Abstract
Superficial irregularities and certain intrinsic stains on the dental enamel surfaces can be resolved by enamel microabrasion, however, treatment for such defects need to be confined to the outermost regions of the enamel surface. Dental bleaching and resin-based composite repair are also often useful for certain situations for tooth color corrections. This article presented and discussed the indications and limitations of enamel microabrasion treatment. Three case reports treated by enamel microabrasion were also presented after 11, 20 and 23 years of follow-ups.
Keywords: Enamel microabrasion, Dental enamel, Clinical diagnosis, Tooth bleaching
INTRODUCTION
Aesthetics is a primary concern among young patients and represents a challenge to the dentist. Discolored teeth are frequently seen in the general population34.
Many attractive smiles are marred by some discoloration or staining, either on an individual tooth or on all teeth. Isolated yellow, brown, or white areas on an otherwise normal enamel surface, though, are common9,34,36. Improved materials and techniques have been developed to remove or mask discoloration to solve these unaesthetic conditions3,14,35.
Such exogenous stains may be of extrinsic etiology, for example, those caused by food dyes (coffee, tea) or tobacco use, or accumulation of plaque and dental calculus, or intrinsic etiology, which can be congenital or acquired30. Dentinogenesis imperfecta and dental fluorosis are considered congenital intrinsic stains; tetracycline dentin staining or injuries are considered acquired intrinsic staining that may be related to the stages of pre or post eruption13,35. Briefly, enamel discolorations result from hypermineralization, hypomineralization, or staining. Any of these terms are consequences of some abnormality in the formation of the inorganic component of the enamel during amelogenesis14,15.
Proposed treatments, depending on the severity of the enamel stains7, range from invasive ceramic veneer bonding restorations to abrasive chemical treatments. Although aesthetic demands for perfect smiles are increasing, economic problems have also influenced the patients' decisions among the treatment options. More conservative approaches based on cheaper and less time-consuming treatments such as bleaching, micro-abrasive treatments and composite resin restorations are widely used2.
Enamel microabrasion is a conservative method for removing enamel to improve discolorations limited to the outer enamel layer. Sundfeld, et al.36 (2007) noted in an in vitro study that the enamel microabrasion technique results in a loss of enamel of around 25 to 200 μm, depending on the number of applications and acids concentration. The use of various acids to remove enamel stains was described early, in 191626. Since then, many variations of this principle have been described. The enamel microabrasion technique has been suggested for aesthetic improvements, employing a mixture of 18% hydrochloric acid and pumice14 or 6.6% and 10%35 hydrochloric acid with silica carbide particles, or even 37% phosphoric acid gel32 associated with extra fine grain pumice in proportions of equal volume.
The aim of this article was to describe and discuss the treatment of patients with enamel stains. A brief review of laboratory and clinical studies about microabrasion is also presented. In addition, three case reports treated by enamel microabrasion were presented after 11, 20 and 23 years of follow-ups.
CASE REPORTS
In Figure 1 was described the usuall microabrasion technique. A teenage girl had idiopathic white enamel demineralization of her maxillary central incisors (Figure 1A). The enamel microabrasion procedures were performed after enamel macroabrasion of the affected enamel surfaces, using a fine-tapered diamond bur (3195 FF, Kg Sorensen Indústria e Comércio Ltda, Barueri, SP, Brazil) under water and air cooling (Figure 1B). Rubber dam isolation was applied and the dental enamel surface was treated with an application of the microabrasive product (Opalustre, Ultradent Products Inc, South Jordan, UT, USA), three times on each of the three teeth at 60-second intervals (Figure 1C, D and E). Teeth were polished with Herjos F fluoridated prophylaxis paste (Vigodent Coltene SA Indústria e Comércio; Rio de Janeiro, RJ, Brasil). A 2% neutral-Ph sodium fluoride gel was applied for 4 minutes. The immediate enamel aspects were satisfactory (Figure 1F and G).
Figure 1.
