Abstract
Purpose
Children are particularly vulnerable to the harmful effects of medical radiation, and children with urolithiasis are one group who may receive repeated radiation-intensive imaging tests. Our study aimed to characterize imaging practices for children presenting to the emergency department (ED) with suspected urolithiasis (SU) and determine factors associated with the choice of imaging study.
Methods
Using the 2006-10 Nationwide Emergency Department Sample (NEDS), we conducted a retrospective cohort study of patients <18 years old presenting with SU. We determined imaging practices for visits in EDs where billing codes for computed tomography (CT) and ultrasound were reliably reported. Logistic regression was used to delineate patient- and hospital-level factors associated with the use of CT vs. ultrasound.
Results
There were 18096 pediatric SU visits in the 1191 NEDS EDs with reliable imaging codes. Of the 11215 patients receiving a CT alone, an ultrasound alone, or both, 9773 (87%) were imaged with CT alone. CT use peaked in 2007, and declined thereafter. On multivariate analysis, the following factors were associated with the use of CT alone: lower proportion of pediatric patients treated in the ED, older age, location in the Midwest or South, evaluation at a non-teaching hospital, and visit on a weekend.
Conclusions
CT use is highly prevalent for children presenting with SU. The lowest CT use is in EDs that care for more children. Ultrasound is used very infrequently regardless of site. Awareness regarding risks of CT and consideration of alternatives including ultrasound are warranted in caring for these patients.
Keywords: Urolithiasis, kidney stones, radiation, computed tomography, ultrasound, national practice patterns, emergency care, pediatrics
Introduction
Over the last two decades, a consensus developed that the gold standard for evaluation of suspected urolithiasis (SU) is the non-contrast computed tomography (NCCT) scan.1, 2 However, multiple recent studies have established a link between radiation exposure from CTs in children and subsequent cancer risk.3, 4 Give such concerns, the radiology community developed the “As Low As Reasonably Achievable” (ALARA) principle to guide imaging choices.5, 6
Previous investigations have evaluated the utility of alternative imaging algorithms for SU in pediatric patients, comparing NCCT with ultrasound. Although NCCT is somewhat more sensitive for stone detection, in approximately 75% of cases children can be evaluated and treated for urolithiasis without NCCT.7, 8 While there has been intensive attention to ALARA and CT alternatives at pediatric centers, approximately 90% of emergency care for children in the United States (US) is provided at adult-focused hospitals;9 these hospital systems may not be as equipped to execute ALARA-based strategies in children compared with pediatric centers
We sought to describe the national utilization of CT versus ultrasound imaging for pediatric patients seen in EDs for SU. Our aims were to (1) determine whether pediatric-focused EDs use less ionizing radiation when evaluating SU in children compared with adult-focused EDs, and (2) identify patient and facility characteristics associated with increased likelihood of undergoing CT.
Materials and Methods
Study Design and Data Source
We conducted a retrospective cohort study of children aged 0-17 years evaluated in EDs throughout the US for urolithiasis and/or flank pain. We utilized the 2006-2010 Nationwide Emergency Department Sample (NEDS), a large, nationally representative database of ED visits. The NEDS was developed and is maintained by the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality, and consists of combined records from HCUP State ED and State Inpatient Databases. NEDS datasets are constructed annually using a sampling scheme that approximates a 20% stratified sample of hospital-based EDs nationally, allowing for the calculation of national estimates of ED visit parameters. The study was determined to be exempt by our hospital’s institutional review board.
Selection of Participants
We identified all ED visits where the patient was <18 years old and had an ICD-9 billing code for urolithiasis (592.0, 592.1, and/or 274.11), and/or renal colic (788.0). We created an algorithm to identify hospitals which reliably report codes for CT and ultrasound within the ED. (Codes for imaging procedures performed at certain facilities may not appear in the NEDS database due to billing factors such as a private radiology group servicing a given hospital, thus generating a separate bill). A hospital was designated as reliably coding the relevant radiologic tests for a given study year if they billed for at least 1 abdominal CT and 1 abdominal for a diagnosis of abdominal pain or appendicitis during that study year. Only patients seen in EDs at one of these “reliable coding” hospitals were included in the final analysis cohort.
Variables Examined
We extracted multiple patient-level variables from the dataset including age, insurance status, gender, income quartile (stratified by patient zip code), disposition status, weekday vs. weekend visit and comorbidities. Comorbidities were classified according to organ system-based categories. There were an insufficient number of infants in the cohort to be used in the final analyses.
