Abstract
BACKGROUND
Media literacy programs have shown potential for reduction of adolescent tobacco use. We aimed to determine if an anti-smoking media literacy curriculum improves students’ media literacy and affects factors related to adolescent smoking.
METHODS
We recruited 1170 9th grade students from 64 classrooms in 3 public urban high schools. Students were randomized by classroom to a media literacy curriculum versus a standard educational program. In an intent-to-treat analysis, we used multi-level modeling to determine if changes in study outcomes were associated with the curricular intervention, controlling for baseline student covariates and the clustering of students within classrooms.
RESULTS
Among participants, mean age was 14.5 years and 51% were male, with no significant differences in baseline characteristics between groups. Smoking media literacy changed more among intervention participants compared with control participants (0.24 vs. 0.08, p < .001). Compared with controls, intervention students exhibited a greater reduction in the perceived prevalence of smoking (−14.0% vs. −4.6%, p < .001). Among those initially susceptible to smoking, intervention participants more commonly reverted to being non-susceptible post-intervention (24% vs. 16%, p = .08).
CONCLUSIONS
A school-based media literacy curriculum is more effective than a standard educational program in teaching media literacy and improving perceptions of the true prevalence of smoking among adolescents.
Keywords: media literacy, media education, smoking, tobacco, school-based, social influences, attitudes, normative beliefs, youth, adolescents
Smoking is the leading cause of preventable morbidity and mortality in the United States, killing 443,000 people each year.1 Because the vast majority of those who will die from smoking begin at age 18 or younger,2 many counter-tobacco interventions appropriately focus on youth.3 An excellent way to reach youth is in a school-based setting, because the vast majority of youth attend school. Historically, school-based anti-smoking programs have been designed using a “social influences” framework based on known risk factors, including demographic factors such as age and socioeconomic status, environmental factors such as parenting and supervision, and personal factors such as sensation seeking and rebelliousness.3,4 However, these programs have not resulted in long-term reduction in tobacco use.3,4
One reason that these programs may have been ineffective is that they underestimated the influence of media on youth behavior. Youth aged 8–18 are now exposed to over 10 hours of media content each day,5 including a substantial number of positive impressions of cigarette smoking.6–10 Research has demonstrated that youth who are exposed to smoking in films are significantly more likely to smoke themselves, with 30%–50% of smoking initiation directly linked to frequent exposure to smoking in movies.11,12 Exposure to mass media promotions and advertisements also significantly increases the risk of smoking initiation in adolescents.13
“Media literacy” aims to buffer this impact of mass media on adolescents’ smoking by empowering youth to analyze and evaluate these media messages actively instead of being passive message targets.14–21 According to the Theory of Reasoned Action (TRA), a well-accepted, broadly-applied theory of health behavior that has been used to predict adolescent smoking,22–24 an individual’s behavior is determined by his or her intentions to perform the behavior, which is in turn predicted by his or her attitudes toward the behavior and sense of subjective normative beliefs regarding it.22 This model may be particularly relevant for media literacy programs because of their potential to reduce the impact of mass media messages on attitudes and normative beliefs.
In addition to focusing the intervention material on media exposures strongly associated with outcomes, media literacy programs tend to be different from traditional social influences programs in terms of “heavy-handedness.” Because traditional social influences programs tend to focus on how to say “no” to smoking, they may be less effective among those more rebellious individuals who tend to defy authority.25 However, media literacy programs try to focus this inherent rebelliousness against corporate influences instead of their own families, friends, and teachers. This may be why media literacy lessons have been not only well-liked by students15,17,26,27 but also associated with prevention of various harmful health behaviors, including alcohol use, obesity, and aggression.14,17,18 Furthermore, as with the more general concept of health literacy, media literacy focuses on individual and social empowerment in decision-making, which are increasingly considered of theoretical and empiric value for improving health outcomes.28,29
Although media literacy programs have also shown potential for prevention of tobacco use among youth,15,17,19,20,26 these studies had methodological limitations, such as quasi-experimental designs and small sample sizes. Whereas the Centers for Disease Control and Prevention30 and other institutions31,32 have called for the use of media literacy to prevent harmful health behaviors such as smoking, more rigorous evaluation is necessary prior to making continued public health investments.
An important “great debate”33 in the field of health-related media literacy relates to how specific media literacy should be regarding the health topic of interest. Although some advocate that health-related media literacy programs should focus on media examples highly specific to the topic (eg, deconstruct only tobacco advertisements within an anti-tobacco program), others focus on the importance of changing a broader concept of media literacy that can be applied to many different types of messages.17,33 Because few programs simultaneously assess their influence on separate constructs of general and topic-specific media literacy, we aimed to explore this important area.14,17
The purpose of this study was to determine if a theory-driven, school-based, 3-session anti-smoking media literacy curriculum delivered to 9th grade students affects students’ media literacy (both general and smoking-specific) and the factors mediating adolescent smoking according to our underlying conceptual model based on the TRA. We hypothesized that, compared with those assigned to the standard tobacco educational program, students in classrooms randomly assigned to the media literacy curriculum would have increased smoking-specific media literacy (Hypothesis 1); increased general media literacy (Hypothesis 2); reduced positive attitudes toward smoking (Hypothesis 3); and reduced positive sense of smoking norms regarding both its popularity (Hypothesis 4a) and elite status (Hypothesis 4b). Our exploratory hypothesis was that exposure to the media literacy curriculum would reduce the intention to smoke among students with initial intention to smoke (Hypothesis 5).
METHODS
We conducted a cluster-randomized trial, with classrooms randomly assigned to either an experimental media-literacy curriculum or a standard educational program about smoking tobacco. This design was required as it was not feasible to allocate individual students to different interventions in the classroom-based setting. There were no important changes to methods or outcomes after trial commencement. The trial was officially registered with www.clinicaltrials.gov before it was begun and was assigned the registration number NCT00398190. A checklist outlining our compliance with CONSORT guidelines is available as Appendix 1.