A: A teenage girl had idiopathic white enamel demineralization of her maxillary central incisors; B: After dental prophylaxis with pumice and water, a fine-tapered diamond bur was used with water cooling to remove the superficial layer of the stained enamel; C: Before treatment, the patient received eyeglasses for protection and the teeth were isolated with a rubber dam; D and E: Opalustre microabrasive product was applied and compressed upon the enamel surfaces, using a rubber cup manufactured with enclosed brush bristles specifically developed for this purpose. The microabrasion “slurry” was applied with high torque, but very slow speed, to prevent splattering. The compound was applied three times on each of the three teeth for intervals of 60 seconds. The teeth were rinsed with water/air spray after each application; F: The teeth were then dried with an air syringe and polished with fluoridated prophylaxis paste. A 2% neutral-Ph sodium fluoride gel was applied to the treated enamel surfaces and left in place for 4 minutes; G: The treated incisors are shown immediately after enamel microabrasion
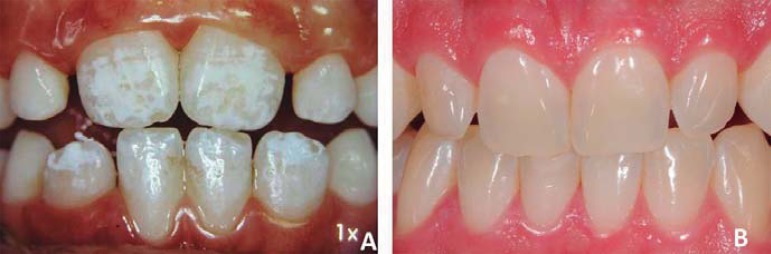
The long-term follow-ups after the enamel microabrasion technique are presented in Figures 2, 3 and 4. Figure 2A presents a 12-year-old girl with idiopathic white enamel demineralization of both the maxillary and mandibular teeth. The microabrasion technique was performed following the steps described in Figure 1. Eleven years from the conclusion of the enamel microabrasion treatment, a new follow-up appointment was scheduled (Figure 2B). It could be noted that the microabraded teeth present a regular, smooth, and lustrous glass-like enamel surface. The worn mesial and incisal surfaces of the maxillary central incisors were reconstructed with composite resin (TPH, Dentsply/Caulk, Milford, DE, USA).
Figure 2.
A: A 12-year-old girl had idiopathic white enamel demineralization of both the maxillary and mandibular teeth; B: The teeth are shown eleven years after the enamel microabrasion. The worn mesial and incisal surfaces of the maxillary central incisors were reconstructed with composite resin, shades A1 and A2
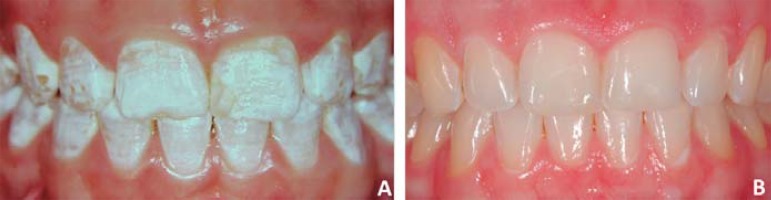
Figure 3.
A: A 9-year-old boy with white enamel demineralization staining of six incisors; B: Twenty years after removal of the white stains on the maxillary central incisors by application of 18% hydrochloric acid and pumice; and after removal of white stains located on the mandibular teeth by application of the PREMA compound. The right mandibular lateral incisor presented a deep white stain; it was restored with resin-based composite
Figure 4.
A: Post-orthodontic white enamel stain of hard texture seen in a young patient; B: 23 years after the removal of stains using 18% hydrochloric acid/pumice and dental bleaching with 15% carbamide peroxide
Figures 3 and 4 present the 20 and 23 year follow-ups, respectively. Figure 3A shows a 9-year-old boy with white stains located only on the dental enamel in the maxillary and mandibular teeth. Stains on the maxillary incisors were removed by the enamel microabrasion technique with an application of 18% hydrochloric acid and pumice. Stains on the mandibular teeth were removed with an application of the enamel microabrasion product PREMA Compound (Premier Dental Products Co, Norristown, PA, USA). The right mandibular lateral incisor presented a deep white stain; it was restored with resin-based composite (Prisma Fill, Dentsply/Caulk, Milford, DE, USA). Figure 3B shows 20 years after the removal of white stains, showing long-term satisfactory results. Figure 4A shows a post-orthodontic white enamel stain of hard texture seen in a young patient. The removal of stains was performed by the enamel microabrasion technique using 18% hydrochloric acid/pumice and dental bleaching with 15% carbamide peroxide (Opalescence, Ultradent Products Inc, South Jordan, UT, USA). Satisfactory aesthetic results can be observed after 23 years (Figure 4B).
