Abstract
The suitability and effectiveness of whole body vibration (WBV) exercise in rehabilitation after injury of the anterior cruciate ligament (ACL) was studied using a specially designed WBV protocol. We wanted to test the hypothesis if WBV leads to superior short term results regarding neuromuscular performance (strength and coordination) and would be less time consuming than a current standard muscle strengthening protocol. In this prospective randomized controlled clinical trial, forty patients who tore their ACL and underwent subsequent ligament reconstruction were enrolled. Patients were randomized to the whole body vibration (n=20) or standard rehabilitation exercise protocol (n=20). Both protocols started in the 2nd week after surgery. Isometric and isokinetic strength measurements, clinical assessment, Lysholm score, neuromuscular performance were conducted weeks 2, 5, 8 and 11 after surgery. Time spent for rehabilitation exercise was reduced to less than a half in the WBV group. There were no statistically significant differences in terms of clinical assessment, Lysholm score, isokinetic and isometric strength. The WBV group displayed significant better results in the stability test. In conclusion, preliminary data indicate that our whole body vibration muscle exercise protocol seems to be a good alternative to a standard exercise program in ACL-rehabilitation. Despite of its significant reduced time requirement it is at least equally effective compared to a standard rehabilitation protocol.
Key points.
In this prospective randomized controlled clinical trial, we tested the hypothesis if WBV leads to superior short term results regarding neuromuscular performance (strength and coordination) and would be less time consuming than a current standard muscle strengthening protocol in forty patients who underwent ACL reconstruction.
Time spent for rehabilitation exercise was reduced to less than a half in the WBV group as compared to the standard exercise group. Both protocols showed no differences regarding clinical assessment, Lysholm score, isokinetic and isometric strength.
Despite a more than 50% reduction in time spent for exercise sessions, the WBV group achieved significant better results in the stability test.
In conclusion, the presented WBV program can be considered as a practical alternative to a standard exercise program during ACL-rehabilitation.
Key words: Knee injury, anterior cruciate ligament, rehabilitation, exercise protocol, neuromuscular performance
Introduction
Anterior cruciate ligament (ACL) ruptures are the knee’s most commonly diagnosed sports injuries (Beynnon et al., 2005a; Majewski et al., 2006). The recommendation of reconstructing the torn ACL using a graft has been established due to the fact that over time, non-treatment of complete ligament injuries seems likely to cause progression of symptomatic instability leading to recurrent injury, damage to the menisci and the articular cartilage as well as activating osteoarthrosis (Delay et al., 2001; Frank and Jackson, 1997; Lohmander et al., 2007). Following reconstruction, the stage of rehabilitation – particularly functional muscle strength training – is of upmost importance (Bosco et al., 1998; Frobell et al., 2010; Shelbourne and Gray, 1997; Shelbourne and Davis, 1999; Wright et al., 2008a; 2008b). The main goal of the rehabilitation process is to support and protect the graft during the postoperative remodeling phase along with simultaneously strengthening the muscles to allow recovery of joint stability and coordination as quickly as possible. Current trends in rehabilitation after ACL reconstruction suggest aggressive or accelerated exercise protocols, which allow immediate full weight bearing with return to high levels of athletic activity (running, cutting, twisting, turning) as early as 3 to 4 months after surgery (Beynnon et al., 2005b; Shelbourne and Gray, 1997; Shelbourne and Davis, 1999; Wright et al., 2008b). To minimize reinjury, it is not only important to regain the measurable strength of the knee stabilizing muscles but also to improve neuromuscular control (Hübscher et al., 2010; Hewett et al., 2006; Risberg and Holm, 2009; Zech et al., 2009). In particular, the ability to activate the hamstring group can offer protection to the ACL-graft (Beynnon et al., 2005b; 2005c; Hooper et al., 2001; Kruse et al., 2012).
Despite enhanced surgical techniques and exhausting rehabilitation, which requires a huge amount of exercise and time, a return to full-range of motion in the knee joint and its former strength capability cannot be guaranteed. Even performance athletes, who are highly motivated and provide an excellent initial condition for recovery of muscle strength and coordination, cannot avoid the high risk of re-injury, which is reported in up to 18% of the operated patients (Kvist, 2004). Therefore, the demand for a rehabilitation program with alternative and even more effective muscle strength and coordination exercise seems to be justified.
The use of vibration training, especially whole body vibration (WBV) in combination with conventional resistance, is an attempt to increase neuromuscular performance and enhance muscle strength and power (Berschin and Sommer, 2010; Beynnon et al., 2005a; Cardinale and Wakeling, 2005; Delecluse et al., 2003; De Ruiter et al., 2003; Issurin and Tennebaum, 1999; Luo et al., 2005; Torvinen et al., 2002). Moreover, WBV is capable of enhancing muscle performance even in well-trained athletes without being extremely time-consuming (Cardinale and Wakeling, 2005). Unfortunately, randomized controlled trials dealing with the impact of WBV therapy on neuromuscular control after ACL reconstruction are scarce (Fu et al., 2013; Moezy et al., 2008; Wright et al., 2008b). WBV therapy protocols as well as vibration device types are differing, and there is still discussion regarding the time span until the start of the rehabilitation protocol after surgery, duration of the program or the exercise intensity. Besides, there is currently no clear consensus on the mechanism how WBV increases neuromuscular performance (De Gail et al., 1996; Rittweger, 2010). Some argue that, because positive effects can be seen within a short time of exercise and that greater strength and power gain appeared in elite athletes, these effects must be the result of improved intramuscular control rather than muscle mass growth.
Based on this knowledge, the objective of this study was to investigate the suitability and effectiveness of WBV exercise in ACL rehabilitation using a specially designed protocol compared to a standard muscle exercise protocol. The latter was almost equivalent to standard accelerated rehabilitation protocols (Wright et al. 2008b). Thus, we tested the hypothesis if the use of our WBV exercise protocol attains better neuromuscular performance (strength and coordination) and would be less time consuming than a current standard muscle exercise in ACL rehabilitation (primary outcome) in the short term.