If patients >19 years old made up >90% of patients seen in a given ED for any diagnosis, then that hospital was classified as non-pediatric-focused, using a previously published definition.10 We also stratified hospitals by quartiles of rate of pediatric patients seen at each hospital for any diagnosis: 1st quartile hospitals had the lowest percentage of pediatric patients and 4th quartile hospitals had the highest percentage of pediatric patients. This stratification resulted in the following groupings: 1st quartile: 0%-19.2% pediatric patients; 2nd quartile: 19.3-23.1% pediatric patients; 3rd quartile: 23.1-26.6% pediatric patients; 4th quartile: 26.6-100% pediatric patients. Other hospital-level characteristics examined included US Census Region, urban-rural location and teaching hospital status.
Outcome Measures
The primary outcome was the imaging that occurred during each ED visit. Our goal was to compare the utilization of CT versus ultrasound specifically. Therefore, patients who received no imaging, and those receiving only plain x-ray, were excluded from the dataset used to analyze imaging strategies. Patients who received x-ray in addition to CT and/or ultrasound were included and classified according to their receipt of CT and/or ultrasound. Patients undergoing the imaging modalities of interest were then grouped as follows: Group 1 received CT alone, and Group 2 received an ultrasound alone, or ultrasound and CT. The rationale for including patients who received both a CT and an ultrasound into Group 2 was that clinical situations exist where an ultrasound done for SU first could be equivocal and necessitate a CT for clarification or confirmation of a diagnosis. As we were not able to determine chronological order of the studies from this database, it seemed reasonable to assume that, in cases where both imaging studies were performed, the ultrasound was likely the initial study. However, it is plausible that a CT was done first in some patients, with an ultrasound done subsequently to establish a baseline for follow-up. Nevertheless, it seemed reasonable to give the benefit of the doubt and classify these cases with others who underwent ultrasound-only evaluation, and assume ultrasound was the initial study.
Statistical Analysis
Descriptive statistics were used to characterize the population of children with SU who were seen at “reliable coding” NEDS EDs, as well as the subset of patients contained within our analytic cohort who received CT alone, or ultrasound +/- CT. Groups 1 (CT alone) and 2 (ultrasound +/-CT) were compared using chi-squared tests to examine the bivariate relationships between choice of imaging modality and potentially relevant patient- and hospital-level factors. Weighted logistic regression was then performed to determine adjusted bivariate and multivariate associations between patient- and hospital-level factors and the outcome of CT administration alone (versus ultrasound +/- CT). Variables were entered into our regression model based on statistical significance on bivariate analyses, taking into consideration collinearity among several hospital-level factors.
Data analysis was conducted using SAS v9.3 (Copyright 2002-2010 by SAS Institute Inc., Cary, NC, USA). Weighted analyses were based on the NEDS stratified sampling scheme using the weight, cluster and strata variables provided by HCUP. A p-value of <0.05 was considered significant.
Results
Characteristics of Study Subjects
We identified 30,045 pediatric ED visits for SU, representing a weighted total of 134,834 visits nationally from 2006-2010 (95% confidence interval (CI) 127,494-142,175). Of these, 18,096 were at hospitals that reliably coded for CT and ultrasound, and 11,215 visits had a CT and/or an ultrasound performed. The characteristics of all patients seen in EDs that reliably reported radiologic codes, as well as the subset in our analysis dataset, are illustrated in Table 1. For the reliably reported cohort, the majority of patients were adolescent (79.3%), female (62.3%), privately insured (56.9%) and evaluated in the South (57.8%). The most notable difference between the reliably reported and analytic cohorts was the percentage of patients admitted to the hospital (13.2% vs. 1.7%, respectively). Otherwise, the cohorts were similar with respect to all other parameters examined.
Table 1.
