Abstract
Objective
To examine the association of patient- and medication-related factors with post-discharge medication errors.
Patients and Methods
The Vanderbilt Inpatient Cohort Study (VICS) includes adults hospitalized with acute coronary syndromes (ACS) and/or acute decompensated heart failure (ADHF). We measured health literacy, subjective numeracy, marital status, cognition, social support, education, income, depression, global health status, and medication adherence in patients enrolled between October 2011 and August 2012. We used binomial logistic regression to determine predictors of discordance between the discharge medication list and patient-reported list during post-discharge medication review.
Results
Among 471 patients, mean age was 59 years; mean total number of medications reported was 12; and 17% had inadequate or marginal health literacy. Half (51%) of patients had ≥1 one discordant medication (i.e., appeared either on the discharge or patient-reported list but not both); 27% failed to report a medication on their discharge list; and 36% reported a medication not on their discharge list. Additionally, 59% had a misunderstanding in indication, dose, or frequency in a cardiac medication. In multivariable analyses, higher subjective numeracy (Odds Ratio (OR)=0.81, 95% Confidence Interval (CI) 0.67-0.98) was associated with lower odds of having discordant medications. For cardiac medications, participants with higher health literacy (OR=0.84, CI 0.74-0.95), higher subjective numeracy (OR=0.77, CI 0.63-0.95), and who were female (OR=0.60, CI 0.46-0.78) had lower odds of misunderstandings in indication, dose, or frequency.
Conclusion
Medication errors are present in approximately half of patients following hospital discharge and are more common among patients with lower numeracy or health literacy.
Keywords: medication errors, health literacy, hospital discharge, patient safety
Introduction
Frequently the discharge process is rushed and disjointed, despite the critical importance of communicating with patients about post-discharge medications. Healthcare providers may not effectively counsel patients regarding medications on the discharge instructions.1 Likewise, patients may have difficulties understanding the changes to their medication regimen, due to limitations in health literacy, numeracy, and other patient factors.2-4 Post-discharge medication errors are common,2 but the patient-related factors associated with such errors are not well understood.
Health literacy, the ability to understand and act upon medical information,5 and numeracy, “the ability to use and understand numbers in daily life”,6 have been associated with medication understanding and adherence.7,8,9 Additionally, other patient factors such as cognitive impairment,10 poor social support,11 and depression12 have been associated with post-discharge outcomes, like unscheduled healthcare utilization or adverse events in patients with cardiovascular disease. However, the independent association of these factors with post-discharge medication errors has not been examined in this population.
Post-discharge medication errors are important because they significantly contribute to adverse drug events (ADEs), or harm due to medications.13-15 Medication errors include: omissions, commissions, and misunderstandings in indication, dose, or frequency.10-13 Errors can be due to differences between medications the patient thinks s/he should be taking and what is prescribed, often due to poor physician-patient communication or patient-related factors, as mentioned above.16,17
Prior studies have demonstrated that 30-70% of patients have medication errors between the discharge list and the patient-reported regimen after discharge,17-21 though few studies have focused on patients with cardiovascular disease. Because multiple types of medications are prescribed and cardiac medications can cause serious harm, patients with cardiovascular disease are at higher risk for errors and ADEs after discharge.13,15,17,22-24
This manuscript describes predictors of medication errors among patients recently hospitalized for cardiovascular disease. Based on our conceptual model of factors associated with post-discharge outcomes,25 we hypothesized that low health literacy and numeracy, more medications on discharge, more changes to medications during hospitalization, impaired cognition, poor social support, low preadmission medication adherence, and depression would be associated with post-discharge medication errors.
Methods
Study setting and design
The Vanderbilt Inpatient Cohort Study (VICS) is a prospective study of patients admitted with cardiovascular disease at Vanderbilt University Hospital. The purpose of VICS is to investigate the impact of patient and social factors on post-discharge health outcomes such as medication safety, quality of life, unplanned hospital utilization, and mortality. The rationale and design of VICS are detailed elsewhere.25 Briefly, participants completed a baseline interview while hospitalized, and follow-up phone calls were conducted at approximately 2-3, 30, and 90 days post-discharge. We conducted an interim analysis of patient- and medication-related factors associated with medication errors after hospital discharge. The study was approved by the Vanderbilt University Institutional Review Board.
Patients
Eligibility screening shortly after admission identified patients with an intermediate or high likelihood of acute coronary syndrome (ACS) or acute decompensated heart failure (ADHF) per a physician's review of the clinical record. Exclusion criteria included: age less than 18 years, inability to communicate in English, unstable psychiatric illness, delirium, low likelihood of follow-up after discharge, on hospice, or otherwise too ill. To be included in this analysis, patients must have completed the medication review portion of the follow-up interview.
