Abstract
Objective
To determine the influence of “structured contraception counseling” on Indian women’s selection of contraceptive methods.
Methods
Women (≥18 and ≤40 years) requesting contraception were enrolled at 36 sites. “Structured contraception counseling” was provided by a health care professional on the available contraceptive methods. Questionnaires on the women’s pre- and post-counseling contraceptive choice, her perceptions, and the reasons behind her post-counseling decision were filled.
Results
Significant reductions were observed in the proportion of women who were indecisive (n = 260; 31.5 % pre-counseling vs. n = 30; 3.6 %, post-counseling [P < 0.001]) and women opting for non-hormonal method (24.6 % pre-counseling vs. 6.8 % post-counseling, [P < 0.001]). Of all the women counseled (n = 825), 89.6 % (739/825) of women chose a hormonal contraceptive method. There were significant difference (P < 0.001) in the women’s choice of contraceptive in the pre- and post-counseling sessions, respectively (combined oral contraceptive: 30.8 vs. 40.7 %; vaginal ring: 1.8 vs. 14.1 %; progestogen only pills: 1.6 vs. 7.9 %; injectable-depot medroxyprogesterone acetate: 5.9 vs. 13.6 %; levonorgestrel-intrauterine system: 3.8 vs. 13.3 %).
Conclusions
Structured contraception counseling using standardized protocol and aids resulted in a significant increase in the selection of modern contraceptive methods. Post-counseling majority of women opted for hormonal methods with an increase in selection of pills and newer alternatives.
Keywords: Hormonal contraceptive, Counseling, Questionnaire, India
Introduction
Unmet need for family planning is an important indicator for assessing the potential demand for family planning services. As per the national family health survey (NFHS-3), 69 % of married women in India had a demand for family planning, 81.5 % of which was satisfied. The contraceptive prevalence rate in women age 15–49 years was 56 % and the unmet need for family planning among married women was 13 % [1]. The contraceptive usage patterns vary widely in India with prevalence of modern contraception reported to be 48.5 %, which mainly includes 5.2 % of condoms, 3.1 % of pills, 1.7 % of intrauterine devices (IUD), 0.1 % of injectable, and the bulk being permanent sterilizations (male and female) 38.3 % [2]. This suggests that though a number of contraceptive choices are available, the usage of modern hormonal contraceptive methods is very low. According to a recent study, only one-third of modern contraceptive users were informed about the side effects or problems of their method and less than 30 % were ever informed about various family planning methods [1]. This suggests an unmet need of comprehensive information on contraceptive methods which can be met via counseling in India.
A woman’s individual needs and preferences determine the best contraceptive method for her. Health care professionals (HCPs) can help women evaluate and compare the available contraceptive options by initiating a dialog during consultations. Counseling provides the HCP an opportunity to understand the individual need of a contraceptive seeker. By counseling and sharing information on various available contraceptives, HCPs can provide women with the information they need to make an informed decision about contraception in the limited time available. Education material on contraceptives tends to make the counseling simplified, efficient, and standardized. A multi-national European study provided compelling evidence that structured contraception information and counseling provided by HCPs enabled women to select alternative forms of contraception which better corresponded to their lifestyle and needs [3]. Similarly, the TEAM-06 study conducted in Spain showed that contraceptive counseling provided by HCPs often influence women to opt for another contraceptive method rather than the one they had originally intended to use [4].
This study primarily aimed to evaluate the role of structure contraceptive counseling on the decision making process and the resultant changes brought about in the contraceptive choice and selection post-counseling in Indian women. Other objectives of the study were to determine women’s perception regarding available contraceptive methods, social, and demographic predictors affecting the choice by sub-group analysis based on age group, education level, employment status, and number of children. The study also analyzed the HCPs pre-counseling preferences with women’s post-counseling choice.
Materials and Methods
This was a cross-sectional, observational study conducted at 36 sites distributed across India. It was conducted in the clinics of participating HCPs (gynecologists), by Organon (India) Private Limited (sponsor) in collaboration with family welfare committee of the federation of the obstetrics and gynecological societies of India (FOGSI). A “Structured contraception counseling” was formulated and provided using a standardized protocol with balanced and comprehensive education material on the available contraceptive methods. Questionnaires with information on the women’s pre- and post-counseling contraceptive choice, her perceptions, and the reasons behind her post-counseling decision were filled both by the HCP and the participating women.