Characteristics of pediatric patients seen in US EDs from 2006-2010 for suspected urolithiasis
| Characteristic | Number of visits (%) | |
|---|---|---|
|
| ||
| Reliably reported cohort (N = 18096) | Analysis cohort (N=11215) | |
|
| ||
| Total number of hospitals represented | 1191 | 1105 |
|
| ||
| Yearly visits per hospital (median, IQR) | 8 [3, 17] | 6 [2, 12] |
|
| ||
| Year | ||
| 2006 | 2769 (15.3) | 1664 (14.8) |
| 2007 | 3036 (16.8) | 1724 (15.4) |
| 2008 | 3921 (21.7) | 2446 (21.8) |
| 2009 | 4008 (22.2) | 2570 (22.9) |
| 2010 | 4362 (24.1) | 2811 (25.1) |
|
| ||
| Age | ||
| Infants (<1 year) | 223 (1.3) | NA* |
| Young children (1-4 years) | 308 (1.7) | 61 (0.54) |
| School-aged children (5-12 years) | 3179 (17.6) | 1778 (15.9) |
| Adolescents (13-17 years) | 14356 (79.3) | 9376 (83.6) |
| Unknown | 20 (0.11) | 0 (0) |
|
| ||
| Gender | ||
| Male | 5176 (37.7) | 4253 (37.9) |
| Female | 8556 (62.3) | 6962 (62.1) |
| Unknown | 7 (0.01) | 0 (0) |
|
| ||
| Insurance status | ||
| Private | 10302 (56.9) | 6720 (59.9) |
| Public | 5457 (30.2) | 3017 (26.9) |
| Other | 2272 (12.6) | 1441 (12.9) |
| Unknown | 65 (0.42) | 37 (0.33) |
|
| ||
| Comorbidities | ||
| Any comorbidity | 3778 (20.9) | 1828 (16.3) |
| Cardiac | 264 (1.5) | 80 (0.71) |
| Pulmonary | 1006 (5.6) | 459 (4.1) |
| Gastrointestinal | 1391 (7.7) | 625 (5.6) |
| Endocrine | 238 (1.3) | 97 (0.86) |
| Oncologic | 52 (0.29) | 18 (0.16) |
| Hematologic | 310 (1.7) | 115 (1.0) |
| Neurologic | 540 (3.0) | 170 (1.5) |
| Psychiatric | 1200 (6.6) | 558 (5.0) |
| Autoimmune | 127 (0.70) | 42 (0.37) |
|
| ||
| Region | ||
| Northeast | 3994 (22.1) | 2485 (22.2) |
| Midwest | 1885 (10.4) | 1008 (9.0) |
| South | 10462 (57.8) | 6706 (59.8) |
| West | 1755 (9.7) | 1016 (9.1) |
|
| ||
| Median household income zip code quartile | ||
| 1 ($1-39,999) | 4630 (25.6) | 2753 (24.6) |
| 2 ($40,000-40,999) | 4722 (26.1) | 2904 (25.9) |
| 3 (50,000-65,000) | 4306 (23.8) | 2639 (23.5) |
| 4 ($66,000+) | 4109 (22.7) | 2747 (24.5) |
| Unknown | 329 (1.8) | 172 (1.5) |
|
| ||
| Pediatric-focused hospital | 620 (3.4) | 173 (1.5) |
|
| ||
| Percentage of pediatric patients seen in ED (quartiles) | ||
| 1 (fewest pediatric patients) | 3680 (20.3) | 2496 (22.3) |
| 2 | 4176 (23.1) | 2683 (23.9) |
| 3 | 4156 (23.0) | 2614 (23.3) |
| 4 (most pediatric patients) | 6084 (33.6) | 3442 (30.5) |
|
| ||
| Rural/urban status | ||
| Urban | 14997 (82.9) | 9270 (82.7) |
| Suburban or rural | 3099 (17.1) | 1945 (17.3) |
|
| ||
| Teaching hospital | 6753 (37.3) | 3659 (32.6) |
|
| ||
| Disposition status | ||
| Discharged | 15709 (86.8) | 11023 (98.3) |
| Admitted | 2387 (13.2) | 192 (1.71) |
|
| ||
| Day seen | ||
| Weekday | 13179 (72.8) | 8156 (72.7) |
| Weekend | 4916 (27.2) | 3058 (27.3) |
| Unknown | 1 (0.01) | 1 (0.01) |
|
| ||
| Imaging strategy | ||
| Any imaging reported | 11926 (65.9) | 11215 (100) |
| CT | 7905 (56.3) | 10185 (90.8) |
| Ultrasound | 1457 (8.1) | 1442 (12.9) |
| Abdominal X-ray | 2040 (11.3) | 1388 (12.4) |
| Intravenous pyelogram | 63 (0.35) | 13 (0.12) |
|
| ||
| Coded diagnosis | ||
| Urolithiasis +/- flank pain | 14687 (81.2) | 9448 (84.2) |
| Flank pain only | 3409 (18.8) | 1767 (15.8) |
Infants excluded from analysis dataset due to insufficient sample size
Principal Findings
Figure 1 illustrates the distribution of imaging practices for pediatric ED patients with SU. Among the overall cohort, 48% of patients received a CT alone. Other combinations of imaging comprised 18% of patients, and 34% had no imaging during the ED visit. In all, <9% of patients received an ultrasound.