However, in some cases the enamel defect cannot be resolved with microabrasion because it penetrates deeper into the enamel (or perhaps even includes the dentin), and a resin-based composite restoration can be accomplished. A teenage boy had deep white enamel stains on the maxillary central incisors (Figure 5A). Tooth preparation for resin-based composite was performed (Figure 5B and C). The teeth were etched for 30 seconds with 35% phosphoric acid (Scotchbond(tm) Etchant, 3M Dental Products Division, St. Paul, MN , USA), Figure 5D. After water rinsing and air drying, a two-step bonding agent was applied (Peak LC Bond, Ultradent Products, Inc., South Jordan, UT, USA). Resin composite restorations were then performed (Vitalescence, Ultradent Products, Inc., South Jordan, UT, USA), as seen in Figure 5E. Complete photo-polymerization was accomplished using a light beam of 1000 mW/cm2 (Ultralux, Dabi Atlante, Ribeirão Preto, SP, Brazil), as seen in Figure 5F. Finishing and polishing were completed using high speed diamond burs (1190F, Kg Sorensen Indústria e Comércio Ltda, Barueri, SP, Brazil) and low speed points (#850 - Jiffy Regular Brushes 10pk) (Jiffy Brushes, Ultradent Products, Inc., South Jordan, USA), as seen in Figure 5G.
Figure 5.
A: A teenage boy had deep white enamel stains on the maxillary central incisors; B: Removal of the remainder of the abnormal white enamel with a fine-tapered diamond bur; C: Tooth preparation for composite resin; D: Etching for 30 seconds with 35% phosphoric acid; E: After water rinsing and air drying, a two-step bonding agent was applied. Resin-based composite restoration was performed; F: Complete photo-polymerization was accomplished using a light beam of 1000 mW/cm²; G: Finishing and polishing were completed using high speed diamond burs and low speed points
A method that can be used for trying to see how deep the white spot is in the enamel is to put a halogen or LED source on the palatal surface and turn it on. If the spot shows its contour and darkens, it may be a deep white spot (Figure 6). Plus, the stains are located on the mid/incisal third, a critical region. Facing this, the patient must be alerted that microabrasion itself probably might not remove the stains and restorative procedures may be necessary.
Figure 6.
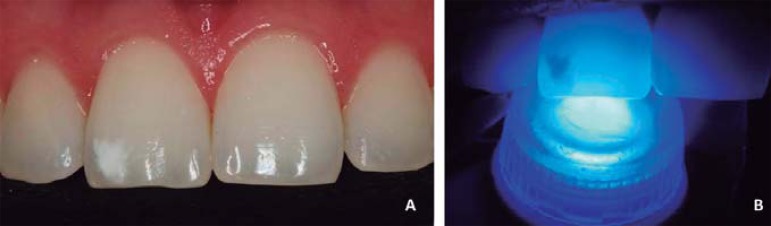
A: Patient with white spots; B: A method that can be used to try to see how deep the white spot in the enamel is to apply a LED source on the palatal surface and turn it on
DISCUSSION
In some cases, there are some difficulties when diagnosing the etiology of the intrinsic enamel stains. When a child ingests excessive amounts of fluoride during the years of amelogenesis, superficial layers of enamel can acquire brown or white chromatic alterations11,20. A diagnostic quandary occurs when such stains are evident, but no history of excessive fluoride ingestion is reported, or possible to be verified. Fluoride is not the only cause of superficial enamel discoloration defects, even though many dentists use "fluorosis" as an all-encompassing description. Some stains can be termed "idiopathic enamel demineralization"11,35 or "fluorosis-like"22.
