Abstract
The purpose of this study was to compare the effectiveness of either continuous moderate intensity exercise training (CMIET) alone vs. CMIET combined with a single weekly bout of high intensity interval training (HIIT) on cardiorespiratory fitness. Twenty nine sedentary participants (36.3 ± 6.9 yrs) at moderate risk of cardiovascular disease were recruited for 12 weeks of exercise training on a treadmill and cycle ergometer. Participants were randomised into three groups: CMIET + HIIT (n = 7; 8-12 x 60 sec at 100% VO2max, 150 sec active recovery), CMIET (n = 6; 30 min at 45-60% oxygen consumption reserve (VO2R)) and a sedentary control group (n = 7). Participants in the CMIET + HIIT group performed a single weekly bout of HIIT and four weekly sessions of CMIET, whilst the CMIET group performed five weekly CMIET sessions. Probabilistic magnitude-based inferences were determined to assess the likelihood that the true value of the effect represents substantial change. Relative VO2max increased by 10.1% (benefit possible relative to control) in in the CMIET + HIIT group (32.7 ± 9.2 to 36.0 ± 11.5 mL·kg-1·min-1) and 3.9% (benefit possible relative to control) in the CMIET group (33.2 ± 4.0 to 34.5 ± 6.1 mL·kg-1·min-1), whilst there was a 5.7% decrease in the control group (30.0 ± 4.6 to 28.3 ± 6.5 mL·kg-1·min-1). It was ‘unclear’ if a clinically significant difference existed between the effect of CMIET + HIIT and CMIET on the change in VO2max. Both exercising groups showed clinically meaningful improvements in VO2max. Nevertheless, it remains ‘unclear’ whether one type of exercise training regimen elicits a superior improvement in cardiorespiratory fitness relative to its counterpart.
Key Points.
Both continuous moderate intensity exercise training (CMIET) alone and CMIET combined with a single weekly bout of high intensity interval training (CMIET + HIIT) elicit ‘possibly beneficial’ clinically meaningful improvements in cardiorespiratory fitness.
Cardiorespiratory fitness improved by ~1.0 MET in the CMIET + HIIT exercise intervention group, which likely leads to important long-term prevention implications as a 1 MET increase in cardiorespiratory fitness has been linked with an 18% reduction in deaths due to CVD.
There was 100% adherence to interval sessions in the CMIET + HIIT group, suggesting this combination of training can be well-tolerated in previously inactive overweight/obese individuals.
Key words: Exercise prescription, prevention, risk factors, cardiovascular disease
Introduction
By the year 2030, the World Health Organization (WHO) predicts cardiovascular disease (CVD) will be responsible for approximately 23 million deaths annually (WHO, 2012). Most CVDs are largely preventable with regular exercise and physical activity having been shown to improve CVD risk factors. Additionally, exercise improves other diseases associated with inactivity and obesity, such as type 2 diabetes and hypertension (Fletcher et al., 1996; Sigal et al., 2006; Thompson et al., 2003). By improving CVD risk factors that contribute to the progression of the disease, the risk of all-cause mortality from CVD can be significantly reduced (Gordon et al., 1989, Gould et al., 2007, Lee et al., 2011). While hypertension, high cholesterol, and obesity undoubtedly contribute to heart disease risk, it has been shown that low cardiorespiratory fitness may be a more powerful predictor of CVD (Blair et al., 1989; 1996). However, despite recent advances in the understanding of the beneficial effects of exercise on cardiovascular and metabolic health, the optimum exercise prescription required to elicit favourable improvements in cardiorespiratory fitness and CVD risk factors remains unclear.
High intensity interval training (HIIT) is emerging as a potential time efficient strategy for health promotion. Current recommended guidelines of 150 minutes of moderate physical activity per week is reduced by half to 75 minutes if the week’s activity is done at a vigorous intensity (ACSM, 2014). HIIT, when compared to continuous moderate intensity exercise training (CMIET), has resulted in equal or superior improvements in VO2max, insulin action and sensitivity, endothelial function, systolic blood pressure, hip and waist circumference and lipid oxidation (DiPietro et al., 2006; Franch et al., 1998; Helgerud et al., 2007; Hickson et al., 1977; MacDougall et al., 1998; Tjonna et al., 2008). The American College of Sports Medicine (ACSM) suggests considering incorporating interval training after a period of initial conditioning – typically 2-3 months - intermittently to avoid excessive orthopaedic stress (ACSM, 2014). Additionally, HIIT may require initial supervision in untrained and high risk individuals (Kessler et al., 2012), and may transiently increase the risk of cardiac events in people with underlying undiagnosed CVD (Mittleman et al., 1993). Therefore, it seems pragmatic and consistent with current recommendations to combine the two types of training to achieve the greatest positive changes in cardiovascular and metabolic health.