Participants
We recruited 3 Pittsburgh, PA area high schools with the assistance of community agencies contracted to provide anti-smoking education in Allegheny County. We purposefully selected 3 schools from their complete list of schools to ensure that: our final student pool would be large enough to confer adequate power for analyses; schools had a history of working with community organizations on other research projects; schools were willing to include and randomize all 9th grade health classrooms; and the final pool of students would be at least 25% African-American. The African-American population was specifically targeted because it bears the greatest burden of morbidity and mortality due to smoking,34 and the Surgeon General’s report on tobacco use highlighted mass media messages as a key factor influencing tobacco use among minorities.34
We focused our trial on 9th grade students because their age is an ideal time for intervention (ie, smoking rates increase up to 3-fold between the 8th and 12th grades). Ninth grade students are more cognitively able than younger students to assimilate the theoretical concepts of media literacy that require abstract thought.16,35
During the study period (September 2006 to May 2008), classrooms (clusters) were eligible to participate if they consisted primarily of 9th grade students in 1 of the 3 selected high schools. Students were eligible to participate if they were enrolled in the participating classrooms.
To have 80% power to detect a difference of 15% in smoking-specific media literacy scores (under 2-tailed testing with alpha = 0.05), and taking the variance inflation factor into consideration due to clustering, we estimated needing 429 students in each arm.
Instruments
Media literacy was assessed with 22 items modified from a validated 18-item scale (Appendix 2).36–38 These 22 items were divided into 2 groups representing smoking-specific media literacy (11 items) and general media literacy (11 items), as the prior 18-item smoking media literacy scale combined smoking-specific and general items, which we deemed important to separate theoretically. The pool of items had to be expanded slightly so that items from each subscale represented each of the theoretical divisions of media literacy (“authors and audiences (AA),” “messages and meanings (MM),” and “representation and reality (RR),” Table 1). All media literacy measures were measured with a Likert-type response scale with 4 response categories ranging from “strongly disagree” to “strongly agree.”
Table 1.
Relationships Between the “AD IT UP” Curriculum and a Conceptual Model of Media Literacy
| Media Literacy Domain | Related Media Literacy Core Concepts45 | “AD IT UP” Lesson | “AD IT UP” Key Question | Skill Targets |
|---|---|---|---|---|
| AA: Authors and Audiences | AA1: authors create media messages for profit and/or influence | “Authority” | Who is the Author of this media message, and what is their motive/purpose? | Determine the author and purpose of a media message. |
| AA2: authors target specific audiences | “Direct, Aim, Fire” | Who is this message Directed against? (That is, who is the target audience?) | Determine the target audience of a media message. | |
| MM: Messages and Meanings | MM1: messages contain values and specific points of view | “The Big Idea” | What Ideas are they trying to get across through this message? | Describe ideas and feelings which message authors intend to convey. |
| MM2: different people interpret messages differently | ||||
| MM3: messages affect attitudes and behaviors | “Techniques” | What Techniques do they use to make this message in order to get those ideas across? | Identify specific production techniques used to convey those ideas and feelings. | |
| MM4: multiple production techniques are used | ||||
| RR: Representation and Reality | RR1: messages filter reality | “Speak the Unspoken” | What is Unspoken or omitted from this message? | Identify salient omissions from the media message. |
| RR2: messages omit information | ||||
| Facilitation of movement from altered attitude and norms toward intention and behavior | “Plan Your Escape” | What is your Plan now that you know what you know? Is this something you want to buy/do or not? | Engage in an evaluative process integrating personal perspectives with information from the media message. |
Outcomes of interest were mediators of smoking according to our underlying conceptual model based on the TRA, which included attitudes, normative beliefs, and intentions related to smoking. Smoking attitudes was measured with 9 items from a validated scale39 via agreement or disagreement with statements such as: “Smoking cigarettes is enjoyable,” “Smoking helps you deal with problems or stress,” and “There is no harm in having a cigarette once in a while (reverse-coded).” This study was based on a composite theoretical model which included aspects of the TRA.39 Attitude items used a Likert-type response scale with 4 response categories ranging from “strongly disagree” to “strongly agree.”
Smoking normative beliefs was evaluated with a 2-factor scale based on previous validation founded on the TRA.40 The first construct measured was “perceived success of smokers,” which was measured by agreement or disagreement with 3 different statements such as “Cool people smoke cigarettes more than uncool people.” These items used a Likert-type response scale with 4 response categories ranging from “strongly disagree” to “strongly agree.” The second construct related to normative beliefs was “perceived prevalence,” which included 3 separate items asking participants to estimate smoking prevalence among their peers.
Intention to smoke was assessed with Pierce’s reliable and valid 3-item susceptibility scale, which defines all participants as “susceptible” who do not indicate a firm intention not to smoke in the future.41
Covariates measured the factors previously established as associated with adolescent smoking. Demographics included age, sex, race, and parental education (as a measure of socioeconomic status). Personal and environmental factors included self-report of grades, sensation seeking as measured by a brief, validated scale,42 rebellious behavior as measured by 3 items from Smith and Fogg’s validated scale,43 and 6 items from Jackson’s 2-factor scale assessing parental style.44
Procedure
All 9th graders at participating schools were invited to participate. Parents were sent a note informing them of the project and a procedure for opting-out of consent if they desired. All participating students provided written assent.
A baseline survey was administered by study personnel trained in survey administration. Students were assigned identification numbers, with no names attached to the surveys. The data were collected in computer laboratories of the selected high schools. Within each school, health classrooms were randomized to receive either the experimental media literacy curriculum (a 3-session version of the “AD IT UP” curriculum) or a control educational program (a 3-session standard anti-tobacco curriculum adapted from a commonly used health textbook). To ensure comparability of the intervention and control groups in terms of class time of day and classroom health teachers, we stratified random allocation according to these two variables. Randomization was conducted by a statistician (SRL) not associated with recruitment of classrooms or development or presentation of curricula, and who was blinded to the identity of the intervention and control groups. Allocations were concealed until interventions were assigned.
