Abstract
Background
The association between high-sensitivity C-reactive protein and recurrent major adverse cardiovascular events (MACE) in patients with ST-elevation myocardial infarction who undergo primary percutaneous coronary intervention remains controversial.
Objective
To investigate the potential association between high-sensitivity C-reactive protein and an increased risk of MACE such as death, heart failure, reinfarction, and new revascularization in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention.
Methods
This prospective cohort study included 300 individuals aged >18 years who were diagnosed with ST-elevation myocardial infarction and underwent primary percutaneous coronary intervention at a tertiary health center. An instrument evaluating clinical variables and the Thrombolysis in Myocardial Infarction (TIMI) and Global Registry of Acute Coronary Events (GRACE) risk scores was used. High-sensitivity C-reactive protein was determined by nephelometry. The patients were followed-up during hospitalization and up to 30 days after infarction for the occurrence of MACE. Student's t, Mann-Whitney, chi-square, and logistic regression tests were used for statistical analyses. P values of ≤0.05 were considered statistically significant.
Results
The mean age was 59.76 years, and 69.3% of patients were male. No statistically significant association was observed between high-sensitivity C-reactive protein and recurrent MACE (p = 0.11). However, high-sensitivity C-reactive protein was independently associated with 30-day mortality when adjusted for TIMI [odds ratio (OR), 1.27; 95% confidence interval (CI), 1.07-1.51; p = 0.005] and GRACE (OR, 1.26; 95% CI, 1.06-1.49; p = 0.007) risk scores.
Conclusion
Although high-sensitivity C-reactive protein was not predictive of combined major cardiovascular events within 30 days after ST-elevation myocardial infarction in patients who underwent primary angioplasty and stent implantation, it was an independent predictor of 30-day mortality.
Keywords: Protein C, Myocardial Infarction / mortality, Electrocardiography, Diagnosis, Prognosis
Introduction
Coronary artery disease (CAD) is a major cause of mortality worldwide. It accounted for 7 million deaths in the year of 2011, which corresponds to 11.2% of the overall mortality during that period1. Within the clinical spectrum of CAD, ST-elevation myocardial infarction (STEMI) accounts for 29%-47% cases of acute coronary syndrome (ACS)2,3. STEMI results from the rupture of an atherosclerotic plaque with superimposed coronary thrombosis in approximately 75% patients4,5.
Inflammatory responses play a key role in plaque rupture6,7. The usefulness of inflammatory markers as indicators of hidden atherosclerosis, in the improvement of risk algorithms8-12, and as predictors of the risk of recurrent events and death during ACS13-20 has been investigated. Among these markers, high-sensitivity C-reactive protein (hs-CRP) is the most extensively studied21.
When it comes to the prognosis of STEMI, there is a series of conflicting results with regard to hs-CRP22-27. Selection biases and heterogeneity of the reperfusion modalities are some of the limitations of the different studies. In the setting of primary percutaneous coronary intervention (pPCI), the data available are controversial and scarce, particularly with regard to short-term events28. Moreover, risk scores with a strong prognostic ability, particularly Thrombolysis in Myocardial Infarction (TIMI) and Global Registry of Acute Coronary Events (GRACE) scores, have been broadly used with the aim of early risk stratification29,30. However, these scores do not include inflammatory markers. This study aimed to assess the association of hs-CRP with a composite endpoint including death, reinfarction, new revascularization, and heart failure, that occurred within 30 days of the index event in patients with STEMI who underwent pPCI and stenting.
Material and Methods
Sample
The study sample was selected from patients diagnosed with STEMI according to the World Health Organization criteria who were admitted to a tertiary care hospital of interventional cardiology between 2002 and 2010. The inclusion criteria were as follows: age ≥ 18 years, both sexes, indication of pPCI and stenting, and ability to fast for at least 12 h. The exclusion criteria were as follows: history of malignancy, presence of human immunodeficiency virus (HIV) infection, presence of inflammatory disease, duration of >24 h between infarction and hospital admission, use of corticosteroid therapy, and current or recent use of nonsteroidal anti-inflammatory drugs (NSAIDs; within the last month).
