Abstract
Objective
The present study aims to analyze perinatal outcomes in twins given special care during pregnancy and labor and to compare fetal and neonatal outcomes in dichorionic twins with monochorionic twins.
Study Design
Eighty eight (88) twin pregnancies booked for care at a tertiary care Fetal Medicine centre were included in this study. The maternal demographic variables, course of pregnancy, fetal problems, and specialized fetal therapeutic and diagnostic interventions were noted. The above parameters were compared in the sub-groups of dichorionic and monochorionic twin pregnancies and related to the perinatal outcome. Statistical analysis was done using the student’s t test and the two-tailed chi sqaure tests with Yate’s continuity correction. A p value <0.05 was considered as significant.
Results
Mean maternal age was 30.34 + 4.81 years (range 19–48). 81 % of the twins were DCDA, and 19 % were MCDA. The mean gestational age at delivery was 34.4 ± 3.5 weeks, and this was not significantly different in MCDA and DCDA groups. Serious fetal problems warranting intervention at the time of initial referral were significantly higher in MCDA twins although overall perinatal outcome in both groups were not different.
Conclusion
Specialized care during pregnancy and labor including active fetal surveillance and therapeutic intervention when indicated improves the perinatal outcome in twin pregnancies and ensured at least one healthy live birth in over 90 % cases, although with an increase in late prematurity.
Keywords: Monochorionicic and dichorionic pregnancies, Multiple births, Pregnancy outcomes, Twins, Fetal interventions, Screening
Introduction
The incidence of multiple gestations is on the rise with increasing maternal age and use of assisted reproduction techniques. Selective fetal reduction of multifetal pregnancies is now widely practiced to reduce the higher-order multiples to twins based on evidence from nonrandomized studies which suggests that this will improve the perinatal outcome [1]. The proportion of twin pregnancies with unique fetal and maternal problems is therefore increasing. Optimizing maternal, fetal, and perinatal outcomes in twin pregnancies continues to be a formidable challenge in the present day clinical practice (Table 1).
Table 1.
Demographic features of study population (n = 88)
| Mean maternal age (years) | 30.34 ± 4.81 (range 19–48) |
| Spontaneous conception | 44 (50 %) |
| Ovulation induction/IUI | 15 (17 %) |
| IVF/ICSI | 29 (33 %) |
| Prior embryo reduction | 8 (9.09 %) |
| Mean gestational age at booking (weeks) | 17.07 ± 6.65 (range 6–33) |
| Dichorionic diamniotic twin pregnancies | 71 (81 %) |
| Monochorionic diamniotic twin pregnancies | 17 (19 %) |
The present study aims to analyze perinatal outcome in twins given special care during pregnancy and labor and to compare fetal and neonatal outcomes in dichorionic twins with monochorionic twins (Table 2).
Table 2.
Indication for initial referral
| DCDA | MCDA | |
|---|---|---|
| Significant fetal problems | 12 (16.9 %) | 10 (58.82 %) p = 0.0011 |
| Routine care | 59 (83.1 %) | 7 (41.18 %) |
Study Design
All twin pregnancies booked for care at this center were included in this study. This is a descriptive (cross-sectional) analysis of all cases of twin pregnancies, which were delivered and were managed at the Apollo Centre for Fetal Medicine, a tertiary Fetal Medicine referral center in North India over a period of 4 years from Sep 2006 to Aug 2010. The maternal demographic variables (Table 1), course of pregnancy, fetal problems (Table 2), and specialized fetal therapeutic and diagnostic interventions were noted (Tables 3 and 4). The above parameters were also separately evaluated in dichorionic and monochorionic twin pregnancies and correlated to the perinatal outcome.
Table 3.
