Abstract
Low-level laser (light) therapy (LLLT) is a fast-growing technology used to treat a multitude of conditions that require stimulation of healing, relief of pain and inflammation, and restoration of function. Although the skin is the organ that is naturally exposed to light more than any other organ, it still responds well to red and near-infrared wavelengths. The photons are absorbed by mitochondrial chromophores in skin cells. Consequently electron transport, adenosine triphosphate (ATP) nitric oxide release, blood flow, reactive oxygen species increase and diverse signaling pathways get activated. Stem cells can be activated allowing increased tissue repair and healing. In dermatology, LLLT has beneficial effects on wrinkles, acne scars, hypertrophic scars, and healing of burns. LLLT can reduce UV damage both as a treatment and as a prophylaxis. In pigmentary disorders such as vitiligo, LLLT can increase pigmentation by stimulating melanocyte proliferation and reduce depigmentation by inhibiting autoimmunity. Inflammatory diseases such as psoriasis and acne can also benefit. The non-invasive nature and almost complete absence of side-effects encourages further testing in dermatology.
Keywords: Acne, Dermatology, Herpes, Laser, LLLT, Low level laser therapy, Phototherapy, Skin disease, Skin Rejuvenation, Pigmentation, Vitiligo
Increasingly, non-invasive therapies for skin disease and skin rejuvenation are used, especially in Western countries where relatively high disposable incomes are combined with the desire for an ideal appearance fostered by societal pressures. Although the skin is the organ that is naturally most exposed to light, it still responds well to red and near-infrared wavelengths delivered at the correct parameters with therapeutic intent. Low-level laser therapy (LLLT) was discovered in the late 1960s, but only in recent times has it been widely applied in dermatology. The introduction of light emitting diode (LED) devices has reduced many of the concerns formerly associated with lasers, such as expense, safety concerns and the need for trained personnel to operate them. In fact, many LED devices are designed for home use and are widely sold on the internet. This review will cover the use of LLLT as possibly the ultimate non-invasive approach to treating the skin.
Low-Level Laser (Light) Therapy and Its Mechanism of Action
LLLT, phototherapy or photobiomodulation refers to the use of photons at a non-thermal irradiance to alter biological activity. LLLT uses either coherent light sources (lasers) or non-coherent light sources consisting of filtered lamps or light-emitting diodes (LED) or, on occasion, a combination of both. The main medical applications of LLLT are reducing pain and inflammation, augmenting tissue repair and promoting regeneration of different tissues and nerves, and preventing tissue damage in situations where it is likely to occur.1,2 In the last few decades, non-ablative laser therapies have been used increasingly for the aesthetic treatment of fine wrinkles, photoaged skin and scars, a process known as photorejuvenation (Table 1). More recently, this approach has also been used for inflammatory acne (Table 1).3 LLLT involves exposing cells or tissue to low-levels of red and near infrared (NIR) light. This process is referred to as ‘low-level’ because the energy or power densities employed are low compared to other forms of laser therapy such as ablation, cutting, and thermally coagulating tissue. Recently, medical treatment with LLLT at various intensities has been found to stimulate or inhibit an assortment of cellular processes.4
Table 1.
Examples of LLLT Devices for Dermatological Applications
| Supplier | Product name | Wavelength (nm) | Power Density (mW/cm2) | Standard Dose(J/cm 2) | Application |
|---|---|---|---|---|---|
|
| |||||
| PhotoMedex (Manchester, UK) | Omnilux | 415 (±5) | 40 | 48 | Acne, photodamage, non-melanoma skin cancers, skin rejuvenation, vitiligo and wound healing post elective surgery |
| 633 (±6) | 105 | 126 | |||
| 830 (±5) | 55 | 66 | |||
|
| |||||
| Edge Systems (Signal Hill, CA) | Delphia del Sol | 420 | 7.4 J per treatment area | Acne, improving skin texture, firmness and resilience, increasing lymphatic system activity, fine lines, wrinkles and superficial hyperpigmentation | |
| 600–700 | |||||
| 700–1000 | |||||
|
| |||||
| Flip 4 (Sainte-Julie, Quebec, Canada) | Max7 | 420–700 | ≤4 | Acne, rejuvenation, injured skin healing including the shortening of the post skin resurfacing erythema duration | |
|
| |||||
| Light BioSciences (Virginia Beach, VA) | Gentlewaves | 588 (±10) | Variable | Anti-aging | |
|
| |||||
| OPUSMED (Montreal, Canada) | LumiPhase-R | 660 | 150 | Skin firmness, rhytid depth, wrinkles | |
|
| |||||
| Revitalight (Chicago, IL) | Revitalight 747 | 420 | 80 | 7.2 J per 90 sec. per treatment area | Fine lines, wrinkles, and age spots on the face, neck and hands |
| Hand Spa | 590 | 80 | |||
| Food Spa | 625 | 80 | |||
| Evolution | 940 | 80 | |||
|
| |||||
| Soli-Tone (Woburn, MA) | LumiFacial | 470 | 84 | Acne, anti-aging, hyperpigmentation, rosacea | |
| Lumilift | 525 | 27 | |||
| 590 | 10 | ||||
| 640 | 89 | ||||
|
| |||||
| DUSA (Wilmington, MA) | BLU-U | 417 | 10 | Acne | |
|
| |||||
| Curelight (Rehovot, Israel) | iClearXL | 405–420 | 60 | Acne, anti-aging, skin rejuvenation, acceleration of healing of post peel and post surgical suture sites | |
| Clear100XL | 890–900 | ||||
|
| |||||
| Lumenis (Santa Clara, CA) | ClearLight | 405–420 | 200 | 60 | Acne |
| Clear100 | |||||
|
| |||||
| LIGHTWAVE Technologies (Phoneix, AZ) | LIGHTWAVE Professional Deluxe LED System | 417 | Anti-aging, skin rejuvenation | ||
| 630 | |||||
| 880 | |||||
|
| |||||
| Dynatronics (Salt Lake City, UT) | Synergie LT2 | 660 | 500 mW (total power) | 6 J per treatment area | Anti-aging, skin firmness, wrinkles, skin tone and texture for face and neck |
| 880 | |||||
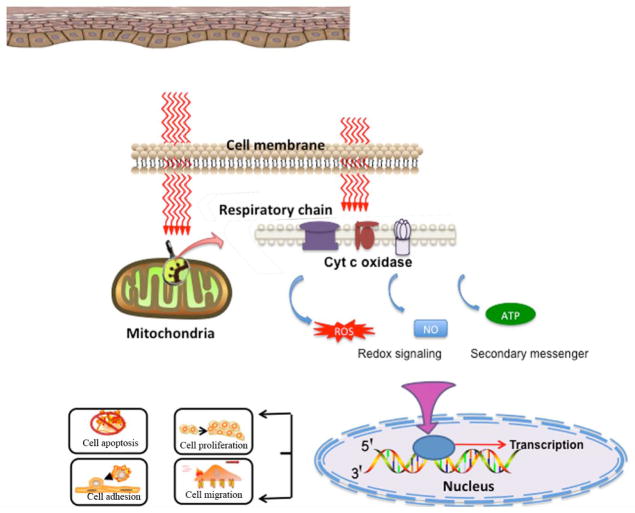
The mechanism associated with the cellular photobiostimulation by LLLT is not yet fully understood. From observation, it appears that LLLT has a wide range of effects at the molecular, cellular, and tissue levels. The basic biological mechanism behind the effects of LLLT is thought to be through absorption of red and NIR light by mitochondrial chromophores, in particular cytochrome c oxidase (CCO) which is contained in the respiratory chain located within the mitochondria,5–7 and perhaps also by photoacceptors in the plasma membrane of cells. Consequently a cascade of events occur in the mitochondria, leading to biostimulation of various processes (Figure 1).8 Absorption spectra obtained for CCO in different oxidation states were recorded and found to be very similar to the action spectra for biological responses to the light.5 It is hypothesized that this absorption of light energy may cause photodissociation of inhibitory nitric oxide from CCO9 leading to enhancement of enzyme activity,10 electron transport,11 mitochondrial respiration and adenosine triphosphate (ATP) production (Figure 1).12–14 In turn, LLLT alters the cellular redox state which induces the activation of numerous intracellular signaling pathways, and alters the affinity of transcription factors concerned with cell proliferation, survival, tissue repair and regeneration (Figure 1).2,5,6,15,16
Figure 1.
Mechanism of action of LLLT.
Basic biological mechanism behind the effects of LLLT is thought to be through absorption of red and NIR light by mitochondrial chromophores, in particular cytochrome c oxidase (CCO) which is contained in the respiratory chain located within the mitochondria 5–7. It is hypothesized that this absorption of light energy may cause photodissociation of inhibitory nitric oxide from CCO 9 leading to enhancement of enzyme activity 10, electron transport 11, mitochondrial respiration and ATP production 12–14. In turn, LLLT by altering the cellular redox state can induce the activation of numerous intracellular signaling pathways; alter the affinity of transcription factors concerned with cell proliferation, survival, tissue repair and regeneration2,5,6,15,16.
