Abstract
Purpose
To describe Mexican-origin youths’ trajectories of depressive symptoms from early to late adolescence and examine the role of three aspects of familism values: supportive, obligation, and referent familism.
Methods
Mexican-origin adolescents (N = 492) participated in home interviews and provided self-reports of depressive symptoms and cultural values at four assessments across an 8-year span. Using a cohort sequential design and accounting for the nesting within the 246 families (2 youth per family), we examined depressive symptoms from ages 12 to 22 years and the within-person, between-sibling, and between-family effects of familism values.
Results
Mexican-origin males’ depressive symptoms decreased across adolescence, while females’ symptoms exhibited a cubic pattern of change. Results revealed that increases in supportive and referent familism values within individuals and across families related to lower levels of depressive symptoms. Findings were most pronounced for referent familism values, as a between-sibling effect also emerged. Obligation familism values were not associated with depressive symptoms.
Conclusions
Our findings provide important descriptive information about Mexican-origin youths’ depressive symptoms and highlight the promotive role of familism values.
Keywords: Mexican-origin Adolescents, Depressive symptoms, Cultural values, Familism values, Cohort-sequential design
The emergence of depressive symptoms and depressive disorders is a concern during adolescence and early adulthood [1]. Youth with increased depressive symptoms are at risk for substance abuse [2], obesity [3], and depression in adulthood [1]. Longitudinal work suggests that adolescence is marked by important intra-individual changes in depressive symptomatology [e.g., 4, 5], and that contextual influences play a role [4]. This work, however, draws largely on European American samples [4, 5,6], with little attention to developmental changes in depressive symptoms among ethnic minority groups and the role of culture in these changes.
This study examined trajectories of depressive symptoms from ages 12 to 22 among Mexican-origin youth and the role of a salient cultural value, familism. Studying Mexican-origin youth is crucial because they are at greater risk than other ethnic and racial minority groups for depressive symptoms [7] and because Mexican-origin individuals comprise 66% of the U.S. Latino population [8]. Understanding the progression of Mexican-origin youths’ depressive symptoms and the role of cultural values during adolescence broadens our understanding of mental health symptomatology and the role of cultural beliefs among ethnic minority adolescents [9].
Trajectories of Depressive Symptoms
Adolescence is marked by numerous developmental tasks, including the formation of identity and the navigation of peer and romantic relationships, while experiencing cognitive and biological changes [10]. Difficulty negotiating these changes is theorized to contribute to greater depressive symptoms. Research on depressive symptoms across adolescence suggest that females report higher levels than males [11] and that females generally report increases in symptoms from about age 12 to 16–18 years old, whereas males report a decline or stability across this time [e.g.,4, 12]. Although the exact mechanisms underlying gender differences are not fully understood, explanations include hormonal differences during puberty, greater susceptibility and exposure to stress, and differences in interpersonal orientation [11].
Our understanding of intra-individual changes in depressive symptoms has largely been informed by studies of European American youth [4, 5, 6] or studies examining cross-cultural comparisons [13, 14]. Scholars have emphasized the need for ethnic-homogenous studies to capture within-group variability in developmental changes among ethnic minority populations [15, 16]. This is especially needed in the study of mental health during adolescence, as this period represents an important time in the development of disorders [10], and ethnic minority youth face unique challenges that are theorized to contribute to changes in symptomatology [9,16]. By first understanding normative patterns of depressive symptoms from early adolescence to young adulthood in Mexican-origin youth, we can then move to understanding deviance and resilience within an ethnic group that makes up nearly two-thirds of the largest ethnic minority group in the U.S [9].
Familism Values and Depressive Symptoms
In addition to describing developmental trajectories of depressive symptoms, it is useful to understand how cultural contexts shape development [9,16]. Mexican culture is commonly characterized by high levels of familism values, or beliefs of loyalty, reciprocity, and solidarity among family members [17]. We focus on three aspects of familism values prominent within Latino subgroups [17, 18, 19]. Supportive familism refers to the belief of dependability, unity, and emotional closeness among family members, obligation familism refers to the belief that family members have a responsibility to other family members and referent familism refers to the belief that one’s behaviors should be in line with familial expectations [17].