Figure 1.
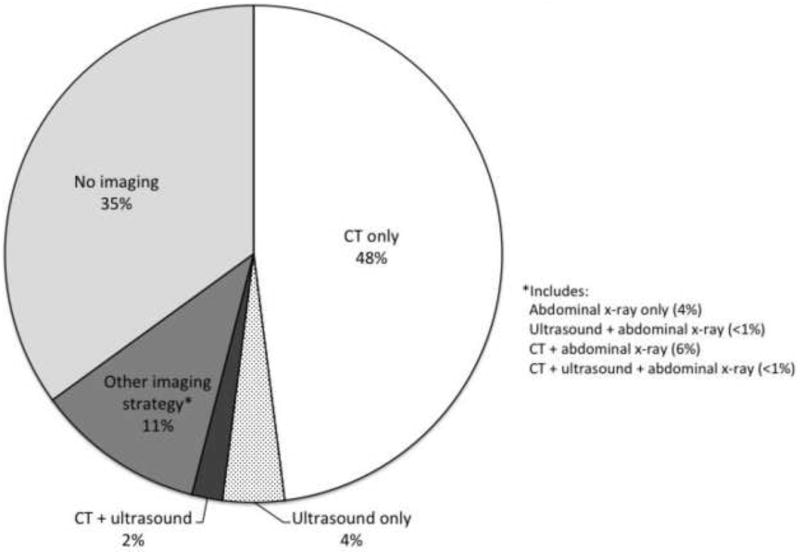
Distribution or imaging studies for pediatric patients with suspected urolithiasis
Among the analytic cohort (n=11,215), patients in Group 1 (CT alone, n=9,773 (87.1%)) were compared with patients in Group 2 (ultrasound +/- CT, n=1,442 (12.9%)) to determine associations with the use of CT alone. CT use appeared to peak in 2007, then decline gradually from 2007-2010 (Figure 2, p<0.0001, Chi-squared trend test). On bivariate analysis (Table 2), patient-level factors associated with the use of CT alone (vs. ultrasound +/- CT) included older age and male gender. Other notable risk factors for higher use of CT alone included hospital location in the Midwest or South, evaluation in an ED that treated a lower percentage of pediatric patients, suburban/rural hospital location, non-teaching hospital status, and evaluation on a weekend. On multivariate modeling (Table 3), the following factors remained significant: lower percentage of pediatric patients seen in the ED, earlier study year, older age, male gender, location in the Midwest or South (vs. Northeast), and weekend visit.
Figure 2.
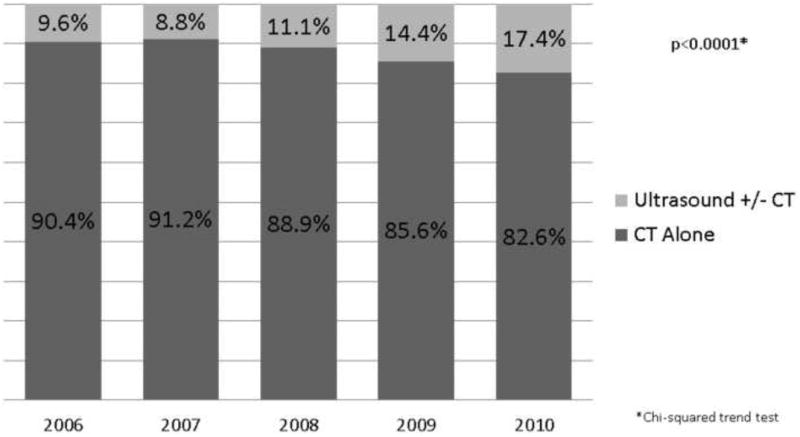
Use of CT alone (vs. ultrasound +/- CT) by study year
Table 2.