Different methods used for Screening for fetal aneuploidies
| NT (nuchal translucency) | 24 (27.27 %) |
| Combined first trimester test | 21 (23.86 %) |
| Second trimester genetic sonogram | 26 (29.54 %) |
| No assessment (booked after 20 weeks) | 16 (18.18 %) |
| Confirmed karyotype after risk assessment (CVS/Amniocentesis) | 3 (3.36 %) |
| Confirmed karyotype electively without risk assessment | 1 (1.12 %) |
Table 4.
Fetal therapeutic interventions
| LASER ablation of umbilical cord in TRAP | 2 |
| LASER septostomy in severe TTTS | 1 |
| Serial amniodrainage | 3 |
| Selective feticide of anomalous twin | 1 |
Statistical analysis was done using the Student’s t test and the two-tailed chi square tests with Yate’s continuity correction. A p value <0.05 was considered as significant.
Results
Over a period of 4 years, there were 101 twin pregnancies which accounted for 4.04 % of all the pregnancies booked for care at our center. Five twin pregnancies are on going, while eight cases were lost to follow-up.
Eighty-eight twin pregnancies (91.66 % of the delivered cases) were followed up till delivery, and complete outcomes with follow-up until date are recorded (Table 5).
Table 5.
Fetal and perinatal outcome measures in study population
| Miscarriage of both twins (<20 weeks GA) | 5 (5.68 %) |
| Single fetal demise (<20 weeks GA) | 2 (2.27 %) |
| Cervical cerclage/pessary | 15 (17.04 %) |
| Mean Gestational age at delivery (weeks) | 34.40 ± 3.5 |
| Preterm births (<37 weeks GA) | 65 (78.31 %) |
| Early preterm births (<34 weeks GA) | 22 (26.51 %) |
| Late preterm births (34–37 weeks GA) | 43(51.81 %) |
| Term births (%) | 18 (20.46 %) |
| Mean birth weight of babies (g) | 1951.56 ± 575.17 |
| Discordant anomalies | 9 (10.2 %) |
| Discordant growth | 50 (56.8 %) |
| Late intrauterine fetal demise | 17 (10.3 %) |
| Live births | 140 (86.4 %) |
| Neonatal deaths | 5 (3.5 %) |
Discussion
The incidence of twins in our population was 4 % which is higher than the expected incidence in the general population (1 %) because the present study represents a cross section of high-risk pregnancies which have been referred to a tertiary fetal medicine center either due to significant fetal problems or for routine care in anticipation of problems. 81 % of the twins were dichorionic (DCDA), while 19 % were monochorionic diamniotic (MCDA) (Fig 1).
Fig. 1.
Distribution of chorionicity of twins in study population
A significantly higher proportion of the MCDA twins were referred because of serious fetal problems(58.82 %) as compared to the DCDA twins (p = 0.0011). The overall livebirth rate in DCDA twins (92.3 %) was significantly higher than that in MCDA (62.5 %), p < 0.001. However, the other parameters of perinatal outcome like gestational age at delivery, mode of delivery or birthweight of babies were not significantly different.
The increased possibility of complications and poor perinatal outcomes in monochorionic twins as compared with dichorionic twins has been established [2]. It has also been shown that even after exclusion of disorders unique to monochorionic placentation, there is persistence of higher perinatal complications in MCDA twins [3, 4]. It is therefore interesting to note that our outcomes were not significantly different in the MCDA and DCDA subgroups inspite of significantly higher proportion of MCDA twins referred due to adverse fetal conditions. This can be attributed to the successful fetal interventions and monitoring. Therapeutic LASER ablation of the umbilical cord in the TRAP sequences and the LASER septostomy in severe TTTS helped in salvaging the co-twin and achieve one live birth. These fetal interventions carry a risk of pregnancy loss as was seen in one case in our series. These procedures must be undertaken judiciously after elaborate counseling and by an appropriately trained operator.