Familism values have received increasing attention, with the theoretical premise that these values promote positive youth development and protect individuals from developing mental health disorders [20, 21]. Empirical studies support this claim. Greater familism values have been found to relate to lower levels of aggressive behaviors [22] and substance abuse [23]. However, studies examining the link between familism values and internalizing symptoms are less consistent. Some studies suggest that familism values relate to greater depressive symptoms in particular groups [24], but other work reports no association [25, 26]. Inconsistent findings could stem from the common practice of conceptualizing all components of familism values as equally beneficial, and thus, operationalizing familism values as a unidimensional construct. Although all three subtypes of familism are interrelated, recent work suggests that familism is multifaceted, with some components being more beneficial than others, especially in relation to internalizing symptoms [19, 27, 28]. That is, components of supportive familism values relate to emotional support, while obligation familism values, and to a lesser extent referent familism values, relate to greater strain [19, 27, 28]. This limited work, however, has been conducted with adults, restricting our understanding of how components of familism values might differentially relate to adolescents’ mental health. The focus on adolescence is important given that this is a time of significant changes in individuals’ cultural values [29] and mental health symptomatology [10]. Understanding if unique components of familism values differentially relate to youths’ depressive symptoms provides insights about the promotive components of cultural values.
The Current Study
This study examined trajectories of Mexican-origin youths’ depressive symptoms from ages 12 to 22 years. We expected Mexican-origin females would increase in symptoms across early to late adolescence and males would be stable or decline. We also examined how intra-individual changes in three dimensions of familism values (i.e., obligation, supportive, and referent) related to intra-individual changes in depressive symptoms. We hypothesized that increases in supportive familism values would relate to decreases in depressive symptoms; however, we made no hypotheses regarding obligation or referent familism values given the limited knowledge of their benefits for depressive symptoms during adolescence.
Method
Participants
Data came from a longitudinal study focused on Mexican-origin family relationships and youth development [30]. The participating 246 Mexican-origin families were recruited through schools in a southwestern metropolitan area, by targeting families who had a child in 7th grade and at least one older sibling (N = 492 adolescents). A full description of the study procedures are described elsewhere [30]; key features are summarized here. To be eligible, the mother, father, and both children had to live together and agree to participate. Mothers had to self-identify as Mexican/Mexican American and be the biological mother of both participating siblings. Fathers had to be the biological or long-term adoptive father (a minimum of ten years) and had to be working at least 20 hours/week. Although not a criterion, 93% of fathers also were of Mexican descent. Time 1 (T1) data collection occurred when younger siblings were in 7th grade (Mage = 13.02, SD = .49). Time 2 (T2), Time 3 (T3), and Time 4 (T4) data were collected 2, 5, and 7 years after T1, when younger siblings were 15.10 (SD = .46), 18.18 (SD = .47), and 20.06 (SD = .56) years old, respectively. Older siblings’ data were collected at T1, T3, and T4 when older siblings averaged 15.96 (SD = 1.52), 21.11 (SD = 1.54) and 23.01 (SD = 1.54) years old, respectively.
Families ranged in socioeconomic levels, with the percentage of families meeting federal poverty guidelines at T1 (18.3%) being similar to two-parent Mexican American families in poverty in the county where the sample was drawn (i.e., 18.6%) [31]. Median household income was $40,000 (range = $3,000 to over $250,000).Adolescents were evenly split by gender and the majority were interviewed in English (83%). Forty-two percent of youth were born in Mexico; 27% were born in the U.S., but had Mexico-born parents and grandparents; 17% were U.S.-born, and had at least one U.S- born parent or grandparent, and 14% were U.S.-born and had no immediate Mexico-born family members. Parents reported 10 years of education (SD = 4.05), on average, and the majority were interviewed in Spanish (65%).
Procedures
At T1, T3, and T4, families participated in home interviews. Bilingual interviewers conducted interviews separately with each family member using laptops. At T2, only younger siblings were re-contacted and interviewed over the phone using the same procedures for in-home interviews at T1. Participating families received a $100 and $125 honorarium at T1 and T3, respectively. At T2 and T4, adolescents received payments of $40 and $75, respectively. The Institutional Review Board approved all procedures.
Measures
All measures were forward-translated to Spanish and back-translated to English [32]. Depressive symptoms were assessed using the Center for Epidemiological Studies Depression Scale [CES-D; 33]. Respondents rated the frequency that each of 20 symptoms occurred on a 4-point scale in the past month (0= Rarely or none of the time, 3 = Most of the time), with high scores indicating higher levels of depressive symptoms. Cronbach’s alphas were .85 (T1), .88 (T2), .90 (T3), and .89 (T4).
Adolescents’ familism obligation (5-items; e.g., “A person should share his/her home with relatives if they need a place to stay”), supportive (6-items; e.g., “Family provides a sense of security because they will always be there for you”), and referent (5-items; e.g., “A person should always think about their family when making important decisions”) values were measured with the Mexican American Cultural Values Scale [18]. Items were rated on a 5-point scale (1 = Strongly disagree, 5 = Strongly agree) with higher scores indicating stronger obligation, support, and referent familism values. Cronbach’s alphas were .77 (T1), .78 (T2), .76 (T3), and .74 (T4) for obligation; .77 (T1), .84 (T2), .78 (T3), and .66 (T4) for supportive familism; and .74 (T1), .74 (T2), .68 (T3), and .75 (T4) for referent familism.