The study was initiated after getting approval of the study from institutional review board (IRB)/independent ethics committee (IEC), in compliance with local laws. Ethical principles that have their origin in the world medical association declaration of Helsinki, and all applicable local laws, rules, and regulations relating to the conduct of the study were followed. The study was conducted from June 2012 to October 2012 in compliance with the protocol (#P08385). Since the study was observational in design, local regulatory authorities were notified about the study.
Sexually active women ≥18 and ≤40 years who consulted HCPs for contraception and who considered starting hormonal contraceptive method or expressed interest in switching (changing) to hormonal methods were invited to participate in the study. Women were included only if they gave informed consent and agreed and were able to fill the questionnaire.
After obtaining the signed informed consent from participating woman, the HCP recorded the method woman intended to use before counseling on Part A1 of the questionnaire. In addition, HCP assessed if hormonal contraception was not suitable for the woman who then could not participate in study. Each eligible participating woman was then asked to fill Part A2 of the questionnaire. This part consisted of questions on socio-demographic profile and opinion on contraceptive methods like combined oral contraceptive (COC), progestogen only pill (POP), injectable-depot medroxyprogesterone acetate (DMPA), intrauterine system (LNG-IUS), and vaginal ring. HCPs used the balanced and comprehensive education material on the available contraceptive methods during verbal “structured contraception counseling” session. The education material for counseling provided fair, balanced overview of the effectiveness of COC, POP, LNG-IUS, DMPA, and vaginal ring, including their mode of action, use, potential risks, benefits, and suitability for individual needs. The education material was drafted by the last two authors, revised and modified by the first two authors, and endorsed by the family welfare committee of FOGSI.
After counseling, woman completed Part B of the questionnaire, which included questions regarding reasons for choosing the contraceptive method and not selecting the other methods. The completed questionnaires were collected and analyzed.
Sample Size and Statistics
A sample size of 653 women was determined to be necessary to detect a 4 % increase in proportion of women choosing vaginal ring or LNG-IUS after counseling as compared to before counseling. This had an assumption that 3 % of women switch from vaginal ring/LNG-IUS to COC/POP/DMPA after counseling. Target enrollment was adjusted by 20 % to compensate for non-evaluable questionnaire and erroneous entry, and this led to final target enrollment of 800 women with 90 % power. All analyses were performed using SAS® version 9.1.3 (Statistical Analysis System, Cary, NC, USA).
Descriptive statistics were summarized using number and percentage of subjects along with 95 % confidence interval (CI). Method selected by women pre- and post-counseling was analyzed using McNemar’s test. Categorical variables were displayed using number of subjects and percentage. The probability to choose a contraceptive method post-counseling was estimated by binomial regression model against agreement or disagreement for women’s perception versus “no opinion/do not know” as a combined reference category. All statistical tests were performed at 5 % significance level.
Results
Demography
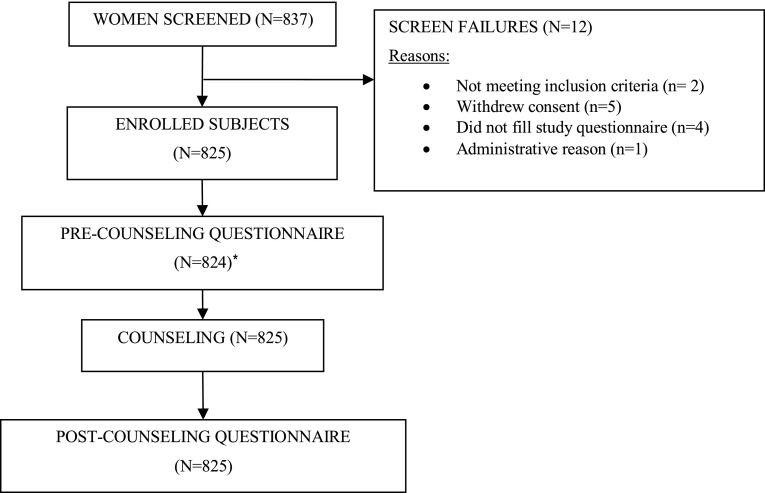
Eight hundred thirty seven (837) women were screened for the eligibility criteria of the study. Of these, 12 were excluded (Fig. 1). Major reasons for exclusions were not meeting study eligibility criteria, not filing study questionnaire, and withdrawal of consent to participate. This resulted in a total of 825 eligible women who were included in the final analysis (Fig. 1). Demographic characteristics of these women are presented in Table 1. History of unplanned pregnancies and induced abortions was reported by 35.9 % (296) and 31.3 % (258) of women, respectively.