Methods
This was a prospective cohort study in which each patient was first approached right after admission to the emergency room. Patients meeting the inclusion criteria, but not the exclusion criteria, were invited to participate in the study and were asked for written informed consent. After receiving consent, a complete history was taken, followed by physical examination. Patients were assessed with respect to population data (age, sex, race), the presence of risk factors for ischemic heart disease (hypertension, diabetes mellitus, dyslipidemia, cigarette smoking, family history of CAD, and obesity), and medications used. Patients with systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, those using anti-hypertensive medication, and those with a previous diagnosis of hypertension were considered hypertensive. Patients with diabetes were defined as those with a previous diagnosis of diabetes mellitus, those consuming hypoglycemic drugs, or those with fasting blood glucose ≥ 126 mg/dL before admission. Dyslipidemia was defined as serum low-density lipoprotein cholesterol (LDL-C) > 130 mg/dL, high-density lipoprotein cholestrol (HDL-C) < 40 mg/dL, triglycerides > 150 mg/dL, or a combination of these. Smokers were considered as those who currently smoked on a regular basis or those who had quit for <1 year. A positive family history was defined as a diagnosis of CAD or other atherosclerotic disease in a male first-degree relative aged < 55 years or a female first-degree relative aged < 65 years. Obesity was diagnosed on the basis of a body mass index of ≥30 kg/m2. Clinical and electrocardiographic characteristics of the infarct, TIMI and GRACE risk scores, and type of hospital care were recorded. Then, a blood sample was drawn for hs-CRP determination. The sample was collected after a 12-h fast, but no later than within the first 24 h of infarct onset. Hs-CRP was determined using the nephelometry method (Dade Behring BNTM II, Liederbach, Germany). From hospital admission to discharge, all patients were followed-up by the research team, and the occurrence of clinical complications such as arrhythmias, heart failure, reinfarction, percutaneous reintervention, coronary artery bypass grafting, and death were recorded.
The primary endpoint of the study was the combination of major adverse cardiovascular events (MACE) including death, heart failure, reinfarction, or new revascularization (whether percutaneous or surgical) within the first 30 days after the index event. Death was considered as that from all causes. The heart failure endpoint was investigated on the basis of clinical parameters suggestive of pulmonary congestion and/or signs of low cardiac output. Reinfarction was defined as angina or anginal equivalent accompanied by a new ST-segment elevation in leads consistent with those of the territory of the artery affected in the index event. New revascularization was characterized by the need for percutaneous or surgical intervention motivated by instability of the clinical picture (elective revascularization were not considered endpoints).
Thirty days after infarction, the patients were assessed in the ambulatory care section of the Institute of Cardiology so that the occurrence of any endpoint of interest could be identified.
Ethical considerations
The research project was approved by the Research Ethics Committee of the Institute of Cardiology/University Foundation of Cardiology, under protocol number 4406.09. All patients provided written informed consent.
Statistical analysis
Sample size calculation: Assuming a MACE prevalence rate of 23% (checked in a preliminary analysis of the database), with an error margin of 5% and a 95% confidence interval (95% CI), the required sample size was calculated to be at least 273 patients. Categorical variables were described as proportions, while quantitative variables were described as means and standard deviations or medians and interquartile ranges. For quantitative variables, Student's t-test or the Mann-Whitney test was used to evaluate comparisons between groups. The chi-square test was used to evaluate comparisons between categorical variables. Multiple logistic regression multivariate analysis was conducted with MACE as a dependent variable. The results of multivariate analyses were expressed as odds ratios (ORs). The significance level was set at p ≤ 0.05, and analyses were conducted using Statistical Package for the Social Sciences (SPSS) software version 19.
Results
A total of 300 patients with a mean age of 59 ± 11 years were evaluated. Most patients were male (69.3%) and Caucasian (89.8%). The most prevalent risk factor for ischemic heart disease was systemic hypertension, found in 62.2% patients. Previous conditions and procedures, as well as the medications used prior to hospitalization, are shown in Table 1.
Table 1.