Family socioeconomic status (SES) and adolescents’ generational status were included as control variables. Family SES was computed by standardizing the log of household income, and mothers’ and fathers’ education levels at T1 (α = .76). Adolescents’ generational status was scored from 0 – 7, based on a sum score in which a “1” was added for each family member born in the U.S. (i.e., adolescent, mother, father, and grandparents)[34].
Data Structure and Analytic Plan
With a cohort sequential design, we examined developmental and age-related changes in depressive symptoms. This approach allowed us to examine different age cohorts over the same period and is advantageous because short-term longitudinal data points are combined into a single longitudinal growth pattern [35]. We focused on depressive symptoms from 12 to 22 years of age because of the low number of data points after age 22. Trajectories of depressive symptoms were examined using multi-level modeling (MLM) growth models [36] in PROC MIXED in SAS 9.2. Growth models take into account the nested nature of our data and can handle missing data patterns inherent in cohort-sequential designs with maximum likelihood [37]. Given the nested data structure, we specified a 3-level growth model with occasions nested within individuals, nested within families. At Level 1, we included age polynomials (i.e., linear, quadratic, and cubic) to describe changes in depressive symptoms. Each individual’s exact age was computed by subtracting the birth date from the interview date. Age was centered at 12 years so that the intercept reflected the depressive symptom mean when adolescents were 12 years old. At Level 2, time-invariant individual characteristics that varied across siblings (i.e., adolescent gender, generational status) were included. Further, we controlled for youth age at T1 to separate longitudinal developmental changes from cross-sectional age differences. Level 3 included family SES as a covariate.
Next we examined the role of each familism dimension on trajectories of depressive symptoms. Familism values were included as time-varying predictors. Time-varying predictors were group-mean centered [38], and thus, reflected a within-person effect of familism values. A significant negative within-person familism values effect suggests that on occasions when an individual reports greater familism values than usual (compared to his/her own cross-time average), he/she also reports lower levels of depressive symptoms than usual. Given the nested structure of the data, we also examined the effect of familism between siblings and between families. Between-sibling familism predictors were group-mean centered (person cross-time mean of familism – family cross-time mean of familism) and between-family familism effects were grand-mean centered (family cross-time mean of familism – sample cross-time grand mean). A significant negative between-sibling effect suggests that when a sibling reports greater familism value than his/her sibling, he/she also reports lower depressive symptoms. Similarly, a significant negative between-family familism effect suggests that in families characterized by greater familism values, adolescents report lower depressive symptoms.
Results
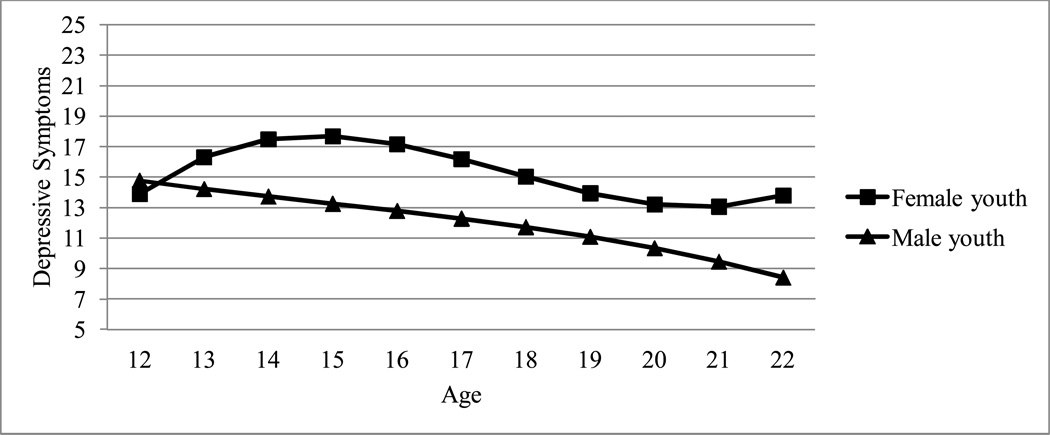
Table 1 presents the means and standard deviations for study variables (see Figure 1 for depressive symptom means). We examined mean-level differences on study variables by adolescent gender, nativity, and generational status. Females reported greater depressive symptoms [F(1,1266) = 35.08, p < .001; Mfemales = 16.74 (SD = 10.74); Mmales = 13.54, (SD = 8.25)], greater supportive familism [F(1,1214) = 10.16, p < .01; Mfemales = 4.49 (SD = 0.53); Mmales = 4.39, (SD = 0.58)] and lower referent familism [F(1,1213) = 8.58, p < .01; Mfemales = 3.98 (SD = 0.65); Mmales = 4.09, (SD = 0.62)] than males. U.S.-born youth born reported lower depressive symptoms [F(1,1266) = 5.67, p < .01; MUS = 14.66 (SD = 9.69); MMexico = 15.99, (SD = 9.76)] and greater supportive familism values [F(1,1213) = 4.22, p < .05; MUS = 4.47 (SD = .55); MMexico = 4.40, (SD = 0.57)] than Mexico-born youth. No differences were observed by generational status. An initial growth model was estimated to examine the overall trajectory of depressive symptoms. Deviance tests were conducted to determine whether variance components should be treated as random or fixed [36]. The overall growth model revealed that depressive symptoms followed a cubic growth trajectory (Table 2, Model A), that the linear term should be fixed at Level 3, and that the quadratic and cubic terms should be fixed at Levels 2 and 3. We then examined variation in depressive symptom trajectories by gender. Results revealed significant differences by gender in the linear, quadratic, and cubic terms (Table 2, Model B). Specifically, males’ trajectories followed a linear decline from 12 to 22 years old, whereas females’ trajectories followed a cubic growth pattern (see Figure 2). Differences by nativity and generational status in depressive symptoms trajectories were examined and revealed no differences.