Baseline assessment
Consenting patients completed an interviewer-administered baseline assessment of demographic information including: self-reported race, ethnicity, educational attainment, and marital status. Household income was collected using the strata from the Behavioral Risk Factor Surveillance System (BRFSS) questionnaire.26
Social support was assessed using the 7-item ENRICHD Social Support Inventory (ESSI).27,28 Patients were asked the questions regarding emotional and instrumental support. ESSI scores range from 8 to 34, with higher scores indicating more social support.
Patients completed the short form of the Test of Functional Health Literacy in Adults (s-TOFHLA),29 a timed test administered in a maximum of 7 minutes. Scores may be categorized as inadequate (0-16), marginal (17-22), or adequate (23-36).
We employed a 3-item version of the Subjective Numeracy Scale (SNS-3), which quantifies the patients' perceived quantitative abilities and preferences for numerical information.30 The SNS-3 has a correlation coefficient of 0.88 with the full-length SNS-8. The internal consistency reliability of the SNS-3 was high (Cronbach's alpha=0.78).30,31 The SNS is reported as the mean on a scale from 1 to 6, with higher scores reflecting better numeracy.
We assessed cognition using the Short Portable Mental Status Questionnaire (SPMSQ), a 10-item measure,32 which is adjusted for educational attainment. Higher scores reflect worse cognitive status, and may be categorized as not impaired (0-2 errors) or impaired (3-10).
Self-rated health status was assessed using five of ten items from the NIH Patient Reported Outcomes Measurement Information System (PROMIS) global health status questionnaire.33 These questions ascertain overall health, quality of life, physical and mental health, and satisfaction with social activities and relationships on a 5-point Likert-type scale. Scores are reported as a mean of the five items (range 1 to 5).
We assessed depression during the two weeks prior to the hospitalization using the Patient Health Questionnaire-8 (PHQ-8).34 Scores are categorized as none/minimal depression (0-4), mild (5-9), moderate (10-14), moderately severe (15-19), and severe (0-24).
Adherence to the pre-admission medication regimen was measured using a 7-item version of the Adherence to Refills and Medications Scale (ARMS-7).35 The ARMS-7 has a high internal consistency reliability (Cronbach's alpha=0.81) and a correlation coefficient of 0.95 with the full-length ARMS-12.36 Responses on the 4-point scale are summed for a score with a possible range of 7 to 28, where lower scores indicate better adherence.
All diagnoses at discharge were retrieved from the medical record and utilized to compute an Elixhauser score to reflect comorbid conditions.37
Medication-related data
Net changes to the patient's medication regimen during hospitalization were tallied by comparing the pre-admission medication list and discharge medication list from the electronic medical record. We did not count equipment or non-drug items (e.g., test strips), but we did include over-the-counter (OTC) medications. Cardiac medications included the following classes: anti-anginal, antiplatelet, anticoagulant, antihypertensive, cholesterol, diabetes, and diuretics. Medications were counted as changed if a dose, frequency, route, or formulation differed, or if a medication was either discontinued or initiated during hospitalization. We summed the number of all medication changes and, separately, the number of changes to cardiac medications. If dose or frequency information was missing in either the pre-admission or discharge medication list, we assumed the medication was not changed.
Outcome measures
For analyses, the discharge medication list was organized into cardiac and non-cardiac medications. The total number of medications was the sum of the medications on the discharge list plus additional patient-reported medications. Additional medications were frequently prescribed prior to hospitalization but not mentioned in the discharge list.
We contacted patients by phone 2-3 days (range 1-7) following discharge to assess all prescription and OTC medications the patient reported s/he was taking. We compared what the patient was taking to the discharge medication list, which was given to them at discharge by the bedside nurse. If patients did not report a medication that appeared on the discharge list or reported a medication not on the discharge list, it was flagged as a potentially discordant medication and probed further. If the patient did not mention the medication initially, but correctly reported it when prompted, or reported that it was stopped or started by a clinician, no error was recorded. Else, it was judged to be discordant and classified as an omission or commission.
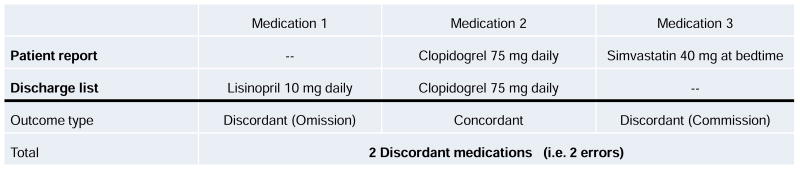
Figure 1 displays how medication errors were counted. In Panel a, a medication was coded as an omission if there was no explanation for a medication that the patient did not report but appeared on the discharge list. Omissions included instances in which the patient did not fill or refill the prescription, stopped the medication without a healthcare provider's order, or reported that s/he was not aware of the medication. A commission was coded if there was no explanation for a patient-reported medication not on the discharge list, unless a healthcare provider had instructed the patient to take the medication after discharge. A commission was also coded if the patient reported having taken a medication prior to hospitalization and continuing it after discharge, but it was not on the discharge list.