Association between patient and hospital factors and CT vs. ultrasound usage in children with suspected urolithiasis
| Characteristic | Group 1-CT only | Group 2 - Ultrasound +/- CT | p-value |
|---|---|---|---|
|
| |||
| Overall (N = 11215) | 9773 (87.1) | 1442 (12.9) | -- |
|
| |||
| Year | <0.0001 | ||
| 2006 | 1505 (90.4) | 159 (9.6) | |
| 2007 | 1572 (91.2) | 152 (8.8) | |
| 2008 | 2175 (88.9) | 271 (11.1) | |
| 2009 | 2199 (85.6) | 371 (14.4) | |
| 2010 | 2332 (82.6) | 489 (17.4) | |
|
| |||
| Age | <0.0001 | ||
| Young children (1-4 years) | 30 (49.2) | 31 (50.8) | |
| School-aged children (5-12 years) | 1451 (81.6) | 327 (18.4) | |
| Adolescents (13-17 years) | 8292 (88.4) | 1084 (11.6) | |
|
| |||
| Gender | 0.001 | ||
| Male | 3764 (88.5) | 489 (11.5) | |
| Female | 6009 (86.3) | 953 (13.7) | |
|
| |||
| Insurance status (N=11178) | 0.23 | ||
| Private | 5829 (86.7) | 891 (13.3) | |
| Public | 2640 (87.5) | 377 (12.5) | |
| Other | 1272 (88.3) | 169 (11.7) | |
|
| |||
| Comorbid condition present | 1570 (85.9) | 258 (14.1) | 0.08 |
|
| |||
| Region | <0.0001 | ||
| Northeast | 1987 (80.0) | 498 (20.0) | |
| Midwest | 917 (91.0) | 91 (9.0) | |
| South | 6035 (90.0) | 971 (10.0) | |
| West | 834 (82.1) | 182 (17.9) | |
|
| |||
| Median Household Income Zip Code Quartile (N = 11043) | <0.0001 | ||
| 1 ($1-39,999) | 2471 (89.8) | 282 (10.2) | |
| 2 ($40,000-40,999) | 2590 (89.2) | 314 (10.8) | |
| 3 (50,000-65,000) | 2299 (87.1) | 340 (12.9) | |
| 4 ($66,000+) | 2258 (82.2) | 489 (17.8) | |
|
| |||
| Pediatric-focused hospital | 109 (63.0) | 64 (37.0) | <0.0001 |
|
| |||
| Percentage of pediatric patients seen in ED (quartiles) | <0.0001 | ||
| 1 (fewest pediatric patients) | 2216 (88.8) | 280 (11.2) | |
| 2 | 2451 (91.4) | 232 (8.7) | |
| 3 | 2342 (89.6) | 272 (10.4) | |
| 4 (most pediatric patients) | 2764 (80.8) | 658 (19.2) | |
|
| |||
| Rural/Urban Status | <0.0001 | ||
| Urban | 7943 (85.7) | 1327 (14.3) | |
| Suburban or rural | 1327 (94.1) | 115 (5.9) | |
|
| |||
| Teaching Hospital | 2916 (79.7) | 743 (20.3) | <0.0001 |
|
| |||
| Disposition Status | 0.91 | ||
| Discharged | 9602 (87.1) | 1421 (12.9) | |
| Admitted | 171 (89.1) | 21 (10.9) | |
|
| |||
| Day Seen (N= 11214) | <0.0001 | ||
| Weekday | 7031 (86.2) | 1125 (13.8) | |
| Weekend | 2741 (89.6) | 317 (10.4) | |
|
| |||
| Coded Diagnosis | 0.0009 | ||
| Urolithiasis +/- flank pain | 7824 (87.7) | 1100 (12.3) | |
| Flank pain only | 1949 (85.1) | 342 (14.9) | |
Table 3.