The experimental curriculum was a 3-session (120 minutes) version of the “AD IT UP” curriculum—a theory-based anti-smoking media literacy curriculum developed and pilot tested with foundation grant funding. This curriculum teaches youth to access, analyze, and evaluate mass media messages involving smoking, such as advertisements, promotions, or film product placements. Each letter of the title refers to one of the 6 lessons contained in the curriculum, which were associated with core concepts from a conceptual model of media literacy and a key question related to media literacy (Table 1).16
The control curriculum was based on the 3-session anti-smoking program (120 minutes) featured in the most widely used health textbook in the region. These 3 lessons, derived from a representative “social influences” program, describe both short- and long-term effects of smoking, support students’ self-efficacy in saying “no” to smoking, and discuss social and psychological issues involving smoking.
The experimental and control curricula were implemented by experienced health educators who were not the students’ regular classroom teachers. This was done to improve implementation fidelity and training procedures, both of which we felt we could standardize more easily with our own staff. They were given appropriate training and practiced implementation on convenience samples of high school students from other (non-study) schools. Each teacher remained with the same cadre of students for each of the 3 sessions to maintain teacher-student rapport and continuity.
We implemented both the intervention and control curricula in a uniform manner. Each of the teachers taught both curricula, and all students were given the same pre- and post-intervention surveys. Each curriculum used a common format, with a slide presentation combined with activities and a 16-page workbook (with different content). The trial was stopped after all respondents completed post-test assessments one week following completion of the curricula, which was an average of 5 weeks following the pre-tests.
Data Analysis
For the intervention and control groups, we computed baseline and follow-up data for all outcome variables. We computed the effect size for all differences over time using Cohen’s d, defined as the mean difference divided by the pooled standard deviation. We used multi-level modeling to account for clustering of individual students within classrooms. Hypotheses 1 through 4 were tested using a change score analysis, with each change score for the outcome of interest as the dependent variable, and the assignment to intervention or control as the independent variable, controlling for covariates. Outcome variables were media literacy, attitudes, and normative beliefs, guided by the TRA. For the exploratory hypothesis, a one-sided Fisher’s exact test was used to determine if intention to smoke at time 2 was associated with group assignment among those who intended to smoke at baseline.
We determined a priori to utilize these multilevel models controlling for age, sex, race, maternal education, grades, parenting style, rebelliousness, and sensation seeking, and accounting for clustering as our primary analyses to be highly conservative with our findings. However, because ultimately we determined that intervention and control participants were no different in terms of any measured covariates, we also conducted simple t-tests comparing differences in intervention and control groups’ change scores. The primary analyses included all participants for whom follow-up data were obtained (“intention to treat” analyses). We tested interactions between basic socio-demographic data (ie, age, sex, and race) and outcomes, to determine whether any of these subgroups particularly drove score changes.
Because analyses focused on change scores, those who did not have complete data from both time points were not included in analyses; no imputation of data was used.
Implementation fidelity was assessed by each instructor using Likert-type items immediately after classroom sessions. Student satisfaction with and impressions of the intervention were also obtained at follow-up.
RESULTS
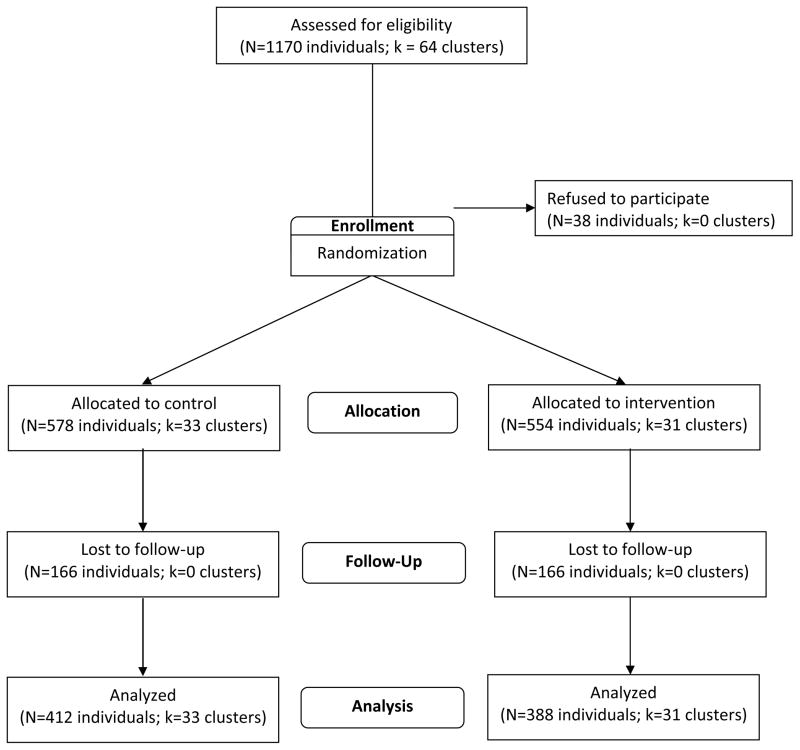
Of the 1170 potentially eligible students representing 64 classrooms, 578 (49.4%) students from 33 classrooms were randomized to the control educational program and 554 (47.4%) students from 31 classrooms were randomized to the intervention curriculum (Figure 1). Overall, 412 (71%) of the 578 students assigned to the control arm, and 388 (70%) of the 554 students assigned to the intervention arm completed the post-test assessment and were analyzed in the primary intention-to-treat analyses.
Figure 1.
Cluster-Randomized Trial Flow Diagram.
The study population was comprised of 51% boys and 50% African Americans, and had a mean age of 14.5 years (Table 2). There were no significant differences between the intervention and control groups in terms of any measured covariate (Table 2).
Table 2.