Table 1.
Means and standard deviations (SD) of depressive symptoms (by gender) and family support, obligation, and referent values from ages 12 to 22 years.
| Depressive Symptoms | Supportive Familism | Obligation Familism | Referent Familism | N | ||
|---|---|---|---|---|---|---|
| Males | Females | Full Sample | Full Sample | Full Sample | Full Sample | |
| Age 12 | 14.79 (06.62) | 16.40 (10.64) | 4.49 (0.42) | 4.34 (0.48) | 4.15 (0.48) | 119 |
| Age 13 | 16.24 (09.03) | 17.72 (11.37) | 4.31 (0.64) | 4.18 (0.66) | 4.06 (0.70) | 131 |
| Age 14 | 14.42 (07.23) | 18.98 (10.73) | 4.55 (0.54) | 4.25 (0.62) | 4.10 (0.69) | 162 |
| Age 15 | 14.15 (08.45) | 17.76 (10.62) | 4.40 (0.70) | 4.27 (0.70) | 4.03 (0.73) | 184 |
| Age 16 | 14.31 (07.83) | 22.19 (11.55) | 4.34 (0.68) | 4.18 (0.73) | 4.00 (0.71) | 57 |
| Age 17 | 15.13 (10.01) | 15.84 (10.24) | 4.38 (0.57) | 4.22 (0.55) | 4.00 (0.63) | 90 |
| Age 18 | 11.47 (07.57) | 16.50 (11.39) | 4.35 (0.56) | 4.09 (0.54) | 3.91 (0.53) | 136 |
| Age 19 | 13.05 (08.15) | 14.94 (08.98) | 4.56 (0.41) | 4.31 (0.52) | 4.04 (0.59) | 134 |
| Age 20 | 11.11 (07.47) | 13.08 (09.81) | 4.48 (0.49) | 4.23 (0.48) | 3.99 (0.62) | 114 |
| Age 21 | 11.13 (08.87) | 14.67 (09.32) | 4.52 (0.42) | 4.28 (0.50) | 4.03 (0.65) | 80 |
| Age 22 | 10.79 (08.50) | 16.19 (12.52) | 4.41 (0.52) | 4.07 (0.63) | 4.00 (0.60) | 60 |
Note. Discrete age was used to describe the sample, such that individuals ranging from 12 – 12.99 were considered 12 years old, 13 – 13.99 were considered 13 years old, etc. Sample size (N) reflects the number of individuals providing data on depressive symptoms at each age.
Figure 1.
Observed depressive symptoms means from age 12 to 22 years old. Note that observed means were graphed based on discrete age; individuals ranging from 12 – 12.99 were considered 12 years old, 13 – 13.99 were considered 13 years old, etc.
Table 2.
