Abstract
The role of inner strength in quality of life (QOL) and self-management, primary variables in the Theory of Inner Strength, were examined with demographic and clinical characteristics in 107 women with cancer. The strongest predictors of QOL were depressive symptoms, inner strength, and time since diagnosis, respectively, accounting for 82% of the variance in QOL. When depressive symptoms were excluded due to multicollinearity, 64% of variance in QOL was explained by inner strength, time since diagnosis, and comorbidities, with inner strength the strongest predictor. The strongest predictors of self-management were depressive symptoms and inner strength, accounting for 17% of the variance. Results contribute to theory development and suggest the value of supporting inner strength to enhance QOL in cancer survivors.
Keywords: cancer, women, inner strength, Theory of Inner Strength, quality of life, self-management
The increase in cancer survival presents a challenge to expand knowledge on human responses to this chronic yet potentially fatal condition. Significant gender differences in quality of life, spiritual well-being, psychological distress, and managing the demands of illness (Ferrell, Dow, Leigh, Ly, & Gulasekaram, 1995; Matud, 2004; Sarna et al., 2005) raise the importance of inquiry into how individual strengths, such as coping strategies, developed by women cancer survivors relate to or influence their quality of life or ability to manage the challenges of their condition.
An interpretive framework can give insight into the experiences of women as they live with a chronic condition and can help identify their needs and improve health outcomes. The middle-range Theory of Inner Strength in Women (TIS) (Dingley, Bush, & Roux, 2001; Dingley, Roux, & Bush, 2000; Roux & Dingley, 2011; Roux, Dingley, & Bush, 2002) provides a framework for understanding the experiences of women who face a challenging life situation or chronic health condition such as cancer. The TIS is a middle-range theory developed inductively in a series of qualitative studies focused on women with chronic conditions, including cancer. Descriptions of women’s experiences provided rich and diverse accounts of individual strengths that facilitated growth and recovery and informed the TIS. Understanding the role of these strengths in women’s self-management of the demands of illness and QOL may assist nurses and other healthcare providers in identifying and facilitating positive coping styles and strategies for women cancer survivors.
The aim of this study was to affirm and determine the extent of the relationships among the primary concepts of the TIS—inner strength, QOL, and self-management. The TIS posits that enhanced quality of life and self-management are outcomes of inner strength. However, the theory is supported at present primarily by qualitative studies. In addition, it is not clear to what extent demographic and health status variables may relate to inner strength and its relationship with QOL and self-management. Quantitative testing to examine the relationships among the concepts of the TIS and other potentially confounding variables is needed to support its application as a foundation for theoretically based assessments and interventions. Given the sound psychometrics found in recent instrument development and testing of the Inner Strength Questionnaire (ISQ) (Lewis & Roux, 2011; Roux, Lewis, Younger, & Dingley, 2003), quantitative theory testing was deemed the reasonable next step in developing this body of research.
Cancer Survivorship
Major changes in cancer survival rates over the last three decades have led clinicians and researchers to challenge some of the prevailing research and practice related to the care of cancer survivors (Dow, 2003), who represent approximately 11.7 million Americans (American Cancer Society, 2011). Advances in the understanding of genetics, more rapid translation of basic science into practice, changes in dose-limiting toxicities, increased rates of screening and early detection, advances in rehabilitation and supportive interventions, and changes in socio-cultural factors have contributed to increases in cancer survival (Rowland, Aziz, Tesauro, & Feuer, 2001). As a result many women are living with the ongoing challenges of managing cancer.
Cancer survivorship is the health and life of persons with cancer from diagnosis until the end of life (National Cancer Institute [NCI], 2011). The current focus of cancer survivorship research is the “physical, psychosocial, and economic issues of cancer from diagnosis until the end of life” (NCI, 2011) and the promotion of health within chronic illness (Dow, 2003). The primary goal of care is to provide cancer survivors the best chance for a long and healthy life by identifying adverse effects and developing effective prevention or intervention strategies (Vaughn & Meadows, 2002), thereby decreasing suffering and increasing wellbeing. Cancer survivorship research focuses on managing health during and beyond acute diagnosis and treatment and optimizing QOL (Dow, 2003), reflecting a paradigm shift toward a chronic illness model. Meeting the challenge of health promotion within the context of chronic illness necessitates an understanding of the cancer survivor’s capacity for self-management and ways to improve quality of life as she moves through diagnosis and treatment to long-term care and survival. In an extensive study of cancer survivors sponsored by the Institute of Medicine (IOM), Hewitt, Greenfield, and Stovall (2006) suggested Survivorship Care Plans to provide a strategy for ongoing care, with specific focus on assessing psychosocial status and addressing distress. Findings from this and other studies suggest that reducing distress by enhancing adjustment to a chronic condition through active self-management of the illness can in turn positively influence both physiological and psychological health parameters, such as QOL, throughout the continuum of care and survivorship. Dow (2003) suggested that self-management outcomes such as maintaining function and general health are reflective of the positive life changes that can be part of an adaptive response to lifethreatening illness.
Theory of Inner Strength
Over the last 18 years, the Theory of Inner Strength in Women has been refined as a gender-sensitive theory applicable to women with chronic health conditions such as breast cancer, heart disease, multiple sclerosis, and organ transplants. The TIS focuses on the developmental process specific to women experiencing challenging life events such as living with chronic health conditions. Although the concept of enhancement of inner strength is not limited by ethnicity or gender, current theory development has focused on the gender-specific needs of women. The theory addresses the human response when a woman is confronted with a difficult and challenging life circumstance.
The following dimensions of the theory characterize the experience of inner strength in women:
Anguish and searching: the fear, vulnerability, and searching for meaning experienced in processing the challenging life event.