If Medical and health organizations are interested in advocating an ‘Exercise is Medicine’ message, health and exercise professionals need accurate information on optimal exercise volume and intensity to prescribe HIIT safely and effectively. Currently, there are no studies that have investigated the impact of performing HIIT one day per week with the combination of CMIET on cardiorespiratory fitness. Furthermore, there is limited data in the literature on the effectiveness of HIIT for overweight and/or sedentary populations (Astorino et al., 2013; Lunt et al., 2014; Sijie et al., 2012).
Therefore, we sought to compare the impact of a 12 week intervention consisting of either CMIET or CMIET combined with a single weekly bout of HIIT (CMIET + HIIT) on cardiorespiratory fitness in a group of sedentary adults at moderate risk of CVD. It was hypothesized that there would be no significant differences in the change in cardiorespiratory fitness, as measured by VO2max, between intervention groups.
Methods
Twenty nine sedentary male (n = 10) and female (n = 19) participants (36.25 ± 6.87 years, body mass 85.70 ± 17.88kgs, height 1.69 ± 0.10m) at moderate risk of CVD were recruited from the community in Auckland, New Zealand. The ACSM risk classification schema was used to risk stratify participants (ACSM, 2014). Participants with two or more positive CVD risk factors were defined as moderate risk. All participants were considered sedentary (i.e., one positive CVD risk factor) as defined elsewhere (ACSM, 2014). Participants also met at least one or more of the following positive CVD risk factors: dyslipidaemia, hypertension, impaired fasting, blood glucose, and obesity. Approval was granted by the University of Auckland Human Participants Ethics Committee (reference 7764) in accordance with international standards and all participants gave their written informed consent (Harriss and Atkinson, 2011). Participants were required to have medical clearance to exercise from a qualified medical practitioner before commencing the study. Individuals were excluded if they had known cardiovascular, metabolic and/or respiratory disease, current cigarette smokers, or unable to perform vigorous exercise.
Initially, resting heart rate (HR) was determined by the R-R interval on a 12-lead electrocardiogram (Schiller, Cardiovit AT-10, Switzerland). Participants were instructed to sit quietly in a chair for five minutes. The lowest measured HR between the fourth and fifth minute of rest was recorded as the resting HR. Participants then completed a modified-Balke, pseudo-ramp graded exercise test (GXT) on a power treadmill (Powerjog GX200, Maine). Participants were continuously monitored via a 12-lead electrocardiogram (ECG) (Schiller, Cardiovit AT-10, Switzerland) that was also used to determine exercise HR. Expired air and gas exchange data were recorded continuously during the GXT using a metabolic analyzer (Moxus, AEI technologies, PA). Before each exercise test, the metabolic analyzer was calibrated with gases of known concentrations (14.01 ± 0.07% O2, 6.00 ± 0.03% CO2) and with room air (20.93%O2 and 0.03% CO2) as per the instruction manual. Volume calibration of the pneumotachometer was done via a 3-Litre calibration syringe system (Hans-Rudolph, Kansas City, MO, USA). The last 15s of the GXT were averaged – this was considered the final data point. The closest neighbouring data point was calculated by averaging the data collected 15s immediately before the last 15s of the test. The mean of the two processed data points represented VO2max. Maximal values for all other gas exchange variables were determined in the same manner. VO2max was confirmed by the attainment of a plateau in VO2 at VO2max, maximal RER > 1.10, and maximal HR within 10 beats per minute of age-predicted maximal HR (Astorino, 2009). All participants attained at least two out of three VO2max criteria at both baseline and post-intervention. The final testing was conducted 2-3 days following the final exercise session at a similar time of day to baseline testing.