Comparison of Baseline Student Characteristics in the Intervention and Control Arms.
| Intervention N = 386 | Control N = 410 | p-value | |
|---|---|---|---|
|
| |||
| Age | 0.13 | ||
| ≤15 | 58% | 52% | |
| >15 | 42% | 48% | |
|
| |||
| Sex | 0.90 | ||
| Boys | 51% | 51% | |
| Girls | 49% | 49% | |
|
| |||
| Race | |||
| White | 43% | 45% | 0.46 |
| Black | 52% | 48% | 0.26 |
| Other | 16% | 14% | 0.45 |
|
| |||
| Maternal Education | 0.46 | ||
| Did not graduate high school | 24% | 25% | |
| Graduated from high school but not college | 35% | 31% | |
| College degree or higher | 41% | 44% | |
|
| |||
| Grades | 0.74 | ||
| A’s and B’s | 56% | 57% | |
| Lower than B’s | 44% | 43% | |
|
| |||
| Demanding Parenting | 0.64 | ||
| Lowest tertile | 54% | 51% | |
| Middle tertile | 16% | 16 % | |
| Highest tertile | 30% | 33% | |
|
| |||
| Responsive Parenting | 0.17 | ||
| Lowest tertile | 38% | 43% | |
| Middle tertile | 42% | 36% | |
| Highest tertile | 20% | 22% | |
|
| |||
| Sensation Seeking | 0.17 | ||
| Lowest tertile | 46% | 40% | |
| Middle tertile | 35% | 36% | |
| Highest tertile | 20% | 24% | |
|
| |||
| Rebelliousness | 0.57 | ||
| Lowest tertile | 49% | 49% | |
| Middle tertile | 21% | 18% | |
| Highest tertile | 30% | 33% | |
|
| |||
| Current Smoker | 0.30 | ||
| Yes | 6% | 5% | |
| No | 94% | 95% | |
|
| |||
| Parental Smoking | 0.62 | ||
| Yes | 60% | 59% | |
| No | 40% | 41% | |
|
| |||
| Friend Smoking | 0.53 | ||
| None | 54% | 53% | |
| Some | 36% | 39% | |
| Most or All | 10% | 8% | |
Internal consistency reliability was adequate for all scales at baseline and follow-up. At baseline, Cronbach’s alpha was 0.76, 0.83, 0.84, 0.69, and 0.75 for general media literacy, smoking media literacy, attitudes, perceived success of smokers, and perceived prevalence of smoking, respectively. At follow-up, Cronbach’s alpha values were 0.88, 0.87, 0.84, 0.71, and 0.81, respectively.
Smoking media literacy increased more among students in the intervention arm compared to those in the control arm (0.24 vs. 0.08, p < .001). Increases were present and statistically significant for SML subscales 1 and 2 (AA and MM), but not for subscale 3 (RR). The changes in general media literacy by intervention arm exhibited a similar pattern, although levels of significance were smaller in magnitude. There were no significant differences between intervention arms in change scores for cigarette attitudes and perceived success of smokers (Table 3). Compared with students in the control arm, students in the intervention arm exhibited a significantly greater reduction in the perceived prevalence of smoking (−14.0% vs. −4.6%, p < .001).
Table 3.
Comparison of Post-Intervention Impressions in Intervention and Control Arms.
| Post-Intervention Perception* | Intervention (N = 410) | Control (N = 386) | Cohen’s d | p-value |
|---|---|---|---|---|
| The instructor was knowledgeable | 2.23 | 2.23 | 0.00 | .94 |
| I learned a lot during this program | 2.21 | 2.11 | 0.13 | .08 |
| I enjoyed this program | 2.05 | 1.91 | 0.18 | .01 |
| I would like more programs like this one | 1.95 | 1.85 | 0.13 | .08 |
| I would recommend this program to a friend | 1.92 | 1.86 | 0.07 | .26 |
| I participated in this program | 1.94 | 1.83 | 0.14 | .06 |
| This program kept my attention | 2.01 | 1.78 | 0.29 | <.001 |
| I am less likely to smoke now that I have seen this program | 2.17 | 2.05 | 0.14 | .06 |
| This program would be effective in getting kids not to smoke | 2.00 | 1.88 | 0.14 | .04 |
| I will look at smoking differently from now on | 2.07 | 1.87 | 0.23 | .001 |
| I will look at advertising differently from now on | 2.09 | 1.86 | 0.26 | <.001 |
Post-intervention perceptions were scored with continuous figures from 0 (strongly disagree) to 3 (strongly agree).
Multivariable analyses, which controlled for clustering of students within classrooms and all covariates, demonstrated similar levels of significance compared with basic t-tests, except for overall improved general media literacy (Table 3). In summary, conservatively relying on the more complex analyses, these results upheld Hypothesis 1 and Hypothesis 4a, but not Hypotheses 2, 3, and 4b.
Among the 236 students who intended to smoke at baseline (121 in the intervention and 115 in the control arm), a larger proportion of intervention than control students changed to being non-susceptible to smoking at follow-up (24% vs. 16%, p = .08).
There were no significant interactions between basic socio-demographic data (ie, age, sex, and race) and outcomes, suggesting that none of these subgroups particularly drove score changes.
Implementation fidelity was self-reported by instructors at >90%. Regardless of program assignment, students were equally likely to agree with statements such as “the instructor was knowledgeable” and “I learned a lot during this program.” However, compared with those assigned to the control condition, students assigned to the intervention had higher rating scores for “I enjoyed this program,” “This program kept my attention,” “I will look at smoking differently from now on,” and “I will look at advertising differently from now on” (Table 3).
DISCUSSION
This study found that students exposed to a media-literacy-based anti-smoking program had significantly improved smoking media literacy and improved perceptions of the true prevalence of smoking compared to youth exposed to a standard school-based social influences anti-smoking program. However, assignment to the intervention was not associated with significant improvements in general media literacy, anti-tobacco attitudes, or assessment of perceived status of smokers. Finally, although a greater proportion of those who intended to smoke at baseline reverted to no intention in the intervention compared with the control, this difference was not statistically significant.
These findings are consistent with others that demonstrated potential benefits for media literacy education as it may apply to substance use.15,17,19,20,26 This study extends prior findings by utilizing a more rigorous experimental design. Additionally, this study uses a well-studied measure of media literacy. Whereas no measure of this complex, multi-faceted construct is perfect, it is heartening that intervention assignment was associated with meaningful effect size changes in the measure.
Assignment to the intervention, which focused on smoking-specific media literacy, was associated with higher differences in smoking-specific media literacy versus general media literacy. Improvements in general media literacy did not have the same magnitude of change, and in complex models that controlled for clustering, the difference was short of reaching statistical significance. This overall pattern is consistent with prior work of others who have found that it may be easier to transfer subject-specific compared with general media literacy concepts.14,15
Exposure to the intervention was not associated with significant differences in smoking-related attitudes. This is not surprising because the control curriculum strongly emphasizes anti-smoking attitudes such as those represented in our measure (eg, that smoking is not attractive, not pleasant, not relaxing). Consistent with what would be expected both the intervention and the control curriculum were associated with moderate changes in attitudes (Table 3).