Methods
Subjects
From a total of 60 consecutive patients who were operated on an ACL injury in the University Hospital of Marburg, Germany, 40 subjects participated in this open, prospective, randomized controlled study. Demographic and clinical data of the subjects are presented in Table 1. All patients enrolled in the study fullfilled the following inclusion criteria: 1) ACL tear with or without concomitant meniscal injury, 2) identical ACL reconstruction surgery by using patellar tendon as a bone-to-bone graft fixed by screws so that accelerated rehabilitation was possible with almost no risk of graft displacement (Fleming et al., 2002; Williams et al., 2004), and 3) all subject had to be non-competitive athletes. Exclusion criteria were: 1) previous injuries and/or surgery of the knee and other joints of the ipsi- and contralateral limb, 2) history of heart or lung disease that would limit rehabilitation exercise, 3) no contraindication for performing WBV exercise as reported by Fu and colleagues (2013), and 4) previous WBV exercise to avoid a possible memory effect. By the use of computer generated numbers, the subjects were randomly divided into a WBV exercise (“experimental”) group and a standard exercise control (“standard”) group, with 20 patients in each group (Figure 1).
Table 1.
Patients data presented as mean ± standard deviation (95% confidence interval) for subjects in WBV and standard rehabilitation programs.
| WBV program | Standard program | |
|---|---|---|
| Total enrolled in investigation, n | 20 | 20 |
| Male | 14 | 15 |
| Female | 6 | 5 |
| Average age, years | 27 ± 4.2 (25.2-28.8) | 28 ± 6.8 (25-30.9) |
| Average weight, kg | ||
| Male | 86.4 ± 7.9 (81.9-90.9) | 87.1 ± 6.2 (84.4-89.8) |
| Female | 67.5 ± 5.3 (65.2-69.8) | 65.3 ± 4.6 (63.3-67.3) |
| Body Mass Index | 23.2 ± 3.4 (21.7-24.7) | 24.3 ± 2.8 (23.1-25.5) |
| Dominant limb, n | ||
| Right | 15 | 13 |
| Left | 5 | 7 |
| Days from injury to surgery | 82.4 ± 39.2 (65.2-99.6) | 90.7 ± 47.9 (69.7-111.7) |
| Time needed per exercise session, min | 40 ± 2.3 (38.9-41.1)** | 85 ± 4.4 (83.1-86.9) |
** p < 0.001 between WBV and standard program.
Figure 1.
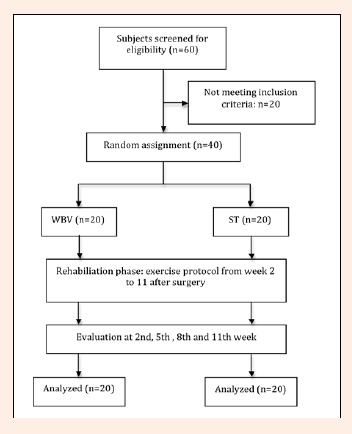
Flow diagram for participants of this study performing the whole body vibration (WBV) or standard exercise (ST) protocol.
Stratified on sex, 29 males (WBV 14, controls 15) and 11 females (WBV 6, controls 5) were randomized to the experimental and control group. This study complied to the laws of the Federal Republic of Germany and followed the Declaration of Helsinki. Written informed consent was obtained from all participants before the tests.
Exercise programs and rehabilitation
All patients underwent a similar postoperative physical therapy program to reduce irritation of damaged tissue and regain mobility. The program included cryotherapy, mobilization exercise, proprioceptive training, stretching and strengthening exercise, functional training, balance exercise and gait re-education. Physical therapy was started on the first day after surgery and continued as an outpatient treatment program on the second week after surgery with a frequency of five times per week in both groups. In addition, muscle exercise three to four times a week started in the 2nd week post surgery and lasted up to the 11th week post surgery. Thus, the total duration of the rehabilitation program was ten weeks.
In each group the individual optimum intensity and amount of exercise was chosen according to the recommended standards of medical sports exercise (Garber et al., 2011). The methodology of the warm-up program was identical in both groups, but differed in the factors power and coordination, which subsequently lead to a variation in the duration of exercise for each session. Absence of pain and signs of inflammation such as tissue swelling were taken as control parameters during and after exercise.
Control group
The protocol of “standard” rehabilitation und muscle strength exercise is based on the principles of accelerated rehabilitation, which means early restoration of full joint movement and weight bearing (Tagesson et al., 2008). Every session lasted about 80 minutes starting with a phase of warm-up followed by stretching and a standard 20 minutes balance exercise to improve balance in bipedal standing. This exercise included standing on the injured leg with and without the use of a wobble board and step ups. Thereafter, muscle strength exercise started. Details of the strengthening program (type of exercise number of sets and repetitions) are shown in Table 2. The training session finished with a cool-down phase similar to the WBV protocol.
Table 2.
Exercise protocol of the control group.
| Standard Muscle Exercise | Phase 1 (up to 6th week) | Phase 2 |
|---|---|---|
| Load | 50-60% of one repetition (rep) maximum | 60-80% of one rep maximum |
| Hip-adduction, proximal (femur) lever, standing-up | 2 to 4 sets 12 to 20 reps |
2 to 4 sets 8 to 12 reps/set |
| Hip-abduction with proximal (femur) lever, standing-up | 2 to 4 sets 12 to 20 reps |
2 to 4 sets 8 to 12 reps/set |
| Hip-extension with proximal (femur) lever, standing –up | 2 to 4 sets 12 to 20 reps |
2 to 4 sets 8 to 12 reps/set |
| Hip-flexion with proximal (femur) lever, standing-up | 2 to 4 sets 12 to 20 reps |
2 to 4 sets 8 to 12 reps/set |
| Leg Curl with proximal (femur) lever, supine /sitting | 2 to 3 sets 15 to 30 reps |
2 to 4 sets 15 to 20 reps/set |
| Leg Press, knee-extension, supine | 2 to 3 sets 15 to 30 reps |
2 to 4 sets 15 to 20 reps/set |
| Calf Rise, plantar flexion, standing-up | 2 to 4 sets 12 to 20 reps |
2 to 4 sets 8 to 12 reps/set |
| Balance Exercise | ||
| Standing on one leg | 10 reps each side | 10 reps each side |
| Standing on one leg on a wobble board | 5 reps each side | 10 reps each side |
| Step ups | 2 min | 2 min |
WBV group
The WBV protocol (Table 3) was developed based on earlier investigations on the influence of WBV exercise in muscle performance in sports and on single case studies of patients with ACL-surgery. WBV exercise always started with a warm-up phase that consisted of 10 to 15 minute cycling on an ergometer cycle at a low speed. Afterwards, patients were stretching muscle and then began up to 20 minutes of muscle exercise on the vibration platform. The last phase included 5 minutes cool-down cycling. All WBV muscle exercises were conducted using the Galileo 2000 WBV machine (Novotec Medical GmbH, Pforzheim, Germany). The platform of the Galileo 2000 has the ability of alternate vertical oscillation, which is different from other WBV exercise machines using bilateral synchronized oscillation. Vibration amplitude varied individually between 5 to 9 mm.