Figure 1.
Classification of medication errors identified during the post-discharge phone interview.
Panel a. Example of outcome codes for the comparison of patient report and discharge list.
Panel b. Three examples of counting misunderstandings for select cardiac medications on discharge list: lisinopril, clopidogrel, and simvastatin.
Footnotes: aExamples of other accepted indication responses for anti-platelet medications: “helps blood flow,” “for clots,” “blood thinner,” “for circulation”
bExamples of other accepted indication responses for lipid lowering medications: “high cholesterol”, “fat in blood”, “high fat”, “high LDL”
Additionally, we randomly selected one medication per cardiac type (e.g. antihypertensives) for more testing, asking the patient to provide the medication's indication, dose, and frequency. Any difference in dose or frequency between the discharge list and the patient's report was considered a misunderstanding, unless the patient reported that a healthcare provider changed the dose or frequency after discharge. Patient responses for indications were judged against a physician-created list of acceptable responses, including common off-label indications and lay terms. An example of how cardiac medication misunderstandings were counted is displayed in Figure 1, Panel b. As shown, a patient could have more than one outcome, e.g. an omission, a commission, and a misunderstanding in indication, dose, or frequency.
Analysis
We sought to examine the association between patient- and medication-related factors and the number of: discordant medications between the discharge and patient list, omissions, commissions, and misunderstandings in indication, dose, or frequency. For each outcome, a binomial logistic regression model was built to examine patient- and medication-related factors (the independent variables) associated with the odds of medication errors. The independent variables are consistent with our conceptual framework reported elsewhere,25 checked for collinearity, and included in all models: age, gender, race (African American, White, or other), marital status, primary diagnosis, education, income, health literacy, subjective numeracy, cognition, global health status, depression, number of medications changed during hospitalization, social support, medication adherence, and Elixhauser comorbidity score. Because each outcome was a count with a different number of possible errors (i.e., different denominators) across patients, the log of the number of possible errors was used as an offset. Thus, exponentiated parameter estimates are odds ratios and have the same interpretation as those from standard logistic regression models. Due to concerns regarding overdispersion, robust or sandwich-based standard errors were used to characterize estimator uncertainty. Multiple imputation was used in the multivariable analyses to avoid deleting any participants who had missing data for any of the covariates. All scale scores were treated as continuous variables for multivariable modeling. Finally, since the continuous variables operate on heterogeneous scales, we chose to quantify continuous covariate effects using odds ratios associated with inter-quartile range changes in the covariates. Data were analyzed in R.38
Results
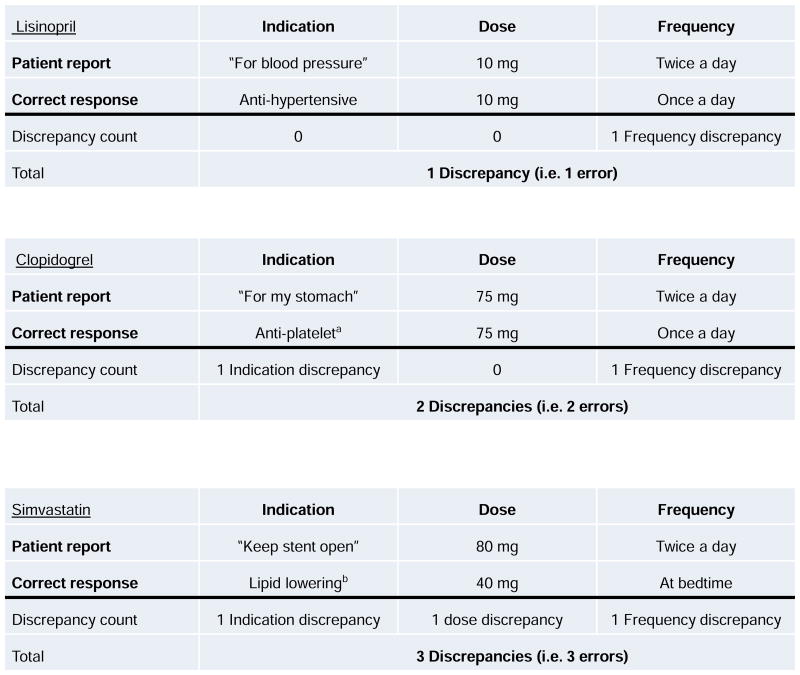
Of the 680 eligible, we enrolled 587 patients between October 2011 and August 2012. Ninety-three eligible patients (13.7%) declined enrollment (Figure 2). Of the 587 enrolled, 471 patients (80%) completed the medication review portion of the post-discharge phone interview and were included in these analyses. The remaining 116 patients did not complete the follow-up call (51), did not complete the medication review (49), withdrew (11), or died prior to discharge (5).