Connectedness: the nurturing of supportive relationships with self, family, friends, and a spiritual power.
Engagement: self-determinism, reframing, and engaging in possibilities.
Movement: rest, activity, honest self-appraisal of one’s abilities, and balance.
Living a new normal.
The fifth hypothesized dimension was determined through psychometric testing of the instrument and reflective analysis to be a consequence or outcome of inner strength (Roux et al., 2002, 2003; Dingley et al., 2001). The new normal was expressed in stories of new activities, relationships, understanding, sense of purpose, and a renewed faith in God or a greater source of strength. The new normal is characterized by a deep personal satisfaction experienced as a result of helping and supporting others, which in turn serves as a source of inner strength. Women who reached a new normal had completed a circle of inner strength as they now nurtured others and acknowledged that extending themselves to others became a source of strength for them. Based on the qualitative analyses, the renewal and adjustment of achieving a new normal facilitated by inner strength are hypothesized to result in improved QOL and effective self-management (Fig. 1).
Figure 1.
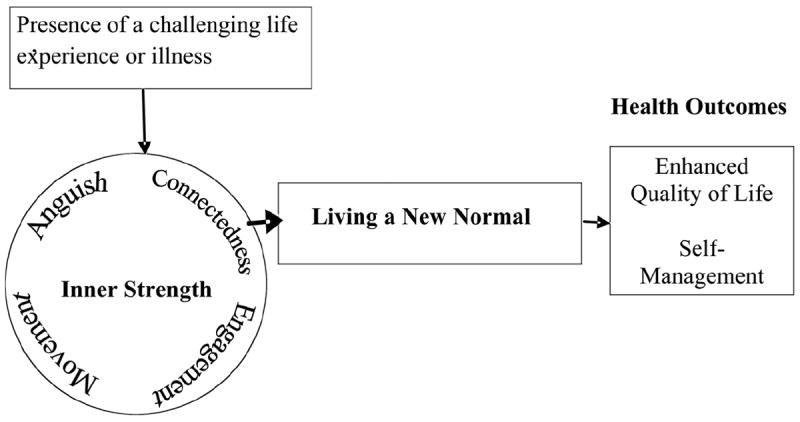
Theory of Inner Strength with dimensions
The concept of inner strength was developed from existing literature in concept analysis and metasynthesis (Dingley et al., 2000; Roux, Bush, & Dingley, 2001; Roux et al., 2002), and the theory was developed inductively in five qualitative studies and three instrument development studies by the author and colleagues. The TIS and the Inner Strength Questionnaire have been used by other scholars and researchers in a variety of settings and populations, including older mothers and adult daughters with hypertension (Shawler, Myers, Rayens, & Moser, 2012), psychoneuroimmunological stress management in breast cancer (McCain, 2004–2009), health promotion during menopause (Putnam, 2007), and living with political revolution and hardship in El Salvador (Rutherford & Parker, 2003).
In this study, the variable of inner strength was hypothesized to affect quality of life and self-management in women surviving cancer. The specific aim was to affirm and determine the extent of the relationships among inner strength, QOL, and self-management. Demographic variables and clinical health status characteristics (including depression) were examined for potential confounding effects (Fig. 2). We sought to determine the extent to which inner strength explained QOL and self-management independent of demographic, clinical, and health status characteristics.
Figure 2.
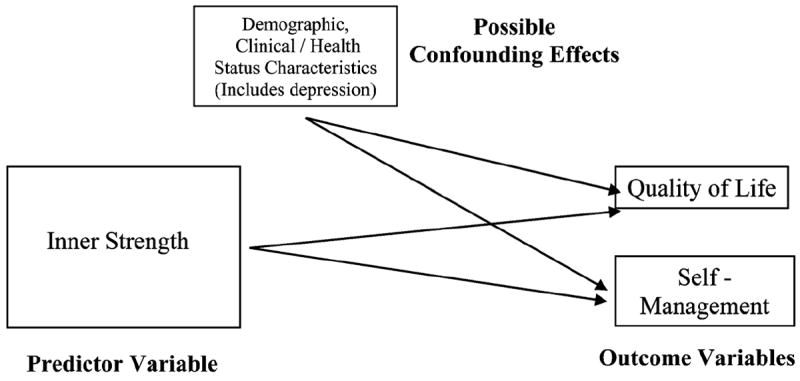
Theory of Inner Strength with confounding variables.
Methods
Design and Sample
A descriptive design was used to test the theoretical model. Two urban medical centers located in the Rocky Mountain region were the setting for this study. One was the state’s primary public safety net institution, providing approximately 42% of all unsponsored health care in the metropolitan area, with a proportionately high percentage of Hispanic cancer patients. The second site was an academic medical center providing approximately 92,000 outpatient visits annually, designated by the National Cancer Institute (NCI) as a comprehensive cancer center for the region.
Using a computer software calculator for power analysis (Lenth, 2006), a sample size of 100 for the two-tailed regression analysis was determined to provide adequate power (β=.88) based on 5 independent (predictor) variables, a standard deviation of 1.0 in the values of predictors, a variance-inflation factor (VIF) of 2.5 reflecting moderate correlation between the predictor variables, an alpha level of .05, an error SD of 1, a detectable beta of .5 (reflecting a small effect size).
Convenience sampling was used to recruit a sample of 107 women. The inclusion criteria were (a) adult women age 18 and over with a medical diagnosis of cancer; (b) time since diagnosis a minimum of 1 month; and (c) the ability to communicate in English either verbally or in writing to provide information necessary to answer survey questions.
Measures
All instruments were self-report tools completed by the study participants. Table 1 lists each variable and its measure.