Table 3.
Exercise protocol of the WBV group
| Time | Exercise |
|---|---|
| Week 2 - 4 | Isometric standing position on the WBV-platform with a vibration frequency of 10 to 15Hz for one minute and with an increasing amount of repetitions (2 up to 6 series). |
| Weeks 5 - 7 | Isometric exercise described above remained, but vibration frequency and hence exercise intensity increased progressively every day in steps of 5 Hz dependent on the patient’s individual shape up to 30Hz. Five series of 1.5 to 2 min. |
| Weeks 8-11, standing-up | Transition to dynamic exercise in the form of squats. Additional load (10% of maximum muscle strength) was applied depending on the individual shape. Five to seven series of 2 minutes. |
The WBV protocol started in the 2nd week after surgery. First, patients were lying in a supine position with the feet parallel at hip width. The knee and hip joint were bent in the sagittal plane over the forefoot with equal work loads on the fore and hind foot. This slide flexion both of the hip and knee joint provide ventral slide of the pelvic girdle due to the problem of shortened iliopsoas. Then, we transferred this preconditioned posture to perform isometric exercise in upright bipedal position without WBV. Patients had to wear shoes while standing on the platform. The goal of this first session was to teach bipedal standing with co-contracted abdominal and back and gluteal muscles and fully erected pelvic and spine.
After this, WBV muscle exercise was started. Patients were asked to take the same defined bipedal upright position as stated above/taught in the first session with slightly bend knee and hip joints. While keeping this posture and performing isometric exercise, the WBV platform operated with a vibration frequency of 10 to 15Hz for one minute and with an increasing amount of repetitions (from 2 up to 6).
From 5th postoperative week on, the defined body posture under isometric exercise as described above remained the same, but vibration frequency and hence exercise intensity increased progressively every day dependent on the patient’s individual shape up to 30Hz. Five series of 1.5 to 2 minutes each were carried out.
The third phase (8th up to 11th week) included the transition from isometric to dynamic exercise in terms of squats. For lower extremity strength, the use of squat or squat position was mostly used; this guarantees a synergistic activation of knee extensor and flexor groups, thus co-activating the hamstring (Beynnon et al., 2005a; Cardinale and Wakeling, 2005). The movement was performed at low speed and with the bipedal up-right position and preactivated abdominal, gluteal and hamstring muscles. Additional load (up to 30% of bodyweight) was applied depending on the individual shape (Figure 2). This period included five to seven series of 2 minutes.
Figure 2.
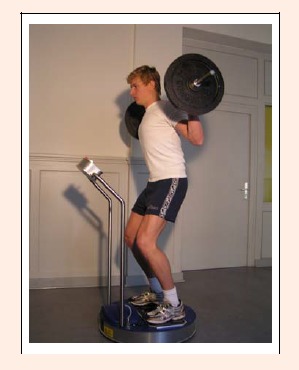
Patient standing on the WBV platform in week 11 after surgery performing exercise in the preconditioned body posture with additional load.
Testing protocols: Time-table of testing
In order to evaluate the rehabilitation progress, all patients were evaluated four times (weeks 2, 5, 8 and 11) after surgery. Main outcome measurement was achieved by measuring isometric, dynamic force parameters and by the use of a balance testing device.
Clinical parameters
The clinical examination of the injured joint including case history was performed at above mentioned four distinct times after surgery. It included measurement of active range of motion using a goniometer. Parameters of inflammation and pain had only been registered but not measured or graded. Measurement of knee joint laxity was evaluated with the KT1000 arthrometer (MEDmetric Corporation, San Diego, CA, U.S.A.) at 90N and 130N posterior anterior directed loads. This was performed immediately after surgery at the operation table and at 11th week after surgery.
Dynamic and isometric muscular strength testing
Isometric and isokinetic testing with a Biodex System 3 dynamometer (Biodex Medical Systems Inc., Shirley, NY, U.S.A.) was used to assess knee flexor and extensor muscle strength (Bemben et al., 1988). In all tests, the order of legs tested was randomly determined. All measurements were followed by a standardized warm-up phase, which included pedaling on an bicycle ergometer (75 to 100 W) and hamstring and quadriceps muscles stretching exercises. The subject was placed on the dynamometer (with 105° of hip flexion) and the body fixed by straps around the thigh, waist and chest to avoid compensative movement.
Isometric testing was performed at 60°, 75° and 90° of knee flexion. Maximum isometric muscle strength of knee extensor and flexor muscle was measured during 5 seconds of maximum isometric contraction.
Isokinetic testing was performed in concentric and eccentric modus with five following repetitions at an angular speed of 60 deg/sec with maximum effort. To protect the graft, we chose an individual restriction of knee movement setting a range of motion (ROM) between 0° of extension and 90° of flexion.
The bilateral comparison permitted determination of asymmetries expressed in percentages and defining the parameters of isometric or isokinetic muscle strength and underwent further analysis.
Postural control test
The patient's postural stability was assessed utilizing the Biodex Stability System (Biodex, Shirley, NY, U.S.A.). The Biodex Stabilometer offers an unstable platform that can assess total, anteroposterior, and mediolateral postural stability (Henrikkson et al., 2001; Pincivero et al., 1995). Prior to testing, subjects were asked to find the most stable foot placement on the platform, and this foot position was maintained throughout all three trials. This was the reference point from which the center of pressure was measured. Thereafter, subjects had to perform a one-leg stand on the free-moving stability platform with the knee slightly flexed and with the contralateral limb flexed to 90 degrees for 20 seconds. The stabilometer setting was at level 4 during all tests (Pincivero et al., 1995). The participants were instructed to keep the platform as stable as possible and had to cross both arms before the chest to minimize their use in attaining balance as outlined in the system operating manual. No verbal feedback was given during the testing. Moreover, we covered the control screen of the panel and patients had to focus straight on a defined spot at horizontal eye level to avoid visual feedback regarding performance during the procedures. Each limb was tested three times as in previous studies (e.g. Pincivero et al. 1995) using the Biodex Stabilometer for an assessment of postural stability, and the mean of the three trials was determined. Results were reported in average degrees of displacement from a stable reference position. A higher score indicates less postural stability. Conversely, the lower the degrees of displacement, the more stable the platform, representing greater postural stability. The Biodex Stabilometer has been shown to provide measurements of total stability index with good reliability of r=.72 (Pincivero et al., 1995).