Intrinsic color alterations may only involve the enamel or dentin, or both. Clinical procedures are used to improve the aspect of the affected teeth, which include: dental bleaching, enamel microabrasion, restorative correction by using tooth colored bonded adhesive materials (porcelain veneers, direct resin-based composite repair, or, in some cases, a combination of procedures)31.
It has been shown that enamel microabrasion using acidic/abrasive products gives immediate and permanent aesthetic results, with insignificant and unrecognizable loss of enamel21,35. The only measure for success is whether the enamel stain surface texture irregularity is confined to the outermost, superficial layer of the enamel10-14,23,35. In the teeth where there are difficulties in diagnosing the depth of the intrinsic stains, it is possible to perform microabrasion with the idea of achieving as much improvement as possible to be followed by other procedures, such as: tooth bleaching or restoration with bonded materials35. Dental bleaching with carbamide peroxide or hydrogen peroxide after enamel microabrasion has been suggested for some patients, since the enamel microabrasion promotes microreduction of the enamel surface6,8,11,35. Microabrasioned teeth can develop a darker shade or yellowish coloration after treatment because the remaining enamel surface is slightly thinner and translucent, so the dentin appears more evident. It has been suggested to wait several weeks after the completion of the microabrasion before bleaching, based on the idea that such a delay will provide ample time for complete enamel surface remineralization with accompanying optical improvement35. Such situation influenced Briso, et al.5 (2013) to evaluate the penetration of hydrogen peroxide applied to microabrasioned enamel, noting that this substrate was more susceptible to hydrogen peroxide diffusion during in-office bleaching5.
The patients' age is not a limiting factor for the enamel microabrasion technique, but there may be difficulties when using the rubber dam on teeth that are not totally erupted. Of course, enamel microabrasion is never indicated when stains are located only within the dentin, such as with dentinogenesis imperfecta or tetracycline discoloration. In patients who have deficient lip sealing (a clinical condition that excessively hinders the formation of a moisturizing pellicle on the enamel, when unprotected by the upper and lower lips), enamel microabrasion can be delayed or contraindicated, because the enamel surfaces are abnormally dry, which makes demineralization stains more apparent. The usual presence of saliva hydrates the enamel and masks such stains by the different light refractions of the enamel surface. Often, these stains are more restricted to the incisal dental third, usually presenting a white opaque coloration and always following the contour of the most common resting position of the upper and lower lips of the patient. All of these characteristics are associated with a judicious examination, and may feature deficient lip sealing. Sundfeld, et al.35, in 2007, found that for the effective disappearance of these stains, lip repositioning should be corrected in some cases.
Orthodontic, educative phonoaudiology techniques for lip or speech therapists may be required to correct lip positioning before enamel microabrasion11,35. However, there may be a correlation of deficient lip sealing with some occlusal changes, requiring a more comprehensive and multidisciplinary evaluation. In clinical cases of lower complexity, deficient lip sealing can be originated by a bad habit constantly repeated by the patient19,37.
Therefore, the treatment of the bad habit can be performed by psychomotor conduction, repositioning the lips - the patient is instructed to do daily exercises during mandibular rest, stimulating them to maintain contact between the upper and lower lips, using a medal attached to a chain, so that the lips keep in touch for the longest period of time possible, thereby, toning the muscle orbicularis of the lips16.
It is appropriate to consider that when facing a white stain with a hard texture, not so evident on the enamel surface, instead of applying microabrasion, it can be camouflage by performing dental bleaching with carbamide or hydrogen peroxide, which act in the dentin tissue, making it lighter2 (Figure 7). It is important to note that after performing dental bleaching on teeth with white stains, they seem more evident after each session because of the dehydration, but after a couple of days they will be rehydrated by the saliva and the stains will be masked.
Figure 7.