Participants in the CMIET and CMIET + HIIT groups were required to attend 5 sessions per week for 12 weeks under the direct supervision of a clinical exercise physiologist who recorded adherence, exercise workloads, and physiological responses to all sessions and in a daily training log. Energy expenditure for each training was estimated from exercise workloads using metabolic calculations published elsewhere (ACSM, 2014) and recorded in training logs. Exercise training sessions took place at different times of the day in order to best accommodate the personal/work schedules of participants. Participants in the CMIET group walked on a treadmill for 15 minutes and cycled on a cycle ergometer for 15 minutes, at an intensity of 45-60% heart rate reserve (HRR). Both the treadmill and cycle ergometer were incorporated into CMIET training sessions because exercise prescription in clinical practice typically utilizes multiple exercise modalities. Participants exercised at 45-55% HRR and 60% HRR for weeks 1-4 and 4-12, respectively. The CMIET + HIIT group performed four sessions of CMIET each week interspersed with one session of HIIT. The HIIT protocol involved eight, 60 second intervals at 100% VO2max, separated by 150 seconds active recovery. The protocol was based on previous research (Little et al., 2010) evaluating men with a high relative VO2max (46 ± 2 mL·kg-1·min-1). After four HIIT sessions, the number of repetitions increased from 8 to 10. For the last four weeks (8-12 weeks), the number of repetitions increased to 12. Recovery was held constant at 150 seconds throughout the 12 weeks. All HIIT sessions were performed on the treadmill. The control group was instructed to maintain their sedentary lifestyle and not increase physical activity levels throughout the 12 weeks.
SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) was used to determine the mean and standard deviation (mean ± SD), along with the percent change (%), for all baseline and post-intervention measures. All baseline-dependent variables and exercise training parameters were compared using general linear model (GLM) ANOVA and, where appropriate, Tukey post-hoc tests. All between-group 12-week changes were analysed using GLM-ANOVA and, where appropriate, Tukey-post hoc tests. The probability of making a type I error was set a p ≤ 0.05. Additionally, inorder to make inferences about true (population) values of the effect of both exercise interventions on cardiorespiratory fitness (i.e., VO2max), the uncertainty in effect was expressed as 90% confidence limits and as likelihoods that the true value of the effect represents a substantial and clinically meaningful change (harm or benefit). Effects were deemed unclear if its confidence interval overlapped thresholds for substantiveness (i.e., effect could be substantially positive and negative or beneficial and detrimental). All probabilistic magnitude-based inferences were calculated using a published spreadsheet (Batterham and Hopkins, 2006).
Results
Twenty nine participants (10 male and 19 female) were recruited for this study with nine individuals withdrawing (5 - change in work and/or study commitments; 2 – prolonged illness of family member; 1 – injury obtained outside study; 1 – personal reasons) from the study before completion. At baseline, all anthropometric and physiological attributes were similar (p > 0.05) across groups. After 12 weeks, changes in VO2max and all other anthropometric and physiological parameters were not (p > 0.05) significantly different in the CMIET + HIIT or CMIET groups compared with the control group. Group data (mean ± SD) for participant characteristics at baseline and post-intervention are presented in Table 1.
Table 1.
Participant charcacteristics for the CMIET + HIIT (n = 7), CMIET (n = 67) and control groups (n = 7) at baseline and post-intervention. Data are means (±SD).