Fig. 1.
Disposition summary of women. *One woman did not complete pre-counseling (A2) question
Table 1.
Characteristics of participating women in the study (n = 825)
| Characteristics | n (%)a | |
|---|---|---|
| Age (mean ± SD) (years) | 29.1 ± 4.8 | |
| Age group (years) | 18–20 | 19 (2.30) |
| 21–30 | 500 (60.6) | |
| 31–40 | 306 (37.1) | |
| Highest educational level achievedb | Primary school | 62 (7.52) |
| Completed high school | 129 (15.7) | |
| College, advanced education after high school | 253 (30.7) | |
| University | 380 (46.1) | |
| Employment status | Not employed | 479 (58.1) |
| Part time employment | 94 (11.4) | |
| Fulltime employed | 252 (30.5) | |
| Status of children | 0 | 148 (17.9) |
| 1–2 | 642 (77.8) | |
| 3–4 | 34 (4.12) | |
| ≥5 | 1 (0.12) | |
| Plan to have (more) children later | Yes | 415 (50.3) |
| No | 310 (37.6) | |
| Do not know yet | 100 (12.1) | |
| Previous unplanned pregnancies | Yes | 296 (35.9) |
| No | 529 (64.1) | |
| Previous induced abortions† | Yes | 258 (31.3) |
| No | 566 (8.7) | |
| . | ||
Participating women: number of women who participated in this study
SD standard deviation
aUnless otherwise specified
bData missing for one woman
Women (825) were counseled for a mean duration (SD) of 24 (13) minutes. Women’s ratings of the counseling and contraceptive information they received from HCPs were largely positive. Majority of women rated the information received through counseling as “very” useful (91.2 % [752]), “very” complete (86.1 % [710]), and “very” fair and balanced (85.3 % [704]).
Contraceptive Choice of Participating Women
Pre-counseling, 43.8 % (362/825) women selected a hormonal method, 24.6 % (203/825) non-hormonal method, and 31.5 % (260/825) were undecided for any contraceptive method. After “structured contraception counseling,” 89.6 % (739/825) of women chose a hormonal contraceptive method.
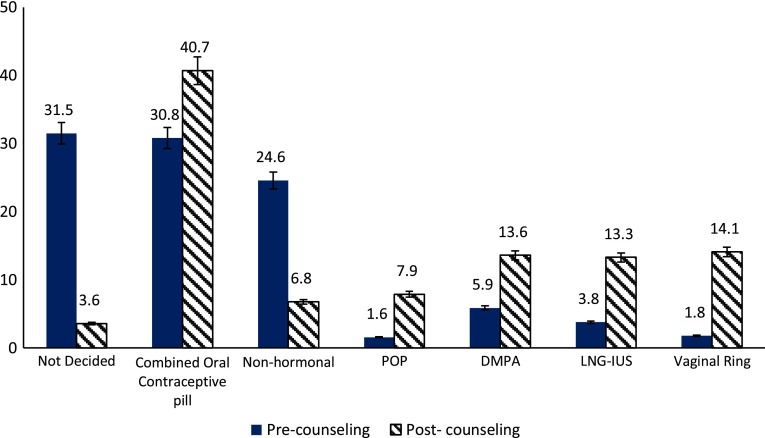
Contraceptive counseling provided to women resulted in statistically significant (P value < 0.0001, Mc Nemar’s test) differences between proportions of women opting each contraceptive method before and after the counseling (Fig. 2). Post-counseling, COCs were chosen by 40.7 % (n = 336; 95 % CI 37.4–44.2), vaginal ring by 14.1 % (n = 116; 95 % CI 11.8–16.6), injectable-DMPA (n = 112; 95 % CI 11.3–16.1) by 13.6 %, LNG-IUS by 13.3 % women (n = 110; 95 % CI 11.1–15.8), POP by 7.9 % women (n = 65; 95 % CI 6.1–9.9), and other non-hormonal methods by 6.8 % women (n = 56; 95 % CI 5.2–8.7). Around, 3.6 % women (n = 30; 95 % CI 2.8–5.8) remained indecisive about method of contraception. Maximum difference (12.2 %; P value < 0.0001) was noted in the proportion of women who chose vaginal ring after counseling as compared to before counseling. Differences in proportions of women who opted for COC, POP, injectable-DMPA, and LNG-IUS post-counseling and pre-counseling were 9.9, 6.3, 7.6, and 9.6 %, respectively.