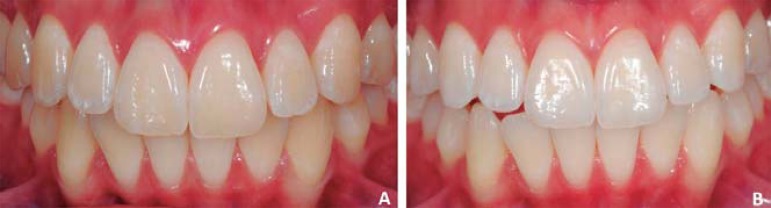
A: Teenage girl, presented with white enamel stain on the maxillary and mandibular teeth; B: After tooth bleaching with 15% carbamide peroxide Opalescence. In some cases, when white stains are small and not prominent, dental bleaching alone using carbamide peroxide or hydrogen peroxide in custom trays may lighten the underlying dentin and enamel sufficiently to camouflage the stain, with no need for microabrasion
Stains and surface irregularities present in the enamel have led researchers to develop materials and techniques for their removal10,12. Croll & Cavanaugh, in 198614 and Sundfeld, et al.35 (2007) proposed the application of a mixture of 18% hydrochloric acid and pumice to try to remove stains with an insignificant loss of enamel (Figure 8). The treatment must be performed with a rubber dam in place, with the patient wearing protective glasses. The mixture is applied with a wooden stick and firm finger pressure for 5 seconds on the stained surface of the enamel, not surpassing a total of 15 applications. Between each application, the enamel submitted to this technique should be washed and dried.
Figure 8.
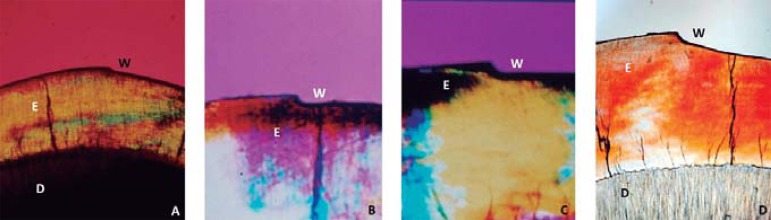
A: Ground tooth section presenting 25 µm enamel loss after 3 applications, of 15 seconds each, of a mixture of 18% hydrochloric acid and pumice (25X); B: 23 µm after 4 applications, of a mixture of Prema Compound enamel microabrasive; C: 42 µm after 4 applications , of 1 minute each, of a mixture of 37% phosphoric acid and pumice; D: 80 µm after, after 4 applications, of 1 minute each, of Opalustre enamel microabrasive. The depression in the enamel convexity (W) designates where the microabrasion was performed. Analyzed by polarized light microscope; E: enamel; D: dentin; W: wear
Trying to obtain an acid/abrasive product that is safer for the oral tissues, the operator, the patient and for an easier application, microabrasive products were developed with a low hydrochloric acid concentration with silicon carbide powder, such as: Opalustre (Ultradent Products Inc, South Jordan, UT, USA), PREMA (Premier Dental Products, Plymouth Meeting, PA, USA) and RM (FGM & Dentscare Ltda, Joinville, SC, Brazil). They are safer and more efficient at slow speed rotary microabrasion15,35. Nahsan, et al.28 (2011) suggested the application of 37% phosphoric acid gel associated with extra fine grain pumice in proportions of equal volume in order to make this technique safer and more practical25,29. Sundfeld, et al.35 (2007) noted that an in vitro application of Opalustre resulted in enamel loss ranging from 25 to 200 μm, corresponding to 1 and 10 applications of the product for one minute on each tooth (Figure 8). It is important to mention that macroabrasion with a fine grit tapered diamond bur can be used to reduce the time needed for the enamel microabrasion technique12,13,35.
In general, in comparing the pre-treatment and the post-treatment control paired analysis, the studies have shown that enamel microabrasion using different compounds is effective in removing stains from the outermost layer of the enamel and improving the appearance of the teeth1,4,8,24,27,30,35. Both phosphoric acid (H3PO4)-pumice and (HCl)-pumice compounds presented effectiveness in treating different severities of dental fluorosis by using the microabrasion technique, however, the mean treatment time with the HCl-pumice was significantly lower than the one with H3PO4-pumice4. In addition, clinically, we have noted that stains are routinely removed with unrecognizable alterations.