Unadjusted and adjusted predictors* of use of CT alone in children with suspected urolithiasis
| Characteristic | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Odds Ratio | 95% CI | p-value | Odds Ratio | 95% CI | p-value | |
|
| ||||||
| 1st (lowest) quartile of pediatric patients (vs. highest quartile) | 1.66 | (1.23-2.22) | <0.0001 | 1.53 | (1.31-1.80) | <0.001 |
|
| ||||||
| Year | <0.0001 | <0.0001 | ||||
| 2006 (ref) | ||||||
| 2007 | 1.40 | (0.91-2.14) | 1.11 | (0.87-1.41) | ||
| 2008 | 0.97 | (0.67-1.41) | 0.77 | (0.62-0.95) | ||
| 2009 | 0.63 | (0.43-0.93) | 0.58 | (0.47-0.71) | ||
| 2010 | 0.52 | (0.36-0.76) | 0.42 | (0.34-0.51) | ||
|
| ||||||
| Age Category | <0.0001 | <0.0001 | ||||
| Young children (1-4 years) (ref) | ||||||
| School-aged children (5-12 years) | 4.96 | (2.95-8.33) | 4.32 | (2.49-7.48) | ||
| Adolescents (13-17 years) | 9.35 | (5.53-15.80) | 7.62 | (4.44-13.09) | ||
|
| ||||||
| Male Gender | 1.14 | (0.99-1.32) | 0.07 | 1.41 | (1.24-1.59) | <0.0001 |
|
| ||||||
| Region | <0.0001 | <0.0001 | ||||
| Northeast (ref) | ||||||
| Midwest | 2.67 | (1.56-4.57) | 2.61 | (2.04-3.33) | ||
| South | 2.31 | (1.78-2.99) | 2.03 | (1.77-2.32) | ||
| West | 1.23 | (0.90-1.70) | 0.99 | (0.81-1.21) | ||
|
| ||||||
| Non-teaching Hospital | 2.42 | (1.92-3.06) | <0.0001 | 1.97 | (1.74-2.24) | <0.0001 |
|
| ||||||
| Weekend Day | 1.41 | (1.20-1.65) | <0.0001 | 1.36 | (1.18-1.56) | <0.0001 |
Weighted logistic regression
Discussion
Our results confirm those of previous investigations evaluating trends in ED CT utilization for pediatric patients, and validate these findings in a large dataset of SU patients. Prior population-level studies have suggested CT use in the ED steadily increased from 1995-2008 overall,9 and from 1999-2007 for abdominal pain specifically.10 Using NHAMCS data, Hryhorchuk and colleagues noted higher CT use in non-pediatric hospitals for patients with abdominal pain,10 mirroring our findings for children with SU.
Investigators have also used NHAMCS data to quantify the increase in CT utilization for patients with SU. Kocher and colleagues noted an increase in CT use for patients of all ages seen in EDs from 1997-2006, and noted that the rates of increase were highest for flank pain diagnoses (OR 9.24 for 2007 vs. 1996). 11 Westphalen and colleagues found an increase in CT utilization from 4% to 43% between 1996 and 2007 for adults seen in the ED for flank pain.
In contrast to the general pediatric and more specific adult NHAMCS data, there is a paucity of population-level data regarding the imaging practices for children with SU. A study of 84 children in Minnesota noted an increase in CT rates from 10% during the time period from 1984-1996 compared with 82% from 1997-2008.12 Our group previously found increased CT rates from 26% in 1999 to 45% in 2008 for children treated for urolithiasis at freestanding children’s hospitals; associations of CT use included older age, public insurance and treating hospital.13
Our present study confirms the high recent rates of CT use seen in the more limited samples previously available. We also confirm the finding that older age is associated with increased CT use, although we did not find an association between insurance status and CT use nationally. Our findings with regard to hospital region and teaching hospital status also indirectly support the notion that significant variation exists by hospital, although we did not examine hospitals individually. More broadly, multiple factors independent of specific patient characteristics were associated with the use of CT.
Another notable finding from our study was the proportion of patients with no imaging study during their visit (34%). We speculate that this could represent patients who had undergone recent imaging who were returning for recurrent symptoms, or those who brought their own imaging studies with them from another hospital. The supposition that these patients represent those with recurrent symptoms is supported by the higher admission rate for the entire cohort compared with those who underwent a CT and/or an ultrasound. A limitation of the NEDS dataset is the inability to track patients across visits, so we were unable to further explore the patient group with no imaging studies.
Our data also suggest that CT use in the ED has peaked, and appears to be slowly decreasing. Several smaller studies have demonstrated similar trends at children’s hospitals;14, 15 we further document this trend among pediatric patients seen primarily at general hospitals. However, the fact remains that a majority of children receiving imaging are still being imaged with CT alone. As most patients (97%) were treated in general-care facilities, and given our finding that facilities with higher proportions of pediatric patients were less likely to use CT alone, we speculate that attention to radiation dosing and/or systems factors facilitating ALARA-based imaging strategies for pediatric patients may be less pronounced at general-care vs. pediatric facilities.