Although LLLT is now used to treat a wide variety of ailments, it remains somewhat controversial as a therapy for 2 principle reasons. First, there are uncertainties about the fundamental molecular and cellular mechanisms responsible for transducing signals from the photons incident on the cells to the biological effects that take place in the irradiated tissue. Second, there are significant variations in terms of dosimetry parameters: wavelength, irradiance or power density, pulse structure, coherence, polarization, energy, fluence, irradiation time, contact vs non-contact application, and repetition regimen. Lower dosimetric parameters can result in reduced effectiveness of the treatment and higher ones can lead to tissue damage.1 This illustrates the concept of the biphasic dose response that has been reported to operate in LLLT 1,18,19. Many of the published studies on LLLT include negative results. It is possibly because of an inappropriate choice of light source and dosage. It may also be due to inappropriate preparation of the patient’s skin before application of LLLT, such as: lack of removal of makeup and oily debris, which can interfere with the penetration of the light source, and failure to account for skin pigmentation.17 Inappropriate maintenance of the LLLT equipment can reduce its performance and interfere with clinical results as well. It is important to consider that there is an optimal dose of light for any particular application.
Laser radiation or non-coherent light has a wavelength and radiant exposure dependent capability to alter cellular behavior in the absence of significant heating.20 Phototherapy employs light with wavelengths between 390–1,100 nm and can be continuous wave or pulsed. In normal circumstances, it uses relatively low fluences (0.04–50 J/cm2) and power densities (< 100 mW/cm2).21 Wavelengths in the range of 390 nm to 600 nm are used to treat superficial tissue, and longer wavelengths in the range of 600nm to 1,100nm, which penetrate further, are used to treat deeper-seated tissues (Figure 2).4 Wavelengths in the range 700 nm to 750 nm have been found to have limited biochemical activity and are therefore not often used.1 Various light sources used in LLLT include inert gas lasers and semiconductor laser diodes such as helium neon (HeNe; 633 nm), ruby (694 nm), argon (488 and 514 nm), krypton (521, 530, 568, 647 nm), gallium arsenide (GaAs; > 760 nm, with a common example of 904 nm), and gallium aluminum arsenide (GaAlAs; 612–870 nm).17 A wide range of LED semiconductors are available at lower wavelengths, whose medium contains the elements indium, phosphide and nitride. One question that has not yet been conclusively answered is whether there is any advantage to using coherent laser light over non-coherent LED light.22 While some medical practitioners treat deep tissue lesions using focused lasers in “points”, in dermatology the use of LEDs is becoming increasingly common due to the relatively large areas of tissue that require irradiation.
Figure 2.
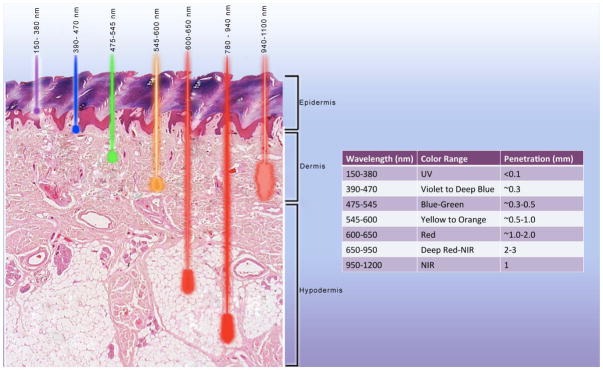
Tissue penetration depths of various wavelengths.
LLLT for Skin Rejuvenation
Skin starts showing its first signs of aging in the late 20s to early 30s and it usually presents with wrinkles, dyspigmentation, telangiectasia, and loss of elasticity. Common histologic and molecular-level features are reduction in the amount of collagen, fragmentation of collagen fibers, elastotic degeneration of elastic fibers, upregulation of matrix metalloproteinases (MMPs), especially MMP-1 and MMP-2, dilated and tortuous dermal vessels, and atrophy and disorientation of the epidermis.23,24 Both chronological and environmental influences are responsible for the aging process of skin; however photodamage seems to be one of the most important causes of these changes.
Several modalities have been developed in order to reverse the dermal and epidermal signs of photo- and chronological aging. The main concept of most of these modalities is removing the epidermis and inducing a controlled form of skin wounding in order to promote collagen biosynthesis and dermal matrix remodeling. The most commonly used interventions as of today are retinoic acid (a vitamin A derivative), dermabrasion, chemical peels, and ablative laser resurfacing with carbon dioxide (CO2) or erbium: yttrium-aluminum-garnet (Er:YAG) lasers or a combination of these wavelengths.25–27 However, these procedures require intensive post-treatment care, prolonged downtime and may lead to complications such as long-lasting erythema, pain, infection, bleedings, oozing, burns, hyper- or hypopigmentation and scarring.28,29 These limitations created a need for the development of alternative rejuvenation procedures that were safer, more effective, had fewer side effects and minimum postoperative care and downtime, which in turn led to the emergence of non-ablative rejuvenation technologies.30–32 Non-ablative skin rejuvenation aims to improve photoaged and aging skin without destroying the epidermis.31,32 Irregular pigmentation and telangiectasia can be treated with intense pulsed light sources (IPL), 532 nm potassium-titanyl-phosphate lasers (KTP), and high-dose 585/595 nm pulsed dye lasers (PDL)33. Wrinkle reduction and skin tightening through thermal injury to the dermis (photothermolysis) can be achieved by other IPL sources (ie, low-dose 589/595 nm PDLs, 1064 & 1320 nm neodymium:yttrium-aluminum-garnet lasers, (Nd:YAG) 1450 nm diode lasers, and 1540 nm erbium fiber lasers).33
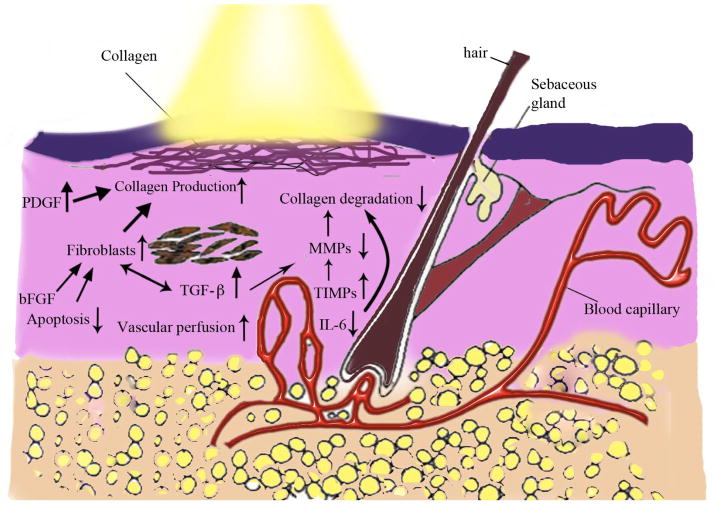
LED which is a novel light source for non-thermal, non-ablative skin rejuvenation has been shown to be effective for improving wrinkles and skin laxity (Figure 3).34–40 It is not a new phenomenon since the first reports of LLLT effects on increased collagen go back to 1987. Studies by Abergel et al. and Yu et al. reported an increase in production of pro-collagen, collagen, basic fibroblast growth factors (bFGF) and proliferation of fibroblasts after exposure to low-energy laser irradiation in vitro and in vivo animal models (Figure 4).41,42 Furthermore, LLLT was already known to increase microcirculation, vascular perfusion in the skin, alter platelet-derived growth factor (PDGF), transforming growth factor (TGF-β1) and inhibit apoptosis (Figure 4).1,43,44 Lee et al. investigated the histologic and ultrastructural changes following a combination of 830 nm, 55 mW/cm2, 66 J/cm2 and 633 nm, 105 mW/cm2, 126 J/cm2 LED phototherapy and observed alteration in the status of MMPs and their tissue inhibitors (TIMPs).33 Furthermore, mRNA levels of IL-1β, TNF-α, ICAM-1, and connexin 43 (Cx43) were increased following LED phototherapy whereas IL-6 levels were decreased (Figure 4) 33. Finally, an increase in the amount of collagen was demonstrated in the post-treatment specimens 33. Pro-inflammatory cytokines IL-1β and TNF-α are thought to be recruited to heal the intentionally formed photothermally-mediated wounds associated with laser treatments, and this cascade of wound healing consequently contributes to new collagen synthesis.33 LED therapy may induce this wound healing process through non-thermal and atraumatic induction of a subclinical ‘quasi-wound’, even without any actual thermal damage which could cause complications as in some other laser treatments.33 TIMPs inhibit MMP activities, so another possible mechanism for the increased collagen could be through the induction of TIMPs (Figure 4). When these observations are put together, it is possible that increased production of IL-1β and TNF-α might have induced MMPs in the early response to LED therapy. This may clear the photodamaged collagen fragments to enable biosynthesis of new collagen fibers. Later on, an increase in the amount of TIMPs might protect the newly synthesized collagen from proteolytic degradation by MMPs.33 Furthermore, increased expression of Cx43 may possibly enhance cell-to-cell communication between dermal components, especially the fibroblasts, and enhance the cellular responses to the photobiostimulation effects from LED treatment, in order to produce new collagen in a larger area which even includes the non-irradiated regions.33 In a clinical study performed by Weiss et al., 300 patients received LED therapy (590 nm, 0.10 J/cm2) alone, and 600 patients received LED therapy in combination with a thermal-based photorejuvenation procedure. Among patients who received LED photorejuvenation alone, 90% reported that they observed a softening of skin texture and a reduction in roughness and fine lines ranging from a significant reduction to sometimes subtle changes.36 Moreover, patients receiving a thermal photorejuvenation laser with or without additional LED photomodulation (n = 152) reported a prominent reduction in post-treatment erythema and an overall impression of increased efficacy with the additional LED treatment.36,45 This reduction in post-treatment erythema could be attributed to anti-inflammatory effects of LLLT.40 Using different pulse sequence parameters, a multicenter clinical trial was conducted, with 90 patients receiving 8 LED treatments over 4 weeks.37,46–48 The outcome of this study showed very favorable results, with over 90% of patients improving by at least one Fitzpatrick photoaging category and 65% of patients demonstrating global improvement in facial texture, fine lines, background erythema, and pigmentation. The results peaked at 4 to 6 months following completion of 8 treatments. Markedly increased collagen in the papillary dermis and reduced MMP-1 were common findings. Barolet et al.’s study is also consistent with the previously mentioned studies. They used a 3-D model of tissue-engineered human reconstructed skin to investigate the potential of 660 nm, 50 mW/cm, 4 J/cm2 LED in modulating collagen and MMP-1 and results showed upregulation of collagen and down-regulation MMP-1 in vitro.40 A split-face, single-blinded clinical study was then carried out to assess the results of this light treatment on skin texture and appearance of individuals with aged/photoaged skin.40 Following 12 LED treatments, profilometry quantification demonstrated that while more than 90% of individuals had a reduction in rhytid depth and surface roughness, 87% of the individuals reported that they have experienced a reduction in the Fitzpatrick wrinkling severity score.40
Figure 3.