It has also been observed that the teeth of patients subjected to enamel microabrasion have a smooth, prism-free layer of enamel and a lustrous surface that increases over time25. This "abrosion effect" (abrasion plus erosion) may be due to the compaction of minerals resulting from the simultaneous erosive and abrasive action of the microabrasion compound on the dental enamel11,17. Fragoso, et al.18 (2011) after evaluating different techniques, concluded that microabrasion followed by polishing with diamond paste or fluoride prophylatic paste provided higher hardness and better surface smoothness of the enamel18. In 1997, Segura, et al.33, through an in vitro polarized microscopic study, showed that enamel after microabrasion technique is more resistant to demineralization than untreated enamel surfaces. In addition, it was observed that there is less colonization by Streptococcusmutans on microabraded enamel.
In assessing stained teeth for enamel microabrasion, bleaching and resin-based composite repair, it is necessary to consider that enamel thickness varies in different crown regions (Figure 9). This makes for more translucency in the incisal third of an anterior tooth, and more opacity as further moving toward the gingival margin. These considerations are important to be remembered when evaluating how much residual enamel there will be after microabrasion, how the tooth will look after bleaching, and what color matching concerns will exist if resin-based composite repair is to be achieved.
Figure 9.
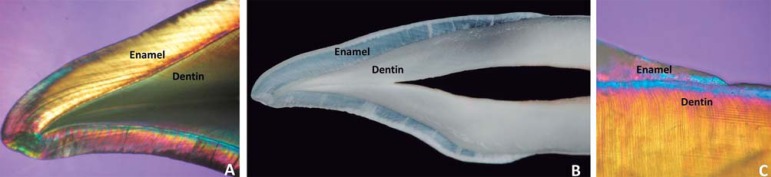
Ground section of an upper incisor tooth - Enamel/dentin interface. A: Incisal third analyzed by polarized light microscope (25X); B. Digital image Nikon D 300 C. Cervical third analyzed by polarized light microscope (25X)
CONCLUSIONS
Correct application of the microabrasion technique, complemented or not by the bleaching or the use of composite resin, allowed for significant improvement in the appearance and color uniformity of the teeth, restoring the patient's self-esteem. Based on these three case reports with long-term follow-ups, it can be concluded that microabrasion was a safe technique, providing favorable results in the patients' smiles overtime.
ACKNOWLEDGEMENT
The authors are gratefull to Dr. Juvenal Alves for authorizing the publication of Figures 8B and 8C.
REFERENCES
- 1.Akin M, Basciftci FA. Can white spot lesions be treated effectively? Angle Orthodontist. 2012;82:770–775. doi: 10.2319/090711.578.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ardu S, Benbachir N, Stavridakis M, Dietschi D, Krejci I, Feilzer A. A combined chemo-mechanical approach for aesthetic management of superficial enamel defects. Br Dent J. 2009;206:205–208. doi: 10.1038/sj.bdj.2009.116. [DOI] [PubMed] [Google Scholar]
- 3.Bailey RW, Christen AG. Effects of a bleaching technic on the labial enamel of human teeth stained with endemic dental fluorosis. J Dent Res. 1970;49:168–170. doi: 10.1177/00220345700490011201. [DOI] [PubMed] [Google Scholar]
- 4.Bassir MM, Bagheri G. Comparison between phosphoric acid and hydrochloric acid in microabrasion technique for the treatment of dental fluorosis. J Conserv Dent. 2013;16:41–44. doi: 10.4103/0972-0707.105297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Briso A, Lima A, Goncalves R, Gallinari M, Santos PD. Transenamel and transdentinal penetration of hydrogen peroxide applied to cracked or microabrasioned enamel. Oper Dent. 2014;39:166–173. doi: 10.2341/13-014-L. [DOI] [PubMed] [Google Scholar]