| CMIET + HIIT | CMIET | Control | ||||
|---|---|---|---|---|---|---|
| Baseline | Post-Interv | Baseline | Post-Interv | Baseline | Post-Interv | |
| Age (years) | 37.9 (7.1) | - | 36.5 (9.2) | - | 34.4 (4.7) | - |
| Anthropometric | ||||||
| Height (m) | 1.68 (.1) | - | 1.73 (.1) | - | 1.67 (.1) | - |
| Body mass (kg) | 85.9 (17.3) | 85.7 (16.7) | 90.2 (25.0) | 89.1 (25.4) | 81.7 (12.5) | 82.5 (12.7) |
| BMI (kg·m-2) | 30.7 (6.3) | 30.6 (6.1) | 29.6 (4.7) | 29.4 (4.7) | 29.2 (4.2) | 29.5 (4.4) |
| Physiological measures | ||||||
| VO2REST | 3.9 (.5) | 4.0 (.8) | 4.1 (.7) | 4.0 (0.7) | 3.9 (.7) | 3.9 (.9) |
| Relative VO2max | 32.7 (9.2) | 36.0 (11.5) | 33.2 (4.0) | 34.5 (6.1) | 30.0 (4.6) | 28.3 (6.5) |
| Absolute VO2max | 2.7 (.7) | 3.0 (.7) | 3.0 (.9) | 3.1 (1.2) | 2.4 (0.4) | 2.3 (.5) |
| RERmax | 1.09 (.07) | 1.10 (.05) | 1.06 (.07) | 1.10 (0.09) | 1.13 (.03) | 1.07 (.08) |
| Ventilationmax | 77.7 (24.6) | 82.8 (21.6) | 83.5 (19.4) | 92.8 (25.1) | 72.2 (14.5) | 67.2 (17.3) |
| HRmax | 175.6 (13.4) | 180.6 (10.4) | 170.8 (8.2) | 174.5 (11.9) | 182.0 (14.8) | 180.3 (12.0) |
| HRREST | 74.7 (6.8) | 66.6 (8.0) | 73.5 (8.2) | 76.7 (4.6) | 76.9 (11.9) | 75.1 (10.2) |
| TrSpeedmax | 5.4 (1.0) | 6.0 (1.1) | 6.4 (1.0) | 6.6 (.9) | 5.6 (.6) | 5.8 (.6) |
| TrGrademax | 11.9 (2.2) | 12.9 (2.3) | 11.3 (2.0) | 11.2 (2.0) | 11.0 (1.4) | 10.3 (1.4) |
Post-Interv: Post-Intervention. VO2REST : Resting VO2 (mL·kg-1·min-1); Relative VO2max (mL·kg-1·min-1); Absolute VO2max (L·min-1); Ventilationmax: Maximal Ventilation (L·min-1); HRmax: Maximal hear rate (beat· min-1); HRREST: Resting hear rate(beat· min-1); TrSpeedmax: Maximal treadmill speed (km·hr-1); TrGrademax: Maximal treadmill grade (%).
Exercise training data were collected every session over the 12 week intervention for both exercise groups (Table 2). The exercise intervention groups were designed so both groups had similar (p > 0.05) exercise caloric expenditure, frequency, type and duration; the only major difference between the groups, was the single weekly interval training session in the CMIET + HIIT group. As illustrated in Table 2 despite the CMIET + HIIT group performing a single weekly interval training bout, relative energy expenditure for each exercise session was similar between the CMIET + HIIT and CMIET groups. Furthermore, both the CMIET + HIIT and CMIET groups had similar treadmill and cycle ergometer exercise intensities for their respective CMIET sessions. Adherence was high (> 85%) in both exercise groups for the CMIET sessions. Of note, there was 100% adherence to the interval training sessions in the CMIET + HIIT group.
Table 2.
Energy expenditure, exercise intensity and adherence for CMIET + HIIT and CMIET groups. Data are means (±SD).
| CMIET + HIIT | CMIET | ||
|---|---|---|---|
| HIIT sessions | CMIET sessions | ||
| Treadmill EE (kcal) | 146.1 (35.1) | 140.7 (31.9) | 146.8 (66.4) |
| Treadmill intensity (METs) | 9.5 (2.1) | 6.1 (1.5) | 6.2 (1.1) |
| Cycle EE (kcal) | - | 122.3 (27.1) | 126.4 (37.8) |
| Cycle intensity (METs) | - | 5.3 (1.1) | 5.3 (0.6) |
| HIIT Active recovery EE (kcal) | 102.7 (26.6) | - | - |
| Total EE (kcal) | 248.8 (57.6) | 263 (59.3) | 273.2 (63.8) |
| Relative Total EE (kcal·kg-1) | 2.9 (0.5) | 3.1 (0.6) | 3.0 (0.6) |
| Relative intensity (%HRR) | 99.1 (2.2) | 59.3 (2.1) | 60.9 (1.9) |
| Adherence (%) | 100 (0.0) | 87.5 (8.7) | 86.7 (5.9) |
EE: energy expenditure; METs: metabolic equivalents (3.5 mL·kg-1·min-1); HRR: heart rate reserve. Assumes participants walked at 3.0 km/h on a flat surface (2.7 METs) during HIIT active recovery periods.