Table 1. Data Collection Instruments.
| Variables | Instruments | Authors | No. of Items | Reliability (alpha) |
|---|---|---|---|---|
| Demographic/clinical/health status | 1. Demographic/clinical/health profile data form | Created for study | 22 | N/A |
| 2. CES-D (Center for Epidemiological Studies Depression scale) | Radloff (1977) | 20 | .83–.92 | |
| Inner strength | ISQ (Inner Strength Questionnaire) | Lewis & Roux (2011);Roux, Lewis, Younger, & Dingley (2003) | 27 | .86–.91 |
| Quality of life | FACT-SP (Functional Assessment of Cancer Therapy—Spirituality Well-Being) | Cella et al. (1993) Brady et al. (1999) | 35 | .85–.90 |
| Self-Management | PAM (Patient Activation Measure) | Hibbard et al. (2005) | 13 | .85–.91 |
Demographic, clinical, and health status profile
Demographic data obtained from the study participants included general information, including age, income, education, race, ethnicity, and social living status, assessed as married, single, living with a partner, divorced, or widowed. In addition, data were obtained on participants’ clinical and health status, including type and stage of cancer, length of time since diagnosis, treatments, co-morbidities, functional ability, and medications.
Depression
The Center for Epidemiological Studies Depression Scale (CES-D) (Radloff, 1977) was used to assess depressive symptomatology. The CES-D is one of the most widely used self-report instruments for epidemiologic studies of depression and has been used in primary care, psychiatric, and related clinical and forensic settings (Naughton & Wiklund, 1993; Nezu, Nezu, McClure, & Zwick, 2002; Snaith, 1993). Approximately 85% of individuals diagnosed with depression after psychiatric evaluation also have a high score on the CES-D (Radloff, 1977). The 20-item instrument measures depressive affect, somatic symptoms, positive affect, and interpersonal relations. For each experience related to depression, the respondent selects the value (0, 1, 2, or 3) that best describes how frequently the experience occurred during the previous week. Total scores of 15 to 21 indicate mild to moderate depressive symptoms; scores over 21 indicate the respondent has experienced major depressive symptoms. Cronbach alpha in this study was .90.
Inner strength
The Inner Strength Questionnaire (ISQ) (Roux et al., 2003) is a 27-item self-report instrument written at a fourth grade level (by Flesch Kincaid Grade Index). Respondents are asked to indicate their level of agreement with each item statement using a 5-point Likerttype scale (strongly agree, agree, slightly agree, disagree, strongly disagree). The ISQ assesses four factors representing dimensions of the theory (i.e., Anguish and Searching, Connectedness, Engagement, and Movement). Total scores can be calculated, as well as scores for each subscale. The maximum possible total score is 135, with higher scores indicating a higher presence of inner strength.
Following content validity testing and pilot testing on 207 community members, the psychometric properties of the ISQ were tested on women with cancer and other major chronic health conditions (Roux et al., 2003). The sample in this second testing included 154 women aged 22–83 residing in 14 states in the Midwest and Mid-Atlantic regions. The instrument was tested a third time in 281 women with a mean age of 52 years, ranging from 19 to 93 years (Roux, Lewis, Younger, & Dingley, 2004). The total variance explained by the four factors was 63%. Each sub-scale of the ISQ had a Cronbach alpha > .80 (Anguish and Searching .85, Connectedness .95, Engagement .85, and Movement .83). Internal consistency reliability of the total ISQ was α=.91. Cronbach alpha for the present study was .89.
Confirmatory factor analysis (using LISREL) validated a four-factor solution that fit the data and supported the theoretical dimensions (Lewis & Roux, 2011). Convergent and discriminant validation by Multitrait-Multimethod (MTMM) (Campbell & Fiske, 1959) analysis also was conducted. Convergent validity of the ISQ was established using the Mastery of Stress Instrument (MSI) (Younger, 1993) (r=.55; p=.01). Divergent validity of the ISQ was demonstrated using the CES-D (Radloff, 1977) (r=−.20; p=.01) and the stress subscale of the MSI (r=−.45; p=.01).
Quality of life and spiritual well-being
The tool selected to measure QOL was the Functional Assessment of Cancer Therapy—Spiritual WELL-Being (FACT-Sp), one instrument from the FACIT Measurement System, a collection of QOL questionnaires targeted at the management of chronic illness (Brady, Peterman, Fitchett, Mo, & Cella, 1999; Cella et al., 1993). The FACIT measurement system is considered appropriate for use with patients with any form of cancer as well as other chronic illness conditions (e.g., HIV/AIDS, multiple sclerosis) and in the general population using a slightly modified version. The FACT-Sp incorporates the domain of spiritual well-being (SpWB) in addition to the four primary domains of physical (PWB), social/family (SWB), emotional (EWB), and functional well-being (FWB). The SpWB scale is 12 questions that measure a sense of meaning and peace and the role of faith in illness (Peterman, Fitchett, Brady, Hernandez, & Cella, 2002). The SpWB had a Cronbach alpha of .93 in the study sample. Cronbach alphas for the subscales were PWB = .85, SWB = .80, EWB = .79, FWB = .88, and SpWB = .83.