- 6.Castro KS, Araújo Ferreira AC, Duarte RM, Sampaio FC, Meireles SS. Acceptability, efficacy and safety of two treatment protocols for dental fluorosis: a randomized clinical trial. J Dent. 2014 doi: 10.1016/j.jdent.2014.01.011. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Celik EU, Yildiz G, Yazkan B. Clinical evaluation of enamel microabrasion for the aesthetic management of mild-to-severe dental fluorosis. J Esthet Restor Dent. 2013;25:422–430. doi: 10.1111/jerd.12052. [DOI] [PubMed] [Google Scholar]
- 8.Celik EU, Yildiz G, Yazkan B. Comparison of enamel microabrasion with a combined approach to the esthetic management of fluorosed teeth. Oper Dent. 2013;38:134–143. doi: 10.2341/12-317-C. [DOI] [PubMed] [Google Scholar]
- 9.Chhabra N, Singbal KP. Viable approach to manage superficial enamel discoloration. Contemp Clin Dent. 2010;1:284–287. doi: 10.4103/0976-237X.76404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Croll TP. Enamel microabrasion for removal of superficial dysmineralization and decalcification defects. J Am Dent Assoc. 1990;120:411–415. doi: 10.14219/jada.archive.1990.0127. [DOI] [PubMed] [Google Scholar]
- 11.Croll TP. Enamel microabrasion. Chicago: Quintessence; 1991. [Google Scholar]
- 12.Croll TP. Hastening the enamel microabrasion procedure eliminating defects, cutting treatment time. J Am Dent Assoc. 1993;124:87–90. doi: 10.14219/jada.archive.1993.0083. [DOI] [PubMed] [Google Scholar]
- 13.Croll TP, Bullock GA. Enamel microabrasion for removal of smooth surface decalcification lesions. J Clin Orthod. 1994;28:365–370. [PubMed] [Google Scholar]
- 14.Croll TP, Cavanaugh RR. Enamel color modification by controlled hydrochloric acid-pumice abrasion. I. technique and examples. Quintessence Int. 1986;17:81–87. [PubMed] [Google Scholar]
- 15.Croll TP, Segura A, Donly KJ. Enamel microabrasion: new considerations in 1993. Pract Periodontics Aesthet Dent. 1993;5:19–28. quiz 29. [PubMed] [Google Scholar]
- 16.Dixit UB, Shetty RM. Comparison of soft-tissue, dental, and skeletal characteristics in children with and without tongue thrusting habit. Contemp Clin Dent. 2013;4:2–6. doi: 10.4103/0976-237X.111585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donly KJ, O'Neill M, Croll TP. Enamel microabrasion: a microscopic evaluation of the "abrosion effect". Quintessence Int. 1992;23:175–179. [PubMed] [Google Scholar]
- 18.Fragoso LS, Lima DA, Alexandre RS, Bertoldo CE, Aguiar FH, Lovadino JR. Evaluation of physical properties of enamel after microabrasion, polishing, and storage in artificial saliva. Biomed Mater. 2011;6(3):035001. doi: 10.1088/1748-6041/6/3/035001. [DOI] [PubMed] [Google Scholar]
- 19.Fujimoto S, Yamaguchi K, Gunjigake K. Clinical estimation of mouth breathing. Am J Orthod Dentofacial Orthop. 2009;136:630–637. doi: 10.1016/j.ajodo.2009.03.034. [DOI] [PubMed] [Google Scholar]
- 20.Haywood VB, Heymann HO. Nightguard vital bleaching: how safe is it? Quintessence Int. 1991;22:515–523. [PubMed] [Google Scholar]
- 21.Kendell RL. Hydrochloric acid removal of brown fluorosis stains: clinical and scanning electron micrographic observations. Quintessence Int. 1989;20:837–839. [PubMed] [Google Scholar]
- 22.Killian CM. Conservative color improvement for teeth with fluorosis-type stain. J Am Dent Assoc. 1993;124:72–74. doi: 10.14219/jada.archive.1993.0111. [DOI] [PubMed] [Google Scholar]