Baseline patient characteristics
| Mean age (years) | 59.76 (± 11) |
| Male sex (%) | 69.3 |
| Caucasian race (%) | 89.8 |
| Risk factors (%) | |
| SAH | 62.2 |
| Cigarette smoking | 48.0 |
| FH | 44.3 |
| Dyslipidemia | 39.9 |
| Diabetes mellitus | 21.6 |
| Obesity | 18.2 |
| Most frequent previous conditions and procedures (%) | |
| AMI | 14.5 |
| Peripheral vascular disease | 7.4 |
| Gastrointestinal disease | 6.8 |
| Ischemic stroke | 5.7 |
| COPD | 3.4 |
| PCI | 11.8 |
| CABG | 3.4 |
| Medications more frequently used before the index AMI (%) | |
| ACEI | 27.0 |
| Antiplatelet drugs | 25.0 |
| Beta-blockers | 22.0 |
| Diuretics | 16.0 |
| Statins | 11.0 |
SAH: systemic arterial hypertension, FH: family history of cardiovascular disease, AMI: acute myocardial infarction, COPD: chronic obstructive pulmonary disease, PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; ACEI, angiotensin converting-enzyme inhibitors
The mean TIMI and GRACE risk scores in the sample cohort were 3.57 (standard deviation, 2.40) and 143.07 (standard deviation, 35.35), respectively. The percentage of patients assigned to Killip classification groups I, II, III, and IV were 83, 12.3, 2, and 2.7%, respectively.
The patients were divided into two groups on the basis of the year of enrollment: group 1 (137 individuals hospitalized between 2002 and 2006) and group 2 (163 patients hospitalized between 2007 and 2010). No significant difference was observed in the in-hospital use of acetylsalicylic acid, thienopyridine, angiotensin-converting enzyme inhibitors (ACEI), beta-blockers, or statins between groups.
During the first 30 days of post-infarction follow-up, 16 deaths occurred, corresponding to an overall mortality of 5.3%. In addition, 96 patients with heart failure (32.2%), one PCI procedure (0.4%), three coronary artery bypass graftings (1.1%), and ten patients with new AMI (3.3%) were identified. Recurrent MACE were observed in 104 patients (34.7%; Table 2).
Table 2.
Incidence of the most frequent endpoints 30 days after ST-elevation AMI
| Endpoints | N | Incidence (%) |
|---|---|---|
| Heart failure | 96 | 32.2 |
| Death | 16 | 5.3 |
| New AMI | 10 | 3.3 |
| CABG | 3 | 1.1 |
| New PCI | 1 | 0.4 |
| MACE | 104 | 34.7 |
AMI: acute myocardial infarction; CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention; MACE: major adverse cardiovascular events (death + heart failure + new PCI + CABG + new AMI).
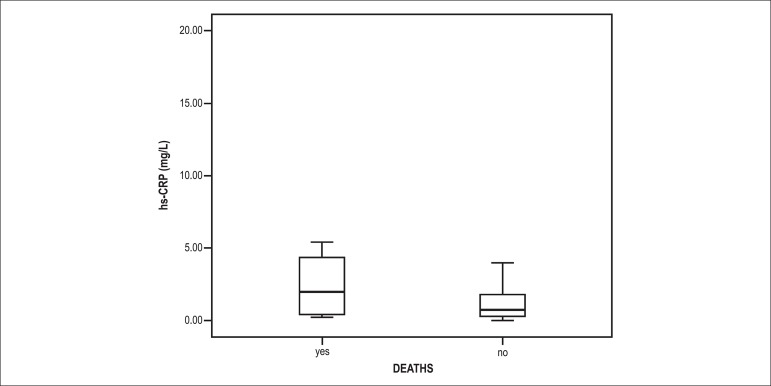
When the patients were compared with respect to the occurrence of MACE within the first 30 days after the index event, we observed a median hs-CRP of 8.0 mg/L (range, 3.7-23.5 mg/L) in the group presenting with the endpoint and 6.4 mg/L (range, 3.1-17.2 mg/L) in the remaining (p = 0.11; Table 3). Among those who developed heart failure, the median hs-CRP was 8.0 mg/L (range, 3.7-26.0 mg/L), while the median hs-CRP was 6.4 mg/L (range, 3.1-15.5 mg/L) in the group without heart failure (p = 0.057). When hs-CRP was assessed in relation to death, there was a significant association (p = 0.05; Figure 1). The causes of death and the respective hs-CRPs in each patient are shown in Table 4.