Rating system (Lysholm Score)
We integrated the Lysholm (Gillquist) Score in this study to examine patients symptoms including locking, instability, pain, swelling, ability to climb stairs and squats (Lysholm and Gillquist, 1982). It is defined by a 100 point scoring system and is one of the most often used scales for the assessment of psychometric parameters following knee joint surgery (Briggs et al., 2009; Tagesson et al., 2008).
Statistical analysis
We determined normal distribution of data by a Kolmogorov-Smirnov test. Repeated-measured analysis of variance (ANOVA) was performed using statistical software (SPSS 16.0, Chicago, IL, U.S.A.). One-factor ANOVA was used to determine the significance of time on the measured parameters. To identify the influence of the factors “time” and “treatment” on the measured parameters, we applied a 2-factor ANOVA. Bonferroni-Dunn post-hoc testing was used to determine the significance of differences between the two groups. The level of significance was set at 95% (p < 0.05) and corrected for multiple comparisons. We calculated eta-squared (s2) as a measure of effect size. The data are presented as mean with one standard deviation and 95% confidence intervals.
Results
All patients started exercise in the 2nd week postoperatively. No patients were lost to follow-up, and each subject was able to carry out the program according to the protocol (100% compliance). Minor complications such as pain or swelling during or after muscle exercise occurred in 12/20 (60%) in the WBV group and 14/20 (70%) in the control group up to the 6th week. This could be easily controlled in every case by reducing the intensity of muscle exercise in the following one or two sessions. The WBV group had exercise 3.8 times per week and the control group 3.4 times per week. Tests taking place in the 2nd, 5th, 8th and 11th week after surgery.
Clinical parameters
Sign of inflammation like overheating, swelling or bruises were comsiderably reduced between the 2nd and 11th week after surgery in both groups. The range of motion increased in both groups up to full motion, however, no differences between WBV and control group were apparent (Table 4). Anterior posterior knee joint laxity measured by KT 1000 was similar between both groups and restored to within 2mm of the contralateral side (Table 5). We found a small but not significant increase of laxity in both groups from intraoperatively to 11 week. The interaction of the factors “group” and “time” was not significant (ANOVA, p = 0.33) and the main effects were not different (ANOVA, factor “group”, p = 0.53, factor “time”, p = 0.19).
Table 4.
Group comparison of range of motion.
| WBV Program | Standard Program | p-value | ||
|---|---|---|---|---|
| Extension Deficit, deg | Week 2 | 19.7 ± 10.6 (15.1-24.4) | 24.3 ± 12.5 (18.8-29.8) | .07 |
| Week 5 | 10.4 ± 8.6 (6.6-14.2) | 15.3 ± 10.5 (10.7-19.9) | .04* | |
| Week 8 | 8.2 ± 7.0 (5.1-11.3) | 9.6 ± 8.5 (5.9-13.3) | .14 | |
| Week 11 | 5.0 ± 5.4 (2.6-7.4) | 7.5 ± 5.7 (5-10) | .11 | |
| Flexion deficit, deg | Week 2 | 15.3 ± 12.2 (10-20.7) | 17.3 ± 9.2 (13.3-21.3) | .23 |
| Week 5 | 8.7 ± 8.9 (4.8-12.6) | 10.5 ± 6.8 (7.5-13.5) | .18 | |
| Week 8 | 5.8 ± 8.0 (2.3-9.3) | 7.2 ± 5.9 (4.6-9.8) | .20 | |
| Week 11 | 3.0 ± 4.7 (1-5) | 4.1 ± 4.4 (2.2-6) | .29 |
Nonsurgical vs. surgical limb: positive values indicate a deficit. Data are presented as mean ± standard deviation (95% confidence interval).
N/A = value is not available.
* p < 0.05 between WBV and standard program.
Table 5.
KT 1000 Arthrometer measurement of anterior-posterior knee laxity at 90N.
| Immediately after surgery | 11 week (mean, SD) |
p-value | |
|---|---|---|---|
| WBV Group | 1.0 ± 2.1 (.1-1.9) |
1.5 ± 2.5 (.4-2.6) |
.29 |
| Control Group | 1.2 ± 1.9 (.4-2.0) |
1.6 ± 2.4 (.6-2.7) |
.25 |
Dynamic and isometric muscular strength testing
Table 6 shows that both groups displayed significant increases in strength with regard to extensor muscles as well as flexor muscles during the rehabilitation period. Patients assigned to the WBV protocol had an increased isometric knee extension strength with 31% deficit in the hamstrings and 36% in the quadriceps compared to the uninjured leg. There were no significant differences between the standard and experimental group (ANOVA, factor “group”, p = 0.22).
Table 6.
Group comparison of strength variables.
| WBV Program | Standard Program | |
|---|---|---|
| Isokinetic Testing Hamstring ratio, % | ||
| Week 2 | N/A | N/A |
| Week 5 | N/A | N/A |
| Week 8 | 64 ± 15 (57-71) | 66 ± 15 (59-73) |
| Week 11 | 76 ± 11 (71-81) | 72 ± 11 (68-77) |
| Isokinetic Testing Quadriceps ratio, % | ||
| Week 2 | N/A | N/A |
| Week 5 | N/A | N/A |
| Week 8 | .54 ± .18 (.46-.62) | .55 ± .18 (.47-.63) |
| Week 11 | .67 ± .18 (.59-.75) | .62 ± .18 (.54-.70) |
| Isometric Testing Hamstring ratio, % | ||
| Week 2 | 56 ± 18 (48-64) | 56 ± 16 (49-63) |
| Week 5 | 63 ± 15 (56-70) | 63 ± 18 (55-71) |
| Week 8 | 68 ±16 (61-75) | 65 ± 15 (58-72) |
| Week 11 | 77 ± 17 (70-85) | 75 ± 17 (68-83) |
| Isometric Testing Quadriceps ratio, % | ||
| Week 2 | 58 ± 25 (47-69) | 57 ± 20 (48-66) |
| Week 5 | 58 ± 25 (47-69) | 57 ± 18 (49-65) |
| Week 8 | 62 ± 21 (53-71) | 67 ± 3 (66-68) |
| Week 11 | 64 ± 9 (60-68) | 70 ± 3 (69-71) * |
Surgical limb as percentage of nonsurgical limb (i.e. surgical / nonsurgical x 100). Data are presented as mean ± standard deviation (95% confidence interval).
N/A = value is not available.
* p < 0.05 between WBV and standard program.