MLM Growth models of males’ and females’ depressive symptoms with familism values as a within-person predictor
| Predictors | Model A: Growth Model |
Model B: Growth Model by Gender |
Model C: Supportive familism |
Model D: Obligation familism |
Model E: Referent familism |
|---|---|---|---|---|---|
| Intercept (Age 12) | 14. 367 (1.11)*** | 13.890 (1.49)*** | 14.259 (1.50)*** | 14.246 (1.51)*** | 14.332 (1.51)*** |
| Age at Time1 | 0.585 (0.20)** | 0.593 (0.19)** | 0.540 (0.19)** | 0.558 (0.19)** | 0.557 (0.19)** |
| SES at Time 1 | −1.398 (0.56)* | −1.530 (0.55)** | −0.920 (0.56)* | −1.333 (0.56)* | −1.371(0.56)* |
| Generational status | 0.117 (0.18) | 0.149 (0.18) | 0.105 (0.17) | 0.119 (0.18) | 0.103 (0.18) |
| Gender | 0.885 (2.04) | 0.214 (2.05) | 0.387 (2.06) | 0.539 (2.06) | |
| Linear Age | 1.319 (0.77)† | 3.130 (1.06)** | 2.971 (1.09)** | 2.868 (1.09)** | 2.810 (1.09)* |
| Quadratic Age | −0.365 (0.16)* | −0.754 (0.22)*** | −0.704 (0.23)** | −0.681 (0.23)** | −0.675 (0.23)** |
| Cubic Age | 0.020 (0.01)* | 0.044 (0.01)** | 0.041 (0.01)** | 0.039 (0.01)** | 0.039 (0.01)** |
| Linear X Gender | −3.712 (1.49)* | −3.167(1.53)* | −3.167 (1.54)* | −3.126 (1.54)* | |
| Quadratic X Gender | 0.793 (0.32)* | 0.656 (0.33)* | 0.657 (0.33)* | 0.645 (0.33)† | |
| Cubic X Gender | −0.048 (0.02)* | −0.040 (0.02)† | −0.040 (0.02)† | −0.039 (0.02)† | |
| Familism (Within-person) | −1.482 (0.59)* | −0.891 (0.57) | −1.246 (0.53)* | ||
| Familism (Between-siblings) | −0.639 (1.02) | −0.881 (0.91) | −2.336 (0.92)* | ||
| Familism (Between-families) | −4.428 (1.15)*** | −1.405 (1.12) | −1.925 (0.97)* | ||
| Random effects | |||||
| Level 1 residual variance | 52.086 (3.39)*** | 51.396 (3.34)*** | 53.715 (3.59)*** | 53.834 (3.60)*** | 53.843 (3.60)*** |
| Level 2 intercept variance | 37.365 (9.67)*** | 34.504 (9.40)*** | 28.401 (9.27)** | 30.161 (9.49)*** | 29.519 (9.44)*** |
| Level 2 linear slope variance | 0.577 (0.22)** | 0.603 (0.22)** | 0.475 (0.23)* | 0.494 (0.23)* | 0.477 (0.23)* |
| Level 3 intercept variance | 13.226 (3.89)*** | 14.573 (3.72)*** | 12.966 (3.61)*** | 14.823 (3.76)*** | 15.064 (3.73)*** |
Note. A 3-level growth model was specified with observations nested with 492 individuals and individuals nested within 246 families
p < .10,
p < .05,
p < .01,
p < .001.
Gender is coded 0 = Female, 1 = Male.
Figure 2.
MLM depressive symptoms trajectories from age 12 to 22 years old.
Next we examined the role of familism values, with a separate model for each component. For supportive familism values (Table 2, Model C), a significant within-person effect emerged. On occasions when individuals reported higher supportive familism values than usual (i.e., than their cross-time average), they also reported lower depressive symptoms. Similarly, a between-family effect emerged; in families characterized by greater supportive familism values, adolescents reported lower depressive symptoms. For obligation familism values (Model D), familism effects were not significant. Finally, for referent familism values (Model E), a significant within-person effect emerged; on occasions when individuals reported higher referent familism values than usual, they reported lower depressive symptoms. A significant between-sibling and between-family effect also emerged suggesting that (a) when a sibling reported greater referent familism than the other sibling, he/she also reported lower depressive symptoms and (b) in families characterized by greater referent familism values, adolescents reported lower depressive symptoms. The relation of all familism values to depressive symptoms did not differ by adolescent gender, nativity, or generational status.
Discussion
Despite evidence to suggest that Mexican-origin youth are at risk for developing depressive symptoms [7], we know little about the developmental progression of depressive symptoms and the role of cultural values in the emergence of symptoms. This group is important to examine because they make up nearly two-thirds of the most youthful and fastest growing ethnic population in the U.S. [8]. Our findings revealed changes in depressive symptoms from early adolescence to young adulthood, and differential relations between dimensions of familism values and depressive symptoms.