Table 3.
High-sensitivity C-reactive protein (Hs-CRP) levels and major adverse cardiovascular events (MACE) 30 days after ST-elevation acute myocardial infarction
Deaths + heart failure + new percutaneous coronary intervention + coronary artery bypass grafting + new acute myocardial infarction
values expressed as medians and interquartile ranges
Figure 1.
Bivariate analysis of high-sensitivity C-reactive protein (hs-CRP) in relation to 30-day mortality after ST-elevation acute myocardial infarction (p = 0.05)
Table 4.
Causes of death and respective hs-CRP levels
| Cases | Death cause(s) | hs-CRP (mg/L) |
|---|---|---|
| 1 | Cardiogenic and septic shock | 4.1 |
| 2 | Cardiogenic shock | 7.6 |
| 3 | Cardiogenic shock | 191.6 |
| 4 | Cardiogenic shock | 38.2 |
| 5 | Cardiogenic shock | 26.7 |
| 6 | Cardiogenic shock | 17.6 |
| 7 | Cardiogenic shock | 33.7 |
| 8 | CHF and pneumonia | 48.8 |
| 9 | Cardiogenic shock | 5.7 |
| 10 | Cardiogenic shock; contrast-induced AKI | 3.4 |
| 11 | CHF | 49.9 |
| 12 | Cardiogenic shock | 54.1 |
| 13 | Cardiogenic shock | 3.2 |
| 14 | Cardiogenic shock | 2.3 |
| 15 | Ventricular fibrillation | 22 |
| 16 | Undetermined | 4.2 |
Hs-CRP: high-sensitivity C-reactive protein; CHF: congestive heart failure; AKI: acute kidney injury
Multivariate analysis of hs-CRP in relation to all-cause mortality, after adjusting the markers for TIMI risk score (Table 5), showed an OR of 1.28 (95% CI, 1.08-1.52; p = 0.005). The OR of the TIMI score extracted from the logistic regression equation was 1.32 (95% CI, 1.09-1.59; p = 0.004) in relation to the same endpoint. On the other hand, when hs-CRP and GRACE risk scores were included in logistic regression, an independent association was found between hs-CRP and 30-day mortality (OR, 1.26; 95% CI, 1.07-1.50; p = 0.007). The OR corresponding to the GRACE score obtained from the same analysis was 1.02 (95% CI, 1.01-1.03; p = 0.002).
Table 5.
Predictors of death within 30 days after ST-elevation AMI (multivariate analysis)
| Odds ratio (95%CI) | p value | |
|---|---|---|
| hsCRP adjusted for TIMI score | 1.28 (1.08-1.52) | 0.005 |
| hsCRP adjusted for GRACE score | 1.26 (1.07-1.50) | 0.007 |
AMI: acute myocardial infarction; 95% CI: 95% confidence interval; hs-CRP: high-sensitivity C-reactive protein; TIMI: Thrombolysis in Myocardial Infarction; GRACE: Global Registry of Acute Coronary Events.
Discussion
The present study evaluated the prognostic role of hs-CRP with regard to the occurrence of 30-day recurrent MACE in patients with AMI treated with pPCI. No statistically significant association between this marker and the composite endpoint was observed. However, hs-CRP was significantly higher in patients who died within 30 days of the index event, and this association remained even after adjustment for TIMI and GRACE risk scores.
The nature of our findings is based on the hypothesis that, in individuals with AMI, the elevation of this biomarker is more attributable to the inflammatory response resulting from myocardial lesions than to vascular inflammation, unlike in individuals with unstable angina, in whom the elevation of CRP levels is associated with plaque instability and recurrent infarctions. Therefore, in patients with ACS and ST-elevation, elevated CRP levels have been related to mortality and heart failure, but not to recurrent infarctions24.