However, it still may be valuable to consider broadening the TRA (Figure 1) as an underlying model. For example, the Message Interpretation Process Model14,15 suggests that behavior choices are influenced not only by logical processes emphasized by the TRA but also by emotional components such as desirability of, personal relevance to, and identification with portrayals. Thus, it is possible that, although traditional interventions may instill certain negative attitudes, media literacy programs may more subtly affect message interpretation which may be more affect-laden and associated with downstream behavioral changes. Similarly, the TRA does not emphasize the concept of empowerment in decision-making, which is hypothesized to link health literacy to health outcomes.28,29 Thus, it will be valuable to assess a more complete set of theoretical constructs in future studies.
Perceived prevalence of smoking is related to smoking behavior; when youth overestimate the proportion of their peers who smoke, they are more likely to smoke themselves.40 In this study, youth assigned to the media literacy intervention showed a greater decrease in perceived prevalence of smoking. Whereas the intervention was not designed for this, and “on paper” the control condition seemed to emphasize the actual prevalence of smoking even more than the media literacy intervention, it may be that the media literacy intervention actually decreased perceived prevalence more by calling into question the reality of the many smoking-related media messages in the environment.
Although our primary purpose was to determine if the intervention taught media literacy as was expected, we also explored whether there were associations between intervention exposure and intention to smoke (Aim 5). A clinically relevant question is how intentions changed among the highest-risk group who began the intervention intending to smoke. There was a meaningful difference in the proportion of participants initially intending to smoke who reverted to non-intending after the intervention vs. the control condition (24% vs. 16%). This study was not powered to detect this more exploratory outcome, and thus, this difference was not statistically significant (p = .08). These preliminary results, which suggest that such media-literacy interventions may be particularly salient for youth initially intending to smoke, should be more deeply explored in future studies. Others have suggested that media literacy may be more effective than standard tobacco education in the populations that are at greatest risk for smoking, such as rebellious and socio-economically disadvantaged youth.30,34
Whereas the intervention was associated with increases in media literacy outcomes, these increases were associated with 2 of the subscales, “authors and audiences” and “messages and meanings,” but not with “representation and reality.” It is unclear as to why this was the case, because the intervention sought to emphasize the difference between representation and reality. One possibility is that, by vilifying tobacco and smoking in general, the control curriculum engendered increased understanding of the stark differences between the way tobacco is often represented in mainstream media and its true effects.
It would be valuable for future research to explore different methods of curriculum implementation. Although regular classroom teachers could be trained in conducting these curricula, it would introduce challenges with regard to standardizing training and implementation fidelity. An interactive Web-based approach may optimize curriculum standardization, but this approach may reduce in-person teacher-student interactions and spontaneity.
Limitations
This study involved 3 urban public schools in the same region of the US; thus, the results may not generalize to other parts of the country. Similarly, because of selection bias, even within this community, respondents may have been different from non-respondents in ways we were not able to assess.
In addition, it is difficult to control for contamination in a study that used the same instructors for both the intervention and the control curriculum. By conducting the study in this way we biased our results toward the null hypothesis, which we considered more conservative and preferable. Although we had limited information about non-respondents, demographic data were not different between assignment groups, and thus, were not likely to have driven results.
The study also had limited statistical power. Although we estimated that 429 participants were necessary in each arm to detect differences in our primary outcome, our final groups included 386 and 410 individuals, respectively. Whereas there were statistically significant differences in the primary outcome, results for other outcomes (eg, general media literacy, intention to smoke) were extremely close and may have achieved significance if we had been able to retain sufficient numbers.
It is also important to note that we selected a relatively aggressive control intervention. Because of the newness of media literacy, it may have been more appropriate to utilize a less robust (eg, “attention-type”) control. However, we used an established and involved control curriculum to keep our conclusions about the potential efficacy of media literacy conservative.
Conclusions
This study breaks important ground in demonstrating that smoking-related media literacy can be taught via school-based interventions and is acceptable to students. Whereas it suggests that media literacy may be associated with important clinically relevant outcomes, such as influencing intention to smoke among high risk individuals, further study with more complex theoretical models and greater statistical power is needed.
IMPLICATIONS FOR SCHOOL HEALTH.
Although tobacco smoking remains a leading cause of preventable US morbidity and mortality, currently accepted school-based prevention programs are not associated with clinically meaningful long-term outcomes. This study suggests that media literacy programs aimed at preventing cigarette smoking present an alternative to standard programs. Furthermore, these programs are feasible to implement in the school-based setting in health classrooms, and they seem to be acceptable to students. However, although assignment to the media literacy group in this study was associated with improvements in certain mediators of smoking, further investigation will be necessary to determine if media literacy education is associated with longer-term behavior outcomes such as experimentation with smoking.
Acknowledgments
Dr. Primack was supported in part by a grant from the Maurice Falk Foundation, a Physician Faculty Scholar Award from the Robert Wood Johnson Foundation, and a career development award from the National Cancer Institute (K07-CA114315). The funders had no role in conduct of the study or writing or approval of this manuscript. We wish to thank our high school partners for their participation in this study.