Trajectories of Depressive Symptoms
Mexican-origin youths’ trajectories of depressive symptoms revealed important gender differences; females’ symptoms increased from 12 to 15–16 years, decreased until 20 years, and then increased again until 22 years, while males’ symptoms declined from ages 12 to 22 years. This is consistent with prior work [4, 5, 6]; however, some unique patterns warrant further discussion. Prior work reveals age-related changes with females’ depressive symptoms increasing until around age 16–18 years, and then declining as individuals enter into their 20s [4, 5]. We found, however, that Mexican-origin females reported the highest depressive symptoms between 15 and 16 years of age, which appears to be slightly earlier than anticipated based on existing literature. Further, an increase in symptoms occurred again after the age of 20. Our findings could point to unique transitions or context changes for Mexican-origin females throughout adolescence that might be relevant for depressive symptoms. For instance, the earlier peak in Mexican-origin females’ symptoms could be associated with their earlier transition to puberty relative to European American adolescents [39]. An increase in symptoms after age 20 could be associated with transitions such as college or family formation. Studies mapping transitions and contextual changes to depressive symptom trajectories are needed to fully explain these fluctuations.
Familism Values and Depressive Symptoms
Scholars have argued for the benefits of familism values for Latino youth adjustment [20, 21]. Recent work suggests, however, that familism values are multidimensional and attention to the specific components is needed, especially in relation to internalizing symptoms [19, 27, 28]. Thus, this study examined how three components of familism values related to Mexican-origin youths’ depressive symptoms. With our design, we were able to examine within-person associations (the relation of an individual’s own fluctuations in familism values to fluctuations in an individual’s own depressive symptoms). Such an examination is a robust test of the theoretical arguments of the benefits of familism values because it takes into account an individual’s average level of familism values and links fluctuations in familism values to fluctuations in depressive symptoms. Further, it allows for the examination of between-sibling and between-family familism values effects on depressive symptoms.
Findings revealed that increases in supportive and referent familism values within individuals and across families were related to lower levels of depressive symptoms. Findings were most pronounced for referent familism values, as all three effects (i.e., within-person, between-sibling, and between-family) were significant only for this component. Together, these findings highlight the multidimensional nature of familism values and suggest adolescents’ mental health benefits from the belief in family unity, dependability, and emotional closeness, and particularly from the belief that one’s behaviors should be in line with familial expectations. From a broader perspective, supportive familism values could reflect the emotional support received from the family, while referent familism values could reflect the importance of and the degree to which an adolescent is grounded in the family. When individuals value the support and significance of their family, they benefit because they are drawing from this support and go to family when difficulties arise.
Although support and referent familism values were linked to depressive symptoms, obligation familism values were not. Limited prior work has suggested that obligation familism values have been related to greater depressive symptoms via dysfunctional thoughts and avoidant coping among adults [27, 28]. Given that adulthood could bring about new responsibilities, familism values that emphasize sacrifices and obligations could require individuals to become more involved in family responsibilities and, in turn, impact their psychological functioning. During adolescence, however, individuals may not yet experience these demands, and thus, obligation familism values may not be linked to depressive symptoms. Future research on the benefits and risks of each familism values’ component and the behaviors associated with these values across development could inform our understanding of the changing role of values.
In summary, this study provides important information about developmental changes in depressive symptoms among Mexican-origin adolescents and the role of familism values. Despite these contributions, the study has notable limitations. First, the inclusion criteria of the study, namely two-parent families, limit the generalizability of our findings to Mexican-origin adolescents in other family structures. Further, while an ethnic-homogenous design has many strengths [15], we are unable to understand how the patterns of Mexican-origin youths’ depressive symptoms compare to those of other ethnic/racial groups. Hypotheses about growth patterns in comparison to other adolescents need to be tested in larger studies. Further, we focused exclusively on cultural values. Although we know that values are a lens through which individuals perceive and organize information [40], a greater understanding of the behaviors associated with each familism value is needed. Studies focused on behavioral manifestations of values would provide insights about the processes by which familism values influence youths’ internalizing symptoms. Additionally, while the current within-person examination provided a strong test of the associations of values and depressive symptoms, we did not address issues of reciprocal causation nor did we rule out the influences of other time-varying experiences (e.g., acculturative stress, discrimination). Future studies examining how prior within-person fluctuations in values predict subsequent depressive symptoms (e.g., lagging the datasets) while also considering other time-varying sociocultural factors are needed. Finally, the cohort-sequential design facilitated the examination of changes across adolescence, but limited our examination of dyadic processes. Future studies focused on dynamic dyadic relations are needed to understand similarities and differences in depressive symptoms within families.
Despite the limitations, this study provides one of the first descriptive accounts of developmental changes in Mexican-origin youths’ depressive symptoms from early adolescence to young adulthood. Further, it broadens our understanding of Mexican-origin youths’ cultural values and contributes to the discourse of the multidimensional nature of familism values. These are integral steps in advancing our knowledge of risk and resilience in Mexican-origin youth.