There is controversy surrounding the prognostic role of CRP in patients with STEMI. In an analysis of approximately 1000 patients with a mean follow-up of 23 months, Suleiman et al.22 verified an association between CRP and higher rates of overall mortality and heart failure after hospital discharge. Foussas et al23 found higher mortality rates within 30 days after STEMI in patients with CRP levels ≥ 5 mg/L, while the TIMI scores were the same in both groups. However, this study was initiated before the use of clopidrogel was widespread, and it did not provide information on the percentage of patients undergoing mechanical reperfusion23.
Whether the results of studies point to an association between CRP and relevant clinical endpoints24 or oppose that hypothesis25,27,31, most available evidence is based on patients receiving thrombolytic drugs. The retrospective design and failure to use the high-sensitivity method for determining CRP are also important limitations25.
In the context of STEMI treated with pPCI, the role of CRP as a prognostic marker has remained unclear. This is attributed to the paucity of evidence in this field and the disparity of information and methodological flaws present in the different publications. Tomoda and Aoki32 evaluated 234 patients with STEMI who underwent pPCI plus stenting and showed that a CRP level of ≥0.3 mg/dL was an independent predictor of a composite endpoint comprising in-hospital coronary reocclusion, reinfarction, target-vessel revascularization, and death. Limitations of this study were a retrospective design, failure to use contemporary technologies of percutaneous intervention, failure to use the high-sensitivity method to determine CRP, and failure to exclude individuals with inflammatory diseases or using antiinflamatory drugs.
In an Italian cohort comprising 758 patients, hs-CRP was associated with short-term mortality, long-term death, AMI and target-vessel revascularization33. This was also a retrospective study and was associated with a high rate of patient exclusion from the cohort (22% of the initial sample) because of the lack of CRP data on admission .
Two other studies showed an association between CRP and short-term MACE34,35. However, these studies were limited by a small sample size of 230 and 146 patients, respectively, and failure to explicitly list potential exclusion criteria, such as the use of NSAIDs and presence of inflammatory diseases. Kruk et al28 also reported that hs-CRP was predictive of in-hospital death without mentioning the exclusion criteria in their article.
Unlike the studies previously mentioned, and still in the context of PCI, Ohlmann et al36 did not show a prognostic relationship among CRP, infarct size, and mortality in a multivariate analysis. A small sample size (87 patients) and the fact that CRP was not determined using the high-sensitivity method may have influenced the results36. In turn, Damman et al37 did not include CRP in the score for the prediction of mortality in a very recent study with a significant number of patients (n = 1034) because the marker was not proven to be associated with mortality when adjusted for TIMI score variables. We should point out that, once again, concomitant inflammatory conditions were not considered and individuals in cardiogenic shock were excluded.
Our study plays an important role in the debate regarding prognosis and patient stratification because it shows an independent association between hs-CRP and a hard endpoint such as mortality. As previously mentioned, the association of CRP with clinically relevant endpoints in the setting of acute ischemic syndromes with ST-elevation has not yet reached a consensus in the literature. This was a prospective study that excluded clinical situations accompanied by an inflammatory response and the use of medications that interfere in this response, and it was conducted with all the contemporary therapeutic armamentarium38. The adjustment of hs-CRP to TIMI and GRACE risk scores29,30 provides our results with even greater consistency.
This study also has some limitations. First was its observational design. Second, it failed to establish a cut-off point for CRP level in relation to mortality. Third, it failed to use the C statistic to evaluate the prognostic accuracy of CRP in the context of STEMI because of the low frequency of this endpoint. Another limitation was the lack of hemodynamic data corresponding to coronary anatomy, which is justified by the fact that this was a fundamentally clinical study.
Conclusions
Although hs-CRP was not predictive of composite MACE within the first 30 days after acute ST-elevation myocardial infarction in patients who underwent primary angioplasty and stenting, this marker proved to be an independent predictor of all-cause mortality.
Footnotes
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conception and design of the research: Ribeiro DRP, Ramos AM, Quadros AS, Portal VL; Acquisition of data: Ribeiro DRP, Ramos AM, Vieira PL, Menti E, Bordin Jr. OL, Souza PAL; Analysis and interpretation of the data, Writing of the manuscript and Critical revision of the manuscript for intellectual content: Ribeiro DRP, Quadros AS, Portal VL; Statistical analysis: Ribeiro DRP, Portal VL.