Self-management
The Patient Activation Measure (PAM) consists of 13 statements that respondents are asked to rate in terms of their level of agreement or disagreement with each item. The responses are based on a 4-point Likert-type scale (disagree strongly, disagree, agree, agree strongly, and an N/A option). The original PAM was developed through a process of conceptualizing and then operationalizing what it means to be an activated patient, including the knowledge, skills, beliefs, and behaviors that a patient needs to self-manage a chronic illness (Hibbard, Stockard, Mahoney, & Tusler, 2004) based on the Chronic Illness Care Model (Bodenheimer, Lorig, Holman, & Grumbach, 2002). The original 22-item PAM is a unidimensional, probabilistic Guttman-like scale. Construct and criterion validity was demonstrated, as those with higher activation reported better health as measured by the SF 8, r=.38, p<.001, and had lower rates of physician office visits, ER visits, and hospital over-night stays; r=−.07, p<.01. In addition, those with higher activation were more likely to exercise, eat a healthy diet, and not smoke. Patients scoring in the upper half (>50) are learning to gain confidence in their ability to take on self-management behaviors and make lifestyle changes (Hibbard et al., 2004).
For purposes of this study and ease of administration, the short 13-item PAM was selected, based on further testing that demonstrated psychometric properties similar to the 22-item version and accounted for 92% of the variance in the original 22-item version (Hibbard, Mahoney, Stockard, & Tusler, 2005). The 13-item PAM had a Cronbach alpha of .90 in the study sample.
Data Collection
After obtaining institutional review board approval, participants were recruited from outpatient oncology treatment settings at the two primary agencies, including an outpatient oncology clinic, cancer resource center, and infusion center. Once consent was obtained, the participants were given a study survey packet to fill out in the outpatient setting. They were informed that on pilot testing in a sample of 12 women, it took approximately 12–15 minutes to complete the survey packet. After completing the surveys, the participants were instructed to place them in the accompanying envelope, seal it, and return it to the researcher directly or to a clinic staff member, who then returned the envelope to the researcher. Several participants were unable to complete the surveys at the time, but returned them directly to the researcher via US mail using a self-addressed-stamped envelope that was provided. The majority of participants recruited from the outpatient centers were able to complete the surveys at the site, as they typically remained in the clinic for several hours and had unoccupied time while receiving their chemotherapy or while waiting in the clinic or resource center.
Data Analysis
Data were entered into a computerized spreadsheet and managed and analyzed using SPSS (Statistical Package for Social Science version 14.0) (Norusis, 2002). Documentation from developers of the instruments was followed to determine participant scores and subscales.
Based on the study purpose and specific aims, data analyses consisted of descriptive, correlational, and hierarchical and stepwise multiple regression analyses. To determine the relationships among inner strength, QOL, and selfmanagement, Pearson product-moment correlations were used. The level of significance for correlations was established as p=.01 (two-tailed) to correct for the number of relationships examined. Hierarchical regression analysis was used to determine the extent to which demographic, clinical, and health status characteristics along with inner strength were related to QOL and self-management. The following predictor variables were entered: (a) demographic data (relationship status, income, age); (b) time since diagnosis and number of comorbidities; (c) CES-D scores; and (d) the ISQ total score. This order was followed in two separate analyses for the outcome (criterion) variables of QOL and self-management. Because a high level of multicollinearity was found between the CES-D and ISQ measures, each analysis was repeated without the CES-D. The level of significance was established at .025 to correct for an inflated alpha. To further examine the relationship of the components of the ISQ (inner strength) to the outcome of QOL, a stepwise regression analysis was computed using the ISQ subscales as predictor variables in place of the total ISQ score.
Results
The age of the 107 participants ranged from 20 to 83, with an average age of 56.5 years. Approximately half (56%) of the women were either married or living with a partner. The majority of participants had at least a high school education (24%, n=26), while 22% (n=24) had some college and 22% (n=24) had completed college. Though most of the women were retired or unemployed, a quarter (26%) were still working full- or part-time. Hispanic women made up 17% (n=18) of the study sample, the rest were primarily white (89%). Most of the women (69%, n=70) had been diagnosed with cancer for 36 months or less while 10% (n=10) had been diagnosed for more than 10 years. The most common cancer diagnosis was breast cancer (42%, n=43) followed by colorectal (12%, n=12) and ovarian (10%, n=10) cancer. Eighty one percent (n=85) had two or fewer additional medical conditions. High blood pressure (30%, n=31), depression/anxiety (29%, n=30), and arthritis (28%, n=29) were the most commonly occurring comorbid conditions. Table 2 provides a more detailed description of the sample participants.
Table 2. Characteristics of Participants.
| N | % | |
|---|---|---|
| Relationship status | ||
| Living with a Partner | 10 | 9.3 |
| Married | 50 | 46.7 |
| Living alone (single, widowed, divorced) | 47 | 43.9 |
| Highest education level | ||
| Junior high school | 4 | 3.7 |
| High school | 26 | 24.3 |
| Technical/some college | 31 | 28.9 |
| Completed college | 24 | 22.4 |
| Graduate education | 22 | 20.5 |
| Employment status | ||
| Full-time | 19 | 17.9 |
| Part-time | 9 | 8.5 |
| Retired | 43 | 40.6 |
| Unemployed | 35 | 33.0 |
| Race | ||
| American Indian/Alaska Native | 1 | 0.9 |
| Asian | 2 | 1.9 |
| Black or African American | 6 | 5.6 |
| Native Hawaiian or Pacific Islander | 2 | 1.9 |
| White | 96 | 89.7 |
| Ethnicity | ||
| Hispanic or Latino | 18 | 16.8 |
| Non-Hispanic or Latino | 89 | 83.2 |
| Religious preference | ||
| Catholic | 30 | 28.3 |
| Protestant | 30 | 28.3 |
| Christian (not included elsewhere) | 20 | 18.9 |
| Other | 15 | 14.1 |
| No current religious affiliation | 11 | 10.4 |
| Cancer type | ||
| Breast | 43 | 43.8 |
| Colorectal | 12 | 12.2 |
| Ovarian | 10 | 10.2 |
| Throat/neck | 8 | 8.0 |
| Lung | 6 | 6.0 |
| All other types | 19 | 19.0 |
| Current cancer stage | ||
| Stage I | 10 | 9.8 |
| Stage II | 12 | 11.8 |
| Stage III | 13 | 12.7 |
| Stage IV | 24 | 23.5 |
| Unknown | 26 | 25.5 |
| Remission | 17 | 16.7 |
| Most common treatment type (not mutually exclusive) | ||
| Chemotherapy | 96 | 89.7 |
| Radiation | 57 | 53.3 |
| Surgery related to cancer | 35 | 32.7 |
| Most common comorbid conditions | ||
| High blood pressure | 31 | 29.5 |
| Depression/anxiety | 30 | 28.6 |
| Arthritis | 29 | 27.6 |
|
|
||
| Percentile cut point
|
||
| Time since diagnosis in months | ||
| Up to 5 months | 25th | |
| Up to 14 months | 50th | |
| Up to 36 months | 75th | |
| Up to 111 months | 90th | |
| 120 to 226 months | 100th | |
The CES-D revealed 57% (n=61) of the participants did not experience symptoms of depression, 18% (n=19) experienced mild to moderate symptoms, while 25% (n=27) experienced major depressive symptoms. The findings were consistent with current literature indicating that 20–25% of women with cancer experience clinically significant depression. There was no difference in the CES-D scores by recruitment site.