Fig. 2.
Women’s pre- and post-counseling contraceptive choice. COC combined oral contraceptive pill, Injectable-DMPA injectable-depot medroxyprogesterone acetate, LNG-IUS levonorgestrel-releasing intrauterine system, POP progestogen only pill, Denominator is the number of women who underwent contraceptive counseling. Difference between pre and post is statistically significant (P value < 0.0001, Mc Nemar’s test).Error bars represent the 95 % confidence interval
Shifts in contraceptive choice of 203 women who chose non-hormonal pre-counseling waere observed, with maximum shift toward the COC method (24.1 % [49/203]) (Table 2). In the present study, counseling helped women arrive at a decision. After counseling, the highest decrease was observed in the proportion of women indecisive about method to be opted (difference in proportions = 27.9 %, P value < 0.0001) (Fig. 2). This decrease was due to shift from pool of women who were indecisive (260) prior to counseling toward hormonal contraceptive methods (Table 2). Maximum of such women (39.2 % [102/260]) opted COCs as the post-counseling method of contraception.
Table 2.
Cross table for contraceptive method women intended to use before counseling and chosen after counseling
| n = 825 | Post-counseling methods chosen by womena, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-counseling methods intended by women | n | COC | Vaginal ring | POP | Injectable-DMPA | LNG-IUS | Other non-hormonal methods | No pre-conceived idea/not yet decided |
| COC | 254 | 173 (68.1 %) | 27 (10.6 %) | 16 (6.3 %) | 7 (2.8 %) | 20 (7.9 %) | 8 (3.1 %) | 3 (1.2 %) |
| Vaginal ring | 15 | 2 (13.3 %) | 8 (53.3 %) | 0 | 0 | 5 (33.3 %) | 0 | 0 |
| POP | 13 | 3 (23.1 %) | 3 (23.1 %) | 4 (30.8 %) | 1 (7.7 %) | 1 (7.7 %) | 1 (7.7 %) | 0 |
| Injectable-DMPA | 49 | 5 (10.2 %) | 2 (4.1 %) | 5 (10.2 %) | 33 (67.3 %) | 4 (8.2 %) | 0 | 0 |
| LNG-IUS | 31 | 2 (6.5 %) | 0 | 4 (12.9 %) | 5 (16.1 %) | 18 (58.1 %) | 2 (6.5 %) | 0 |
| Other non-hormonal methods | 203 | 49 (24.1 %) | 40 (19.7 %) | 16 (7.9 %) | 28 (13.8 %) | 37 (18.2 %) | 25 (12.3 %) | 8 (3.9 %) |
| No pre-conceived idea/not yet decided | 260 | 102 (39.2 %) | 36 (13.8 %) | 20 (7.7 %) | 38 (14.6 %) | 25 (9.6 %) | 20 (7.7 %) | 19 (7.3 %) |
Figures in bold: Participants with no change in opinion about contraceptive methods
COC combined oral contraceptive pill, Injectable-DMPA injectable-depot medroxyprogesterone acetate, LNG-IUS, levonorgestrel-releasing intrauterine system, POP progestogen only pill
aPercentage calculated from pre-counseling number under respective category of corresponding contraceptive method as denominator
A considerable decrease in number of women with unplanned pregnancies who had “no pre-conceived idea about contraceptive method” (32 % [95/296] pre-counseling; 3 % [9/296] post-counseling) was observed. In addition, among women with unplanned pregnancies opted for non-hormonal methods (25.5 % [75/296]) as their intended method of contraception before counseling, and 2.7 % (8/296) opted for the same after counseling.