Sources of Funding
There were no external funding sources for this study.
Study Association
This article is part of the thesis of master submitted by Daniel Rios Pinto Ribeiro, from Programa de pós-graduação de Ciências da Saúde - Cardiologia da Fundação Universitária de Cardiologia.
References
- 1.World Health Organization. (WHO) The 10 leading causes of death by broad income group. Geneva: 2011. [Access 2013 Out 10]. Available from: http://www.who.int/mediacentre/factsheets/fs310/en/index.html. [Google Scholar]
- 2.Roe MT, Parsons LS, Pollack CV, Jr, Canto JG, Barron HV, Every NR, et al. National Registry of Myocardial Infarction Investigators Quality of care by classification of myocardial infarction: treatment patterns for ST-segment elevation vs non-ST- segment elevation myocardial infarction. Arch Intern Med. 2005;165(14):1630–1636. doi: 10.1001/archinte.165.14.1630. [DOI] [PubMed] [Google Scholar]
- 3.Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, et al. The Euro Heart Survey Investigators The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27(19):2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 4.Falk E. Pathogenesis of atherosclerosis. J Am Coll Cardiol. 2006;47(8) Suppl:C7–12. doi: 10.1016/j.jacc.2005.09.068. [DOI] [PubMed] [Google Scholar]
- 5.Kubo T, Imanishi T, Takarada S, Kuroi A, Ueno S, Yamano T, et al. Assessment of culprit lesion morphology in acute myocardial infarction: ability of optical coherence tomography compared with intravascular ultrasound and coronary angioscopy. J Am Coll Cardiol. 2007;50(10):933–939. doi: 10.1016/j.jacc.2007.04.082. [DOI] [PubMed] [Google Scholar]
- 6.Ross R. Atherosclerosis: an inflammatory disease. N Engl J Med. 1999;340(2):115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 7.Weintraub HS. Identifying the vulnerable patient with rupture-prone plaque. Am J Cardiol. 2008;101(12A):3F–10F. doi: 10.1016/j.amjcard.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 8.Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297(6):611–619. doi: 10.1001/jama.297.6.611. Erratum in JAMA. 2007;297(13):1433. [DOI] [PubMed] [Google Scholar]
- 9.Zethelius B, Berglund L, Sundström J, Ingelsson E, Basu S, Larsson A, et al. Use of multiple biomarkers to improve the prediction of death from cardiovascular causes. N Engl J Med. 2008;358(20):2107–2116. doi: 10.1056/NEJMoa0707064. [DOI] [PubMed] [Google Scholar]
- 10.Ridker PM, Rifai N, Clearfield M, Downs JR, Weis SE, Miles JS, et al. Air Force/Texas Coronary Atherosclerosis Prevention Study Investigators Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med. 2001;344(26):1959–1965. doi: 10.1056/NEJM200106283442601. [DOI] [PubMed] [Google Scholar]
- 11.Blake GJ, Ridker PM, Kuntz KM. Projected life-expectancy gains with statin therapy for individuals with elevated C-reactive protein levels. J Am Coll Cardiol. 2002;40(1):49–55. doi: 10.1016/s0735-1097(02)01914-9. [DOI] [PubMed] [Google Scholar]
- 12.Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr, Kastelein JJ, et al. JUPITER Study Group Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195207–2195207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 13.Morrow DA, de Lemos JA, Sabatine MS, Wiviott SD, Blazing MA, Shui A, et al. Clinical relevance of C-reactive protein during follow-up of patients with acute coronary syndromes in the Aggrastat-to-Zocor Trial. Circulation. 2006;114(4):281–288. doi: 10.1161/CIRCULATIONAHA.106.628909. [DOI] [PubMed] [Google Scholar]
- 14.Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, et al. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994;331(7):417–424. doi: 10.1056/NEJM199408183310701. [DOI] [PubMed] [Google Scholar]
