Abbreviation list
BMS - Bare metal stent
BVS - Bioresorbable vascular scaffold
DES - Drug-eluting stent
ISR - In-stent restenosis
LAD - Left anterior descending
OCT - Optical coherence tomography
PCI - Percutaneous coronary intervention
Introduction
Bioresorbable vascular scaffolds (BVS) demonstrate favourable outcomes in patients with stable coronary disease with simple de novo coronary lesions1,2 and are considered the "fourth revolution" in percutaneous coronary intervention (PCI) technology. BVS represent a promising alternative to drug-eluting stents (DES) while offering the same advantages. We present the first case of in-stent restenosis (ISR) successfully treated with an everolimus-eluting BVS (ABSORB; Abbott Vascular, Santa Clara, CA) and discuss its potential advantages in such lesion.
Case Report
A 72-year-old male presented with a 3-week history of relapsing Canadian Cardiovascular Society class 3/4 angina. He had undergone PCI of the proximal left anterior descending (LAD) 4 years prior using a 2.75 x 18 mm sirolimus-eluting stent (Cypher Cordis, Miami, FL). His medical regimen included aspirin and a statin. Resting ECG and cardiac biomarkers were normal. Given the severity of his symptoms and his past medical history, it was decided to proceed directly to coronary angiography.
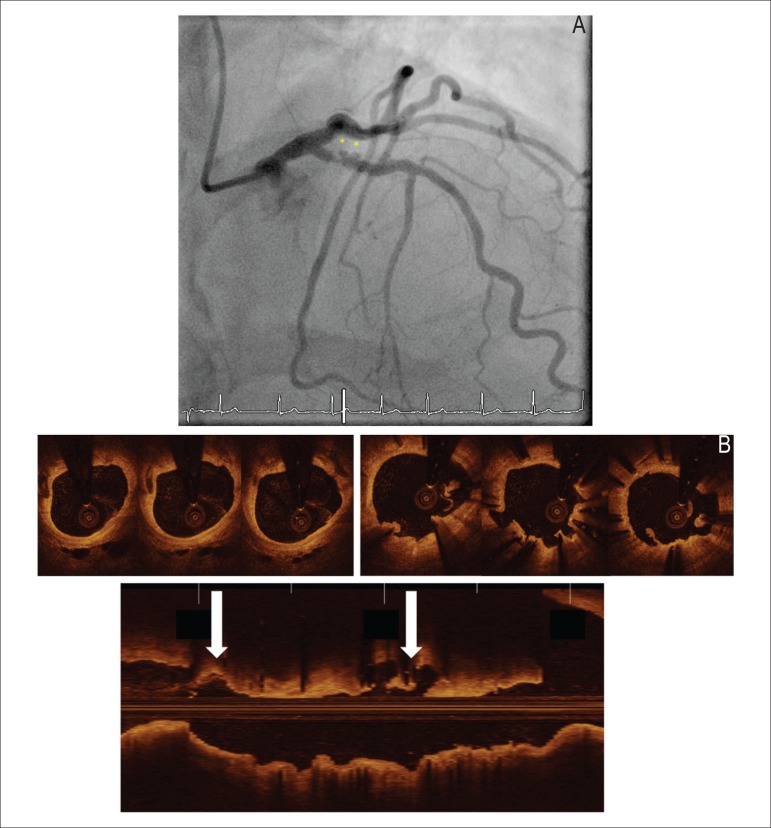
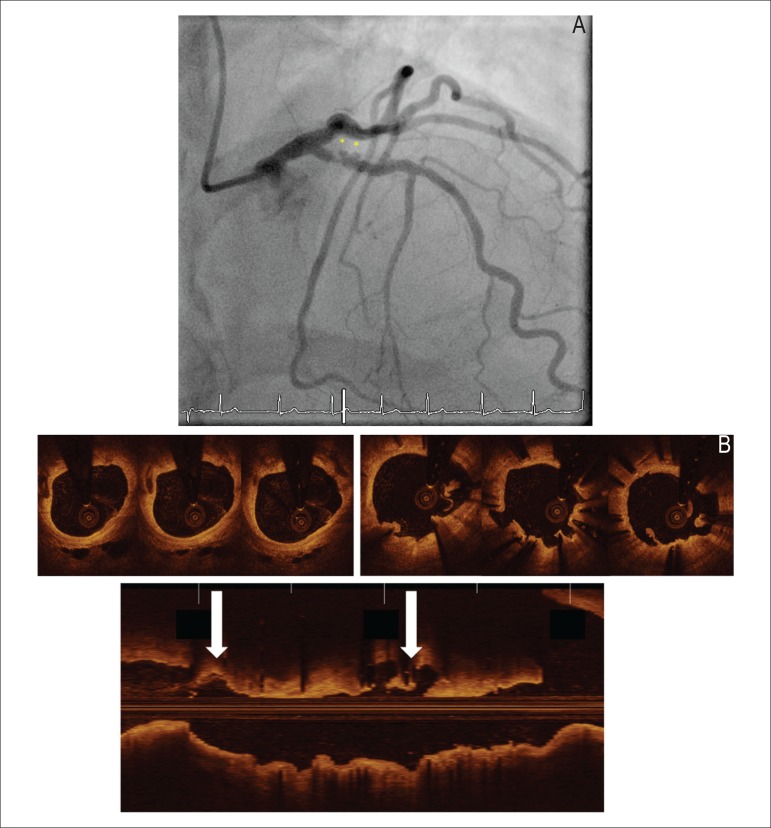
The coronary angiogram showed a severe 95% ISR lesion of the proximal LAD with thrombus and multiple areas of contrast staining outside the stent contour, compatible with coronary micro-aneurysms (Figure 1A). Thromboaspiration revealed white thrombus. Optical coherence tomography (OCT) was compatible with a localized hypersensitivity reaction to first-generation DES (Figure 1B). After consensus with the referring physician, an ABSORB everolimus-eluting BVS 3.0 x 18 mm was deployed (Figure 2A). Repeated OCT showed good scaffold apposition and coverage of the micro-aneurysms (Figure 2B). The patient was discharged the following day on dual antiplatelet therapy with aspirin and ticagrelor. The patient was asymptomatic at 6 months clinical follow-up.