Given these realities, we suggest a hospital-level approach incorporating a systematic strategy for dose reduction via the use of ultrasound and/or low-dose CT scanners and protocols. One specific strategy could include a protocol of renal ultrasound plus an abdominal x-ray, with the use of CT only in equivocal cases. Although less sensitive and specific than the use of NCCT upfront, this concept has shown promise as a strategy for balancing diagnostic capabilities and radiation exposure in both adults,16 and in children.7, 8 A similar approach has been successfully implemented for pediatric patients with suspected appendicitis presenting to the ED.17
Despite the appeal of a staged ultrasound +/- CT protocol, this approach may not be realistic for all hospitals or at all times. For example, Burr and colleagues noted that for pediatric ED patients with abdominal pain, CT was done more commonly during nighttime hours;18 our data show higher CT use on weekends. A staged approach would require availability of both CT and ultrasound imaging equipment and personnel at all times; this may not be feasible for every facility. Implementation of radiation dose reduction strategies may be a more attainable goal that can be more consistently applied. Data from both the adult19-23 and pediatric24 literature demonstrate that CT dose reductions of >50% are attainable without sacrificing diagnostic quality for the vast majority of patients with SU. Ultimately, the decision regarding whether to apply a staged ultrasound +/- CT, a CT dose-reduction protocol, or both lies with the individual hospital.
This study should be interpreted in light of its limitations. NEDS is limited by its retrospective nature and lack of clinical detail, thus we were unable to control directly for considerations including patient severity or account for clinician decision-making regarding imaging strategy. The database relies on diagnostic and procedural coding to classify patient diagnoses and imaging, and so is subject to concerns inherent to administrative databases including misclassification, clerical error, and omission. Furthermore, we determined that certain facilities reported imaging unreliably (or not at all); therefore our analysis was limited to patients seen at those hospitals which did reliably report. It is possible that in this (necessary) selection we have created a skewed sample, if the characteristics of patient management at the reporting hospitals differed systematically from management at non-reporting hospitals. Finally, we were unable to determine what proportion of CTs were done using pediatric and/or dose-reduction protocols. Some of the apparent “overuse” of CT observed in this study may in fact be appropriate use, if these CTs are being performed at centers that have instituted effective dose-reduction strategies. Thus, important targets for further investigation include determining the percentage of EDs that have specific protocol for CT scanning in children, as well as determining how often low-dose protocols are being implemented for pediatric (and adult) patients with SU.
Conclusions
CT use appears to be highly prevalent for children with SU seen in US EDs. However, the rate of increase in CT use for pediatric patients with SU does appear to have leveled off. The lowest CT use is seen in EDs that care for more children. Ultrasound is used very infrequently regardless of site. Awareness regarding risks of CT and consideration of strategies including ultrasound and low dose scanning protocols are warranted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Smith RC, Verga M, McCarthy S, et al. Diagnosis of acute flank pain: value of unenhanced helical CT. AJR American journal of roentgenology. 1996;166:97. doi: 10.2214/ajr.166.1.8571915. [DOI] [PubMed] [Google Scholar]
- 2.Fielding JR, Steele G, Fox LA, et al. Spiral computerized tomography in the evaluation of acute flank pain: a replacement for excretory urography. The Journal of urology. 1997;157:2071. [PubMed] [Google Scholar]
- 3.Brenner D, Elliston C, Hall E, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR American journal of roentgenology. 2001;176:289. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 4.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strauss KJ, Goske MJ, Kaste SC, et al. Image gently: Ten steps you can take to optimize image quality and lower CT dose for pediatric patients. AJR American journal of roentgenology. 2010;194:868. doi: 10.2214/AJR.09.4091. [DOI] [PubMed] [Google Scholar]