- 15.Morrow DA, Rifai N, Antman EM, Weiner DL, McCabe CH, Cannon CP, et al. C-reactive protein is a potent predictor of mortality independently of and in combination with troponin T in acute coronary syndromes: a TIMI 11A substudy. Thrombolysis in Myocardial Infarction. J Am Coll Cardiol. 1998;31(7):1460–1465. doi: 10.1016/s0735-1097(98)00136-3. [DOI] [PubMed] [Google Scholar]
- 16.Toss H, Lindahl B, Siegbahn A, Wallentin L. Prognostic influence of increased fibrinogen and C-reactive protein levels in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. Circulation. 1997;96(12):4204–4210. doi: 10.1161/01.cir.96.12.4204. [DOI] [PubMed] [Google Scholar]
- 17.Lindahl B, Toss H, Siegbahn A, Venge P, Wallentin L. Markers of myocardial damage and inflammation in relation to long-term mortality in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. N Engl J Med. 2000;343(16):1139–1147. doi: 10.1056/NEJM200010193431602. [DOI] [PubMed] [Google Scholar]
- 18.Heeschen C, Hamm CW, Bruemmer J, Simoons ML. Predictive value of C-reactive protein and troponin T in patients with unstable angina: a comparative analysis. CAPTURE Investigators. Chimeric c7E3 AntiPlatelet Therapy in Unstable angina REfractory to standard treatment trial. J Am Coll Cardiol. 2000;35(6):1535–1542. doi: 10.1016/s0735-1097(00)00581-7. [DOI] [PubMed] [Google Scholar]
- 19.Biasucci LM, Liuzzo G, Grillo RL, Caligiuri G, Rebuzzi AG, Buffon A, et al. Elevated levels of C-reactive protein at discharge in patients with unstable angina predict recurrent instability. Circulation. 1999;99(7):855–860. doi: 10.1161/01.cir.99.7.855. [DOI] [PubMed] [Google Scholar]
- 20.James SK, Armstrong P, Barnathan E, Califf R, Lindahl B, Siegbahn A, et al. GUSTO-IV-ACS Investigators Troponin and C-reactive protein have different relations to subsequent mortality and myocardial infarction after acute coronary syndrome: a GUSTO-IV substudy. J Am Coll Cardiol. 2003;41(6):916–924. doi: 10.1016/s0735-1097(02)02969-8. [DOI] [PubMed] [Google Scholar]
- 21.Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111(12):1805–1812. doi: 10.1172/JCI18921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suleiman M, Khatib R, Agmon Y, Mahamid R, Boulos M, Kapeliovich M, et al. Early Inflammation and Risk of Long-Term Development of Heart Failure and Mortality in Survivors of Acute Myocardial Infarction: Predictive Role of C-Reactive Protein. J Am Coll Cardiol. 2006;47(5):962–968. doi: 10.1016/j.jacc.2005.10.055. [DOI] [PubMed] [Google Scholar]
- 23.Foussas SG, Zairis MN, Lyras AG, Patsourakos NG, Tsirimpis VG, Katsaros K, et al. Early prognostic usefulness of C-reactive protein added to the Thrombolysis In Myocardial Infarction Risk Score in acute coronary syndromes. Am J Cardiol. 2005;96(4):533–537. doi: 10.1016/j.amjcard.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 24.Suleiman M, Aronson D, Reisner SA, Kapeliovich MR, Markiewicz W, Levy Y, et al. Admission C-reactive protein levels and 30-day mortality in patients with acute myocardial infarction. Am J Med. 2003;115(9):695–701. doi: 10.1016/j.amjmed.2003.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Nikfardjam M, Müllner M, Schreiber W, Oschatz E, Exner M, Domanovits H, et al. The association between C-reactive protein on admission and mortality in patients with acute myocardial infarction. J Intern Med. 2000;247(3):341–345. doi: 10.1046/j.1365-2796.2000.00670.x. [DOI] [PubMed] [Google Scholar]
- 26.Zebrack JS, Anderson JL, Maycock CA, Horne BD, Bair TL, Muhlestein JB, et al. Intermountain Heart Collaborative Study Group Usefulness of high-sensitivity C-reactive protein in predicting long-term risk of death or acute myocardial infarction in patients with unstable or stable angina pectoris or acute myocardial infarction. Am J Cardiol. 2002;89(2):145–149. doi: 10.1016/s0002-9149(01)02190-7. [DOI] [PubMed] [Google Scholar]