Figure 2.
Flow chart displaying how patient eligibility was determined.
Table 1 displays the patients' baseline characteristics. The average age was 59 years (Standard Deviation (SD) 12), 48% were female, and 19% were non-white. Most patients (71%) had diagnosis of ACS, while 8% had both ACS and ADHF. Seventeen percent (17%) of patients had inadequate or marginal health literacy. Of note, 72% of patients reported some level of depression prior to hospitalization. Participants self-reported taking an average of 12 medications post-discharge (range 1-31). Two hundred and forty two patients (51%) had at least one discordant medication; among them, the median number of discordant medications was 2 (interquartile range: 1, 3). There were 129 participants (27%) not taking a medication that was on the discharge list (an omission), and 168 (36%) were taking a medication not listed on the discharge list (error of commission). Additionally, 279 participants (59%) reported a misunderstanding in indication, dose, or frequency for at least one cardiac medication tested. Of those participants who had at least 1 medication misunderstanding, the median number of misunderstandings was 2 (interquartile range: 1, 3).
Table 1. Baseline characteristics of study sample (N=471).
| Variable | Mean (SD) or N (%) |
|---|---|
| Age, years | 59.4 (12.5) |
| Female | 226 (47.9) |
| Racea | |
| White | 380 (80.7) |
| Black | 80 (16.9) |
| All other races | 10 (2.1) |
| Marital status | |
| Single/never married | 43 (9.1) |
| Widowed | 58 (12.3) |
| Separated/divorced | 79 (16.8) |
| Married/living with partner | 291 (61.8) |
| Social support (ENRICHD), possible range 8-34 | 25.7 (4.3) |
| Education, years | |
| 0-8 | 23 (4.9) |
| 9-11 | 42 (8.9) |
| 12/GED | 135 (28.7) |
| 13-15 | 162 (34.4) |
| 16 | 63 (13.4) |
| 17+ | 46 (9.8) |
| Income, dollarsb | |
| 0 to 9,999 | 34 (7.2) |
| 10,000 to 14,999 | 30 (6.4) |
| 15,000 to 19,999 | 35 (7.4) |
| 20,000 to 24,999 | 56 (11.9) |
| 25,000 to 34,999 | 86 (18.3) |
| 35,000 to 49,000 | 78 (16.6) |
| 50,000 to 74,999 | 61 (13.0) |
| 75,000 to 99,999 | 42 (8.9) |
| 100,000 + | 39 (8.3) |
| Primary diagnosis | |
| Acute coronary syndromes (ACS) | 333 (70.7) |
| Acute decompensated heart failure (ADHF) | 99 (21.0) |
| Both ACS and ADHF | 39 (8.3) |
| Health literacy (s-TOFHLA)c | |
| Inadequate, score 0-16 | 46 (9.8) |
| Marginal, 17-22 | 33 (7.0) |
| Adequate, 23-36 | 387 (82.2) |
| Subjective numeracy (SNS), possible range 1 to 6 | 4.3 (1.4) |
| Cognition (SPMSQ) | |
| No impairment, 0-2 errors | 436 (92.6) |
| Impaired, 3-10 errors | 35 (7.4) |
| Global health status (PROMIS), possible range 1 to 5 | 2.9 (0.8) |
| Depression (PHQ-8) | |
| No depression, score 0-4 | 130 (27.6) |
| Mild depression, 5-9 | 166 (35.2) |
| Moderate, 10-14 | 112 (23.8) |
| Moderately severe, 15-19 | 44 (9.3) |
| Severe, 20-24 | 19 (4.0) |
| Medication adherence (ARMS-7)d, possible range 7 to 28 | 9.6 (2.6) |
Missing data for 1 participant;
Missing data for 10 participants;
Missing data for 5 participants;
Missing data for 8 participants
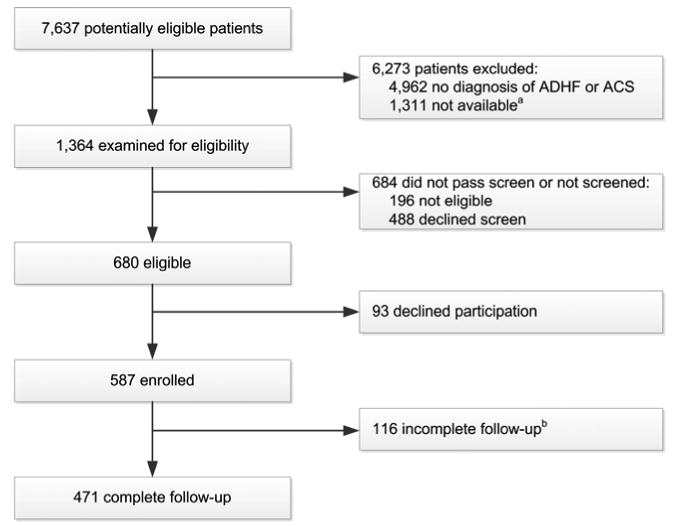
In adjusted analyses (Figure 3), higher subjective numeracy was associated with lower odds of having discordant medications (OR=0.81, CI 0.67-0.98, per 2 point change on the SNS). Being separated or divorced (OR=0.58, CI 0.34-0.98) or widowed (OR=0.58, CI 0.34-0.99) was associated with lower odds of having errors of commission. In contrast, higher levels of depression were associated with higher odds of errors of commission (OR=1.36, CI 1.00-1.85, per 8 unit change on the PHQ). Similarly, race other than White or Black (OR=2.02, CI 1.13-3.60) and higher educational attainment (OR=1.29, CI 1.06-1.56, per 4 year change) were associated with higher odds of having discordant medications, mostly attributable to errors of commission. No risk factors were significantly associated (p<0.05) with errors of omission.