Contraceptive Choice of Health Care Professional
Before counseling, HCPs selected a contraceptive method for 260 women who had no opinion on the selection of any contraceptive method (Table 3). For more than half (53.46 % [139/260]) women HCPs had no preference for any contraceptive method. HCPs preferred hormonal methods for 44.2 % (115/260) women, these included COCs for 24.2 % (63/260), POPs for 8.5 % (22/260), and vaginal ring for 4.2 % (11/260) women. For 7.3 % (19/260) women HCPs marked either injectable-DMPA or LNG-IUS as the preferred method of contraception. For women of age groups 21–30 and 31–40 years, COC was that most frequently chosen method. Non-hormonal contraceptive methods were chosen by the HCP for < 2.5 % (6/260) women.
Table 3.
Cross table for contraceptive method chosen by HCP for woman before counseling and method chosen by woman after counseling
| n = 260 | Post-counseling methods chosen by womena, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-Counseling Method chosen by HCP | n | COC | vaginal ring | POP | Injectable-DMPA | LNG-IUS | Other non-hormonal method | no pre-conceived idea/not yet decided |
| COC | 63 | 44 (69.8 %) | 3 (4.8 %) | 1 (1.6 %) | 9 (14.3 %) | 1 (1.6 %) | 4 (6.3 %) | 1 (1.6 %) |
| Vaginal ring | 11 | 5 (45.5 %) | 1 (9.1 %) | 0 | 5 (45.5 %) | 0 | 0 | 0 |
| POP | 22 | 2 (9.1 %) | 0 | 12 (54.5) | 2 (9.1 %) | 3 (13.6 %) | 2 (9.1 %) | 1 (4.5 %) |
| Injectable-DMPA | 10 | 0 | 0 | 0 | 10 (100 %) | 0 | 0 | 0 |
| LNG-IUS | 9 | 3 (33.3 %) | 0 | 1 (11.1 %) | 0 | 5 (55.6 %) | 0 | 0 |
| other non-hormonal methods | 6 | 1 (16.7 %) | 2 (33.3 %) | 0 | 0 | 0 | 1 (16.7 %) | 2 (33.3 %) |
| No pre-conceived idea/not yet decided | 139 | 47 (33.8 %) | 30 (21.6 %) | 6 (4.3 %) | 12 (8.6 %) | 16 (11.5 %) | 13 (9.4 %) | 15 (10.8 %) |
Figures in bold: Participants with no change in opinion about contraceptive methods
COC combined oral contraceptive pill, Injectable-DMPA injectable-depot medroxyprogesterone acetate, LNG-IUS levonorgestrel-releasing intrauterine system, POP progestogen only pill
aPercentage calculated from pre-counseling number under respective category of corresponding contraceptive method as denominator
Perception and Reasons for Contraceptive Method Selection
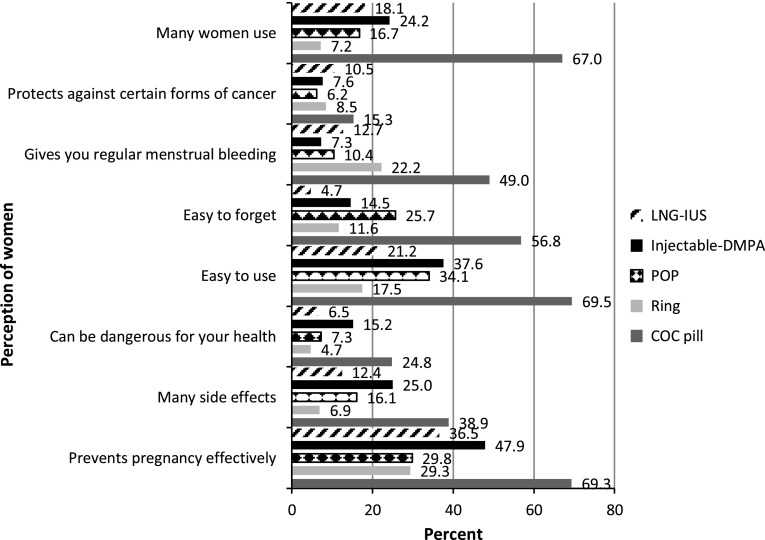
Pre-counseling perceptions of women about the hormonal contraceptive methods are shown in Fig. 3. Association between the perceptions and method chosen after counseling showed that women who agreed with statements for COC pill like “can be dangerous for health,” “has many side effects,” “easy to forget,” and disagreed that COC pill “prevents pregnancy effectively,” “easy to use” had opted for this method less often as compared with women with “no opinion/do not know” (Table 4). Women who agreed with the statement that POP “has many side effects” opted less for POP method compared with women with “no opinion/do not know.” Women who agreed with the statements for vaginal ring like “regular menstrual bleeding,” “prevents pregnancy effectively,” “protects against certain forms of cancer,” and were in disagreement with statements like “starting a new ring is easy to forget” and “can be dangerous for health” had opted vaginal ring more often as compared to women who belonged to the category of “no opinion/do not know.” Similarly, women who disagreed that vaginal ring “has many side effects” and “easy to use” had opted for this method less often.