Appendix 1. CONSORT 2010 checklist of information to include when reporting a randomised trial*
| Section/Topic | Item No | Checklist item | Reported on page No |
|---|---|---|---|
| Title and abstract | |||
| 1a | Identification as a randomised trial in the title | 1
|
|
| 1b | Structured summary of trial design, methods, results, and conclusions (for specific guidance see CONSORT for abstracts) | 2–3
|
|
| Introduction | |||
| Background and objectives | 2a | Scientific background and explanation of rationale | 4–7
|
| 2b | Specific objectives or hypotheses | 7
|
|
| Methods | |||
| Trial design | 3a | Description of trial design (such as parallel, factorial) including allocation ratio | 8
|
| 3b | Important changes to methods after trial commencement (such as eligibility criteria), with reasons | 8
|
|
| Participants | 4a | Eligibility criteria for participants | 8–9
|
| 4b | Settings and locations where the data were collected | 8–9
|
|
| Interventions | 5 | The interventions for each group with sufficient details to allow replication, including how and when they were actually administered | 10–14
|
| Outcomes | 6a | Completely defined pre-specified primary and secondary outcome measures, including how and when they were assessed | 10–11
|
| 6b | Any changes to trial outcomes after the trial commenced, with reasons | 8
|
|
| Sample size | 7a | How sample size was determined | 9
|
| 7b | When applicable, explanation of any interim analyses and stopping guidelines | NA
|
|
| Randomisation: | |||
| Sequence generation | 8a | Method used to generate the random allocation sequence | 12
|
| 8b | Type of randomisation; details of any restriction (such as blocking and block size) | 12
|
|
| Allocation concealment mechanism | 9 | Mechanism used to implement the random allocation sequence (such as sequentially numbered containers), describing any steps taken to conceal the sequence until interventions were assigned | 12–13
|
| Implementation Blinding | 10 | Who generated the random allocation sequence, who enrolled participants, and who assigned participants to interventions | 12
|
| 11a | If done, who was blinded after assignment to interventions (for example, participants, care providers, those assessing outcomes) and how | 12
|
|
| 11b | If relevant, description of the similarity of interventions | 13–14 | |
| Statistical methods | 12a | Statistical methods used to compare groups for primary and secondary outcomes | 14–15
|
| 12b | Methods for additional analyses, such as subgroup analyses and adjusted analyses | 15
|
|
| Results | |||
| Participant flow (a diagram is strongly recommended) | 13a | For each group, the numbers of participants who were randomly assigned, received intended treatment, and were analysed for the primary outcome |
Figure 1
|
| 13b | For each group, losses and exclusions after randomisation, together with reasons |
Figure 1
|
|
| Recruitment | 14a | Dates defining the periods of recruitment and follow-up | 9
|
| 14b | Why the trial ended or was stopped | 14
|
|
| Baseline data | 15 | A table showing baseline demographic and clinical characteristics for each group |
Table 2
|
| Numbers analysed | 16 | For each group, number of participants (denominator) included in each analysis and whether the analysis was by original assigned groups | 14–15
|
| Outcomes and estimation | 17a | For each primary and secondary outcome, results for each group, and the estimated effect size and its precision (such as 95% confidence interval) |
Tables 3–4
|
| 17b | For binary outcomes, presentation of both absolute and relative effect sizes is recommended | NA
|
|
| Ancillary analyses | 18 | Results of any other analyses performed, including subgroup analyses and adjusted analyses, distinguishing pre-specified from exploratory | 17–19
|
| Harms | 19 | All important harms or unintended effects in each group (for specific guidance see CONSORT for harms) | NA
|
| Discussion | |||
| Limitations | 20 | Trial limitations, addressing sources of potential bias, imprecision, and, if relevant, multiplicity of analyses | 24–25
|
| Generalisability | 21 | Generalisability (external validity, applicability) of the trial findings | 24
|
| Interpretation | 22 | Interpretation consistent with results, balancing benefits and harms, and considering other relevant evidence | 20–24
|
| Other information | |||
| Registration | 23 | Registration number and name of trial registry | 8
|
| Protocol | 24 | Where the full trial protocol can be accessed, if available | NA
|
| Funding | 25 | Sources of funding and other support (such as supply of drugs), role of funders | 27
|
Table 4.
Comparison of Outcomes in the Intervention and Control Arms
| Outcome | Intervention (N = 410) | Control (N = 386) | p-Value* | p-Value† | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| T1 | T2 | δ‡ | d§ | T1 | T2 | δ‡ | d§ | |||
| Total Smoking Media Literacy (SML)|| | 1.84 | 2.08 | 0.24 | 0.46 | 1.87 | 1.95 | 0.08 | 0.16 | <.001 | .001 |
| SML Subscale 1 | 2.04 | 2.29 | 0.25 | 0.35 | 2.10 | 2.10 | 0.00 | 0.01 | <.001 | .001 |
| SML Subscale 2 | 1.70 | 1.97 | 0.27 | 0.52 | 1.72 | 1.83 | 0.11 | 0.21 | <.001 | <.001 |
| SML Subscale 3 | 2.00 | 2.15 | 0.15 | 0.24 | 2.03 | 2.10 | 0.07 | 0.10 | .16 | .26 |
|
| ||||||||||
| Total General Media Literacy (ML)|| | 2.04 | 2.12 | 0.08 | 0.16 | 2.09 | 2.07 | −0.02 | 0.04 | .01 | .06 |
| ML Subscale 1 | 1.87 | 2.04 | 0.17 | 0.24 | 1.93 | 1.93 | 0.00 | 0.01 | .002 | .01 |
| ML Subscale 2 | 2.08 | 2.14 | 0.06 | 0.10 | 2.15 | 2.11 | −0.04 | 0.08 | .03 | .12 |
| ML Subscale 3 | 2.06 | 2.14 | 0.08 | 0.12 | 2.10 | 2.11 | 0.01 | 0.01 | .19 | .34 |
|
| ||||||||||
| Total Cigarette Attitudes|| | 0.58 | 0.80 | 0.22 | 0.41 | 0.58 | 0.78 | 0.20 | 0.38 | .70 | .69 |
|
| ||||||||||
| Total perceived success of smokers|| | 0.92 | 0.96 | 0.04 | 0.05 | 0.87 | 0.93 | 0.06 | 0.08 | .61 | .82 |
|
| ||||||||||
| Total perceived prevalence (%) | 64.0 | 50.0 | −14.0 | 0.76 | 63.1 | 58.5 | −4.60 | 0.25 | <.001 | <.001 |
t-tests comparing differences between intervention and control outcomes.
Controlling for clustering and age, gender, race, maternal education, grades, parenting style, sensation seeking, and rebelliousness.
Differences between follow-up and baseline.
Cohen’s d, a measure of effect size.
Media literacy (smoking-specific and general, as well as all subscales), attitudes, and the first normative beliefs scale (“perceived success of smokers”) were scaled to continuous figures with a minimum of 0 and a maximum of 3.