Figure 3.
Factors associated with discordant medications (panel a), errors of omission (panel b), and commission (panel c), reported as odds ratio with 95% confidence intervals.
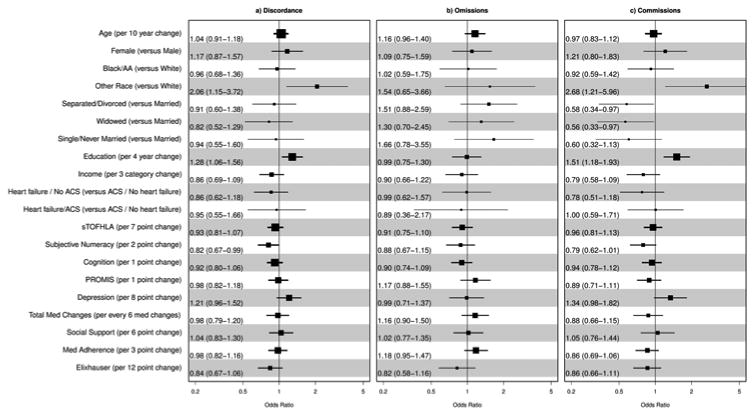
For the cardiac medications tested (Figure 4), higher health literacy (OR=0.84, CI 0.74-0.95, per 7 point change on the s-TOFHLA) and higher subjective numeracy (OR=0.77, CI 0.63-0.95, per 2 point change on the SNS) were associated with lower odds of misunderstandings in indication, dose, or frequency, mostly attributable to errors in indication. Older age (OR=1.16, CI 1.02-1.33, per 10-year change) and being single (OR=1.68, CI 1.04-2.70) were associated with higher odds of misunderstandings in indication, dose, or frequency, again mostly attributable to errors in indication (Panel a, b). Being female (OR=0.60, CI 0.46-0.78) was associated with lower odds of misunderstandings, particularly in indication and dose. Finally, worse cognitive function (OR=1.38, CI 1.05-1.82) was associated with higher odds of misunderstandings in frequency. Having a primary diagnosis of heart failure (OR=0.35, CI 0.16-0.76) was associated with lower odds of a frequency misunderstanding (Panel c).
Figure 4.
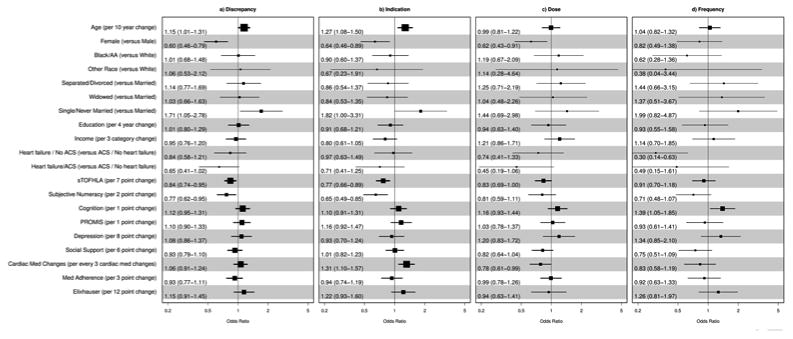
Factors associated with any misunderstanding (indication, dose, or frequency—panel a), indication (panel b), dose (panel c), and frequency (panel d).
Comments
We identified at least one medication error, or unintentional discrepancy between the discharge list and patient report, in 51% of patients. As hypothesized, higher levels of health literacy and numeracy were associated with lower odds of medication errors. However, we did not observe significant associations between medication errors and other potential risk factors – medications changed during hospitalization, poor social support, or low preadmission medication adherence.