Quality of life average scores were generally lower than those for females in both general and cancer populations. The subscale scores for the PWB (physical wellbeing), SWB (social well-being), EWB (emotional wellbeing), and total FACT-G (functional assessment of cancer therapy—general) were significantly lower (p<.05) in the study sample compared to the cancer population norms for females.
Self-management PAM scores were higher than in the conversion table provided by the scale developers, indicating a high average activation level. In addition, 81% (n=86) of participants scored in the upper half of the score range, indicating a high level of activation, with 10% (n=11) of participants reaching the maximum score of 100.
The mean score for the Inner Strength Questionnaire (ISQ) was 108.6 (SD=13.8), with a range of scores from 47 to 133. Seventy-five percent of participants scored in the upper third of the scale. The total and subscale scores indicated an overall strong presence of inner strength.
As shown in Table 3, significant correlations were found between inner strength and QOL, inner strength and self-management, and self-management and QOL. However, the strongest relationships were between inner strength and QOL, as demonstrated by the ISQ and FACTSp subscale correlation matrix, with weaker relationships of both inner strength and QOL with self-management (as measured by the PAM). Additionally, depressive symptoms were negatively correlated with inner strength, QOL, and self-management.
Table 3. Correlations Among Subscales of Inner Strength and Quality of Life Measures, Depressive Symptoms, and Self-Management.
| Variables | FFWB | FPWB | FSWB | FSpWB | Engage | Conn | Ang | Move | CESD | PAM |
|---|---|---|---|---|---|---|---|---|---|---|
| FEWB | .588*** | .507*** | .304** | .459*** | .480*** | .062 | .693*** | .376*** | −.645*** | .266** |
| FFWB | .691*** | .438*** | .681*** | .431*** | .068 | .438*** | .549*** | −.698*** | .464*** | |
| FPWB | .294** | .472*** | .241* | .052 | .416*** | .357*** | −.592*** | .271** | ||
| FSWB | .402*** | .290** | .141 | .237* | .459*** | −.569*** | .181 | |||
| FSpWB | .468*** | .414*** | .372*** | .385*** | −.594*** | .342*** | ||||
| Engage | .346*** | .292** | .569*** | −.491*** | .309** | |||||
| Conn | −.062 | .317** | −.067 | .015 | ||||||
| Ang | .160 | −.434*** | .164* | |||||||
| Move | −.540*** | .259** | ||||||||
| CES-D | −.307** |
Note. Subscales of the Functional Assessment of Cancer Therapy—Spiritual Well-Being; FEWB, Emotional well being; FFWB, Functional well being; FPWB, Physical well being; FSWB, Social/Family well being; FSpWB, Spiritual well being. Subscales of the Inner Strength Questionnaire: Engage, Engagement; Conn, Connectedness; Ang, Anguish/Searching; Move, Movement. CESD, Center for Epidemiological Studies Depression Scale. PAM, Patient Activation Measure.
p< .05.
p< .01.
p< .001.
Hierarchical regression for the outcome variable of QOL revealed the full model was significant, F(7,91)= 59.32, p<.001, explaining 82% of the variance in QOL. Depressive symptoms were the strongest predictor of QOL, contributing 52%. Inner strength added 13%, as much as time since diagnosis (8%) and number of co-morbidities (5%) combined. Relationship status, level of income, and age accounted for only 2% of the explained variance. In the final model, the CES-D (depressive symptoms), t(105)= −9.5, p<.001; the ISQ (inner strength), t(105)=8.2, p<.001; and time since diagnosis, t(101)=3.27, p=.002 were statistically significant predictors of QOL (Table 4).
Table 4. Final Model of Predictors of Quality of Life (as Measured by FACTSp) in Hierarchical Multiple Regression (n = 107).
| Variable | B | SE | t | p-Value |
|---|---|---|---|---|
| (Constant) | 29.620 | 13.442 | .204 | .030 |
| Age | −.036 | .094 | −.384 | .702 |
| Adequacy of Income | −.280 | 1.654 | −.173 | .863 |
| Relationship status | .346 | .915 | .378 | .706 |
| Time since diagnosis | .070 | .021 | 3.267 | .002 |
| No. of comorbidities | −.552 | .877 | −.629 | .531 |
| CES-D | −1.141 | .120 | −9.514 | <.001 |
| ISQ | .890 | .108 | 8.213 | <.001 |
Note. CESD, Center for Epidemiological Studies Depression Scale, ISQ, Inner Strength Questionnaire, FACTSp, Functional Assessment of Cancer Therapy Spiritual Well-Being.