Concentric peak torque in the injured flexor muscles increased to 26% deficit in the WBV group compared to 28% deficit in the control group at respective angular speeds of 60 deg/sec. The deficit in the extensor muscles was significantly reduced to 35% in the WBV group (ANOVA, factor “time”, p = 0.02) and to 38% in the control group (ANOVA, factor “time”, p = 0.01). Therefore the reduction of muscle strength deficit over time was almost completely comparable in both contraction modes without a significant difference between the groups (ANOVA, p = 0.32).
Postural control test
The experimental group showed considerable and significant improvement of balance during the period represented by a lower stability index at each testing session (ANOVA, factor “time”, p = 0.03). In contrast, the small improvement of the controls was not statistically significant (p = 0.36). The comparison of groups showed a significant better development of the experimental group (ANOVA, factor “group”, p = 0.02). For detailed results see Table 7.
Table 7.
Group comparison of stability index.
| WBV Program | Standard Program | p-value | |
|---|---|---|---|
| Week 2 | 4.7 ± 2.3 (3.7-5.7) | 5.4 ± 3.0 (4.1-6.7) | .17 |
| Week 5 | 4.0 ± 1.8 (3.2-4.8) | 5.1 ± 2.4 (4.0-6.2) | .07 |
| Week 8 | 3.3 ± 1.5 (2.6-4.0) | 4.9 ± 2.4 (3.9-6.0) | .02 * |
| Week 11 | 3.1 ± 1.3 (2.5-3.7) | 4.7 ± 2.8 (3.5-5.9) | .01 * |
The scale ranges from 0 to 10. Higher values indicate less postural stability. Data are presented as mean ± standard deviation (95% confidence interval).
* p < 0.05 between WBV and standard program.
Rating system (Lysholm Score)
The score results showed a constant and significant improvement in both groups (ANOVA, interaction of factors “group” and “time”, p = 0.01). The values reached 85 in the WBV group compared to 87 in the control group. There were no statistically significant differences between both groups (ANOVA, factor “group”, p = 0.47).
Time spent per session
When regarding the time spent for a rehabilitation session as criterion for effectiveness, we found an average time span of 40 ± 2.3 minutes per session of the WBV group which is highly significant shorter compared to the 85 ± 4.4 minutes (p < 0.001) spent by the controls.
Discussion
The goal of this preliminary study was to investigate whether a new concept of strength exercise using squats or squat position with WBV as the main stimulus would be applicable and suitable in ACL rehabilitation. Therefore, we replaced strength and balance exercises by a novel WBV exercise training program and compared it to a current muscle exercise program used in ACL rehabilitation.
The methodical approach of this prospective randomised controlled study allowed a comparison of both protocols using clinical, strength and neuromuscular parameters. Both groups were comparable with regard to ACL-replacement, graft, graft-fixation, variance of age and sex. All patients had the precondition to follow accelerated rehabilitation, which was instrumental in decreasing the postoperative complications associated with prolonged immobilization of the postoperative knee (Wright et al., 2008b).
Overall, the experimental group conducting the WBV exercise protocol reached equal results compared to the control group, which were even better regarding balance performance. This is in congruence with prior investigations who reported an improved postural balance and knee proprioception in patients that underwent WBV training after ACL reconstruction (Moezy et al., 2008). However, the WBV group was significantly better at all times although the control group performed balance exercise on the wobble board (Table 7). Apparently this way of improving the ability to maintain one-leg stand on an unstable platform can be regarded as even more effective than the balance exercise on an unstable wobble board (Torvinen et al., 2002). One possible reason could be the better ability of muscle co-contraction, which is influenced by the specific posture of the trunk (Berschin and Sommer, 2010). In contrast to other existing studies using WBV in ACL tear rehabilitation (Moezy et al., 2008; Fu et al., 2013), we paid special attention to keep and maintain this posture throughout the WBV exercise program.
Ligament laxity measured by KT-1000 was similar in both groups, indicating sufficient mechanical joint stability. Immediately after surgery we detected only small values of laxity. The side to side differences restored as well after 11 weeks within 2 mm. The magnitude of the difference was lower than those of Beynnon and co-workers (2005a), which at the same time is an expression for better stability in the anterior drawer and Lachman tests. Besides this aspect, there was no difference between both groups regarding the restoration of full knee ROM, as well. Both, knee stability and full ROM, are important factors for reaching a preinjury level of strength, mobility and sports participation with low re-injury rates in the long run (Ardern et al., 2012; Kvist, 2004; Tagesson et al., 2008). These results lead us to the assumption that WBV therapy is a safe method despite being applied as early as two weeks after surgery in patients who underwent ACL reconstruction showing no disadvantage of functional outcome measures. Concerning the possible risk of graft damage or loss of fixation, co-contraction of the extensor and flexor muscle chain can reduce the load to a minimum, even during squat exercise at a low speed within the possible range of motion (Beynnon et al., 2005a). However, we have no long-term outcome of these parameters.
Therefore, the recovery of pre-injury levels of muscle strength for better control of knee motion and weight bearing to protect the ACL-graft is a central goal of rehabilitation. As described in previous studies, the strength deficit in the injured limb can still be detected 11 weeks after surgery (Beard and Dodd, 1998; Hiemstra et al., 2000). In our study the parameters of muscle strength are almost comparable in both groups. About 60% of quadriceps and 70% of hamstring deficits were noted in the surgical limb compared to the non-surgical limb in both groups, which were comparable to previously reported ratios (Beard and Dodd, 1998).
Against expectation, no significant higher values in maximum isometric and isokinetic muscle strength of the hamstring muscles were detected in the WBV group. Thus, we conclude that WBV exercise does not necessarily lead to higher values of knee flexor muscle strength compared to standard exercise using this testing device. This may be the result of isometric and isokinetic muscle strength measurement in an open chain exercise performed in a sitting position, which does not reflect WBV exercise in closed chain exercise and bipedal standing position. However, our standard exercise protocol partially included closed chain exercise, as well, indicating that different balance abilities in both groups might be the reason for the prediscribed contradiction.
The patient questionnaire confirmed a good compliance in carrying out WBV training. The assessment of the subjective rehabilitation progress via Lysholm Score in addition to the objective measurement of clinical parameters displayed similar results for both groups. Despite being widely-used, the Lysholm questionnaire is under discussion, because some authors found it less sensitive for the ACL patients especially to evaluate knee function over time (Bengtsson et al., 1996). However, as it can be seen in all scoring systems despite of adequate weighting, these results can only represent an overall estimation of knee status (Briggs et al., 2009).