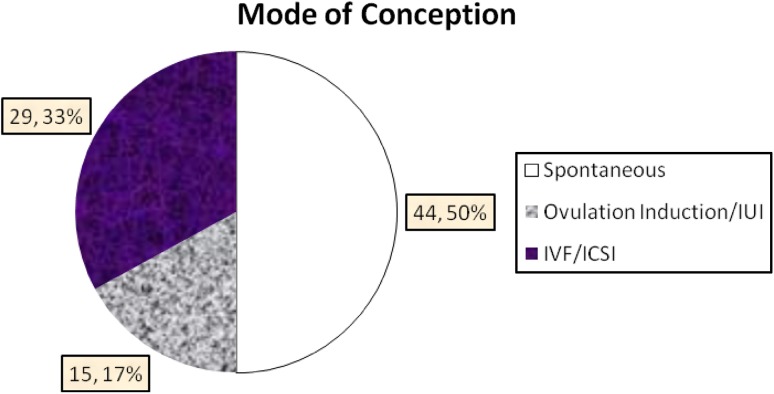
Forty-four (50 %) pregnancies were conceived naturally, while 15(17 %) had ovulation induction with or without intrauterine insemination (IUI), and 29(33 %) had conceived with either Invitro fertilization (IVF) or intra cytoplasmic sperm injection (ICSI). Prior embryo reduction from higher-order multiples was performed in 8 cases (9.09 %).
It is interesting to note that the proportion of spontaneous conceptions and assisted conceptions were similar in the overall study population. However, significantly higher number of MCDA twins had been spontaneously conceived compared with DCDA (p = 0.0012) (Table 6) (Fig 2).
Table 6.
Comparison of fetal and perinatal outcomes in DCDA and MCDA subgroups
| DCDA (n = 71) | MCDA (n = 17) | p value | |
|---|---|---|---|
| Mean maternal age (years) | 30.76 ± 4.8 | 31.00 ± 6.24 | 0.094991198 |
| Spontaneous conception | 42 (59.15 %) | 15 (88.23 %) | 0.0012 |
| Mean gestational age at booking (weeks) | 17.54 ± 6.74 | 19.7 ± 5.68 | 0.050792407 |
| Miscarriage | 4 (5.63 %) | 1 (5.88) | 0.9683 |
| Discordant anomaly | 5 (7.04 %) | 4 (23.52 %) | 0.1165 |
| Discordant growth | 42 (16.9 %) | 8 (18.75 %) | 0.5275 |
| Late intrauterine fetal demise | 5/130 (3.8 %) | 12/32 (37.5 %) | <0.001 |
| Mean gestational age at delivery (weeks) | 34.37 ± 2.64 | 32.03 ± 4.57 | 0.099103121 |
| Early preterm births (<34 weeks GA) | 16/67 (23.88 %) | 6/16 (36.75 %) | 0.6273 |
| Late preterm births (34–37 weeks GA) | 35/67 (52.24 %) | 8/16 (50 %) | 0.6273 |
| Term births (after 37 weeks GA) | 16/67 (23.88 %) | 2/16 (12.25 %) | 0.6305 |
| LSCS | 62/67 (92.53 %) | 10/16 (62.9 %) | 0.0009 |
| Live births | 120/130 (92.3 %) | 20/32 (62.7 %) | <0.001 |
| Mean birth weight (g) | 2027.98 ± 493.23 | 1591.25 ± 777.59 | 0.00293327 |
| Neonatal deaths | 5 (3.5 %) | – |
Fig. 2.