- 27.Mega JL, Morrow DA, De Lemos JA, Sabatine MS, Murphy SA, Rifai N, et al. B-type natriuretic peptide at presentation and prognosis in patients with ST-segment elevation myocardial infarction: An ENTIRE-TIMI-23 substudy. J Am Coll Cardiol. 2004;44(2):335–339. doi: 10.1016/j.jacc.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 28.Kruk M, Przyluski J, Kalinczuk L, Pregowski J, Deptuch T, Kadziela J, et al. ANIN Myocardial Infarction Registry Group Association of Non-Specific Inflammatory Activation With Early Mortality in Patients With ST-Elevation Acute Coronary Syndrome Treated With Primary Angioplasty. Circ J. 2008;72(2):205–211. doi: 10.1253/circj.72.205. [DOI] [PubMed] [Google Scholar]
- 29.Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an In TIME trial substudy. Circulation. 2000;102(17):2031–2037. doi: 10.1161/01.cir.102.17.2031. [DOI] [PubMed] [Google Scholar]
- 30.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, et al. Global Registry of Acute Coronary Events Investigators Predictors of Hospital Mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163(19):2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 31.Steg PG, Ravaud P, Tedgui A, Puel J, Moyse D, Curaudeau E, et al. ELISCOR Investigators Predischarge C-reactive protein and 1-year outcome after acute coronary syndromes. Am J Med. 2006;119(8):684–692. doi: 10.1016/j.amjmed.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 32.Tomoda H, Aoki N. Prognostic value of C-reactive protein levels within six hours after the onset of acute myocardial infarction. Am Heart J. 2000;140(2):324–328. doi: 10.1067/mhj.2000.108244. [DOI] [PubMed] [Google Scholar]
- 33.Ortolani P, Marzocchi A, Marrozzini C, Palmerini T, Saia F, Taglieri N, et al. Predictive value of high sensitivity C-reactive protein in patients with ST-elevation myocardial infarction treated with percutaneous coronary intervention. Eur Heart J. 2008;29(10):1241–1249. doi: 10.1093/eurheartj/ehm338. [DOI] [PubMed] [Google Scholar]
- 34.Magadle R, Hertz I, Merlon H, Weiner P, Mohammedi I, Robert D. The relation between preprocedural C-reactive protein levels and early and late complications in patients with acute myocardial infarction undergoing interventional coronary angioplasty. Clin Cardiol. 2004;27(3):163–168. doi: 10.1002/clc.4960270314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yip HK, Hang CL, Fang CY, Hsieh YK, Yang CH, Hung WC, et al. Level of high-sensitivity C-reactive protein is predictive of 30-day outcomes in patients with acute myocardial infarction undergoing primary coronary intervention. Chest. 2005;127(3):803–808. doi: 10.1378/chest.127.3.803. [DOI] [PubMed] [Google Scholar]
- 36.Ohlmann P, Jaquemin L, Morel O, El Behlgiti R, Faure A, Michotey MO, et al. Prognostic value of C-reactive protein and cardiac troponin I in primary percutaneous interventions for ST-elevation myocardial infarction. Am Heart J. 2006;152(6):1161–1167. doi: 10.1016/j.ahj.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 37.Damman P, Beijk MA, Kuijt WJ, Verouden NJ, van Geloven N, Henriques JP, et al. Multiple biomarkers at admission significantly improve the prediction of mortality in patients undergoing primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2011;57(1):29–36. doi: 10.1016/j.jacc.2010.06.053. [DOI] [PubMed] [Google Scholar]
- 38.Boden WE, Eagle K, Granger CB. Reperfusion strategies in acute ST-segment elevation myocardial infarction: a comprehensive review of contemporary management options. J Am Coll Cardiol. 2007;50(10):917–929. doi: 10.1016/j.jacc.2007.04.084. [DOI] [PubMed] [Google Scholar]