Examples of LLLT devices in dermatology for home and clinical use.
Figure 4.
Possible mechanism of actions for LLLT’s effects on skin rejuvenation.
LLLT aids skin rejuvenation through increasing collagen production and decreasing collagen degradation. Increase in collagen production occurs by LLLT’s increasing effects on PDGF and fibroblast production which happens through decreasing apoptosis, increasing vascular perfusion, bFGF and TGF-β. Decrease in IL-6, and increase in TIMPs which in turn reduce MMPs all aid in reduction of collagen degradation.
LLLT for Acne
Pathogenesis of acne vulgaris has not yet been clarified, however current consensus is that it involves four main events: follicular hyperconification, increased sebum secretion effected by the androgenic hormone secretions, colonization of Propionibacterium acnes and inflammation.49 P. acnes plays a key role by acting on triglycerides and releasing its cytokines which in turn trigger inflammatory reactions and alter infundibular keratinization.49 Current treatments for acne vulgaris include topical and oral medications such as topical antibiotics, topical retinoids, benzoyl peroxide, alpha hydroxy acids, salicylic acid, or azaleic acid. In severe cases, systemic antibiotics such as tetracycline and doxycycline, oral retinoids, and some hormones are indicated.50 Medications work by counteracting microcomedone formation, sebum production, P. acnes, and inflammation.50 Despite many options that are available for treatment of acne vulgaris, many patients still respond inadequately to treatment or experience some adverse effects.
Phototherapy (light, lasers, and photodynamic therapy) has been proposed as an alternative therapeutic modality to treat acne vulgaris and was proposed to have less side effects compared to other treatment options.51 Exposure of sunlight was reported to be highly effective for treatment of acne with efficacy up to 70%.52 The sunlight decreases the androgenic hormones in the sebaceous gland, but the unwanted effect of exposure to UVA and UVB limits sunlight for the treatment of acne. Recently, phototherapy with visible light (mainly blue light, red light or combination of both) started being used in the treatment of acne (Figure 3).52 One mechanism of action of phototherapy for acne is through the absorption of light (specifically blue light) by porphyrins that have been produced by P. acnes as a part of its normal metabolism, and that act as endogenous photosensitizers. 49,53 This process causes a photochemical reaction and forms reactive free radicals and Singlet oxygen species which in turn lead to bacterial destruction (Figure 5).49,53 Red light is known to penetrate deeper in tissues when compared to blue light.50 It has been demonstrated that red light can affect the sebum secretion of sebaceous glands and change keratinocyte behavior.54 Furthermore, red light might also exert its effects by modulating cytokines from macrophages and other cells, which in turn could reduce inflammation.51,54
Figure 5.
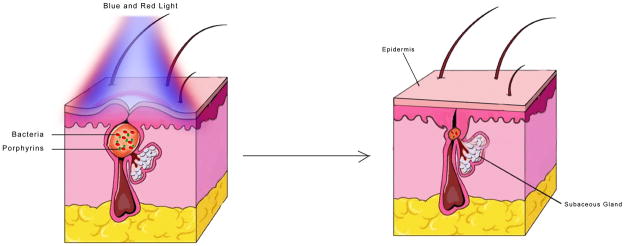
Illustration of acne treatment with red and blue light.
Red and blue light when used in combination have synergistic effects in treatment of acne. P. acnes synthesizes and stores a large amount of porphyrins. Once the porphyrin is exposed to visible light (specifically blue light) it becomes chemically active and transfers to an excited state, resulting in formation of reactive free radicals and singlet oxygen which in turn causes membrane damage in P. acnes 49,53. Red light is proposed to exert its effects through reducing the inflammatory process 51,54.
Several studies reported that LLLT in the red to near infrared spectral range (630–1000 nm) and nonthermal power (less than 200 mW) alone or in combination with other treatment modalities (mainly blue light), is effective for treatment of acne vulgaris.17,49,52,54,55 One of these studies demonstrated significant reduction in active acne lesions after 12 sessions of treatment using 630-nm red spectrum LLLT with a fluence of 12 J/cm2 twice a week for 12 sessions in conjunction with 2% topical clindamycin; however the same study showed no significant effects when a 890 nm laser was used.50 A few studies also showed that the combination of blue light and red light have synergistic effects in acne treatment.49,54–56 It is proposed that synergistic effects of mixed light is due to synergy between the anti-bacterial and anti-inflammatory effect of blue and red light respectively (Figure 5).49,56 It is also worth mentioning that in most studies improvement in inflammatory lesions were higher than the improvement in comedones.49,56
LLLT for Photoprotection
It is widely accepted that the UV range (< 400 nm) exposure is responsible for almost all damaging photo-induced effects on human skin.57–59 Some proposed mechanisms for UV induced skin damage are collagen breakdown, formation of free radicals, inhibition of DNA repair, and inhibition of the immune system.57–59 Existing solutions to prevent UV induced damaging effects are based on minimizing the amount of UV irradiation that reaches the skin, which is achieved by either avoidance of sun exposure or by use of sunscreens. However sometimes sun avoidance might be hard to implement, especially for the people involved in outdoor occupations or leisure activities. On the other hand, the photoprotective efficacy of topical sunscreens have their own limitations as well, which include decreased efficacy following water exposure or perspiration, spectral limitations, possible toxic effects of nanoparticles that are contained by most sunscreens,60 user allergies, and compliance.
It has recently been suggested that infrared (IR) exposure might have protective effects against UV-induced skin damage mainly by triggering protective/repair responses to UV irradiation. In the natural environment, visible and IR solar wavelengths predominate in the morning and UVB and UVA are maximal around noon which suggest that mammalians already possess a natural mechanism which, in reaction to morning IR radiation, prepares the skin for upcoming potentially damaging UV radiation at noon.61 However, opposing views also exist, such as Krutmann’s study demonstrating IR-induced disturbance of the electron flow of the mitochondrial electron transport chain which leads to inadequate energy production in dermal fibroblasts.62 Schroeder’s report is another example stating that IR alters the collagen equilibrium of the dermal extracellular matrix by leading to an increased expression of the collagen-degrading enzyme MMP-1, and by decreasing the de novo synthesis of the collagen itself.59 As previously mentioned, the same light source may have opposite effects on the same tissue depending on the parameters used and these conflicting views are probably due to the biphasic effects of light.18,19
Menezes et al. demonstrated that non-coherent near infrared radiation (NIR) (700–2,000 nm) generated a strong cellular defense against solar UV cytotoxicity in the absence of rising skin temperature and it was assumed to be a long-lasting (at least 24 hours) and cumulative phenomenon.63 Following this study, Frank et al. proposed that IR irradiation prepares cells to resist UVB-induced damage by affecting the mitochondrial apoptotic pathway.64 IR pre-irradiation of human fibroblasts was shown to inhibit UVB activation of caspase-9 and -3, partially release of cytochrome c and Smac/Diablo, decrease pro-apoptotic (ie, Bax) and increase anti-apoptotic proteins (ie, Bcl-2 or Bcl-xL).64 The results suggested that IR inhibited UVB-induced apoptosis by modulating the Bcl2/Bax balance, pointing to a role of p53, a sensor of gene integrity involved in cell apoptosis and repair mechanisms. In a further study, Frank et al. studied more specifically the role of the p53 cell signaling pathway in the prevention of UVB toxicity.64 The response to IR irradiation was shown to be p53 dependent which further suggests that IR irradiation prepares cells to resist and/or to repair further UVB-induced DNA damage. Finally, the IR induction of defense mechanisms was supported by Applegate et al. who reported that the protective protein, ferritin, normally involved in skin repair (scavenger of Fe2+ otherwise available for oxidative reactions) was induced by IR radiation.65
In an in vitro study, it was reported that an increase dermal fibroblast procollagen secretion reduces metalloproteinases (MMP) or collagenase production following non-thermal non-coherent deep red visible LED exposures (660 nm, sequential pulsing mode).40 These results correlated with significant clinical improvement of rhytids in vivo.40 In a subsequent in vivo pilot study, effect of this wavelength in 3 healthy subjects using a minimal erythemal dose (MED) method adapted from sunscreen SPF determination has been investigated.61 The results showed that LED therapy was effective, achieving a significant response in the reduction of the erythema induced by UVB.61 Following this pilot study a further investigation has been performed to find out in vivo aspects of this phenomenon. Effects of non-thermal, non-coherent 660 nm LED pulsed treatments in providing enhanced skin resistance prior to upcoming UV damage was investigated in a group of subjects with normal fair skin and patients presenting polymorphous light eruption (PLE). Results suggested that LED based therapy prior to UV exposure provided significant dose-related protection against UVB induced erythema. A significant reduction in UVB induced erythema reaction was observed in at least one occasion in 85% of subjects as well as in the patients suffering from PLE. Furthermore, a sun protection factor SPF-15-like effect and a reduction in post-inflammatory hyperpigmentation were observed. An in vitro study by Yu et al. revealed that HeNe laser irradiation stimulated an increase in nerve growth factor (NGF) release from cultured keratinocytes and its gene expression.66 NGF is a major paracrine maintenance factor for melanocyte survival in skin.67 It was shown that NGF can protect melanocytes from UV-induced apoptosis by upregulating BCL-2 levels in the cells.68 Therefore, an increase in NGF production induced by HeNe laser treatment may provide another explanation for the photoprotective effects of LLLT.