Absolute VO2max increased by 11.1% (range: -7.5 to 26.2%) in the CMIET + HIIT group and by 3.7% (range: -12.0 to 18.4%) in the CMIET group; with a decrease of 4.2% (range: -19.1 to 12.4%) in the control group. When adjusting VO2max for any changes in body mass during the 12 week intervention, the magnitude of the changes were still similar; relative VO2max increased 10.1% in the CMIET + HIIT group and by 3.9% in the CMIET group, but decreased by 5.7% in the sedentary control group. Individual relative VO2max changes from baseline to post-intervention are illustrated in Figure 1.
Figure 1.
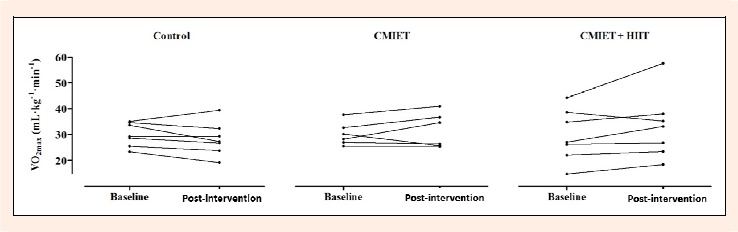
Individual changes in relative VO2max from baseline to post-intervention for control (left), CMIET (middle), and CMIET + HIIT (right) groups.
Table 3 shows the effects of exercise training on mean changes in VO2max and chances that the true differences are substantial. There were possible beneficial changes in VO2max at post-program in the CMIET + HIIT group. Likewise, there were possibly beneficial changes in VO2max at post-program in the CMIET group. However, it was ‘unclear’ if a clinically significant difference existed between the effect of CMIET + HIIT and CMIET on the change in VO2max.
Table 3.
Effect of exercise training on mean changes in VO2max and chances that the true differences are substantial.
| Chances that the true effect has substantial... | |||||
|---|---|---|---|---|---|
| Mean differences | ±90% Confidence limits | Benefit (%) | Harm (%) | Practical assessment | |
| CMIET + HIIT (relative to control) | |||||
| Relative VO2max (mL·kg-1·min-1) | 4.9 | 1.0, 8.8 | 89 | .4 | Possibly beneficial |
| Absolute VO2max (L·min-1) | .4 | .1, .6 | 91 | .3 | Possibly beneficial |
| CMIET + HIIT (relative to control) | |||||
| Relative VO2max (mL·kg-1·min-1) | 3.0 | -.5, 6.5 | 74 | 2 | Possibly beneficial |
| Absolute VO2max (L·min-1) | .2 | 0, .5 | 72 | 2 | Possibly beneficial |
| CMIET + HIIT (relative to CMIET) | |||||
| Relative VO2max (mL·kg-1·min-1) | 1.9 | -2.3, 6.2 | 48 | 5 | Unclear |
| Absolute VO2max (L·min-1) | .1 | -.2, .5 | 42 | 7 | Unclear |
If changes of benefit and harm both > 5% the true effect was deemed unclear (could be beneficial or harmful). Otherwise, chances of benefit or harm were assessed in the following manner: < 1%, almost certainly not, 1-5%, very unlikely; 5-25%, unlikely 25-75%, possibly: 75-95%, likely: 95-99%, very likely: >99%, almost certain.
Discussion
The main finding of the present study is that both a combination of CMIET + HIIT and CMIET alone are possibly beneficial training strategies for improving cardiorespiratory fitness. Although much recent research has focused on the effectiveness of HIIT, to our knowledge, this is the first study to examine how combining a single day of HIIT with CMIET may improve cardiorespiratory fitness more than CMIET alone. Given that HIIT may require a lesser time course to elicit greater improvements in cardiorespiratory fitness (Astorino et al., 2013), identification of the optimal exercise prescription for the different components of HIIT remain a crucial area of research. Our novel findings provide important preliminary evidence on the minimal threshold, with respect to HIIT training frequency (i.e., days per week), required to elicit a favourable change in cardiorespiratory fitness.