Fig. 3.
Women’s perceptions about contraceptive methods pre-counseling. Percentage of women who agreed with each statement
Table 4.
Association between perception of contraceptive method (pre-counseling) and method adopted (post-counseling) using binomial regression
|
The dark and light shaded areas represent negative and positive statistically significant (P < 0.05) estimates using binomial regression for predicting the choice of contraceptive method
With regard to category “no opinion”/“do not know,” the estimates for “Agree” and “Disagree” imitate the difference in probability to choose the method
CI confidence interval, COC combined oral contraceptive pill, Injectable-DMPA injectable-depot medroxyprogesterone acetate, LNG-IUS levonorgestrel-releasing intrauterine system, POP progestogen only pill
Post-counseling reasons for selecting hormonal contraceptive methods are shown in Table 5. Among women who selected COCs, “ease of use” was stated as the most frequent reason (70.5 % [237/336]), “breast feeding” was reported by 83.1 % (54/65) for POP, “convenience” 75.9 % (88/116) by those who chose vaginal ring, “long action” 96.4 % (106/110) for LNG-IUS, “convenience” and “3-monthly use” 84.8 % (95/112) each by women who selected injectable-DMPA. Across all the age groups, most frequent reason reported by women for non-selection of any contraceptive method was “discussion with partner.”
Table 5.
Reasons for selection of contraceptive methods by women (n = 825)
| %a | ||
|---|---|---|
| COC | Easy to use | 70.5 |
| Convenience | 68.5 | |
| Regular menstrual bleeding | 67.9 | |
| Daily use | 60.4 | |
| POP | Breast feeding | 83.1 |
| Easy to use | 75.4 | |
| Convenience | 70.8 | |
| Daily use | 67.7 | |
| Injectable-DMPA | 3 monthly use | 84.8 |
| Convenience | 84.8 | |
| Will not forget it | 70.5 | |
| Low chance of side effects | 47.3 | |
| Vaginal ring | Convenience | 75.9 |
| Will not forget it | 74.1 | |
| Monthly use | 72.4 | |
| Regular menstrual bleeding | 64.7 | |
| LNG-IUS | Long acting | 96.4 |
| Convenience | 76.4 | |
| Will not forget it | 74.5 | |
| Still effective if I experience vomiting diarrhea | 53.6 | |
COC combined oral contraceptive pill, Injectable-DMPA injectable-depot medroxyprogesterone acetate, LNG-IUS levonorgestrel-releasing intrauterine system, POP progestogen only pill
aPercentage calculated with denominator as number of women who chose specific hormonal method
Discussion
This study explored the impact of a balanced and comprehensive structured counseling session by the HCP on contraceptive choices made by women. Several studies have reported the need and utilization of contraceptives in India [5–8]. However, there is a lack of studies evaluating the impact of contraceptive counseling on the selection of contraceptive methods. The present study was the first of its kind as it provided a complete perspective on contraceptive use among women from 36 study centers using 8 different languages on five hormonal methods in India. In the present study of the five common hormonal contraceptive methods, the combined hormonal contraceptive pills were found to be the most commonly used contraceptive method in India; this is in conformity with the results for India in the world contraceptive use pattern survey. Contraceptive choices were significantly found to be significantly influenced by the time-bound counseling sessions provided by HCPs, as evident by the change in proportion of women choosing a particular method pre- versus post-counseling [2]. In our study, structured contraception counseling of an average duration of 24 min about various available hormonal contraceptive methods helped most women (96.3 %) to choose a contraceptive method. Similar observations regarding contraceptive counseling selection were reported in studies conducted in different countries [3, 9].