LLLT for Herpes Virus Lesions
One of the most common virus infections is caused by herpes simplex virus (HSV). HSV is chronic and lasts one’s entire life. The exposure of the host to several kinds of physical or emotional stresses such as fever, exposure to UV light, and immune suppression causes virus reactivation and migration through sensory nerves to skin and mucosa, localizing particularly on the basal epithelium of the lips and the perioral area.69 Up to 60% of sufferers will experience a prodromic stage, after which the lesions develop through stages of erythema, papule, vesicle, ulcer and crust, until healing is achieved. It is accompanied by pain, burning, itching, or tingling at the site where the blisters form. Immune responses to HSV infection involve: macrophages, Langerhans cells, natural killer cells, lymphocyte-mediated delayed-type hypersensitivity, and cytotoxicity.70
While several anti-viral drugs such as acyclovir and valacyclovir are used to control recurrent herpes outbreaks, only limited reduction in the lesions’ healing time has been observed.69 Furthermore, development of drug-resistant HSV strains is of increasing significance especially in immunocompromised patients.70 Therefore, new therapy modalities that can shorten the recurrent episodes and cause prominent reduction of related pain and inflammation are necessary.
LLLT has been suggested as an alternative to current medications for accelerated healing, reducing symptoms and influencing the length of the recurrence period.69,71,72 Among 50 patients with recurrent perioral herpes simplex infection (at least once per month for more than 6 months), when LLLT (690 nm, 80 mW/cm2, 48 J/cm2) was applied daily for 2 weeks during recurrence-free periods it was shown to decrease the frequency of herpes labialis episodes.73 In another study with similar irradiation parameters (647 nm, 50 mW/cm2, 4.5 J/cm2), investigators achieved a significant prolongation of remission intervals from 30 to 73 days in patients with recurrent herpes simplex infection.74 Interestingly, patients with labial herpes infection showed better results than those with genital infection. However, irradiation did not effect established HSV latency in a murine model.75
Even though mechanism of action is still not clear, an indirect effect of LLLT on cellular and humoral components of the immune system involved in antiviral responses rather than a direct virus-inactivating effect was proposed.76 Inoue et al. investigated tuberculin reactions at the bilateral sites of the backs of sensitized guinea pigs. They applied a single low-power laser irradiation dose at a fluence of 3.6 J per cm2on one side and compared it to contralateral non-irradiated sites.77 Interestingly, following irradiation, tuberculin reaction was suppressed not only at the irradiated site but also at the contralateral nonirradiated site. It is worth to note that this phenomenon was observed when mononuclear cells were dominant in the perivascular cellular infiltration. Based on their results, they have suggested a possible systemic inhibitory effect of LLLT on delayed hypersensitivity reactions.77 Activation and proliferation of lymphocytes78–81 and macrophages82 as well as the synthesis and expression of cytokines83,84 following low intensities of red and NIR light have been reported by several investigators. The question of whether these effects of LLLT have any influence on HSV infection remains to be determined.
LLLT for Vitiligo
Vitiligo is an acquired pigmentary disorder characterized by depigmentation of the skin and hair. The underlying mechanism of how the functional melanocytes disappear from the involved skin is still under investigation. However, findings suggest that regardless of the pathogenetic mechanism involved, keratinocytes, fibroblasts, melanoblasts and melanocytes may all be involved in both the depigmentation and also the repigmentation processes of vitiligo.66,85–89 Therefore, stimulation of these epidermal and dermal cells may be a possible treatment option. Due to the obscure pathogenesis of the disease, treatment of vitiligo has generally been unsatisfactory. Current existing therapies that induce varying degrees of repigmentation in patients with vitiligo are topical corticosteroids, phototherapy, and photochemotherapy (PUVA).89 In 1982, a group of investigators found that low energy laser irradiation had effects on defective biosynthesis of catecholamine in certain dermatological conditions including scleroderma and vitiligo.90,91 Later on, one of the investigators from the same group reported that after 6–8 months of treating 18 vitiglio patients with low-energy HeNe laser (632 nm, 25 mW/cm2 ) therapy, marked repigmentation was observed in 64% of the patients and some follicular repigmentation was observed in the remaining 34%.91 Since then, LLLT has been suggested as an alternative effective treatment option for patients with vitiligo.66,88,89
Segmental-type vitiligo is associated with a dysfunction of the sympathetic nerves in the affected skin and it is relatively resistant to conventional therapies.66 Based on the previous reports stating that HeNe laser irradiation leads to improvement in nerve injury92–94 and LLLT induces repigmentation responses,95,96 it was proposed that the HeNe laser might be a potential treatment modality for treatment of segmental type vitiligo. 66 When the HeNe laser light was administered locally (3 J/cm2, 1.0 mW, 632.8 nm), marked perilesional and perifollicular repigmentation (> 50%) was observed in 60% of patients with successive treatments. Both NGF and bFGF stimulate melanocyte migration and deficiencies of these mediators may participate in the development of vitiligo.86,97,98 In the same study, when cultured keratinocytes and fibroblasts were irradiated with 0.5–1.5 J per cm2 HeNe laser, significant increase in bFGF release both from keratinocytes and fibroblasts as well as a significant increase in NGF release from keratinocytes was reported. 66 Additionally, the medium from HeNe laser irradiated keratinocytes stimulated [3H]thymidine uptake and proliferation of cultured melanocytes. Another study by Lan et al. demonstrated that the HeNe laser (632.8 nm, 1 J/cm2 and 10 mW) stimulates melanocyte proliferation through enhanced α2β1 integrin expression88 and induces melanocyte growth through upregulation of the expression of phosphorylated cyclic-AMP response element binding protein (CREB) which is an important regulator of melanocyte growth.88 ECM molecules are also important elements of the pigmentation process due to their regulatory roles for physiological functions of pigment cells including morphology, migration, tyrosinase activity and proliferation.99–101 Type IV collagen is present in the basement membrane and is known to have an intricate relationship with melanocytes in the epidermis such as increasing melanocyte mobility.89 Following, HeNe irradiation, the attachment of melanocytes to type IV collagen was found to be significantly enhanced which also indicated modulation of melanocyte physiological function by HeNe laser irradiation.88 Furthermore, among various ECM proteins found in the dermis, fibronectin was shown to have significant effects on both differentiation and migration of cultured melanoblasts and melanocytes.102,103 In 1983, Gibson et al. demonstrated that the physical distribution of fibronectin in vivo was closely associated with the migration path undertaken by melanoblasts during the repigmentation process of vitiligo.104 Based on Lan at al.’s findings, an immature melanoblast cell line (NCCmelb4) showed significant decrease in the attachment to fibronectin following HeNe laser treatment while the attachment of a more differentiated melanoblast cell line (NCCmelan5) to fibronectin increased about 20% following 1 J/cm2, 10 mW HeNe laser treatment.89 Lastly, expression of integrin a5b1 which mediate locomotion of pigment cells was found to be enhanced on NCCmelb4 cells.89
LLLT for Producing Depigmentation