In the past decade low cardiorespiratory fitness has garnered considerable attention as an independent and powerful predictor of CVD risk and premature mortality. For example, Williams (2001) showed in a meta-analysis that there was a precipitous increase in relative risk for CVD in the lowest quartile of cardiorespiratory fitness. More recently Blair (2009) estimated that low cardiorespiratory fitness accounted for more overall deaths when compared to deaths which could be attributed to traditional CVD risk factors, such as obesity, smoking, hypertension, high cholesterol, and diabetes. In the present study cardiorespiratory fitness improved by ~1.0 MET and 0.35 METs in the CMIET + HIIT and CMIET exercise intervention groups, respectively. These improvements likely have important long-term prevention implications as a recent study reported a 1 MET increase in cardiorespiratory fitness was associated with an 18% reduction in deaths due to CVD (Barlow et al., 2012).
Relative VO2max increased 10.1% in the CMIET + HIIT group. This improvement in cardiorespiratory fitness falls within the range of what has been reported elsewhere in the literature as it pertains to the effectiveness of HIIT in previously sedentary overweight/obese adults. For instance, Sijie et al. (2012) showed an 8.4% improvement in VO2max in a cohort of overweight young women following 12 weeks of HIIT performed five sessions each week at intensities of 85% VO2max. In comparison, Astorino, Schubert et al. (2013) reported more pronounced improvements in cardiorespiratory fitness in previously sedentary women who undertook two separate chronic interval training regimens. After 12 weeks VO2max improved 22.3% in a group who performed 6-10 x 1 min interval bouts at 60-80% Wmax for 3 days each week. The second group who performed 6-10 x 1 min interval bouts at 80-90% Wmax for 3 days each week improved 21.9%. More recently, Lunt and colleagues (2014) investigated the effectiveness of 12 weeks of two forms of HIIT (aerobic interval training and maximal volitional interval training) in overweight inactive adults. The aerobic interval training exercise group performed 4 interval bouts of 4 minutes at 85-95% maximal heart rate, interspersed with 3 minutes of active recovery walking between interval bouts at 65-75% maximal heart rate, for three sessions per week. In contrast, the maximal volitional interval training group performed 3-to-6 interval bouts of 30-45 seconds at volitional maximal intensity, interspersed with 4 minutes of light active recovery walking between interval bouts, for three sessions per week. The largest improvement in VO2max was observed in the aerobic interval training exercise group at 2.1%. A likely explanation for the different VO2max improvement findings across studies may be attributable to the differences in adherence to the HIIT sessions. For example, there was 100% adherence to interval sessions in the present study and 96.4% in the study by Astorino and colleagues (2013). Conversely, adherence to interval training in the Lunt, Draper et al. (2014) investigation was considerably lower at 59% and 75% for the aerobic interval training and maximal volitional interval training groups, respectively.
Future research in this area may wish to focus on identifying the optimal frequency, intensity, time, and type (i.e., F.I.T.T) for HIIT. Similar to CMIET, where clear dose response relationships have been established (ACSM, 2014), it is highly probable comparable dose response relationships exist between various F.I.T.T. parameters of HIIT and positive cardiometabolic adaptations. For instance, the aforementioned Astorino, Schubert, et al. (2013) study showed ‘HI’ HIIT (at 80-90% Wmax) elicited more rapids gains in VO2max over the first 3 week of the exercise intervention when compared to ‘LO’ HIIT (60-80% Wmax). Additionally, the identification of the minimal threshold above which favourable training adaptations are likely to be elicited for HIIT is yet to be established. To this extent our current findings lend important preliminary evidence as we found a frequency of one day per week of HIIT, in addition to CMIET, conferred possibly beneficial clinical improvements in cardiorespiratory fitness. However, this ‘minimal threshold’ hypothesis for HIIT frequency requires further investigation with a research design (i.e., a HIIT intervention 1 day per week vs. 2 days per week) focused solely on this particular question. Moreover, additional future research may wish to focus on the minimal threshold required of HIIT factors (e.g., intensity of interval bouts, interval bouts per session, and time of each interval bout) to promote positive cardiometabolic health.
There are several limitations to the current study that warrant discussion. First, additional sample size may have resulted in a ‘more clear’ picture of possible differences in the effect between the two exercise interventions on cardiorespiratory fitness. Second, whilst participants were instructed to not change diet during the intervention, this confounder was not directly measured at either baseline or post-intervention. Last, although energy expenditure for all exercise training sessions throughout the intervention were tightly prescribed and monitored, we did not measure energy expenditure from outside physical activities which were independent of the study. It is plausible that changes in daily physical activity patterns over the course of the investigation may have influenced the results.