- 6.Slovis TL. The ALARA concept in pediatric CT: myth or reality? Radiology. 2002;223:5. doi: 10.1148/radiol.2231012100. [DOI] [PubMed] [Google Scholar]
- 7.Passerotti C, Chow JS, Silva A, et al. Ultrasound versus computerized tomography for evaluating urolithiasis. The Journal of urology. 2009;182:1829. doi: 10.1016/j.juro.2009.03.072. [DOI] [PubMed] [Google Scholar]
- 8.Johnson EK, Faerber GJ, Roberts WW, et al. Are stone protocol computed tomography scans mandatory for children with suspected urinary calculi? Urology. 2011;78:662. doi: 10.1016/j.urology.2011.02.062. [DOI] [PubMed] [Google Scholar]
- 9.Larson DB, Johnson LW, Schnell BM, et al. Rising use of CT in child visits to the emergency department in the United States, 1995-2008. Radiology. 2011;259:793. doi: 10.1148/radiol.11101939. [DOI] [PubMed] [Google Scholar]
- 10.Hryhorczuk AL, Mannix RC, Taylor GA. Pediatric abdominal pain: use of imaging in the emergency department in the United States from 1999 to 2007. Radiology. 2012;263:778. doi: 10.1148/radiol.12111726. [DOI] [PubMed] [Google Scholar]
- 11.Kocher KE, Meurer WJ, Fazel R, et al. National trends in use of computed tomography in the emergency department. Annals of emergency medicine. 2011;58:452. doi: 10.1016/j.annemergmed.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 12.Dwyer ME, Krambeck AE, Bergstralh EJ, et al. Temporal trends in incidence of kidney stones among children: a 25-year population based study. The Journal of urology. 2012;188:247. doi: 10.1016/j.juro.2012.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Routh JC, Graham DA, Nelson CP. Trends in imaging and surgical management of pediatric urolithiasis at American pediatric hospitals. J Urol. 2010;184:1816. doi: 10.1016/j.juro.2010.03.117. [DOI] [PubMed] [Google Scholar]
- 14.Menoch MJ, Hirsh DA, Khan NS, et al. Trends in computed tomography utilization in the pediatric emergency department. Pediatrics. 2012;129:e690. doi: 10.1542/peds.2011-2548. [DOI] [PubMed] [Google Scholar]
- 15.Tompane T, Bush R, Dansky T, et al. Diagnostic imaging studies performed in children over a nine-year period. Pediatrics. 2013;131:e45. doi: 10.1542/peds.2012-1228. [DOI] [PubMed] [Google Scholar]
- 16.Catalano O, Nunziata A, Altei F, et al. Suspected ureteral colic: primary helical CT versus selective helical CT after unenhanced radiography and sonography. AJR American journal of roentgenology. 2002;178:379. doi: 10.2214/ajr.178.2.1780379. [DOI] [PubMed] [Google Scholar]
- 17.Ramarajan N, Krishnamoorthi R, Barth R, et al. An interdisciplinary initiative to reduce radiation exposure: evaluation of appendicitis in a pediatric emergency department with clinical assessment supported by a staged ultrasound and computed tomography pathway. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2009;16:1258. doi: 10.1111/j.1553-2712.2009.00511.x. [DOI] [PubMed] [Google Scholar]
- 18.Burr A, Renaud EJ, Manno M, et al. Glowing in the dark: time of day as a determinant of radiographic imaging in the evaluation of abdominal pain in children. Journal of pediatric surgery. 2011;46:188. doi: 10.1016/j.jpedsurg.2010.09.088. [DOI] [PubMed] [Google Scholar]
- 19.Hamm M, Knopfle E, Wartenberg S, et al. Low dose unenhanced helical computerized tomography for the evaluation of acute flank pain. The Journal of urology. 2002;167:1687. [PubMed] [Google Scholar]
- 20.Kluner C, Hein PA, Gralla O, et al. Does ultra-low-dose CT with a radiation dose equivalent to that of KUB suffice to detect renal and ureteral calculi? Journal of computer assisted tomography. 2006;30:44. doi: 10.1097/01.rct.0000191685.58838.ef. [DOI] [PubMed] [Google Scholar]
- 21.Poletti PA, Platon A, Rutschmann OT, et al. Low-dose versus standard-dose CT protocol in patients with clinically suspected renal colic. AJR American journal of roentgenology. 2007;188:927. doi: 10.2214/AJR.06.0793. [DOI] [PubMed] [Google Scholar]
- 22.Niemann T, Kollmann T, Bongartz G. Diagnostic performance of low-dose CT for the detection of urolithiasis: a meta-analysis. AJR American journal of roentgenology. 2008;191:396. doi: 10.2214/AJR.07.3414. [DOI] [PubMed] [Google Scholar]
- 23.Ciaschini MW, Remer EM, Baker ME, et al. Urinary calculi: radiation dose reduction of 50% and 75% at CT--effect on sensitivity. Radiology. 2009;251:105. doi: 10.1148/radiol.2511081084. [DOI] [PubMed] [Google Scholar]
- 24.Karmazyn B, Frush DP, Applegate KE, et al. CT with a computer-simulated dose reduction technique for detection of pediatric nephroureterolithiasis: comparison of standard and reduced radiation doses. AJR American journal of roentgenology. 2009;192:143. doi: 10.2214/AJR.08.1391. [DOI] [PubMed] [Google Scholar]