Most studies carried out for vitiligo show the stimulatory effects of LLLT on pigmentation; however in a previously mentioned study, while testing effects of blue and red laser for acne treatment, an interesting and unexpected result was found for the first time.49 Combining both blue (415 +−5 nm, irradiance 40 mW/cm2, 48 J/cm2 ) and red (633 +- 6 nm, 80 mW/cm2, 96 J/cm2 ) light produced an overall decrease in the melanin level. Instrumental measurement results showed that melanin level increased by 6.7 (the median of differences between the melanin level before and after one treatment session) after blue light irradiation without a statistical significance (P > .1), whereas it decreased by 15.5 with statistical significance (P < .005) after red light irradiation. This finding may have some relationship with the laser’s brightening effect of the skin tone, which 14 out of 24 patients spontaneously reported after the treatment period. However as of today, no other studies investigated or reported similar decrease in melanin levels following red light irradiation. Considering that different parameters are used for vitiligo and acne treatment, different effects of red light on the same tissue might be due to the biphasic effects of LLLT.18,19
LLLT for Hypertrophic Scars and Keloids
Hypertrophic scars and keloids are benign skin tumors that usually form following surgery, trauma, or acne and are difficult to eradicate. Fibroblastic proliferation and excess collagen deposits are the 2 main characteristics105 and imbalance between rates of collagen biosynthesis and degradation superimposed on the individual’s genetic predisposition have been implicated in their pathogenesis. A wide range of surgical (eg, cryotherapy, excision), non-surgical (e.g., pharmacological, mechanical pressure, silicone gel dressings), and laser therapies (CO2, pulsed dye, fractional ablative, and non-ablative lasers) have been tested with variable success, however until now, an optimal treatment of these lesions remains to be found.106–108 It has recently been proposed that poor regulation of interleukin (IL)-6 signaling pathways and transforming growth factor beta-I (TGF-βI) expression have a significant role in this process and thus inhibition of the IL-6 pathway and/or TGF-βI could be a potential therapeutic target.106,107,109–111 Based on the reports demonstrating the effects of LLLT on decreasing IL-6 mRNA levels,33 modulation of PDGF, TGF-β, interleukins such as IL-13 and IL- 15, MMPs, which are all also associated with abnormal wound healing,112,113 it was proposed to be an alternative therapy to existing treatment options. The use of LLLT as a prophylactic method to alter the wound healing process to avoid or attenuate the formation of hypertrophic scars or keloids has been investigated by Barolet and Boucher in 3 cases studies, where following scar revision by surgery or CO2 laser ablation on bilateral areas, a single scar was treated daily by the patient at home with NIR - LED 805 nm at 30 mW/cm2 and 27 J/cm2.112 The first patient had pre-auricular linear keloids bilaterally post-face lift procedure and surgical scar revision/excision had been performed. The second patient had hypertrophic scars on the chest bilaterally post-acne when the CO2 laser was used for resurfacing. The third patient had hypertrophic scars on the back bilaterally post-excision and again the CO2 laser was used for resurfacing. As a result, significant improvements on the NIR-LED treated vs the control scar were seen in all efficacy measures and moreover no significant treatment-related adverse effects were reported.112
LLLT for Burns
In a clinical study by Weiss et al. 10 patients received LED treatment (590 nm) for acute sunburn using a once-or twice-daily treatment regimen for 3 days, treating only half of the affected anatomic area.36 Decreased symptoms of burning, redness, swelling, and peeling were reported. One patient received LED treatment twice daily for 3 days only on half of his back, and other half was left untreated.36 When compared with the untreated side, decreased MMP-1 was demonstrated on the LED-treated side through immunofluorescence staining. Moreover, RT-PCR gene expression analysis showed a significant decrease in MMP-1 gene expression on the LED-treated side at both 4 and 24 hours post–UV injury compared with the untreated side. Other significant changes were also noted with LED treatment related to inflammation and dermal matrix composition 4 days post–ultraviolet (UV) exposure.36
One of the main complications of receiving laser treatment is burns which may be devastating for the patient. LED was suggested as a treatment modality for facilitating faster healing. A group of 9 patients who had a variety of second-degree burns from nonablative laser devices were given LED therapy once a day for 1 week and according to both the patient and the physician, healing occurred 50% faster.36 Also the same investigators conducted a pilot study, where one forearm was injured by a CO2 laser using a computer pattern generator to deliver the identical treatment to both test sites. Both sites received daily dressing changes using a non-stick dressing and Polysporin ointment, but one site also received additional LED treatment.36 As a result, when compared to the untreated control site, accelerated reepithelialization was observed in the LED-treated site 36.
LLLT for Psoriasis
More recently LLLT has been considered for treatment of plaque psoriasis. A recent preliminary study investigated the efficacy of a combination of 830 nm (near infrared) and 630 nm (visible red light) to treat recalcitrant psoriasis using LED irradiation. All patients with psoriasis resistant to conventional therapy were enrolled and were treated sequentially with 830 nm and 630 nm wavelengths in 2 20-min sessions with 48 hours between session for 4 or 5 weeks. The results showed no adverse side effects and a resolution of psoriasis.114 The limitation of this study was the small number of patients enrolled, however the results observed encourage future investigations for use of LLLT in treating psoriasis.
Conclusion
LLLT appears to have a wide range of applications of use in dermatology, especially in indications where stimulation of healing, reduction of inflammation, reduction of cell death and skin rejuvenation are required. The application of LLLT to disorders of pigmentation may work both ways by producing both repigmentation of vitiligo, and depigmentation of hyperpigmented lesions depending on the dosimetric parameters. The introduction of LED array-based devices has simplified the application to large areas of skin. There is no agreement as yet on several important parameters particularly whether red, NIR, or a combination of both wavelengths is optimal for any particular application. There is a credibility gap that needs to be overcome before LLLT is routinely applied in every dermatologist’s office.
Acknowledgments
This work was supported by the US NIH (R01AI050875 to MRH)
Footnotes
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure for Potential Conflicts of Interest and none were reported. Dr Gupta has received a grant from Boyscast Fellowship, Rolo-11, in India. All other authors have nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012 Feb;40(2):516–533. doi: 10.1007/s10439-011-0454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta A, Avci P, Sadasivam M, et al. Shining light on nanotechnology to help repair and regeneration. Biotechnol Adv. 2012 Aug 21; doi: 10.1016/j.biotechadv.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seaton ED, Mouser PE, Charakida A, Alam S, Seldon PM, Chu AC. Investigation of the mechanism of action of nonablative pulsed-dye laser therapy in photorejuvenation and inflammatory acne vulgaris. Br J Dermatol. 2006 Oct;155(4):748–755. doi: 10.1111/j.1365-2133.2006.07429.x. [DOI] [PubMed] [Google Scholar]
- 4.Barolet D. Light-emitting diodes (LEDs) in dermatology. Semin Cutan Med Surg. 2008 Dec;27(4):227–238. doi: 10.1016/j.sder.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Karu TI, Kolyakov SF. Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg. 2005 Aug;23(4):355–361. doi: 10.1089/pho.2005.23.355. [DOI] [PubMed] [Google Scholar]
- 6.Greco M, Guida G, Perlino E, Marra E, Quagliariello E. Increase in RNA and protein synthesis by mitochondria irradiated with helium-neon laser. Biochem Biophys Res Commun. 1989 Sep 29;163(3):1428–1434. doi: 10.1016/0006-291x(89)91138-8. [DOI] [PubMed] [Google Scholar]