Our results must be placed into the context of prior studies that specifically looked at post-discharge medication errors. First, the frequency of omission (27%) and commission (36%) errors are similar to what we have reported in the PILL-CVD study, which enrolled a comparable inpatient population.39 Furthermore, 41% of patients in the current study correctly reported the indication, dose, and frequency for tested cardiac medications. Prior studies have reported each outcome individually: 64-79% of patients reported the correct indication,40,41 56% the correct dosage,40 and 68% the correct frequency.40 The frequency of errors in our sample was similar to prior studies18,19,42,43 but much higher than that the 14% observed by Coleman et al.17 In their study, medication errors were assessed by a geriatric nurse practitioner (GNP) during in-home interviews of recently discharged older adults. This method may have allowed the GNP to synthesize multiple sources of information in determining the patient's correct medications.
Similar to our findings, Maniaci et al. found that there was no association between regimen knowledge and educational attainment.40 Additionally, several studies have documented an association between the number of medications and medication errors.17,39,44 However, we did not observe that relationship in these analyses.
Notably, Lindquist et al. found a similar prevalence (56%) of post-discharge medication errors in a sample of older adults.2 Lower health literacy was found to be a significant risk factor for unintentional non-adherence, which is congruent with our results.
To our knowledge, ours is the first study to demonstrate a relationship between low numeracy and post-discharge medication errors. Low numeracy has been linked to other health outcomes: poor self-efficacy and self-care in diabetes and asthma management;45,46 poorer glycemic control in diabetes;47 poorer quality of life in asthma (mediated by self-efficacy);48 and, poorer medication management in chronic diseases.49 Interestingly, in our analyses numeracy was not associated specifically with misunderstandings in dose or frequency, which are the more numerical aspects of medication instructions. Rather, numeracy was associated with having a discordant medication (errors of omission or commission) and having a misunderstanding in indication.
Strengths of this study include: relatively large sample size, high response rates, and the use of both objective and subjective measures of social determinants of health including health literacy and numeracy. We also acknowledge the limitations of our study. Our study included only patients admitted with ACS or ADHF, limiting the generalizability. We recorded but did not delve into the etiology of differences between the discharge medication list and patient report, giving patients the benefit of the doubt when reporting that a clinician had changed the regimen. Patients also could have reported what was printed on their list or bottles, as opposed to what they actually were taking, biasing our results toward the null hypothesis. Additionally, we relied on the discharge list given to the patient, which may have had errors due to suboptimal medication reconciliation practices. Patients who were too ill or refused to complete the phone interview may have been at increased risk for having medication errors, whereby our results under-estimate the frequency of errors in our sample. We did not assess clinical outcomes such as ADEs; however, health literacy has not previously been associated with ADEs.41 Although we found that patients who self-identified as other than White or Black had higher odds of having discordant medications and errors of commission, we note that this group was small. Lastly, we did not perform a Bonferroni correction for multiple testing, but we did clearly identify a pre-specified set of covariates prior to building the analytical models.
Conclusion
In summary, we determined that half of patients with ACS and/or ADHF had a medication error in the days following hospital discharge. These errors have the potential to harm patients, thus we must understand which factors are associated with an increased risk of errors. We found that patients with low health literacy and numeracy are at increased risk of medication errors; therefore, identification of patients at risk can help clinicians provide appropriate discharge medication education.
Acknowledgments
We thank Joanna Lee for organizing and entering data and Dr. Jesse Ehrenfeld for providing Elixhauser scores.
Research support: R01 HL109388 from the National Heart, Lung and Blood Institute to Dr. Kripalani, and in part by the National Center for Research Resources grant UL1 RR024975-01, now at the National Center for Advancing Translational Sciences, grant 2 UL1 TR000445-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The funding agency was not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Drs. Mixon and Kripalani had full access to all study data and take responsibility for data integrity and the accuracy of data analysis. Additionally, Dr. Mixon is a VA HSR&D Career Development awardee at the Nashville VA. The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
List of abbreviations used 3 or more times in manuscript
- ACS
Acute Coronary Syndrome
- ADEs
Adverse Drug Events
- ADHF
Acute Decompensated Heart Failure
- CI
Confidence interval
- OR
Odds ratio
Footnotes
Conflict of interest disclosures: Dr. Kripalani is a consultant to and holds equity in PictureRx, LLC. No other authors have conflicts of interest or financial disclosures.