Another major finding of our study was a shorter muscle exercise period in the WBV group. As time spent for rehabilitation is one of the important factors not for competetive (varsity) athletes only but also for subjects engaging in regular recreational sports, the WBV group was highly effective in reaching the rehabilitation milestones. Despite a reduction to less than half of the time the control group needed, isometric and isokinetic muscle strength values matched those of the experimental group, which even showed significant better results in the stability test. This advantage seems noteworthy, not only for the possible improvement of the patients´ compliance and motivation due to a shorter exercise session, but also from an economical point of view. A recent study by Mather and colleagues (2013) estimated a life-time cost of about 38.000 US$ for each patient who underwent ACL reconstruction in the United States of America. One key point in the reduction of injury-related costs is the length of the rehabilitation program and the time needed to return to preinjury levels of physical activity. Here, our study gives additional evidence in which way a WBV rehabilitation program might reduce health care costs. However, further trials are needed to analyze if our WBV protocol could eventually lead to a better cost-effectiveness with equal or even more favourable results compared to established rehabilitation programs.
To the best of the authors´ knowledge, there are only two published RCT adressing the impact of WBV training on neuromuscular control in patients who underwent ACL reconstruction. Moezy and colleagues (2008) compared four weeks of WBV training with conventional strength training starting three months after ACL surgery. The twelve patients in the WBV group performed static and dynamic squats as well as single-leg stance on a vibration platform. Throughout the 12 sessions, there was an increase in vibration frequency (from 30 to 50 Hz), amplitude (from 2.5 to 5 mm) and duration (from 4 to 16 minutes). The conventional group performed flexibility and proprioceptive training along with progressive strengthening exercises. After one month of training, patients in the WBV group had greater improvements in postural stability and proprioception.
Fu and colleagues (2013) investigated 48 patients, of whom 24 received either eight weeks of conventional rehabilitation or additional WBV therapy starting one month after surgery. The WBV group had a total of 16 sessions with an increase in vibration frequency (from 35 to 50 Hz), a consistent amplitude of 4 mm and a gradual increase of training and resting time. The protocol was composed of both static and dynamic exercises (high squat, low squat, single-legged squat). In this study, the WBV group showed better results in single-legged hop, postural control and shuttle run control than the reference group.
However, the authors of both studies did not further consider the influence of the patients´ body posture while exercising on the WBV platform, as stated above. Besides, they used a training period of four and eight weeks, respectively, which could be too short for the prevention of re-injury and restoration of full muscle function (Zech et al., 2009). Furthermore, both studies did not use an accelerated rehabilitation protocol. Fu and colleagues (2013) also mentioned the lack of a common rating system such as the Lysholm score for comparison in their study.
Against the background of the existing reports, our study adds the following novel information: 1) The feasibility of an accelerated WBV protocol in patients undergoing ACL rehabilitation starting as early as week 2 after surgery, 2) the use of a vibration platform with the feature of side-alternating oscillation, which is different from common WBV exercise machines using synchronous vertical oscillation, 3) special focus on the maintained body posture during exercise on the WBV platform and its possible influence on neuromuscular performance, and 4) examination of the time spent for rehabilitation.
Besides the type of vibration platform, our study differed in the vibration frequencies. We started with an platform vibration frequency between 10 and 15 Hz during the first two weeks, which was lower than in most other studies (Rittweger, 2010). It is known that increases in the natural frequency between 10 and 50 Hz as an expression of tissue stiffness of a vibrating system lead to an increase in muscle activity of the lower extremity (Cardinale and Wakeling, 2005). Moreover, Rittweger and colleagues (2002) showed that even with vibration frequencies of 18 Hz, there was an increase in metabolic power compared to the baseline condition using a Galileo WBV machine. Higher vibration frequencies may lead to skidding of the patients´ feet, which alters the posture on the WBV platform and possible vibration effects on neuromuscular performance (Rauch et al., 2010; Rittweger, 2010). Since the early post-operative beginning of our rehabilitation protocol, we started with lower frequencies and increased them subsequently from the 5th post-operative week on to 30 Hz. To minimize resonance phenomena, especially to the eye bulbs, and vibration transmissibility, we asked patients to keep the preconditioned posture while standing upright on the WBV platform. Moreover, the transmissibility is smaller in side-alternating WBV compared to synchronous WBV (Rittweger, 2010).
Study limitations
Important limitations of our study are the short observation period during the rehabilitation process. As long-term outcome is one of the key points of rehabilitation, our data needs further exploration over a distance of at least two years for better interpretation and validation of the results. Therefore, to take account for study drop-outs and patients lost to follow-up, a greater sample size is needed to achieve reproducible results. Against this background, we were unable to calculate a sample-size for a sufficient statistical testing power due to the preliminary character of this study. The lack of comparable data for our WBV rehabilitation protocol was the main reason for a post hocpower calculation, which produced a sufficient value (d2 = 0.67). Additionally, all measured parameters except balance testing did not differ between groups. This might be the result of the small sample size, co-factor influences between the groups, or different levels of muscular activity within the patients this early after surgery. Due to the methodology of this open trial, there is the possibility of information bias because the outcome assessors were not blinded. Although participants received no information about the performance of the other group throughout and after completion of the study, they were not blinded to their treatment and thus could potentially give selective information regarding clinical parameters (pain, subjective instability etc.) and Lysholm Score data.
Regarding a better stability test performance, future follow-up studies combined with additional EMG-monitoring are needed to confirm that muscle co-activation patterns are the reason for this observation. The follow-up investigation of both groups six months post surgery gave no information that the ACL-graft had been influenced negatively i.e. by resonance phenomena of bone due to the vibration load. Using this WBV protocol on other grafts and graft-fixation methods may involve a slightly increased risk, however, it should still be within the same acceptable limits of a standard rehabilitation program.
Conclusion
The stage of rehabilitation is of upmost importance following reconstructive ACL surgery. As there is an abundance of different rehabilitation approaches, we present a novel WBV rehabilitation protocol starting as early as the second week after surgery in this prospective randomized trial. Our short-term results underline the advantages of this protocol compared to a standard muscle exercise program. We found equivalent results in muscle strength, knee joint stability and subjective quality of life with special regard to knee function after ACL reconstruction. Even more, postural control was improved in the WBV group despite a more than 50% reduction in time spent for exercise sessions. With these preliminary findings, our whole body vibration muscle exercise protocol could be considered as a practical alternative to a standard exercise program in ACL-rehabilitation. However, further studies are needed to evaluate and reproduce these effects with a longer follow-up and investigate possible co-activation patterns of muscles using additional experiments.
