery. Plast Reconstr Surg. 1992;8:853–5. doi: 10.1097/00006534-199205000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Harma A, Inan M, Ertem K. The Morel-Lavallee lesion: A conservative approach to closed degloving injuries. Acta Orthop Traumatol Turc. 2004;38:270–3. [PubMed] [Google Scholar]
- 11.Gilbert BC, Bui-Mansfield LT, Dejong S. MRI of a Morel-Lavallee Lesion. AJR Am J Roentgenol. 2004;182:1347–8. doi: 10.2214/ajr.182.5.1821347. [DOI] [PubMed] [Google Scholar]
- 12.Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee Lesion of the Knee Twenty-Seven Cases in the National Football League. Am J Sports Med. 2007;35:1162–7. doi: 10.1177/0363546507299448. [DOI] [PubMed] [Google Scholar]