Author contributions: Study concept and design: Mixon, Kripalani. Acquisition, analysis, and interpretation of data: Mixon, Myers, Leak, Jacobsen, Cawthon, Goggins, Nwosu, Schildcrout, Kripalani. Manuscript drafts: Mixon, Goggins, Nwosu, Schildcrout, Kripalani. Critical manuscript revisions for important intellectual content: Mixon, Myers, Leak, Jacobsen, Cawthon, Goggins, Nwosu, Schildcrout, Schnelle, Speroff, Kripalani. Statistical analysis: Goggins, Nwosu, and Schildcrout. Administrative, technical, and material support: Cawthon, Goggins, Kripalani. Study supervision: Kripalani.
Presented at Society of General Internal Medicine 35th Annual Meeting; April 25, 2013; Denver, Colorado.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cua YM, Kripalani S. Medication use in the transition from hospital to home. Annals of the Academy of Medicine, Singapore. 2008;37(2):136–141. [PMC free article] [PubMed] [Google Scholar]
- 2.Lindquist LA, Go L, Fleisher J, Jain N, Friesema E, Baker DW. Relationship of health literacy to intentional and unintentional non-adherence of hospital discharge medications. J Gen Intern Med. 2012 Feb;27(2):173–178. doi: 10.1007/s11606-011-1886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haynes KT, Oberne A, Cawthon C, Kripalani S. Pharmacists' recommendations to improve care transitions. Ann Pharmacother. 2012 Sep;46(9):1152–1159. doi: 10.1345/aph.1Q641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Archives of Internal Medicine. 2006;166(9):955–964. doi: 10.1001/archinte.166.9.955. [DOI] [PubMed] [Google Scholar]
- 5.Selden CR, Zorn M, Ratzan S, Parker RM. Current bibliographies in medicine: health literacy. Bethesda, MD: National Library of Medicine; 2000. [Google Scholar]
- 6.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med Nov. 2006;31(5):391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 7.Campbell NL, Boustani MA, Skopelja EN, Gao S, Unverzagt FW, Murray MD. Medication adherence in older adults with cognitive impairment: a systematic evidence-based review. Am J Geriatr Pharmacother. 2012 Jun;10(3):165–177. doi: 10.1016/j.amjopharm.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Loke YK, Hinz I, Wang X, Salter C. Systematic review of consistency between adherence to cardiovascular or diabetes medication and health literacy in older adults. Ann Pharmacother. 2012 Jun;46(6):863–872. doi: 10.1345/aph.1Q718. [DOI] [PubMed] [Google Scholar]
- 9.Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011 Feb;9(1):11–23. doi: 10.1016/j.amjopharm.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaudhry SI, Wang Y, Gill TM, Krumholz HM. Geriatric conditions and subsequent mortality in older patients with heart failure. J Am Coll Cardiol. 2010 Jan 26;55(4):309–316. doi: 10.1016/j.jacc.2009.07.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calvillo-King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013 Feb;28(2):269–282. doi: 10.1007/s11606-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reese RL, Freedland KE, Steinmeyer BC, Rich MW, Rackley JW, Carney RM. Depression and rehospitalization following acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011 Nov 1;4(6):626–633. doi: 10.1161/CIRCOUTCOMES.111.961896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 14.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ Canadian Medical Association Journal. 2004;170(3):345–349. [PMC free article] [PubMed] [Google Scholar]
- 15.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. Adverse drug events occurring following hospital discharge. Journal of General Internal Medicine. 2005;20:317–323. doi: 10.1111/j.1525-1497.2005.30390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. Journal of General Internal Medicine. 2008;23(9):1414–1422. doi: 10.1007/s11606-008-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coleman EA, Smith JD, Raha D, Min SJ. Posthospital medication discrepancies: prevalence and contributing factors. Archives of Internal Medicine. 2005;165(16):1842–1847. doi: 10.1001/archinte.165.16.1842. [DOI] [PubMed] [Google Scholar]
- 18.Mesteig M, Helbostad JL, Sletvold O, Rosstad T, Saltvedt I. Unwanted incidents during transition of geriatric patients from hospital to home: a prospective observational study. BMC Health Serv Res. 2010;10:1. doi: 10.1186/1472-6963-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lalonde L, Lampron AM, Vanier MC, Levasseur P, Khaddag R, Chaar N. Effectiveness of a medication discharge plan for transitions of care from hospital to outpatient settings. Am J Health Syst Pharm. 2008 Aug 1;65(15):1451–1457. doi: 10.2146/ajhp070565. [DOI] [PubMed] [Google Scholar]
- 20.Hain DJ, Tappen R, Diaz S, Ouslander JG. Cognitive impairment and medication self-management errors in older adults discharged home from a community hospital. Home Healthc Nurse. 2012 Apr;30(4):246–254. doi: 10.1097/NHH.0b013e31824c28bd. [DOI] [PubMed] [Google Scholar]
- 21.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Archives of Internal Medicine. 2006;166(5):565–571. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 22.Persell SD, Heiman HL, Weingart SN, et al. Understanding of drug indications by ambulatory care patients. American Journal of Health-System Pharmacy. 2004;61(23):2523–2527. doi: 10.1093/ajhp/61.23.2523. [DOI] [PubMed] [Google Scholar]
- 23.Unroe KT, Pfeiffenberger T, Riegelhaupt S, Jastrzembski J, Lokhnygina Y, Colon-Emeric C. Inpatient medication reconciliation at admission and discharge: A retrospective cohort study of age and other risk factors for medication discrepancies. Am J Geriatr Pharmacother. 2010 Apr;8(2):115–126. doi: 10.1016/j.amjopharm.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong JD, Bajcar JM, Wong GG, et al. Medication reconciliation at hospital discharge: evaluating discrepancies. Annals of Pharmacotherapy. 2008;42(10):1373–1379. doi: 10.1345/aph.1L190. [DOI] [PubMed] [Google Scholar]
- 25.Meyers AG, Salanitro AH, Wallston KA, et al. Determinants of health after hospital discharge: Rationale and design of the Vanderbilt Inpatient Cohort Study (VICS) 2013 doi: 10.1186/1472-6963-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System Survey Questionnaire. [Accessed March 10, 2010];2010 http://www.cdc.gov/brfss/index.htm. .