Acknowledgments
We thank Ann Crouter, Mark Roosa, Nancy Gonzales, Roger Millsap, Jennifer Kennedy, Leticia Gelhard, Sarah Killoren, Melissa Delgado, Emily Cansler, Shawna Thayer, Devon Hageman, Ji-Yeon Kim, Lilly Shanahan, Chum Bud Lam, Megan Baril, Anna Solmeyer, and Shawn Whiteman for their assistance in conducting this investigation. Funding was provided by NICHD Grant R01 HD39666 (Updegraff, PI) and the Cowden Fund to the T. Denny Sanford School of Social and Family Dynamics at ASU.
Footnotes
We are grateful to the families and youth who participated in this project, and to the following schools and districts who collaborated: Osborn, Mesa, and Gilbert school districts; Willis Junior High School; Supai and Ingleside Middle Schools; St. Catherine of Siena; St. Gregory; St. Francis Xavier; St. Mary-Basha; and St. John Bosco.
Implications and Contributions: The study described changes in depressive symptoms across adolescence among the largest ethnic subgroup of the Latino population. Findings suggest that Mexican-origin youth benefit from the endorsement of supportive and referent familism values, salient in Mexican culture, furthering our knowledge of how cultural resources can promote positive adjustment during adolescence.
References
- 1.Thaper A, Collishaw S, Pine DS, et al. Depression in adolescence. Lancet. 2012;379:1056–1067. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aseltine RH, Gore S, Colten ME. The co-occurance of depression and substance abuse in late adolescence. Dev and Psychopathol. 1998;10:549–570. doi: 10.1017/s0954579498001746. [DOI] [PubMed] [Google Scholar]
- 3.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 4.Ge X, Natsuaki MN, Conger R. Trajectories of depressive symptoms and stressful life events among male and female adolescents in divorced and nondivorced families. Dev Psycholopath. 2006;18:253–273. doi: 10.1017/S0954579406060147. [DOI] [PubMed] [Google Scholar]
- 5.Peterson AC, Sarigiani PA, Kennedy RE. Adolescent depression: Why more girls? J Youth Adolesc. 1991;20:247–271. doi: 10.1007/BF01537611. [DOI] [PubMed] [Google Scholar]
- 6.Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. J Consult Clin Psychol. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- 7.Roberts RR, Roberts CR, Chen YR. Ethnocultural differences in prevalence of adolescent depression. Amer J of Comm Psychol. 1997;25:95–110. doi: 10.1023/a:1024649925737. [DOI] [PubMed] [Google Scholar]
- 8.The Pew Research Center. [Accessed December 20, 2012];Census 2010: 50 million Latinos Hispanics account for more than half of the nation’s growth in past decade. Available at: http://www.pewhispanic.org/files/reports/140.pdf.
- 9.García Coll C, Akerman A, Cicchetti D. Cultural influences on developmental processes and outcomes: Implications for the study of development and psychopathology. Dev Psychopathol. 2000;12:333–356. doi: 10.1017/s0954579400003059. [DOI] [PubMed] [Google Scholar]
- 10.Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. J Consult Clin Psychol. 2002;70:6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- 11.Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annu Rev Clin Psychol. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]
- 12.Kim J, McHale SM, Crouter AC, et al. Longitudinal linkages between sibling relationships and adjustment from middle childhood through adolescence. Dev Psychol. 2007;43:960–973. doi: 10.1037/0012-1649.43.4.960. [DOI] [PubMed] [Google Scholar]
- 13.Adkins DE, Wang V, Dupre MW. Structure and stress: Trajectories of depressive symptoms across adolescence and young adulthood. Soc Forces. 2009;88:31–60. doi: 10.1353/sof.0.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown JS, Meadows SO, Elder GH. Race-ethnic inequality and psychological distress: Depressive symptoms from adolescence to young adulthood. Dev Psychol. 2007;43:1295–1311. doi: 10.1037/0012-1649.43.6.1295. [DOI] [PubMed] [Google Scholar]
- 15.McLoyd VC. Changing demographics in the American population: Implications for research on minority children and adolescents. In: McLoyd VC, Steinberg L, editors. Studying minority adolescents: Conceptual, methodological, and theoretical issues. Mahwah, NJ: Lawrence Erlbaum; 1998. pp. 3–28. [Google Scholar]
- 16.García Coll C, Crnic K, Lamberty G, et al. An integrative model for the study of developmental competencies in minority children. Child Dev. 1996;67:1891–1914. [PubMed] [Google Scholar]
- 17.Sabogal F, Marín G, Otero-Sabogal R, et al. Hispanic familism and acculturation: What changes and what doesn’t? Hisp J Behav Sci. 1987;9:397–412. [Google Scholar]