- 7.Karu TI, Pyatibrat LV, Kalendo GS. Photobiological modulation of cell attachment via cytochrome c oxidase. Photochem Photobiol Sci. 2004 Feb;3(2):211–216. doi: 10.1039/b306126d. [DOI] [PubMed] [Google Scholar]
- 8.Oron U. Light therapy and stem cells: a therapeutic intervention of the future? Interventional Cardiology. 2011;3(6):627–629. [Google Scholar]
- 9.Lane N. Cell biology: power games. Nature. 2006 Oct 26;443(7114):901–903. doi: 10.1038/443901a. [DOI] [PubMed] [Google Scholar]
- 10.Wong-Riley MT, Liang HL, Eells JT, et al. Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem. 2005 Feb 11;280(6):4761–4771. doi: 10.1074/jbc.M409650200. [DOI] [PubMed] [Google Scholar]
- 11.Pastore D, Greco M, Petragallo VA, Passarella S. Increase in <--H+/e- ratio of the cytochrome c oxidase reaction in mitochondria irradiated with helium-neon laser. Biochem Mol Biol Int. 1994 Oct;34(4):817–826. [PubMed] [Google Scholar]
- 12.Karu T, Pyatibrat L, Kalendo G. Irradiation with He-Ne laser increases ATP level in cells cultivated in vitro. J Photochem Photobiol B. 1995 Mar;27(3):219–223. doi: 10.1016/1011-1344(94)07078-3. [DOI] [PubMed] [Google Scholar]
- 13.Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999 Mar;49(1):1–17. doi: 10.1016/S1011-1344(98)00219-X. [DOI] [PubMed] [Google Scholar]
- 14.Harris DM. Editorial Comment Biomolecular Mechanisms of Laser Biostimulation. Journal of clinical laser medicine & surgery. 1991;9(4):277–280. [Google Scholar]
- 15.Liu H, Colavitti R, Rovira, Finkel T. Redox-dependent transcriptional regulation. Circ Res. 2005 Nov 11;97(10):967–974. doi: 10.1161/01.RES.0000188210.72062.10. [DOI] [PubMed] [Google Scholar]
- 16.Peplow PV, Chung TY, Ryan B, Baxter GD. Laser photobiomodulation of gene expression and release of growth factors and cytokines from cells in culture: a review of human and animal studies. Photomed Laser Surg. 2011 May;29(5):285–304. doi: 10.1089/pho.2010.2846. [DOI] [PubMed] [Google Scholar]
- 17.Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, Alam M. Low-level laser therapy for wound healing: mechanism and efficacy. Dermatol Surg. 2005 Mar;31(3):334–340. doi: 10.1111/j.1524-4725.2005.31086. [DOI] [PubMed] [Google Scholar]
- 18.Huang YY, Sharma SK, Carroll J, Hamblin MR. Biphasic dose response in low level light therapy - an update. Dose Response. 2011;9(4):602–618. doi: 10.2203/dose-response.11-009.Hamblin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang YY, Chen AC, Carroll JD, Hamblin MR. Biphasic dose response in low level light therapy. Dose Response. 2009;7(4):358–383. doi: 10.2203/dose-response.09-027.Hamblin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Basford JR. Low intensity laser therapy: still not an established clinical tool. Lasers Surg Med. 1995;16(4):331–342. doi: 10.1002/lsm.1900160404. [DOI] [PubMed] [Google Scholar]
- 21.AlGhamdi KM, Kumar A, Moussa NA. Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci. 2012 Jan;27(1):237–249. doi: 10.1007/s10103-011-0885-2. [DOI] [PubMed] [Google Scholar]
- 22.Hode L. The importance of the coherency. Photomed Laser Surg. 2005 Aug;23(4):431–434. doi: 10.1089/pho.2005.23.431. [DOI] [PubMed] [Google Scholar]
- 23.Kligman LH. Photoaging. Manifestations, prevention, and treatment. Clin Geriatr Med. 1989 Feb;5(1):235–251. [PubMed] [Google Scholar]
- 24.Takema Y, Yorimoto Y, Kawai M, Imokawa G. Age-related changes in the elastic properties and thickness of human facial skin. Br J Dermatol. 1994 Nov;131(5):641–648. doi: 10.1111/j.1365-2133.1994.tb04975.x. [DOI] [PubMed] [Google Scholar]
- 25.Branham GH, Thomas JR. Rejuvenation of the skin surface: chemical peel and dermabrasion. Facial Plast Surg. 1996 Apr;12(2):125–133. doi: 10.1055/s-0028-1082404. [DOI] [PubMed] [Google Scholar]
- 26.Airan LE, Hruza G. Current lasers in skin resurfacing. Facial Plast Surg Clin North Am. 2005 Feb;13(1):127–139. doi: 10.1016/j.fsc.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Paasch U, Haedersdal M. Laser systems for ablative fractional resurfacing. Expert Rev Med Devices. 2011 Jan;8(1):67–83. doi: 10.1586/erd.10.74. [DOI] [PubMed] [Google Scholar]
- 28.Nanni CA, Alster TS. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. 1998 Mar;24(3):315–320. doi: 10.1111/j.1524-4725.1998.tb04161.x. [DOI] [PubMed] [Google Scholar]
- 29.Sriprachya-Anunt S, Fitzpatrick RE, Goldman MP, Smith SR. Infections complicating pulsed carbon dioxide laser resurfacing for photoaged facial skin. Dermatol Surg. 1997 Jul;23(7):527–535. doi: 10.1111/j.1524-4725.1997.tb00679.x. discussion 535–526. [DOI] [PubMed] [Google Scholar]
- 30.Sachdev M, Hameed S, Mysore V. Nonablative lasers and nonlaser systems in dermatology: current status. Indian J Dermatol Venereol Leprol. 2011 May-Jun;77(3):380–388. doi: 10.4103/0378-6323.79733. [DOI] [PubMed] [Google Scholar]
- 31.Weiss RA, McDaniel DH, Geronemus RG. Review of nonablative photorejuvenation: reversal of the aging effects of the sun and environmental damage using laser and light sources. Semin Cutan Med Surg. 2003 Jun;22(2):93–106. doi: 10.1053/sder.2003.50008. [DOI] [PubMed] [Google Scholar]
- 32.Hardaway CA, Ross EV. Nonablative laser skin remodeling. Dermatol Clin. 2002 Jan;20(1):97–111. ix. doi: 10.1016/s0733-8635(03)00049-4. [DOI] [PubMed] [Google Scholar]
- 33.Lee SY, Park KH, Choi JW, et al. A prospective, randomized, placebo-controlled, double-blinded, and split-face clinical study on LED phototherapy for skin rejuvenation: clinical, profilometric, histologic, ultrastructural, and biochemical evaluations and comparison of three different treatment settings. J Photochem Photobiol B. 2007 Jul 27;88(1):51–67. doi: 10.1016/j.jphotobiol.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 34.Dierickx CC, Anderson RR. Visible light treatment of photoaging. Dermatol Ther. 2005 May-Jun;18(3):191–208. doi: 10.1111/j.1529-8019.2005.05019.x. [DOI] [PubMed] [Google Scholar]
- 35.Weiss RA, Weiss MA, Geronemus RG, McDaniel DH. A novel non-thermal non-ablative full panel LED photomodulation device for reversal of photoaging: digital microscopic and clinical results in various skin types. J Drugs Dermatol. 2004 Nov-Dec;3(6):605–610. [PubMed] [Google Scholar]
- 36.Weiss RA, McDaniel DH, Geronemus RG, et al. Clinical experience with light-emitting diode (LED) photomodulation. Dermatol Surg. 2005 Sep;31(9 Pt 2):1199–1205. doi: 10.1111/j.1524-4725.2005.31926. [DOI] [PubMed] [Google Scholar]
- 37.Weiss RA, McDaniel DH, Geronemus RG, Weiss MA. Clinical trial of a novel nonthermal LED array for reversal of photoaging: clinical, histologic, and surface profilometric results. Lasers Surg Med. 2005 Feb;36(2):85–91. doi: 10.1002/lsm.20107. [DOI] [PubMed] [Google Scholar]
- 38.Bhat J, Birch J, Whitehurst C, Lanigan SW. A single-blinded randomised controlled study to determine the efficacy of Omnilux Revive facial treatment in skin rejuvenation. Lasers Med Sci. 2005;20(1):6–10. doi: 10.1007/s10103-005-0330-5. [DOI] [PubMed] [Google Scholar]
- 39.Russell BA, Kellett N, Reilly LR. A study to determine the efficacy of combination LED light therapy (633 nm and 830 nm) in facial skin rejuvenation. J Cosmet Laser Ther. 2005 Dec;7(3–4):196–200. doi: 10.1080/14764170500370059. [DOI] [PubMed] [Google Scholar]
- 40.Barolet D, Roberge CJ, Auger FA, Boucher A, Germain L. Regulation of skin collagen metabolism in vitro using a pulsed 660 nm LED light source: clinical correlation with a single-blinded study. J Invest Dermatol. 2009 Dec;129(12):2751–2759. doi: 10.1038/jid.2009.186. [DOI] [PubMed] [Google Scholar]
- 41.Abergel RP, Lyons RF, Castel JC, Dwyer RM, Uitto J. Biostimulation of wound healing by lasers: experimental approaches in animal models and in fibroblast cultures. J Dermatol Surg Oncol. 1987 Feb;13(2):127–133. doi: 10.1111/j.1524-4725.1987.tb00510.x. [DOI] [PubMed] [Google Scholar]
- 42.Yu W, Naim JO, Lanzafame RJ. The effect of laser irradiation on the release of bFGF from 3T3 fibroblasts. Photochem Photobiol. 1994 Feb;59(2):167–170. doi: 10.1111/j.1751-1097.1994.tb05017.x. [DOI] [PubMed] [Google Scholar]
- 43.Schindl A, Heinze G, Schindl M, Pernerstorfer-Schon H, Schindl L. Systemic effects of low-intensity laser irradiation on skin microcirculation in patients with diabetic microangiopathy. Microvasc Res. 2002 Sep;64(2):240–246. doi: 10.1006/mvre.2002.2429. [DOI] [PubMed] [Google Scholar]