- 27.Enhancing Recovery in Coronary Heart Disease (ENRICHD) study intervention: rationale and design. Psychosom Med. 2001 Sep-Oct;63(5):747–755. [PubMed] [Google Scholar]
- 28.Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. The ENRICHD investigators. Am Heart J. 2000 Jan;139(1 Pt 1):1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 29.Nurss JR, Parker RM, Williams MV, Baker DW. Short test of functional health literacy in adults. Snow Camp, NC: Peppercorn Books and Press; 1998. [Google Scholar]
- 30.Wallston KA, McNaughton C, Storrow A, Cavanaugh K, Rothman RL. Validation of a short, 3-item version of the Subjective Numeracy Scale (SNS-3). Health Literacy Research Conference; Chicago, IL. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Medical Decision Making. 2007;27(5):672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 32.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975 Oct;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 33.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009 Sep;18(7):873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009 Apr;114(1-3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 35.Kripalani S. In: Development of the 7-item Adherence to Refills and Medications Scale (ARMS-7) Wallston KA, editor. Nashville: 2011. [Google Scholar]
- 36.Kripalani S, Risser J, Gatti M, Jacobson TA. Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low-literacy patients with chronic disease. Value in Health. 2009;12(1):118–123. doi: 10.1111/j.1524-4733.2008.00400.x. [DOI] [PubMed] [Google Scholar]
- 37.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical Care. 2009;47(6):626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 38.R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. computer program. [Google Scholar]
- 39.Salanitro AH, Osborn CY, Schnipper JL, et al. Effect of patient- and medication-related factors on inpatient medication reconciliation errors. J Gen Intern Med. 2012;27(8):924–932. doi: 10.1007/s11606-012-2003-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maniaci MJ, Heckman MG, Dawson NL. Functional health literacy and understanding of medications at discharge. Mayo Clinic Proceedings. 2008;83(5):554–558. doi: 10.4065/83.5.554. [DOI] [PubMed] [Google Scholar]
- 41.Mosher HJ, Lund BC, Kripalani S, Kaboli PJ. Association of health literacy with medication knowledge, adherence, and adverse drug events among elderly veterans. J Health Commun. 2012;17(Suppl 3):241–251. doi: 10.1080/10810730.2012.712611. [DOI] [PubMed] [Google Scholar]
- 42.Hain D, Diaz S, Tappen R, Ouslander JG. Medication discrepancies and research implications among older adults discharged home from a community hospital. Charles E. Schmidt College of Biomedical Science, Florida Atlantic University; 2011. [Google Scholar]
- 43.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stitt DM, Elliott DP, Thompson SN. Medication discrepancies identified at time of hospital discharge in a geriatric population. Am J Geriatr Pharmacother. 2011 Aug;9(4):234–240. doi: 10.1016/j.amjopharm.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 45.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011 Jul 19;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 46.Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. 2013 Mar;28(3):444–452. doi: 10.1007/s11606-012-2241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Annals of Internal Medicine. 2008;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 48.Apter AJ, Wang X, Bogen D, et al. Linking numeracy and asthma-related quality of life. Patient Educ Couns. 2009 Jun;75(3):386–391. doi: 10.1016/j.pec.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Waldrop-Valverde D, Osborn CY, Rodriguez A, Rothman RL, Kumar M, Jones DL. Numeracy skills explain racial differences in HIV medication management. AIDS Behav. 2010 Aug;14(4):799–806. doi: 10.1007/s10461-009-9604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]