A hierarchical regression without the CES-D also was significant, F(7,91)=27.43, p<.001, explaining 64% of the variance in QOL. ISQ (inner strength) was the strongest predictor, explaining 48% of variance in QOL. In the final model, time since diagnosis, t(101)=3.79, p=.001; number of comorbidities, t(103)=−2.41, p=.018; and the ISQ (inner strength), t(105)=11.11, p<.001, were statistically significant predictor variables. Only 14% of additional variance was explained by adding time since diagnosis and number of comorbidities to the model (Table 5). Based on the findings, a revised graphic representation of the theory (related to QOL) is presented in Figure 3.
Table 5. Final Model of Predictors of Quality of Life (as Measured by FACTSp) in Hierarchical Multiple Regression With CES-D Excluded From Analysis (n = 107).
| Variable | B | SE | t | p-Value |
|---|---|---|---|---|
| (Constant) | −45.270 | 15.304 | 2.958 | .040 |
| Age | .050 | .131 | .377 | .707 |
| Adequacy of income | −1.676 | 2.314 | −.724 | .471 |
| Relationship status | −.506 | 1.278 | −.396 | .693 |
| Time since diagnosis | .112 | .030 | 3.788 | <.001 |
| No. of comorbidities | −2.859 | 1.184 | −2.414 | .018 |
| ISQ | 1.435 | .129 | 11.116 | <.001 |
Note. CESD, Center for Epidemiological Studies Depression Scale, ISQ, Inner Strength Questionnaire, FACTSp, Functional Assessment of Cancer Therapy Spiritual Well-Being.
Figure 3.
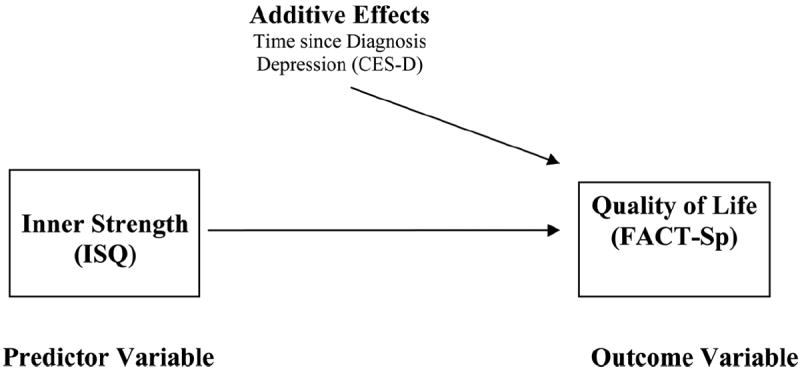
A revised Theory of Inner Strength in women with cancer, based on predictors explaining 82% of variance in quality of life.
In the hierarchical regression analysis for the outcome variable of self-management (as measured by the PAM) including depressive symptoms in the analysis, the full model was significant, F(4,94)=2.639, p=.016. However, the total variance explained by the full model was only 17%. Of the variance explained, the CES-D accounted for 12%, while the ISQ accounted for only 4%. Relationship status, income, and age accounted for 1.3%. Time since diagnosis and number of comorbidities explained less than 1% of variance. Results of the second hierarchical regression without the CES-D indicated this revised model was not significant, F(4,94)=2.38, p=.035. The full model explained 13% of variance, with the ISQ accounting for 12%.
In a stepwise regression analysis including the ISQ subscales in place of the total score, the Connectedness subscale was removed based on statistical criteria to remove from the model, leaving Engagement, Movement, and Anguish in the final model as statistically significant, F(9, 89)=25.13, p<001, accounting for 72% of variance in QOL. The Engagement subscale accounted for the larger amount of variance (37%), followed by Movement (10%) and Anguish (8%). Keeping the demographic variables (relationship status, income, age) and health status variables (time since diagnosis, number of comorbidities) constant, these covariates accounted for 4% and 13% of variance, respectively. In the final stepwise regression model, time since diagnosis, t(101)=3.89, p=.001, Engagement, t(105)=5.37, p=.001, Movement, t(105)= 5.69, p=.001, and Anguish, t(105)=4.92, p=.001 were statistically significant (Table 6).
Table 6. Final Model of Predictors of Quality of Life (as Measured by FACTSp) in Stepwise Multiple Regression With ISQ Subscales Replacing Total Score and CES-D Excluded From Analysis (n = 107).
| Variable | B | SE | t | p-Value |
|---|---|---|---|---|
| (Constant) | −59.591 | 15.70 | −3.796 | <.001 |
| Age | .118 | .122 | .968 | .336 |
| Adequacy of income | −1.208 | 2.107 | −.573 | .568 |
| Relationship status | .146 | 1.179 | .124 | .902 |
| Time since diagnosis | .105 | .027 | 3.890 | <.001 |
| No. of comorbidities | −2.436 | 1.078 | −2.259 | .026 |
| Engagement | 2.881 | .537 | 5.368 | <.001 |
| Movement | 1.810 | .318 | 5.694 | <.001 |
| Anguish/Searching | 1.304 | .265 | 4.929 | <.001 |
Note. CESD, Center for Epidemiological Studies Depression Scale, ISQ, Inner Strength Questionnaire, FACTSp, Functional Assessment of Cancer Therapy Spiritual Well-Being.