Biographies

Gereon BERSCHIN
Employment
PD at the Department of Sports Science and Motology, Philipps-University Marburg, Marburg, Germany
Degree
PhD
Research interests
Exercise and Training, Biomechanics, Posture, Rehabilitation
E-mail: berschin@staff.uni-marburg.de

Björn SOMMER
Employment
Resident physician at the Department of Neurosurgery, University of Erlangen-Nuremberg, Erlangen, Germany.
Degree
MD
Research interests
Non-invasive diagnostics, Orthotic management of the lower limb, Haemodynamics.
E-mail: bjoern.sommer@uk-erlangen.de

Antje BEHRENS
Employment
Sports Therapist
Degree
PhD
Research interests
Rehabilitation
Hans-Martin SOMMER
Employment
Professor emeritus of the Department of Sports Science and Motology, Philipps-University Marburg, Marburg, Germany
Degree
PhD, MD
Research interests
Motor control, Gait and Posture, Pathomechanisms of sports injuries
E-mail: hmsommer@t-online.de
References
- Ardern C.L., Taylor N.F., Feller J.A., Webster K.E.(2012) Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. American Journal of Sports Medicine 40, 41-48 [DOI] [PubMed] [Google Scholar]
- Beard D.J., Dodd C.A.(1998) Home or supervised rehabilitation following anterior cruciate ligament reconstruction: a randomized controlled trial. Journal of Orthopaedic and Sports Physical Therapy 27, 134-143 [DOI] [PubMed] [Google Scholar]
- Bemben M.G., Grump K.J., Massey B.H.(1988) Assessment of technical accuracy of the Cybex II ® isokinetic dynamometer and analog recording system. Journal of Orthopaedic and Sports Physical Therapy 10, 12-17 [Google Scholar]
- Bengtsson J., Möllborg, J, Werner S.(1996) A study for testing the sensitivity and reliability of the Lysholm knee scoring scale. Knee Surgery, Sports Traumatology, Arthroscopy 4, 27-31 [DOI] [PubMed] [Google Scholar]
- Berschin G., Sommer H.M.(2010) The influence of posture on transmission and absorption of vibration energy in whole body vibration exercise. Sportverletzung Sportschaden 24, 36-39 (In German: English abstract). [DOI] [PubMed] [Google Scholar]
- Beynnon B.D., Uh B.S., Johnson R.J., Abate J.A., Nichols C.E., Fleming B.C., Poole A.R., Roos H.(2005a) Rehabilitation after cruciate ligament reconstruction. A prospective randomized, double blind comparison of programs administered over 2 different time intervals. American Journal of Sports Medicine 33, 347-359 [DOI] [PubMed] [Google Scholar]
- Beynnon B.D., Johnson R.J., Abate J.A., Fleming B.C., Nichols C.E.(2005b) Treatment of anterior cruciate ligament injuries, Part 1. American Journal of Sports Medicine 33, 1579-1602 [DOI] [PubMed] [Google Scholar]
- Beynnon B.D., Johnson R.J., Abate J.A., Fleming B.C., Nichols C.E.(2005c) Treatment of anterior cruciate ligament injuries, Part 2. American Journal of Sports Medicine 33, 1751-1767 [DOI] [PubMed] [Google Scholar]
- Bosco C., Cardinale M., Tsarpela O., Colli R., Tihanyi J., von Duvillard S.P., Viru A.(1998) The influence of whole body vibration on jumping performance. Biology of Sport 15, 157-164 [Google Scholar]
- Briggs K.K., Lysholm J., Tegner Y., Rodkey W.G., Kocher M.S., Steadman J.R.(2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. American Journal of Sports Medicine 37, 890-897 [DOI] [PubMed] [Google Scholar]
- Cardinale M., Wakeling J.(2005)Whole body vibration exercise: are vibrations good for you? British Journal of Sports Medicine 39, 585-589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeGail P., Lance J.W., Neilson P.D.(1996) Difference on tonic and phasic reflex mechanisms produced by vibration on muscles in man. Journal of Neurology, Neurosurgery, and Psychiatry 29, 1-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delay B.S., Smolinski R.J., Wind W.M., Bowman D.S.(2001). Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. American Journal of Knee Surgery 14, 85-91 [PubMed] [Google Scholar]
- Delecluse C., Roelants M., Verschueren S.(2003) Strength increase after whole-body vibration compared with resistance training. Medicine and Science in Sports and Exercise 35, 1033-1041 [DOI] [PubMed] [Google Scholar]
- De Ruiter C.J., Van Raak S.M., Schilperoort J.V, Hollander A.P., de Haan A.(2003). The effects of 11 weeks whole body vibration training on jump height, contractile properties and activation of human knee extensors. European Journal of Applied Physiology 90, 595-600 [DOI] [PubMed] [Google Scholar]
- Fleming B.C., Brattbakk B., Peura G.D., Badger G.J., Beynnon B.D.(2002) Measurement of anterior-posterior knee laxity: a comparison of three techniques. Journal of Orthopaedic Research 20, 421-426 [DOI] [PubMed] [Google Scholar]
- Frank C.B., Jackson D.W.(1997) The science of reconstruction of the anterior cruciate ligament. Journal of Bone and Joint Surgery. American volume 79, 1556-1576 [DOI] [PubMed] [Google Scholar]
- Frobell R.B., Roos E.M., Roos H.P., Ranstam J., Lohmander S.(2010) A randomized trial of treatment for acute anterior cruciate ligament tears. New England Journal of Medicine 363, 331-342 [DOI] [PubMed] [Google Scholar]
- Fu C.L., Yung S.H., Law K.Y., Leung K.H., Lui P.Y., Siu H.K., Chan K.M.(2013) The effect of early whole-body vibration therapy on neuromuscular control after anterior cruciate ligament reconstruction: a randomized controlled trial. American Journal of Sports Medicine 41, 804-814 [DOI] [PubMed] [Google Scholar]
- Garber C.E., Blissmer B., Deschenes M.R., Franklin B.A., Lamonte M.J., Lee I.M., Nieman D.C., Swain D.P., the American College of Sports Medicine. (2011) American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Medicine and Science in Sports and Exercise 43, 1334-1359 [DOI] [PubMed] [Google Scholar]
- Henriksson M., Ledin T., Good L.(2001) Postural control after anterior cruciate ligament reconstruction and functional rehabilitation. American Journal of Sports Medicine 29, 359-366 [DOI] [PubMed] [Google Scholar]
- Hewett T.E., Ford K.R., Myer G.D.(2006)Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. American Journal of Sports Medicine 34, 490-498 [DOI] [PubMed] [Google Scholar]
- Hiemstra L.A., Webber S., Mac Donald P.B., Kriellaars D.J.(2000) Knee strength deficits after hamstring tendon and patellar tendon anterior cruciate ligament reconstruction. Medicine and Science in Sports and Exercise 32, 1472-1479 [DOI] [PubMed] [Google Scholar]