The second normative beliefs scale (“perceived prevalence”) utilized figures between 0 and 100 representing the average perceived prevalence for smoking.
Appendix 2. Media Literacy Items
| Media Literacy Domain | Smoking-Specific Media Literacy Item | General Media Literacy Item |
|---|---|---|
| AA: Authors and Audiences |
|
|
| MM: Messages and Meanings |
|
|
| RR: Representation and Reality |
|
|
Footnotes
We strongly recommend reading this statement in conjunction with the CONSORT 2010 Explanation and Elaboration for important clarifications on all the items. If relevant, we also recommend reading CONSORT extensions for cluster randomised trials, non-inferiority and equivalence trials, non-pharmacological treatments, herbal interventions, and pragmatic trials. Additional extensions are forthcoming: for those and for up to date references relevant to this checklist, see www.consort-statement.org.
Human Subjects Approval Statement
IRB approval was obtained from the University of Pittsburgh (IRB #0606146) and all required school administrators.
Contributor Information
Brian A. Primack, Email: bprimack@pitt.edu, Division of General Internal Medicine, Department of Medicine, University of Pittsburgh School of Medicine, 230 McKee Place Suite 600, Pittsburgh, PA 15213, Phone: (412) 586-9789.
Erika L. Douglas, Email: douglasel@upmc.edu, University of Pittsburgh Medical Center, USS Tower, 57-W90, 600 Grant Street; Pittsburgh, PA 15219, Phone: (412) 647-7617.
Stephanie R. Land, Email: stephanie.land@nih.gov, National Cancer Institute, National Institutes of Health, 6130 Executive Blvd., MSC 7337, Bethesda, MD 20892-7337, Phone: (301) 496-0277
Elizabeth Miller, Email: elizabeth.miller@chp.edu, Division of Adolescent Medicine, Department of Pediatrics, University of Pittsburgh School of Medicine, Pittsburgh, PA, 3420 Fifth Avenue, Pittsburgh, PA 15213, Phone: (412) 692-8504
Michael J. Fine, Email: finemj@upmc.edu, VA Center for Health Equity Research and Promotion, VA Pittsburgh Healthcare System (646), 7180 Highland Drive (151C-H), Pittsburgh, PA 15206, Phone: (412) 954-5206.
References
- 1.Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses--United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Cigarette smoking among adults: United States, 2004. MMWR Morb Mortal Wkly Rep. 2005;54(44):1121–1147. [PubMed] [Google Scholar]
- 3.Wiehe SE, Garrison MM, Christakis DA, Ebel BE, Rivara FP. A systematic review of school-based smoking prevention trials with long-term follow-up. J Adolesc Health. 2005;36(3):162–169. doi: 10.1016/j.jadohealth.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Peterson AV, Jr, Kealey KA, Mann SL, Marek PM, Sarason IG. Hutchinson Smoking Prevention Project: long-term randomized trial in school-based tobacco use prevention--results on smoking. J Natl Cancer Inst. 2000;92(24):1979–1991. doi: 10.1093/jnci/92.24.1979. [DOI] [PubMed] [Google Scholar]
- 5.Rideout V, Foehr U, Roberts D. Generation M2: Media in the Lives of 8–18 Year-olds. Menlo Park, CA: Kaiser Family Foundation; 2010. [Google Scholar]
- 6.Long JA, O’Connor PG, Gerbner G, Concato J. Use of alcohol, illicit drugs, and tobacco among characters on prime-time television. Subst Abus. 2002;23(2):95–103. doi: 10.1080/08897070209511479. [DOI] [PubMed] [Google Scholar]
- 7.Thompson KM, Yokota F. Depiction of alcohol, tobacco, and other substances in G-rated animated feature films. Pediatrics. 2001;107(6):1369–1374. doi: 10.1542/peds.107.6.1369. [DOI] [PubMed] [Google Scholar]
- 8.Primack BA, Longacre MR, Beach ML, Adachi-Mejia AM, Titus LJ, Dalton MA. Association of established smoking among adolescents with timing of exposure to smoking depicted in movies. J Natl Cancer Inst. 2012;104(7):549–555. doi: 10.1093/jnci/djs138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dal Cin S, Stoolmiller M, Sargent JD. When movies matter: exposure to smoking in movies and changes in smoking behavior. J Health Commun. 2012;17(1):76–89. doi: 10.1080/10810730.2011.585697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Smoking in top-grossing movies--United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(27):910–913. [PubMed] [Google Scholar]
- 11.Dalton MA, Sargent JD, Beach ML, Titus-Ernstoff L, Gibson JJ, Ahrens MB, et al. Effect of viewing smoking in movies on adolescent smoking initiation: a cohort study. Lancet. 2003;362(9380):281–285. doi: 10.1016/S0140-6736(03)13970-0. [DOI] [PubMed] [Google Scholar]
- 12.Titus-Ernstoff L, Dalton MA, Adachi-Mejia AM, Longacre MR, Beach ML. Longitudinal study of viewing smoking in movies and initiation of smoking by children. Pediatrics. 2008;121(1):15–21. doi: 10.1542/peds.2007-0051. [DOI] [PubMed] [Google Scholar]
- 13.Lovato C, Watts A, Stead LF. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database Syst Rev. 2011;(10):CD003439. doi: 10.1002/14651858.CD003439.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Austin EW, Johnson KK. Effects of general and alcohol-specific media literacy training on children’s decision making about alcohol. J Health Commun. 1997;2(1):17–42. doi: 10.1080/108107397127897. [DOI] [PubMed] [Google Scholar]
- 15.Austin EW, Pinkleton BE, Hust SJT, Cohen M. Evaluation of an American Legacy Foundation/Washington State Department of Health media literacy pilot study. Health Commun. 2005;18(1):75–95. doi: 10.1207/s15327027hc1801_4. [DOI] [PubMed] [Google Scholar]
- 16.National Association for Media Literacy Education. [Accessed on October 17, 2012.];Core Principles of Media Literacy Education in the United States. Available at: http://namle.net/wp-content/uploads/2009/09/NAMLE-CPMLE-w-questions2.pdf.