- 44.Ben-Dov N, Shefer G, Irintchev A, Wernig A, Oron U, Halevy O. Low-energy laser irradiation affects satellite cell proliferation and differentiation in vitro. Biochim Biophys Acta. 1999 Jan 11;1448(3):372–380. doi: 10.1016/s0167-4889(98)00147-5. [DOI] [PubMed] [Google Scholar]
- 45.Kucuk BB, Oral K, Selcuk NA, Toklu T, Civi OG. The anti-inflammatory effect of low-level laser therapy on experimentally induced inflammation of rabbit temporomandibular joint retrodiscal tissues. J Orofac Pain. 2010 Summer;24(3):293–297. [PubMed] [Google Scholar]
- 46.Geronemus RG, Weiss RA, Weiss MA, et al. Non-ablative LED photomodulation light activated fibroblast stimulation clinical trial. Lasers Surg Med. 2003;25:22. [Google Scholar]
- 47.McDaniel DH, Newman J, Geronemus R, et al. Non-ablative non- thermal LED photomodulation—a multicenter clinical photoaging trial. Lasers Surg Med. 2003;15:22. [Google Scholar]
- 48.Weiss RA, McDaniel DH, Geronemus R, et al. Non-ablative, non- thermal light emitting diode (LED) phototherapy of photoaged skin. Laser Surg Med. 2004;16:31. [Google Scholar]
- 49.Lee SY, You CE, Park MY. Blue and red light combination LED phototherapy for acne vulgaris in patients with skin phototype IV. Lasers Surg Med. 2007 Feb;39(2):180–188. doi: 10.1002/lsm.20412. [DOI] [PubMed] [Google Scholar]
- 50.Aziz-Jalali MH, Tabaie SM, Djavid GE. Comparison of Red and Infrared Low-level Laser Therapy in the Treatment of Acne Vulgaris. Indian J Dermatol. 2012 Mar;57(2):128–130. doi: 10.4103/0019-5154.94283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rotunda AM, Bhupathy AR, Rohrer TE. The new age of acne therapy: light, lasers, and radiofrequency. J Cosmet Laser Ther. 2004 Dec;6(4):191–200. doi: 10.1080/14764170410008124. [DOI] [PubMed] [Google Scholar]
- 52.Cunliffe WJ, Goulden V. Phototherapy and acne vulgaris. Br J Dermatol. 2000 May;142(5):855–856. doi: 10.1046/j.1365-2133.2000.03528.x. [DOI] [PubMed] [Google Scholar]
- 53.Ross EV. Optical treatments for acne. Dermatol Ther. 2005 May-Jun;18(3):253–266. doi: 10.1111/j.1529-8019.2005.05024.x. [DOI] [PubMed] [Google Scholar]
- 54.Sadick NS. Handheld LED array device in the treatment of acne vulgaris. J Drugs Dermatol. 2008 Apr;7(4):347–350. [PubMed] [Google Scholar]
- 55.Goldberg DJ, Russell BA. Combination blue (415 nm) and red (633 nm) LED phototherapy in the treatment of mild to severe acne vulgaris. J Cosmet Laser Ther. 2006 Jun;8(2):71–75. doi: 10.1080/14764170600735912. [DOI] [PubMed] [Google Scholar]
- 56.Papageorgiou P, Katsambas A, Chu A. Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris. Br J Dermatol. 2000 May;142(5):973–978. doi: 10.1046/j.1365-2133.2000.03481.x. [DOI] [PubMed] [Google Scholar]
- 57.Sinha RP, Hader DP. UV-induced DNA damage and repair: a review. Photochem Photobiol Sci. 2002 Apr;1(4):225–236. doi: 10.1039/b201230h. [DOI] [PubMed] [Google Scholar]
- 58.Calles C, Schneider M, Macaluso F, Benesova T, Krutmann J, Schroeder P. Infrared A radiation influences the skin fibroblast transcriptome: mechanisms and consequences. J Invest Dermatol. 2010 Jun;130(6):1524–1536. doi: 10.1038/jid.2010.9. [DOI] [PubMed] [Google Scholar]
- 59.Schroeder P, Calles C, Benesova T, Macaluso F, Krutmann J. Photoprotection beyond ultraviolet radiation--effective sun protection has to include protection against infrared A radiation-induced skin damage. Skin Pharmacol Physiol. 2010;23(1):15–17. doi: 10.1159/000257259. [DOI] [PubMed] [Google Scholar]
- 60.Kimura E, Kawano Y, Todo H, Ikarashi Y, Sugibayashi K. Measurement of skin permeation/penetration of nanoparticles for their safety evaluation. Biol Pharm Bull. 2012;35(9):1476–1486. doi: 10.1248/bpb.b12-00103. [DOI] [PubMed] [Google Scholar]
- 61.Barolet D, Boucher A. LED photoprevention: reduced MED response following multiple LED exposures. Lasers Surg Med. 2008 Feb;40(2):106–112. doi: 10.1002/lsm.20615. [DOI] [PubMed] [Google Scholar]
- 62.Krutmann J, Schroeder P. Role of mitochondria in photoaging of human skin: the defective powerhouse model. J Investig Dermatol Symp Proc. 2009 Aug;14(1):44–49. doi: 10.1038/jidsymp.2009.1. [DOI] [PubMed] [Google Scholar]
- 63.Menezes S, Coulomb B, Lebreton C, Dubertret L. Non-coherent near infrared radiation protects normal human dermal fibroblasts from solar ultraviolet toxicity. J Invest Dermatol. 1998 Oct;111(4):629–633. doi: 10.1046/j.1523-1747.1998.00338.x. [DOI] [PubMed] [Google Scholar]
- 64.Frank S, Oliver L, Lebreton-De Coster C, et al. Infrared radiation affects the mitochondrial pathway of apoptosis in human fibroblasts. J Invest Dermatol. 2004 Nov;123(5):823–831. doi: 10.1111/j.0022-202X.2004.23472.x. [DOI] [PubMed] [Google Scholar]
- 65.Applegate LA, Scaletta C, Panizzon R, Frenk E, Hohlfeld P, Schwarzkopf S. Induction of the putative protective protein ferritin by infrared radiation: implications in skin repair. Int J Mol Med. 2000 Mar;5(3):247–251. doi: 10.3892/ijmm.5.3.247. [DOI] [PubMed] [Google Scholar]
- 66.Yu HS, Wu CS, Yu CL, Kao YH, Chiou MH. Helium-neon laser irradiation stimulates migration and proliferation in melanocytes and induces repigmentation in segmental-type vitiligo. J Invest Dermatol. 2003 Jan;120(1):56–64. doi: 10.1046/j.1523-1747.2003.12011.x. [DOI] [PubMed] [Google Scholar]
- 67.Yaar M, Grossman K, Eller M, Gilchrest BA. Evidence for nerve growth factor-mediated paracrine effects in human epidermis. J Cell Biol. 1991 Nov;115(3):821–828. doi: 10.1083/jcb.115.3.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhai S, Yaar M, Doyle SM, Gilchrest BA. Nerve growth factor rescues pigment cells from ultraviolet-induced apoptosis by upregulating BCL-2 levels. Exp Cell Res. 1996 May 1;224(2):335–343. doi: 10.1006/excr.1996.0143. [DOI] [PubMed] [Google Scholar]
- 69.de Paula Eduardo C, Bezinelli LM, de Paula Eduardo F, et al. Prevention of recurrent herpes labialis outbreaks through low-intensity laser therapy: a clinical protocol with 3-year follow-up. Lasers Med Sci. 2011 Nov 16; doi: 10.1007/s10103-011-1019-6. [DOI] [PubMed] [Google Scholar]
- 70.Whitley RJ, Kimberlin DW, Roizman B. Herpes simplex viruses. Clin Infect Dis. 1998 Mar;26(3):541–553. doi: 10.1086/514600. quiz 554–545. [DOI] [PubMed] [Google Scholar]
- 71.Munoz Sanchez PJ, Capote Femenias JL, Diaz Tejeda A, Tuner J. The effect of 670-nm low laser therapy on herpes simplex type 1. Photomed Laser Surg. 2012 Jan;30(1):37–40. doi: 10.1089/pho.2011.3076. [DOI] [PubMed] [Google Scholar]
- 72.Bello-Silva MS, de Freitas PM, Aranha AC, Lage-Marques JL, Simoes A, de Paula Eduardo C. Low- and high-intensity lasers in the treatment of herpes simplex virus 1 infection. Photomed Laser Surg. 2010 Feb;28(1):135–139. doi: 10.1089/pho.2008.2458. [DOI] [PubMed] [Google Scholar]
- 73.Schindl A, Neumann R. Low-intensity laser therapy is an effective treatment for recurrent herpes simplex infection. Results from a randomized double-blind placebo-controlled study. J Invest Dermatol. 1999 Aug;113(2):221–223. doi: 10.1046/j.1523-1747.1999.00684.x. [DOI] [PubMed] [Google Scholar]
- 74.Landthaler M, Haina D, Waidelich W. Treatment of zoster, post-zoster pain and herpes simplex recidivans in loco with laser light. Fortschr Med. 1983 Jun 9;101(22):1039–1041. [PubMed] [Google Scholar]
- 75.Perrin D, Jolivald JR, Triki H, et al. Effect of laser irradiation on latency of herpes simplex virus in a mouse model. Pathol Biol (Paris) 1997 Jan;45(1):24–27. [PubMed] [Google Scholar]
- 76.Korner R, Bahmer F, Wigand R. The effect of infrared laser rays on herpes simplex virus and the functions of human immunocompetent cells. Hautarzt. 1989 Jun;40(6):350–354. [PubMed] [Google Scholar]
- 77.Inoue K, Nishioka J, Hukuda S. Suppressed tuberculin reaction in guinea pigs following laser irradiation. Lasers Surg Med. 1989;9(3):271–275. doi: 10.1002/lsm.1900090310. [DOI] [PubMed] [Google Scholar]
- 78.Inoue K, Nishioka J, Hukuda S. Altered lymphocyte proliferation by low dosage laser irradiation. Clin Exp Rheumatol. 1989 Sep-Oct;7(5):521–523. [PubMed] [Google Scholar]