- 18.Knight GP, Gonzales NA, Saenz DS, et al. The Mexican American cultural values scale for adolescents and adults. J Early Adolesc. 2009;30:444–481. doi: 10.1177/0272431609338178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calzada EJ, Tamis-LeMonda CS, Yoshikawa H. Familismo in Mexican and Dominican Families from low-income urban communities. J Fam Issues. 2012:1–29. [Google Scholar]
- 20.Neblett EW, Rivas-Drake D, Umaña-Taylor AJ. The promise of racial and ethnic protective factors in promoting ethnic minority youth development. Child Dev Perspect. 2012;6:295–303. [Google Scholar]
- 21.Gonzales NA, Germán M, Fabrett FC. U.S. Latino youth. In: Chang EC, Downey CA, editors. Handbook of race and development of mental health. NY: Springer; 2012. pp. 259–278. [Google Scholar]
- 22.Marsiglia FF, Parsai M, Kulis S. Effects of familism and family cohesion on problem behaviors among adolescents in Mexican immigrant families in the Southwest United States. J Ethn Cult Divers Soc Work. 2009;18:203–220. doi: 10.1080/15313200903070965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Unger JB, Ritt-Olson A, Teran L, et al. Cultural values and substance use in multiethnic sample of California adolescents. Addict Res Theory. 2002;10:257–279. [Google Scholar]
- 24.Ying U, Han M. Familism and mental health: Variation between Asian American children of refugees and immigrants. Int J Appl Psychoanal. Stud. 2007;4:333–348. [Google Scholar]
- 25.Updegraff KA, Umaña-Taylor AJ, McHale SM, et al. Mexican-origin youth’s cultural orientations and adjustment: Changes from early to late adolescence. Child Dev. 2012;83:1655–1671. doi: 10.1111/j.1467-8624.2012.01800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gonzales NA, Coxe S, Roosa MW, et al. Economic hardship, neighborhood context, and parenting: Prospective effects on Mexican-American adolescent’s mental health. Am J Community Psychol. 2009;47:98–113. doi: 10.1007/s10464-010-9366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sayegh P, Knight BG. The effects of familism and cultural justification on mental and physical health of family caregivers. J Gerontol. 2011;66B:3–14. doi: 10.1093/geronb/gbq061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Losada A, Márquez-González M, Knight BG, et al. Psychosocial factors and caregivers’ distress: Effects of familism and dysfunctional thoughts. Aging Ment Health. 2010;14:193–202. doi: 10.1080/13607860903167838. [DOI] [PubMed] [Google Scholar]
- 29.Knight GP, Jacobson RP, Gonzales NA, et al. An evaluation of the psychological research on acculturation and enculturation processes among recently immigrating populations. In: Dalla RL, Defrain J, Johnson J, Abbot DA, editors. Strengths and challenges of new immigrant families: Implications for research, education, policy and service. Lanham, MD: Lexington; 2009. pp. 9–31. [Google Scholar]
- 30.McHale SM, Updegraff KA, Shanahan L, et al. Sibling differential treatment in Mexican American families. J Marriage & Fam. 2005;67:1259–1274. doi: 10.1111/j.1741-3737.2005.00215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau. Projections of the total resident population by 5-year age groups, race, and Hispanic origin with special age categories: Middle series, 2001 to 2005. Washington, D.C: U.S. Census Bureau, Population Division; 2000. [Google Scholar]
- 32.Knight GK, Roosa MW, Umaña-Taylor AJ, editors. Studying ethnic minority and economically disadvantaged populations. Washington DC: APA; 2009. [Google Scholar]
- 33.Radloff L. The CES-D Scale: A self-report depression scale for researching the general population. Appl Psychol Meas. 1977;7:385–401. [Google Scholar]
- 34.Umaña-Taylor AJ, Fine MA. Examining ethnic identity among Mexican-origin adolescents living in the United States. Hisp J of Behav Sciences. 2004;26:36–59. [Google Scholar]
- 35.Duncan SC, Duncan TE, Hops H. Analysis of longitudinal data within accelerated longitudinal designs. Psychol Methods. 1996;1:236–248. [Google Scholar]
- 36.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Hoffman & Stawski; 2002. [Google Scholar]
- 37.Enders CK. Applied missing data analysis. New York, NY: The Guilford Press; 2010. [Google Scholar]
- 38.Singer JD, Willet JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 39.Sun SS, Schubert CM, Liang R, et al. Is sexual maturity occurring earlier among U.S. children? J Adolesc Health. 2005;37:345–55. doi: 10.1016/j.jadohealth.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 40.Kuperminc GP, Wilkins NJ, Roche C, et al. Risk, resilience, and positive development among Latino youth. In: Villarruel FA, et al., editors. Handbook of US. Latino psychology. Los Angeles, CA: Sage; 2009. pp. 213–233. [Google Scholar]