In contrast to counseling provided on three hormonal methods reported in the European CHOICE study, the present study included counseling on five hormonal methods [3]. Counseling provided to women resulted in statistically significant differences between contraceptive methods marked by women in pre- and post-counseling questionnaire. However, among hormonal contraceptive methods, maximum difference in proportions was observed for women who chose the vaginal ring after counseling as compared to pre-counseling. This was probably the most novel method of which awareness was also low during the pre-counseling session. After counseling, switching between various hormonal contraceptive methods was observed. In addition, a significant switch after counseling was observed from non-hormonal methods to hormonal methods of contraception.
Counseling helped a majority of the women who were indecisive about any contraceptive method to make a choice. The majority of the women opted for hormonal methods with an increase in selection of COCs and newer alternatives. This pattern for switching is consistent with previous findings of comprehensive study across five European countries, where changes in women’s pre-counseling and post-counseling choices were statistically significant after counseling sessions [3, 10].
Age-specific choice of contraception in this study is in line with the concept that no single contraceptive method satisfies all potential users all times. Availability of a variety of contraceptive methods is important if individual needs are to be met, and to choose a method that optimally fits with life stages [11].
In conformity with many studies, there were varied reasons reported by women for selecting a contraceptive method. The most common reasons for selecting hormonal contraceptive methods were ease of use for COC, “breast feeding” for POP, convenience for vaginal ring, “long action” for LNG-IUS, and “convenience” and “3-monthly use” for injectable-DMPA, and the most common reasons for not choosing other available contraceptive methods were health hazard and many side effects [3, 7, 12].
Our study revealed that the HCP had a substantial influence on women’s contraceptive choice. More than 50 % of women who were indecisive about any contraceptive method before counseling chose the HCP’s preferred method after counseling. Majority of such women opted for COCs which their HCP recommended prior to counseling. These findings were similar to another international study [9]. While this demonstrates the necessity of counseling by a HCP especially for women who are unaware of contraceptive methods in developing countries like India, it is important to adhere to the principles of non-directive, non-coercive, and non-judgmental counseling.
Though the study has significant findings, limitation of our study includes no follow-up visit to assess participant’s actual choice and compliance, no direct involvement of male partners in counseling, and no inclusion of non-hormonal reversible modern methods in the educational material of counseling and provider’s bias.
The strengths of this study were the sample size of 825 women who enrolled from diverse regions of India and the use of a unique standard structured counseling material (developed by FOGSI). In conclusion, this study showed that COCs are the most frequently preferred contraceptive method among Indian women. “Structured contraception counseling” using standardized protocol and aids resulted in a significant empowerment and increase in selection and uptake of modern contraceptive methods by Indian women with the potential of giving them the autonomy of choice.
Acknowledgments
Family Welfare Committee, Federation of Obstetrics and Gynecological Societies of India (FOGSI) and the participating study investigators (Dr. Anita Soni, Dr. Arnab Basak, Dr. Atul Ganatra, Dr. Atul Munshi, Dr. Avan Dadina, Dr. Fahmida Banu, Dr. Gayatri Deshpande, Dr. Geeta Balsarkar, Dr. Jaiashree Gajraj, Dr. Kiran Desai, Dr. M. Krishna Kumari, Dr. Mala Arora, Dr. Mitra Saxena, Dr. Pallaniappan, Dr. Parag Biniwale, Dr. Poonam Gupta, Dr. Priti Vyas, Dr. Priyadarshini, Dr. Pushpa Jaiswal, Dr. Ratnaboli Chakravorty, Dr. Rekha Kurian, Dr. Rupam Arora, Dr. Rupashree Bhoyar, Dr. S. R. Pal, Dr. Sarmistha Patra, Dr. Saswati Sanyal Choudhury, Dr. Sonal Kotdawala, Dr. Sreekrishna Rao, Dr., Sukumar Barik, Dr. Sunita Chandra, Dr. Susheela Rani, Dr. Uma Ram, Dr. Uma Sheshagiri Dr. Vijay Lakshmi R). Editorial assistance was provided by Dr Varun Sharma of GVK Biosciences Pvt. Limited.
Compliance with ethical requirements and Conflict of interest
The study was initiated after getting approval of the study from Institutional Review Board (IRB)/Independent Ethics Committee (IEC), in compliance with local laws. Ethical principles that have their origin in the world medical association declaration of Helsinki, and all applicable local laws, rules, and regulations relating to the conduct of the study were followed. Informed consent was obtained from all patients for being included in the study. Since the study was observational in design, local regulatory authorities were notified about the study.