- Hooper D.M., Morrissey M.C., Drechsler W., Morrissey D., King J.(2001) Open and closed kinetic chain exercises in the early period after anterior cruciate ligament reconstruction. Improvement in level malking, stair ascent, and stair descent. American Journal of Sports Medicine 29, 167-174 [DOI] [PubMed] [Google Scholar]
- Hübscher M., Zech A., Pfeifer K., Hänsel F., Vogt L., Banzer W.(2010) Neuromuscular training for sports injury prevention: a systematic review. Medicine and Science in Sports and Exercise 42, 413-421 [DOI] [PubMed] [Google Scholar]
- Issurin V.B., Tennebaum G.(1999) Acute and residual effects of vibratory stimulation training on explosive strength in elite and amateur athletes. Journal of Sports Sciences 17, 177-182 [DOI] [PubMed] [Google Scholar]
- Kruse L.M., Gray B., Wright R.W.(2012) Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. Journal of Bone and Joint Surgery. American Volume 94, 1737-1748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvist J.(2004) Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Medicine 34, 269-280 [DOI] [PubMed] [Google Scholar]
- Lohmander L.S., Englund P.M., Dahl L.L., Roos E.M.(2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. American Journal of Sports Medicine 35, 1756-1769 [DOI] [PubMed] [Google Scholar]
- Luo J., McNamara B., Moran K.(2005) The use of vibration training to enhance muscle strength and power. Sports Medicine 35, 23-41 [DOI] [PubMed] [Google Scholar]
- Lysholm J., Gillquist J.(1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. American Journal of Sports Medicine 10, 150-154 [DOI] [PubMed] [Google Scholar]
- Majewski M., Susanne H., Klaus S.(2006) Epidemiology of athletic knee injuries: A 10-year study. Knee 13, 184-188 [DOI] [PubMed] [Google Scholar]
- Mather R.C., 3rd, Koenig L., Kocher M.S., Dall T.M., Gallo P., Scott D.J., Bach B.R., Jr., Spindler K.P.,MOON Knee Group (2013) Societal and economic impact of anterior cruciate ligament tears. Journal of Bone and Joint Surgery. American volume 95, 1751-1759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moezy A., Olyaei G., Hadian M., Razi M., Faghihzadeh S.(2008) A comparative study of whole body vibration training and conventional training on knee proprioception and postural stability after anterior cruciate ligament reconstruction. British Journal of Sports Medicine 42, 373-378 [DOI] [PubMed] [Google Scholar]
- Pincivero D.M., Lephart S.M., Henry T.(1995)Learning effects and reliability of the Biodex Stability System. Journal of Athletic Training 30, 48 [Google Scholar]
- Rauch F., Sievanen H., Boonen S., Cardinale M., Degens H., Felsenberg D., Roth J., Schoenau E., Verschueren S, Rittweger J.(2010) Reporting whole-body vibration intervention studies: recommendations of the International Society of Musculoskeletal and Neuronal Interactions. Journal of Musculoskeletal and Neuronal Interactions 10, 193-198 [PubMed] [Google Scholar]
- Risberg M.A., Holm I.(2009) The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. American Journal of Sports Medicine 37, 1958-1966 [DOI] [PubMed] [Google Scholar]
- Rittweger J., Ehrig J., Just K., Mutschelknauss M., Kirsch K.A., Felsenberg D.(2002) Oxygen uptake in whole-body vibration exercise: influence of vibration frequency, amplitude, and external load. International Journal of Sports Medicine 23, 428-432 [DOI] [PubMed] [Google Scholar]
- Rittweger J.(2010) Vibration as an exercise modality: how it may work, and what its potential might be. European Journal of Applied Physiology 108, 877-904 [DOI] [PubMed] [Google Scholar]
- Shelbourne K.D., Gray T.(1997) Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. American Journal of Sports Medicine 25, 786-795 [DOI] [PubMed] [Google Scholar]
- Shelbourne K.D., Davis T.J.(1999) Evaluation of knee stability before and after participation in a functional sports agility program during rehabilitation after anterior cruciate ligament reconstruction. American Journal of Sports Medicine 27, 156-161 [DOI] [PubMed] [Google Scholar]
- Tagesson S., Oberg B., Good L., Kvist J.(2008) A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: a randomized clinical trial evaluating dynamic tibial translation and muscle function. American Journal of Sports Medicine 36, 298-307 [DOI] [PubMed] [Google Scholar]
- Torvinen S., Kannu P., Sievänen, H., Järvinen, T.A., Pasanen M., Kontulainen S., Järvinen, T.L., Järvinen, M., Oja P., Vuori I.(2002) Effect of a vibration exposure on muscular performance and body balance. Randomized cross-over study. Clinical Physiology and Functional Imaging 22, 145-152 [DOI] [PubMed] [Google Scholar]
- Williams G.N., Snyder-Mackler L., Barrance P.J., Axe M.J., Buchanan T.S.(2004) Muscle and tendon morphology after reconstruction of the anterior cruciate ligament with autologous semitendinosus-gracilis graft. Journal of Bone and Joint Surgery 86-A, 1936-1946 [DOI] [PubMed] [Google Scholar]
- Wright R.W., Preston E., Fleming B.C., Amendola A., Andrish J.T., Bergfeld J.A., Dunn W.R., Kaeding C., Kuhn J.E., Marx R.G., McCarthy E.C., Parker R.C., Spindler K.P., Wolcott M., Wolf B.R., Williams G.N.(2008a) A systematic review of anterior cruciate ligament reconstruction rehabilitation: part I: continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. Journal of Knee Surgery 21, 217-224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright R.W., Preston E., Fleming B.C., Amendola A., Andrish J.T., Bergfeld J.A., Dunn W.R., Kaeding C., Kuhn J.E., Marx R.G., McCarthy E.C., Parker R.C., Spindler K.P., Wolcott M., Wolf B.R., Williams G.N.(2008b) A systematic review of anterior cruciate ligament reconstruction rehabilitation: part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. Journal of Knee Surgery 21, 225-234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zech A., Hübscher M., Vogt L., Banzer W., Hänsel F., Pfeifer K.(2009) Neuromuscular training for rehabilitation of sports injuries: a systematic review. Medicine and Science in Sports and Exercise 41, 1831-1841 [DOI] [PubMed] [Google Scholar]