Conclusion
In the current study, after completion of the 12 week intervention, both exercising groups (CMIET + HIIT and CMIET) showed favourable improvements in VO2max, although it still remains ‘unclear’ whether a clinically significant difference exists between the two exercise training groups. A particularly novel aspect of the present study was the combination of a single session per week of HIIT in combination with CMIET. It is important to recognize that HIIT is a relatively new strategy of exercise training for non-athletic populations; however, additional research is needed to investigate the minimal and optimal F.I.T.T requirements of HIIT.
Biographies

Brendon ROXBURGH
Employment
Health and Performance Clinic Team Leader, The University of Auckland
Degree
MSc
Research interests
Clinical exercise physiology, high intensity interval training
E-mail: b.roxburgh@auckland.ac.nz

Paul NOLAN
Employment
Professional Teaching Fellow, The University of Auckland
Degree
MSc
Research interests
Exercise testing, cardiac rehabilitation, clinical exercise physiology
E-mail: p.nolan@auckland.ac.nz
Ryan WEATHERWAX
Employment
Lecturer, High Altitude Performance Lab manager, Western State Colorado University
Degree
MSc
Research interests
Cancer and exercise, health-related physical fitness, physiological adaptations to training
E-mail: rweatherwax@western.edu

Lance DALLECK
Employment
Assistant Professor, Western State Colorado University
Degree
PhD
Research interests
Exercise prescription, primary prevention, VO2max verification
E-mail: ldalleck@western.edu
References
- American College of Sports Medicine. (2014) ACSM’s Guidelines for exercise testing and prescription. 9th edition Lippincott Williams & Wilkins, Baltimore [Google Scholar]
- Astorino T.A., Schubert M.M., Palumbo E., Stirling D., McMillan D.W., Cooper C., Godinez J., Martinez D., Gallant R. (2013) Magnitude and time course of changes in maximal oxygen uptake in response to distinct regimens of chronic interval training in sedentary women. European Journal of Applied Physiology 113, 2361-2369 [DOI] [PubMed] [Google Scholar]
- Astorino T.A. (2009) Alterations in VO2max and the VO2 plateau with manipulation of sampling interval. Clinical Physiology and Functional Imaging 29, 60-67 [DOI] [PubMed] [Google Scholar]
- Barlow C.E., Defina L.F., Radford N.B., Berry J.D., Cooper K.H., Haskell W.L., Jones L.W., Lakoski S.G. (2012) Cardiorespiratory fitness and long-term survival in “low-risk” adults. Journal of the American Heart Association 1, e001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham A., Hopkins W. (2006) Making meaningful inferences about magnitudes. International Journal of Sports Physiology and Performance 1, 50-57 [PubMed] [Google Scholar]
- Blair S.N. (2009) Physical inactivity: The biggest public health problem of the 21st century. British Journal of Sports Medicine 43, 1-2 [PubMed] [Google Scholar]
- Blair S., Kampert J., Kohl H., Barlow C., Macera C., Paffenbarger R., Gibbons L. (1996) Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. The Journal of the American Medical Association 276, 205-210 [PubMed] [Google Scholar]
- Blair S., Kohl H., Paffenbarger R., Jr, Clark D., Cooper K., Gibbons W. (1989) Physical fitness and all-cause mortality: a prospective study of healthy men and women. The Journal of the American Medical Association 262, 2395-2401 [DOI] [PubMed] [Google Scholar]
- Boutcher S. (2010) High-intensity intermittent exercise and fat loss. Journal of Obesity 2011, 1-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiPietro L., Dziura J., Yeckel C., Neufer P. (2006) Exercise and improved insulin sensitivity in older women: evidence of the enduring benefits of higher intensity training. Journal of Applied Physiology 100, 142-149 [DOI] [PubMed] [Google Scholar]
- Dumville J., Torgerson D., Hewitt C. (2006) Research methods: reporting attrition in randomised controlled trials. British Medical Journal 332, 969-971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher G., Balady G., Blair S., Blumenthal J., Caspersen C., Chaitman B., Epstein S., Froelicher E., Froelicher V., Pina I. (1996) Statement on exercise: benefits and recommendations for physical activity programs for all Americans. Circulation 94, 857-862 [DOI] [PubMed] [Google Scholar]