- 23.Killian CM, Croll TP. Enamel microabrasion to improve enamel surface texture. J Esthet Dent. 1990;2:125–128. doi: 10.1111/j.1708-8240.1990.tb00627.x. [DOI] [PubMed] [Google Scholar]
- 24.Limeback H, Vieira AP, Lawrence H. Improving esthetically objectionable human enamel fluorosis with a simple microabrasion technique. Eur J Oral Sci. 2006;114:123–129. doi: 10.1111/j.1600-0722.2006.00317.x. [DOI] [PubMed] [Google Scholar]
- 25.Machado LS, Sundfeld D, Neto, Oliveira GB, Carvalho TC, Oliveira FG, Sundfeld RH. Combining enamel microabrasion and dental bleaching: recovering smile aesthetics. Dent Today. 2013;32:110–111. [PubMed] [Google Scholar]
- 26.McCloskey RJ. A technique for removal of fluorosis stains. J Am Dent Assoc. 1984;109:63–64. doi: 10.14219/jada.archive.1984.0297. [DOI] [PubMed] [Google Scholar]
- 27.Murphy TC, Willmot DR, Rodd HD. Management of postorthodontic demineralized white lesions with microabrasion: a quantitative assessment. Am J Orthod Dentofacial Orthop. 2007;131:27–33. doi: 10.1016/j.ajodo.2005.04.041. [DOI] [PubMed] [Google Scholar]
- 28.Nahsan FP, Silva LM, Baseggio W, Franco EB, Francisconi PA, Mondelli RF, et al. Conservative approach for a clinical resolution of enamel white spot lesions. Quintessence Int. 2011;42:423–426. [PubMed] [Google Scholar]
- 29.Paula A, Santos PH, Oliveira FG, Machado LS, Neto DS, Sundfeld RH. Integrating techniques to restore an adolescent's smile. Dent Today. 2012;31:88, 90–91. [PubMed] [Google Scholar]
- 30.Price RB, Loney RW, Doyle MG, Moulding MB. An evaluation of a technique to remove stains from teeth using microabrasion. J Am Dent Assoc. 2003;134:1066–1071. doi: 10.14219/jada.archive.2003.0320. [DOI] [PubMed] [Google Scholar]
- 31.Reston EG, Corba DV, Ruschel K, Tovo MF, Barbosa AN. Conservative approach for esthetic treatment of enamel hypoplasia. Oper Dent. 2011;36:340–343. doi: 10.2341/10-189-T. [DOI] [PubMed] [Google Scholar]
- 32.Rodrigues MC, Mondelli RF, Oliveira GU, Franco EB, Baseggio W, Wang L. Minimal alterations on the enamel surface by micro-abrasion: in vitro roughness and wear assessments. J Appl Oral Sci. 2013;21:112–117. doi: 10.1590/1678-7757201302117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Segura A, Donly KJ, Wefel JS, Drake D. Effect of enamel microabrasion on bacterial colonization. Am J Dent. 1997;10:272–274. [PubMed] [Google Scholar]
- 34.Sheoran N, Garg S, Damle SG, Dhindsa A, Opal S, Gupta S. Esthetic management of developmental enamel opacities in young permanent maxillary incisors with two microabrasion techniques - a split mouth study. J Esthet Restor Dent. 2014 doi: 10.1111/jerd.12096. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 35.Sundfeld RH, Croll TP, Briso AL, Alexandre RS, Sundfeld D., Neto Considerations about enamel microabrasion after 18 years. Am J Dent. 2007;20:67–72. [PubMed] [Google Scholar]
- 36.Sundfeld RH, Rahal V, Croll TP, De Alexandre RS, Briso AL. Enamel microabrasion followed by dental bleaching for patients after orthodontic treatment - case reports. J Esthet Restor Dent. 2007;19:71–77. doi: 10.1111/j.1708-8240.2007.00069.x. [DOI] [PubMed] [Google Scholar]
- 37.Yamaguchi K, Morimoto Y, Nanda RS, Ghosh J, Tanne K. Morphological differences in individuals with lip competence and incompetence based on electromyographic diagnosis. J Oral Rehabil. 2000;27:893–901. doi: 10.1046/j.1365-2842.2000.00596.x. [DOI] [PubMed] [Google Scholar]