Figure 1.
Baseline Angiogram and Optical Coherence Tomography
(A) Baseline angiogram showing a severe restenotic lesion of the proximal left anterior descending artery with 2 micro-aneurysms (asterisk), with contrast staining outside the previously implanted drug-eluting stent suggesting late-acquired malapposition secondary to hypersensitivity vasculitis. (B) Optical coherence tomography performed after initial thrombectomy and balloon dilatation angioplasty showing typical late acquired malapposition features with “sunflower” appearance (top right panel) and 2 small pockets representing micro-aneurysms (asterisk; lower panel).
Figure 2.
Post PCI Angiogram and Optical Coherence Tomography
(A) Final coronary angiography showing exclusion of the 2 micro-aneurysms present at baseline. (B) Final optical coherence tomography showing good BVS apposition with covering of the 2 micro-aneurysms and thrombus entrapment.
Discussion
To the best of our knowledge, this is the first report describing the use of a BVS in a case of ISR and late acquired malapposition secondary to first-generation DES. The ABSORB BVS consists of resorbable polymers containing the antiproliferative drug everolimus. Prospective studies of BVS showed favourable outcomes in simple, de novo coronary lesions1,2, with long-term positive vessel remodelling, late lumen enlargement, complete resorption of the vascular scaffold, and progressive filling of the previously occupied space with proteoglycans at follow-up3. However, these studies specifically excluded ISR lesions.
In the current report, a local delayed hypersensitivity vasculitis caused by a sirolimus-eluting stent was suspected to be the causal mechanism leading to late acquired stent malapposition, restenosis, with superimposed very late thrombosis4. Typical angiographic findings present in our patient, including positive remodelling and micro-aneurysms of the mid-segment of the stent. This hypersensitivity reaction has been attributed to the polymer coating of sirolimus-eluting stents, which, importantly, differs from the one used in the ABSORB BVS4.
In this particular case, the use of BVS had several advantages: avoidance of accumulation of multiple layers of metallic stent, avoidance of re-exposure to the same "allergic antigen" and most importantly, hypothetically, the healing process of BVS characterized by late lumen enlargement and replacement of the platform by proteoglycans, resulting in filling of the micro-aneurysms and exclusion of the nidus involved in the genesis of neo-thrombi. Angiographic follow-up with OCT imaging at 2 years or beyond will potentially validate the latest hypothesis.
Conclusion
BVS are a promising addition to the PCI arsenal in managing complex coronary lesions. This case report demonstrates novel use of this technology to treat an ISR lesion of DES characterized by late acquired malapposition.
Footnotes
Potential Conflict of Interest
The author Erick Schampaert has conflict with Abbott Vascular Consultant and Philippe Genereux has conflict with Abbott Vascular Speaker Fee.
Author contributions
Cadrin-Tourigny J and Dong L, conception and design of the research, acquision of data, analysis and interpretation of the data, statistical analysis, writing of the manuscript and critical revision of the manuscript for intellectual content; Maehara A, conception and design of the research, acquision of data, analysis and interpretation of the data, obtaining financing, writing of the manuscript, critical revision of the manuscript for intellectual content; Schampaert E and Genereux P, conception and design of the research, acquision of data, analysis and interpretation of the data, writing of the manuscript, critical revision of the manuscript for intellectual content.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Ormiston JA, Serruys PW, Regar E, Dudek D, Thuesen L, Webster MW, et al. A bioabsorbable everolimus-eluting coronary stent system for patients with single de-novo coronary artery lesions (ABSORB): a prospective open-label trial. Lancet. 2008;371(9616):899–907. doi: 10.1016/S0140-6736(08)60415-8. [DOI] [PubMed] [Google Scholar]
- 2.Serruys PW, Onuma Y, Ormiston JA, de Bruyne B, Regar E, Dudek D, et al. Evaluation of the second generation of a bioresorbable everolimus drug-eluting vascular scaffold for treatment of de novo coronary artery stenosis: six-month clinical and imaging outcomes. Circulation. 2010;122(22):2301–2312. doi: 10.1161/CIRCULATIONAHA.110.970772. [DOI] [PubMed] [Google Scholar]
- 3.Serruys PW, Ormiston JA, Onuma Y, Regar E, Gonzalo N, Garcia-Garcia HM, et al. A bioabsorbable everolimus-eluting coronary stent system (ABSORB): 2-year outcomes and results from multiple imaging methods. Lancet. 2009;373(9667):897–910. doi: 10.1016/S0140-6736(09)60325-1. [DOI] [PubMed] [Google Scholar]
- 4.Virmani R, Guagliumi G, Farb A, Musumeci G, Grieco N, Motta T, et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004;109(6):701–705. doi: 10.1161/01.CIR.0000116202.41966.D4. [DOI] [PubMed] [Google Scholar]