Discussion
Inner strength was among the most predictive variables for QOL in the final statistical model that included depressive symptoms and time since diagnosis. After removing depressive symptoms from the model because of the high level of multicollinearity found between the CES-D and the ISQ in the final dataset, the strongest predictors of QOL were inner strength, time since diagnosis, and number of comorbid conditions. The predictive model for self-management was also statistically significant, but this result should be interpreted with caution, as the total variance explained was limited to 17%, with depressive symptoms and inner strength the strongest predictors. Of the subscales of the ISQ, the Engagement subscale was the most predictive of QOL, followed by Movement and Anguish/Searching. Statistical models both with and without depressive symptoms were highly predictive of quality of life, consistent with the TIS.
The revised version of the TIS is consistent with literature showing that hopefulness, having purpose in life, personal relationships and support from others, and positive and spiritual changes, as well as longer time since diagnosis were associated with positive QOL scores (Ferrell et al., 1995). In contrast, depression and comorbid conditions were associated with poor QOL in cancer patients (Sarna et al., 2005). Similarly, in a study of Hurricane Katrina survivors, interview data revealed a lower prevalence of suicidality was strongly related to two dimensions of personal growth after the trauma: (a) faith in one’s ability to rebuild life, and (b) realization of inner strength (Kessler, Galea, Jones, & Parker, 2006). In a qualitative study investigating the meaning of survival and quality of life for women experiencing long-term survival of invasive breast cancer, Musick (2002) found themes of stability, resilience/hardiness, positive attitude/fighting spirit, inner strength, social support, spirituality, healing activities, and faith. In a synthesis of studies involving 1,525 cancer patients, psychological well-being was the strongest domain of QOL from both a psychometric testing standpoint and in providing insight into the personal experience of the cancer patient (Ferrell, 1996).
Though inner strength and depressive symptoms were predictors of self-management, the total variance explained was limited. Further consideration of the conceptualization of self-management is warranted prior to any additional investigation. Unclear in the literature is whether certain patient characteristics or intrinsic factors, such as inner strength, contribute to self-management over the undulating course of living with a chronic illness. Some researchers have suggested social support may be a significant factor in self-management, but studies show mixed findings (Gleeson-Kreig, Bernal & Woolley, 2002). A number of sources suggest that while self-management support and participatory decision-making are important components of the chronic illness model and chronic care, they do not appear to be well-understood or established as a dominant approach in care by health providers (Bodenheimer et al., 2002; IHI, 2012). Although the state of the science has progressed to intervention studies, a degree of clarity about the concept of self-management has been only recently established. While the use of the PAM provided a broad view of self-management in this study, more condition- specific measures may be more useful in future investigations. More powerful analysis methods also should be considered for future research, along with inclusion of a larger and more diverse sample.
Findings of this study provide further theory refinement and additional instrument validation for the Theory of Inner Strength and the Inner Strength Questionnaire, respectively.
With additional validation, the TIS may provide a framework for nursing interventions to enhance quality of life and self-management. Scholarly efforts are ongoing to explore using the items of the ISQ as a foundation for a clinical tool to assess inner strength in women and suggest possible interventions. The scholarly work of inner strength research in women holds promise for developing and implementing theoretically-based interventions for cancer survivors. Further research is being developed by the authors to test a community-based intervention to determine its effects on inner strength, and hence on quality of life and self-management in women surviving cancer.
The results of the current study support the premise that women who experience inner strength have enhanced QOL and self-management abilities. Understanding ways to facilitate inner strength may be valuable for women as they move through the recovery process and survivorship. From a practice perspective, the findings reinforce the need to focus on individual client strengths and their relationship to positive outcomes such as quality of life.
Acknowledgments
This research was supported in part by a grant from Alpha Kappa Chapter-at-Large, Sigma Theta Tau International.
Contributor Information
Catherine Dingley, Post Doctoral Research Fellow, College of Nursing, University of Utah, Salt Lake City, UT.
Gayle Roux, Professor and Associate Dean for Research and Clinical Scholarship College of Nursing, Texas Woman’s University, Denton, TX.
References
- American Cancer Society. Cancer facts and figures 2011. 2011 Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-029771.pdf.
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- Brady M, Peterman A, Fitchett G, Mo M, Cella D. A case for including spirituality in quality of life measurement in oncology. Pyscho-Oncology. 1999;8:417–428. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Campbell DT, Fiske DW. Convergent and discriminant validation by the Multitrait-Multimethod Matrix. Psychological Bulletin. 1959;56:81–101. [PubMed] [Google Scholar]
- Cella DF, Tulsky DS, Gray G, Sarafin B, Linn E, Bonomi A, Brannon J, et al. The Functional Assessment of Cancer Therapy Scale: Development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- Dingley C, Roux G, Bush H. Inner strength: A concept analysis. Journal of Theory Construction and Testing. 2000;4(2):30–35. [Google Scholar]
- Dingley CE, Bush HA, Roux G. Inner strength in women recovering from coronary artery disease: A grounded theory. Journal of Theory Construction and Testing. 2001;5(2):45–52. [Google Scholar]
- Dow KH. Challenges and opportunities in cancer survivorship research. Oncology Nursing. 2003;30:455–469. doi: 10.1188/03.ONF.455-469. [DOI] [PubMed] [Google Scholar]
- Ferrell BR, Dow KH, Leigh S, Ly J, Gulasekaram P. Quality of life in long-term cancer survivors. Oncology Nursing Forum. 1995;22:915–922. [PubMed] [Google Scholar]
- Ferrell BR. The quality of lives: 1,525 voices of cancer. Oncology Nursing Forum. 1996;23:907–916. [PubMed] [Google Scholar]
- Gleeson-Kreig J, Bernal H, Woolley S. The role of support in the self-management of diabetes mellitus among a Hispanic population. Public Health Nursing. 2002;19:215–222. doi: 10.1046/j.0737-1209.2002.19310.x. [DOI] [PubMed] [Google Scholar]
- Hewitt M, Greenfield S, Stovall E Committee on Cancer Survivorship: Improving Care and Quality of Life, Institute of Medicine and National Research Council. From cancer patient to cancer survivor—lost in transition. Washington D.C.: National Academies Press; 2006. [Google Scholar]
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Services Research. 2005;40:1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney E, Tusler M. Development of the patient activation measure (PAM): Conceptualizing and measuring activation in patients and consumers. HSR: Health Services Research. 2004;34:1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IHI. Partnering in Self-Management Support: A Toolkit for Clinicians. 2012 Retrieved from http://www.ihi.org/knowledge/Pages/Tools/SelfManagementToolkitforClinicians.aspx.