Mode of conception
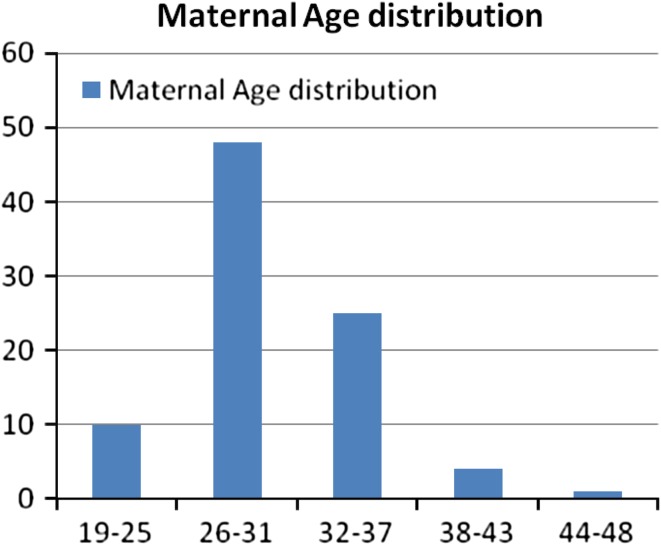
The mean maternal age in the study population (n = 88) was 30.34 + 4.81 years with the range from 19 to 48 years. The maternal age distribution in the study population is shown in Fig. 3.
Fig. 3.
Maternal age distribution in study population
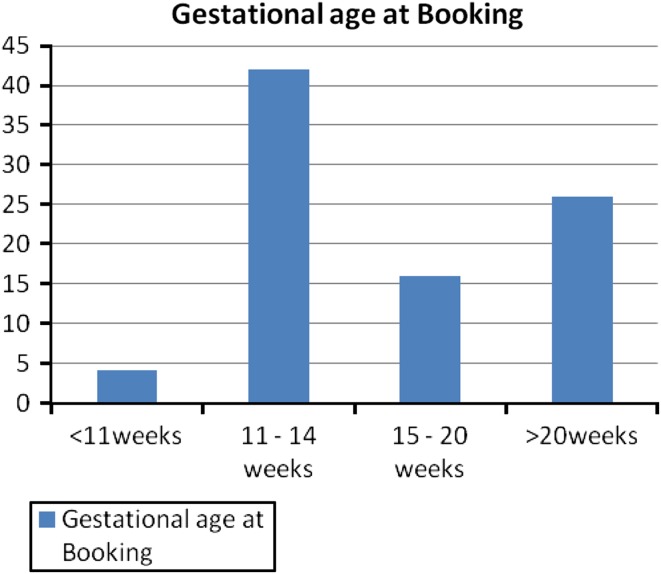
The mean gestational age at booking was 17.07 + 6.65 (range 6–33). When we analyzed the distribution of the individual cases as per the gestational age at booking, most of the cases booked were between 11 and 20 weeks (Fig. 4).
Fig. 4.
Gestational age at booking
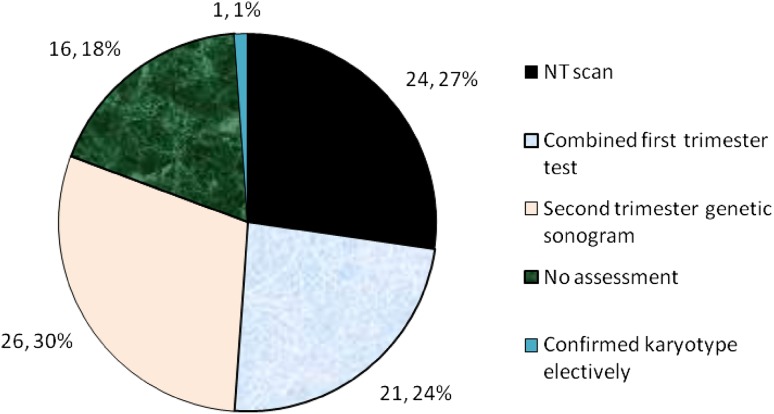
Various options for screening for fetal aneuploidies were offered to women depending on their gestational age at booking. All women who booked before 14 weeks were offered the nuchal translucency scan or the combined first trimester screening test. Those who booked between 14 and 20 weeks were offered the genetic sonogram (Fig. 5).
Fig. 5.