- Franch J., Madsen K., Djurhuus M., Pedersen P. (1998) Improved running economy following intensified training correlates with reduced ventilatory demands. Medicine & Science in Sports & Exercise 30, 1250-1256 [DOI] [PubMed] [Google Scholar]
- Gibala M., Little J., MacDonald M., Hawley J. (2012) Physiologi-cal adaptations to low-volume, high-intensity interval training in health and disease. The Journal of Physiology 590, 1077-1084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon D., Probstfield J., Garrison R., Neaton J., Castelli W., Knoke J., Jacobs D., Bangdiwala S., Tyroler H. (1989) High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation 79, 8-15 [DOI] [PubMed] [Google Scholar]
- Gould A., Davies G., Alemao E., Yin D., Cook J. (2007) Cholesterol reduction yields clinical benefits: meta-analysis including recent trials. Clinical Therapy 29, 778-794 [DOI] [PubMed] [Google Scholar]
- Harriss D., Atkinson G. (2011) Update - ethical standards in sport and exercise science research. International Journal of Sports Medicine 32, 819-821 [DOI] [PubMed] [Google Scholar]
- Helgerud J., Hoydal K., Wang E., Karlsen T., Berg P., Bjerkaas M., Simonsen T., Helgesen C., Hjorth N., Bach R. (2007) Aerobic high-intensity intervals improve VO2max more than moderate training. Medicine & Science in Sports & Exercise 39, 665-671 [DOI] [PubMed] [Google Scholar]
- Kessler H.S., Sisson S.B., Short K.R. (2012) The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Medicine 42(6), 489-509 [DOI] [PubMed] [Google Scholar]
- Lee D., Sui X., Artero E., Lee I., Church T., McAuley P., Stanford F., Kohl H., Blair S. (2011) Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the aerobics center longitudinal study. Circulation 124, 2483-2490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little J., Safdar A., Wilkin G., Tarnopolsky M., Gibala M. (2010) A practical model of low volume high intensity interval training induces mitochondrial biogenesis in human skeletal muscle: potential mechanisms. The Journal of physiology 588, 1011-1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunt H., Draper N., Marshall H.C., Logan F.J., Hamlin M.J., Shearman J.P., Cotter J.D., Kimber N.E., Blackwell G., Frampton C.M.A. (2014) High intensity interval training in a real world setting: A randomized controlled feasibility study in overweight inactive adults, measuring change in maximal oxygen uptake. PLoS ONE 9, e83256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDougall J., Hicks A., MacDonald J., McKelvie R., Green H., Smith K. (1998) Muscle performance and enzymatic adaptations to sprint interval training. Journal of Applied Physiology 84, 2138-2142 [DOI] [PubMed] [Google Scholar]
- Sigal R., Kenny G., Wasserman D., Castaneda-Sceppa C., White R. (2006) Physical activity/exercise and type 2 diabetes. Diabetes Care 27, 2518-2539 [DOI] [PubMed] [Google Scholar]
- Sijie T., Hainai Y., Fengying Y., JianXiong W. (2012) High intensity exercise interval training in overweight young women. Journal of Sports Medicine and Physical Fitness 52, 255-262 [PubMed] [Google Scholar]
- Thompson P., Buchner D., Pina I., Balady G., Williams M., Marcus B., Berra K., Blair S., Costa F., Franklin B. (2003) Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Arteriosclerosis, Thrombosis, and Vascular Biology 107, 3109-3116 [DOI] [PubMed] [Google Scholar]
- Tjonna A., Lee S., Rognmo O., Stolen T., Bye A., Haram P., Loennechen J., Al-Share Q., Skogvoll E., Slordahl S. (2008) Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation 118, 346-354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams P.T. (2001) Physical fitness and activity as separate heart disease risk factors: A meta-analysis. Medicine & Science in Sports & Exercise 33, 754-761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization). (2012) Global atlas on cardiovascular disease prevention and control. 1st edition World Health Organization, Geneva [Google Scholar]