- 17.Bergsma LJ, Carney ME. Effectiveness of health-promoting media literacy education: a systematic review. Health Educ Res. 2008;23(3):522–542. doi: 10.1093/her/cym084. [DOI] [PubMed] [Google Scholar]
- 18.Hobbs R. A review of school-based initiatives in media literacy education. Am Behav Sci. 2004;48(1):42–59. [Google Scholar]
- 19.Kupersmidt JB, Scull TM, Austin EW. Media literacy education for elementary school substance use prevention: study of media detective. Pediatrics. 2010;126(3):525–531. doi: 10.1542/peds.2010-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinkleton BE, Weintraub Austin E, Cohen M, Miller A, Fitzgerald E. A statewide evaluation of the effectiveness of media literacy training to prevent tobacco use among adolescents. Health Commun. 2007;21(1):23–34. doi: 10.1080/10410230701283306. [DOI] [PubMed] [Google Scholar]
- 21.Salgado MV, Perez-Stable EJ, Primack BA, Kaplan CP, Mejia RM, Gregorich SE, et al. Association of media literacy with cigarette smoking among youth in Jujuy, Argentina. Nicotine Tob Res. 2012;14(5):516–521. doi: 10.1093/ntr/ntr240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azjen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- 23.Unger JB, Rohrbach LA, Howard-Pitney B, Ritt-Olson A, Mouttapa M. Peer influences and susceptibility to smoking among California adolescents. Subst Use Misuse. 2001;36(5):551–571. doi: 10.1081/ja-100103560. [DOI] [PubMed] [Google Scholar]
- 24.Faucher MA, Carter S. Why girls smoke: a proposed community-based prevention program. JOGNN. 2001;30(5):463–471. doi: 10.1111/j.1552-6909.2001.tb01565.x. [DOI] [PubMed] [Google Scholar]
- 25.Burt RD, Dinh KT, Peterson AV, Jr, Sarason IG. Predicting adolescent smoking: a prospective study of personality variables. Prev Med. 2000;30(2):115–125. doi: 10.1006/pmed.1999.0605. [DOI] [PubMed] [Google Scholar]
- 26.Primack BA, Fine D, Yang CK, Wickett D, Zickmund S. Adolescents’ impressions of antismoking media literacy education: qualitative results from a randomized controlled trial. Health Educ Res. 2009;24(4):608–621. doi: 10.1093/her/cyn062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rich M. Health literacy via media literacy: video intervention/prevention assessment. Am Behav Sci. 2004;48(2):165–188. [Google Scholar]
- 28.Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16(Suppl 3):30–54. doi: 10.1080/10810730.2011.604391. [DOI] [PubMed] [Google Scholar]
- 29.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention (CDC) MediaSharp: Analyzing Tobacco and Alcohol Messages. Atlanta, GA: CDC; 1999. [Google Scholar]
- 31.American Academy of Pediatrics Committee on Public Education. Media education. Pediatrics. 1999;104 (2 Pt 1):341–343. [PubMed] [Google Scholar]
- 32.Office of National Drug Control Policy. Helping Youth Navigate the Media Age: A New Approach to Drug Prevention. Washington, DC: Office of National Drug Control Policy; 2001. [Google Scholar]
- 33.Hobbs R. The seven great debates in the media literacy movement. J Commun. 1998;48(1):16–32. [Google Scholar]
- 34.US Department of Health and Human Services (USDHHS) Tobacco Use among US Racial/Ethnic Minority Groups — African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General. Atlanta, GA: USDHHS; 1998. [PubMed] [Google Scholar]
- 35.Keating D. Adolescent thinking. In: Adelson J, editor. Handbook of Adolescent Psychology. New York, NY: Wiley; 1979. pp. 211–246. [Google Scholar]
- 36.Primack BA, Hobbs R. Association of various components of media literacy and adolescent smoking. Am J Health Behav. 2009;33(2):192–201. doi: 10.5993/ajhb.33.2.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Primack BA, Gold MA, Switzer GE, Hobbs R, Land SR, Fine MJ. Development and validation of a smoking media literacy scale for adolescents. Arch Ped Adol Med. 2006;160(4):369–374. doi: 10.1001/archpedi.160.4.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Primack BA, Gold MA, Land SR, Fine MJ. Association of cigarette smoking and media literacy about smoking among adolescents. J Adolesc Health. 2006;39(4):465–472. doi: 10.1016/j.jadohealth.2006.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Buller DB, Borland R, Woodall WG, Hall JR, Burris-Woodall P, Voeks JH. Understanding factors that influence smoking uptake. Tob Control. 2003;12(Suppl 4):IV16–IV25. doi: 10.1136/tc.12.suppl_4.iv16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Primack BA, Switzer GE, Dalton MA. Improving measurement of normative beliefs involving smoking among adolescents. Arch Ped Adol Med. 2007;161(5):434–439. doi: 10.1001/archpedi.161.5.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Berry CC. Tobacco industry promotion of cigarettes and adolescent smoking. JAMA. 1998;279(7):511–515. doi: 10.1001/jama.279.7.511. [DOI] [PubMed] [Google Scholar]
- 42.Stephenson MT, Hoyle RH, Palmgreen P, Slater MD. Brief measures of sensation seeking for screening and large-scale surveys. Drug Alcohol Depend. 2003;72(3):279–286. doi: 10.1016/j.drugalcdep.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 43.Smith GM, Fogg CP. Psychological antecedents of teenage drug use. In: Simmons R, editor. Research in Community and Mental Health: An Annual Compilation of Research. Greenwich, CT: JAI; 1979. pp. 87–102. [Google Scholar]
- 44.Jackson C, Henriksen L, Foshee V. The Authoritative Parenting Index: predicting health risk behaviors among children and adolescents. Health Educ Behav. 1998;25(3):319–337. doi: 10.1177/109019819802500307. [DOI] [PubMed] [Google Scholar]
- 45.Bazalgette C. Key aspects of media education. In: Alvarado M, Boyd-Barrett O, editors. Media Education: An Introduction. London, England: British Film Institute; 1992. pp. 198–219. [Google Scholar]