- 79.Yu W, Chi LH, Naim JO, Lanzafame RJ. Improvement of host response to sepsis by photobiomodulation. Lasers Surg Med. 1997;21(3):262–268. doi: 10.1002/(sici)1096-9101(1997)21:3<262::aid-lsm6>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 80.Schindl L, Schindl M, Polo L, Jori G, Perl S, Schindl A. Effects of low power laser-irradiation on differential blood count and body temperature in endotoxin-preimmunized rabbits. Life Sci. 1997;60(19):1669–1677. doi: 10.1016/s0024-3205(97)00109-4. [DOI] [PubMed] [Google Scholar]
- 81.Manteifel V, Bakeeva L, Karu T. Ultrastructural changes in chondriome of human lymphocytes after irradiation with He-Ne laser: appearance of giant mitochondria. J Photochem Photobiol B. 1997 Mar;38(1):25–30. doi: 10.1016/s1011-1344(96)07426-x. [DOI] [PubMed] [Google Scholar]
- 82.Bolton P, Young S, Dyson M. Macrophage responsiveness to light therapy: a dose response study. Laser Ther. 1990;2:101–106. [Google Scholar]
- 83.Funk JO, Kruse A, Kirchner H. Cytokine production after helium-neon laser irradiation in cultures of human peripheral blood mononuclear cells. J Photochem Photobiol B. 1992 Dec;16(3–4):347–355. doi: 10.1016/1011-1344(92)80022-n. [DOI] [PubMed] [Google Scholar]
- 84.Yu HS, Chang KL, Yu CL, Chen JW, Chen GS. Low-energy helium-neon laser irradiation stimulates interleukin-1 alpha and interleukin-8 release from cultured human keratinocytes. J Invest Dermatol. 1996 Oct;107(4):593–596. doi: 10.1111/1523-1747.ep12583090. [DOI] [PubMed] [Google Scholar]
- 85.Lee AY. Role of keratinocytes in the development of vitiligo. Ann Dermatol. 2012 May;24(2):115–125. doi: 10.5021/ad.2012.24.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yu R, Huang Y, Zhang X, Zhou Y. Potential role of neurogenic inflammatory factors in the pathogenesis of vitiligo. J Cutan Med Surg. 2012 Jul-Aug;16(4):230–244. doi: 10.1177/120347541201600404. [DOI] [PubMed] [Google Scholar]
- 87.Kitamura R, Tsukamoto K, Harada K, et al. Mechanisms underlying the dysfunction of melanocytes in vitiligo epidermis: role of SCF/KIT protein interactions and the downstream effector, MITF-M. J Pathol. 2004 Apr;202(4):463–475. doi: 10.1002/path.1538. [DOI] [PubMed] [Google Scholar]
- 88.Lan CC, Wu CS, Chiou MH, Chiang TY, Yu HS. Low-energy helium-neon laser induces melanocyte proliferation via interaction with type IV collagen: visible light as a therapeutic option for vitiligo. Br J Dermatol. 2009 Aug;161(2):273–280. doi: 10.1111/j.1365-2133.2009.09152.x. [DOI] [PubMed] [Google Scholar]
- 89.Lan CC, Wu CS, Chiou MH, Hsieh PC, Yu HS. Low-energy helium-neon laser induces locomotion of the immature melanoblasts and promotes melanogenesis of the more differentiated melanoblasts: recapitulation of vitiligo repigmentation in vitro. J Invest Dermatol. 2006 Sep;126(9):2119–2126. doi: 10.1038/sj.jid.5700372. [DOI] [PubMed] [Google Scholar]
- 90.Mandel A, Dunaeva LP. Effect of laser therapy on blood levels of serotonin and dopamine scleroderma patients. Vestn Dermatol Venerol. 1982 Aug;(8):13–17. [PubMed] [Google Scholar]
- 91.Mandel AS, Haberman HF, Pawlowski D, Goldstein E. Non PUVA nonsurgical therapies for vitiligo. Clin Dermatol. 1997 Nov-Dec;15(6):907–919. doi: 10.1016/s0738-081x(97)00132-6. [DOI] [PubMed] [Google Scholar]
- 92.Khullar SM, Brodin P, Barkvoll P, Haanaes HR. Preliminary study of low-level laser for treatment of long-standing sensory aberrations in the inferior alveolar nerve. J Oral Maxillofac Surg. 1996 Jan;54(1):2–7. doi: 10.1016/s0278-2391(96)90290-6. discussion 7–8. [DOI] [PubMed] [Google Scholar]
- 93.Anders JJ, Borke RC, Woolery SK, Van de Merwe WP. Low power laser irradiation alters the rate of regeneration of the rat facial nerve. Lasers Surg Med. 1993;13(1):72–82. doi: 10.1002/lsm.1900130113. [DOI] [PubMed] [Google Scholar]
- 94.Rochkind S, Rousso M, Nissan M, Villarreal M, Barr-Nea L, Rees DG. Systemic effects of low-power laser irradiation on the peripheral and central nervous system, cutaneous wounds, and burns. Lasers Surg Med. 1989;9(2):174–182. doi: 10.1002/lsm.1900090214. [DOI] [PubMed] [Google Scholar]
- 95.Mandel A. Skin repigmentation after laser therapy. Vestn Dermatol Venerol. 1984 Sep;(9):26–29. [PubMed] [Google Scholar]
- 96.Yu HS. Treatment of vitiligo vulgaris with helium-neon laser. MB Derma. 2000;35(13–18) [Google Scholar]
- 97.Peacocke M, Yaar M, Mansur CP, Chao MV, Gilchrest BA. Induction of nerve growth factor receptors on cultured human melanocytes. Proc Natl Acad Sci U S A. 1988 Jul;85(14):5282–5286. doi: 10.1073/pnas.85.14.5282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wu CS, Lan CC, Chiou MH, Yu HS. Basic fibroblast growth factor promotes melanocyte migration via increased expression of p125(FAK) on melanocytes. Acta Derm Venereol. 2006;86(6):498–502. doi: 10.2340/00015555-0161. [DOI] [PubMed] [Google Scholar]
- 99.Morelli JG, Yohn JJ, Zekman T, Norris DA. Melanocyte movement in vitro: role of matrix proteins and integrin receptors. J Invest Dermatol. 1993 Oct;101(4):605–608. doi: 10.1111/1523-1747.ep12366064. [DOI] [PubMed] [Google Scholar]
- 100.Hedley SJ, Wagner M, Bielby S, Smith-Thomas L, Gawkrodger DJ, MacNeil S. The influence of extracellular matrix proteins on cutaneous and uveal melanocytes. Pigment Cell Res. 1997 Feb-Apr;10(1–2):54–59. doi: 10.1111/j.1600-0749.1997.tb00466.x. [DOI] [PubMed] [Google Scholar]
- 101.Ma HJ, Zhu WY, Wang DG, Yue XZ, Li CR. Endothelin-1 combined with extracellular matrix proteins promotes the adhesion and chemotaxis of amelanotic melanocytes from human hair follicles in vitro. Cell Biol Int. 2006 Dec;30(12):999–1006. doi: 10.1016/j.cellbi.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 102.Ideta R, Soma T, Tsunenaga M, Ifuku O. Cultured human dermal papilla cells secrete a chemotactic factor for melanocytes. J Dermatol Sci. 2002 Jan;28(1):48–59. doi: 10.1016/s0923-1811(01)00145-1. [DOI] [PubMed] [Google Scholar]
- 103.Takano N, Kawakami T, Kawa Y, et al. Fibronectin combined with stem cell factor plays an important role in melanocyte proliferation, differentiation and migration in cultured mouse neural crest cells. Pigment Cell Res. 2002 Jun;15(3):192–200. doi: 10.1034/j.1600-0749.2002.01079.x. [DOI] [PubMed] [Google Scholar]
- 104.Gibson WT, Couchman JR, Weaver AC. Fibronectin distribution during the development of fetal rat skin. J Invest Dermatol. 1983 Dec;81(6):480–485. doi: 10.1111/1523-1747.ep12522723. [DOI] [PubMed] [Google Scholar]
- 105.Uitto J, Kouba D. Cytokine modulation of extracellular matrix gene expression: relevance to fibrotic skin diseases. J Dermatol Sci. 2000 Dec;24 (Suppl 1):S60–69. doi: 10.1016/s0923-1811(00)00143-2. [DOI] [PubMed] [Google Scholar]
- 106.Wolfram D, Tzankov A, Pulzl P, Piza-Katzer H. Hypertrophic scars and keloids--a review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009 Feb;35(2):171–181. doi: 10.1111/j.1524-4725.2008.34406.x. [DOI] [PubMed] [Google Scholar]
- 107.Bouzari N, Davis SC, Nouri K. Laser treatment of keloids and hypertrophic scars. Int J Dermatol. 2007 Jan;46(1):80–88. doi: 10.1111/j.1365-4632.2007.03104.x. [DOI] [PubMed] [Google Scholar]
- 108.Louw L. The keloid phenomenon: progress toward a solution. Clin Anat. 2007 Jan;20(1):3–14. doi: 10.1002/ca.20374. [DOI] [PubMed] [Google Scholar]
- 109.Uitto J. IL-6 signaling pathway in keloids: a target for pharmacologic intervention? J Invest Dermatol. 2007 Jan;127(1):6–8. doi: 10.1038/sj.jid.5700604. [DOI] [PubMed] [Google Scholar]
- 110.Ghazizadeh M, Tosa M, Shimizu H, Hyakusoku H, Kawanami O. Functional implications of the IL-6 signaling pathway in keloid pathogenesis. J Invest Dermatol. 2007 Jan;127(1):98–105. doi: 10.1038/sj.jid.5700564. [DOI] [PubMed] [Google Scholar]
- 111.Liu W, Wang DR, Cao YL. TGF-beta: a fibrotic factor in wound scarring and a potential target for anti-scarring gene therapy. Curr Gene Ther. 2004 Mar;4(1):123–136. doi: 10.2174/1566523044578004. [DOI] [PubMed] [Google Scholar]
- 112.Barolet D, Boucher A. Prophylactic low-level light therapy for the treatment of hypertrophic scars and keloids: a case series. Lasers Surg Med. 2010 Aug;42(6):597–601. doi: 10.1002/lsm.20952. [DOI] [PubMed] [Google Scholar]
- 113.Hamblin MR, Demidova TN. Mechanisms of low level light therapy – an introduction. Proc SPIE. 2006;6140:61001–61012. [Google Scholar]
- 114.Ablon G. Combination 830-nm and 633-nm light-emitting diode phototherapy shows promise in the treatment of recalcitrant psoriasis: preliminary findings. Photomed Laser Surg. 2010 Feb;28(1):141–146. doi: 10.1089/pho.2009.2484. [DOI] [PubMed] [Google Scholar]