Various screening modalities offered to study population
The optimum modality of screening for fetal aneuploidy in twin pregnancies has remained controversial. Emerging evidence supports the use of the first trimester combined test with satisfactory efficacy in twins. It is notable that the first trimester combined screening has been offered as a routine test only since 2008 after the evidence supporting its use became strong [5]. In the present study, three women underwent invasive fetal diagnostic procedures like chorionic villus Sampling (CVS) and amniocentesis. Three women were allocated as high risks for fetal aneuploidies after screening, while one voluntarily opted for CVS instead of any screening tests. All fetal karyotype reports were normal, and there was no procedure-related pregnancy loss.
The overall preterm delivery rate in the present study population is 78.3 %, and the mean gestational age at delivery is 34.4 weeks. This appears to be a very high rate of preterm births, and we analyzed them to see the distribution of early-and late-preterm births in this group. We found that 33.85 % of these were early-preterm (<34 weeks) deliveries which were mostly due to pressing fetal indications or spontaneous preterm labor. The incidence of spontaneous preterm labour was 17.0 %. A cervical cerclage or pessary was inserted in 15 (17.04 %) women, but the indications varied because of previous history of miscarriage and reduced cervical length in present pregnancy to elective cerclage. The late preterm (between 34 and 37 weeks) accounted for 66.15 % of all preterm deliveries. Most of the deliveries were elective cesarean sections at this gestation period accounting for the 51.81 % incidence of late-preterm births (Fig. 6).
Fig. 6.
Distribution of gestational age at delivery
If we analyze the distribution of gestational age at delivery, then most deliveries have taken place between 33 and 36 weeks of gestation, at which time the neonatal survival is of the order of 95 %.
We get the impression that twin pregnancies increase the anxiety levels in the parents and caregivers, which manifests in an inclination toward earlier delivery. We hope that with this study, we can reassure obstetricians that with active fetal surveillance, it is safe to allow twin pregnancies to continue to term, thus reducing our alaraming preterm delivery rate of 78.3 % in this group.
Conclusion
The present study has shown that with active fetal surveillance and intervention, perinatal outcome can be improved in twin pregnancies. Especially in monochorionic twins, appropriately timed therapeutic interventions for TRAP and TTTS can help us save the co-twin. Early identification and monitoring of growth discrepancy can help in optimising the time of delivery. It is unclear whether such a protocol could increase the risk of intervention and prematurity. We hope that this study helps us to reduce iatrogenic prematurity.
We are in the process of collecting the data of the neonatal outcomes of the pregnancies which are delivered in Indraprastha Apollo Hospitals and their long-term follow-up.
References
- 1.Dodd J, Crowther C. Multifetal pregnancy reduction of triplet and higher-order multiple pregnancies to twins. Fertil Steril. 2004;81:1420. doi: 10.1016/j.fertnstert.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 2.Hack KE, Derks JB, Elias SG, et al. Increased perinatal mortality and morbidity in monochorionic versus dichorionic twin pregnancies: clinical implications of a large Dutch cohort study. BJOG. 2008;115(1):58–67. doi: 10.1111/j.1471-0528.2007.01556.x. [DOI] [PubMed] [Google Scholar]
- 3.Acosta-Rojas R, Becker J, Munoz-Abellana B, et al. Catalunya and Balears Monochorionic Network. Twin chorionicity and the risk of adverse perinatal outcome. Int J Gynaecol Obstet. 2007;96(2):98–102. doi: 10.1016/j.ijgo.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Leduc L, Takser L, Rinfret D, et al. Persistance of adverse obstetric and neonatal outcomes in monochorionic twins after exclusion of disorders unique to monochorionic placentation. Am J Obstet Gynecol. 2005;193(5):1670–1675. doi: 10.1016/j.ajog.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Kagan KO, Wright D, Baker A, et al. Screening for trisomy 21 by maternal age, fetal nuchal translucency thickness, free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol. 2008;31(6):618–624. doi: 10.1002/uog.5331. [DOI] [PubMed] [Google Scholar]