- Kessler RC, Galea S, Jones RT, Parker HA. Mental illness and suicidality after Hurricane Katrina. Bulletin of the World Health Organization. 2006;84:930–939. doi: 10.1590/S0042-96862006001200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenth RV. Java Applets for Power and Sample Size [Computer software] 2006 Retrieved from http://www.stat.uiowa.edu/~rlenth/Power.
- Lewis K, Roux G. Psychometric testing of the Inner Strength Questionnaire: Living with chronic health conditions. Applied Nursing Research. 2011;24:153–160. doi: 10.1016/j.apnr.2009.06.003. [DOI] [PubMed] [Google Scholar]
- Matud MP. Gender differences in stress and coping styles. Personality and Individual Differences. 2004;37:1401–1415. doi: 10.1016/j.paid.2004.01.010. [DOI] [Google Scholar]
- McCain N. PNI-based stress management in early breast cancer. National Cancer Institute; 2004–2009. R01#CA114718-01. [Google Scholar]
- Musick KG. Doctoral dissertation. University of Northern Colorado; 2002. Long-term survival among women with breast cancer: A multiple-case study. [Google Scholar]
- Naughton MJ, Wiklund I. A critical review of dimensionspecific measures of health related quality of life in cross-cultural research. Quality of Life Research. 1993;2:397–432. doi: 10.1007/BF00422216. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute (NCI) NCI dictionary of cancer terms. 2011 Retrieved from http://cancer.gov/definitions.
- Nezu AM, Nezu CM, McClure KS, Zwick ML. Assessment of depression. In: Gotlib I, Hammen C, editors. Handbook of depression. New York, NY: The Guilford Press; 2002. pp. 61–85. [Google Scholar]
- Norusis M. SPSS Guide to data analysis. Upper Saddle River, NJ: Prentice Hall; 2002. [Google Scholar]
- Peterman AH, Fitchett G, Brady M, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- Putnam K. Health promotion for mid-life women during menopause (Doctoral dissertation) Virginia Commonwealth University; Richmond, Virginia: 2007. [Google Scholar]
- Radloff LS. The CES-D Scale: A self- report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roux GM, Bush HA, Dingley CE. Inner strength in women with breast cancer. Journal of Theory Construction & Testing. 2001;5:19–27. [Google Scholar]
- Roux G, Dingley C. Promoting inner strength. In: Lester J, Schmitt P, editors. A personalized approach to cancer rehabilitation and survivorship. Pittsburgh, PA: Oncology Nursing Society; 2011. pp. 295–304. [Google Scholar]
- Roux GM, Dingley CE, Bush HA. Inner strength in women: Metasynthesis of qualitative findings in theory development. Journal of Theory Construction & Testing. 2002;6:19–27. [Google Scholar]
- Roux G, Lewis K, Younger J, Dingley C. Development and testing of the Inner Strength Questionnaire. Journal of Cultural Diversity. 2003;10:4–5. [PubMed] [Google Scholar]
- Roux G, Lewis K, Younger J, Dingley C. Life transition in women: Psychometric analysis of the Inner Strength Questionnaire. Proceedings of the National Congress on the State of the Science in Nursing Research; Washington, DC. 2004. Oct, [Google Scholar]
- Rowland JH, Aziz N, Tesauro G, Feuer EJ. The changing face of cancer survivorship. Seminars in Oncology Nursing. 2001;17:236–240. doi: 10.1053/sonu.2001.27912. [DOI] [PubMed] [Google Scholar]
- Rutherford MS, Parker K. Inner strength in Salvadoran women: A secondary analysis. Journal of Cultural Diversity. 2003;10:6–10. [PubMed] [Google Scholar]
- Sarna L, Cooley ME, Williams RD, Chernecky C, Padilla G, Danao LL. Quality of life and meaning of illness of women with lung cancer. Oncology Nursing Forum. 2005;32:9–19. doi: 10.1188/05.ONF.E9-E19. [DOI] [PubMed] [Google Scholar]
- Shawler C, Myers J, Rayens M, Moser D. Older mothers and adult daughters: Inner strength, health related quality of life and hypertension self-management. Proceedings of the Southern Nursing Research Society; New Orleans, LA. 2012. Feb, [Google Scholar]
- Snaith P. What do depression rating scales measure? British Journal of Psychiatry. 1993;163:293–298. doi: 10.1192/bjp.163.3.293. [DOI] [PubMed] [Google Scholar]
- Vaughn DJ, Meadows AT. Cancer survivorship research: The best is yet to come. Journal of Clinical Oncology. 2002;20:888–890. doi: 10.1200/JCO.2002.20.4.888. [DOI] [PubMed] [Google Scholar]
- Younger JB. Development and testing of the Mastery of Stress instrument. Nursing Research. 1993;42:68–73. [PubMed] [Google Scholar]