Dr. Nozer Sheriar, Dr. Ritu Joshi, and Dr. Bhaskar Pal were investigators in this study and have received investigator's grant from MSD. Dr. Basab Mukherjee nothing to declare. Dr. Ashish Birla and Dr. Subrat K Ray are employees of Organon India Pvt. Limited.
Nozer Sheriar
is a Consultant Obstetrician and Gynecologist in Breach Candy, Hinduja Healthcare Surgical, Holy Family and Masina Hospitals. He is the Secretary General and Past MTP Committee Chair of the Federation of Obstetric and Gynecological Societies of India and Past President of the Mumbai Obstetric and Gynecological Society. He also holds many positions as Member, Board of Directors, IPAS and CEDPA India; Member, Technical Advisory Panel, Ministry of Health and Family Welfare, Government of India; and Member, Medical Advisory Panel, Family Planning Association of India. He is also a Former Member in the Governing Council of the International Planned Parenthood Federation.
References
- 1.International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-06: India: Volume I. Mumbai: IIPS;2007. http://www.measuredhs.com/pubs/pdf/FRIND3/00FrontMatter00.pdf. Accessed 2 Jun 2013.
- 2.United Nations, Department of Economic and Social Affairs, Population Division. 2011. World Contraceptive Use 2010 (POP/DB/CP/Rev2010). http://www.un.org/esa/population/publications/wcu2010/WCP_2010/Data.html. Accessed 2 Jun 2013.
- 3.Bitzer J, Gemzell-Danielsson K, Roumen F, et al. The CHOICE study: effect of counselling on the selection of combined hormonal contraceptive methods in 11 countries. Eur J Contracept Reprod Health Care. 2012;17:65–78. doi: 10.3109/13625187.2011.637586. [DOI] [PubMed] [Google Scholar]
- 4.Lete I, Doval JL, Perez-Campos E, et al. Factors affecting women’s selection of a combined hormonal contraceptive method: the TEAM-06 Spanish cross-sectional study. Contraception. 2007;76:77–83. doi: 10.1016/j.contraception.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Makade KG, Padhyegurjar M, Padhyegurjar SB, et al. Study of contraceptive use among married women in a slum in Mumbai. Natl J Community Med. 2012;3:40–43. [Google Scholar]
- 6.Jain R, Muralidhar S. Contraceptive methods: needs, options and utilization. J Obstet Gynecol India. 2012;61:626–634. doi: 10.1007/s13224-011-0107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nanda J, Kumar Adak D, Bharati P. Contraceptive practices among adolescent married women in Tamil Nadu, India. Asian Pac J Trop Dis. 2011;1:37–41. doi: 10.1016/S2222-1808(11)60054-6. [DOI] [Google Scholar]
- 8.Kumar M, Meena J, Sharma S, et al. Contraceptive use among low-income urban married women in India. J Sex Med. 2011;8:376–382. doi: 10.1111/j.1743-6109.2010.02047.x. [DOI] [PubMed] [Google Scholar]
- 9.Merckx M, Donders GG, Grandjean P, et al. Does structured counselling influence combined hormonal contraceptive choice? Eur J Contracept Reprod Health Care. 2011;16:418–429. doi: 10.3109/13625187.2011.625882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gemzell-Danielsson K, Thunell L, Lindeberg M, et al. Comprehensive counselling about combined hormonal contraceptives changes the choice of contraceptive methods: results of the CHOICE program in Sweden. Acta Obstet Gynecol Scand. 2011;90:869–877. doi: 10.1111/j.1600-0412.2011.01180.x. [DOI] [PubMed] [Google Scholar]
- 11.Baveja R, Buckshee K, Das K, et al. Evaluating contraceptive choice through the method-mix approach. An Indian Council of Medical Research (ICMR) task force study. Contraception. 2000;61:113–119. doi: 10.1016/S0010-7824(00)00089-5. [DOI] [PubMed] [Google Scholar]
- 12.Bhasin SK, Pant M, Metha M, et al. Prevalence of usage of different contraceptive methods in East Delhi—a cross sectional study. Indian J Community Med. 2005;30:53–55. [Google Scholar]