Abstract
Objectives
To study the various predictors of success for vaginal birth after cesarean (VBAC) and to study the maternal and fetal outcomes in them and their comparison with control group.
Methods
This prospective observational study included 100 women with previous cesarean section in the study group and 100 primigravidas in the control group. Various predictors for success of VBAC were analyzed and maternal and fetal outcomes were compared with the control group using student t test, Pearson χ2 test, and Mann–Whitney U test.
Results
Of 100 women with prior cesarean Sect. 65 had successful trial of labor, while 35 underwent a repeat cesarean section. Maternal complications in the previous CS group were 15 % as compared to only 2 % in the control group (p < 0.001).
Conclusion
Maternal pre-pregnancy BMI, non-recurring indications of previous cesarean section, good Bishop’s score at the time of admission, spontaneous onset of labor, and neonatal birth weight were significantly related to high chances of success of vaginal birth after previous cesarean section. Maternal complications were more common in study group, but the fetal outcomes were similar.
Keywords: VBAC, Previous cesarean section, Predictors
Introduction
With the increasing number of cesareans in today’s era, we are often faced with the challenge of managing women with previous cesarean deliveries. In 1916, Dr. Edwin Cragin gave the famous statement“……..once a cesarean, always a cesarean.” This statement was apt in those times when the cesarean was almost always done by classical method. Now that the surgical techniques have vastly changed and we perform lower segment cesarean sections, this statement no longer holds its iron.
Vaginal birth after cesarean (VBAC) is a safe method of delivery and has many advantages but it carries the risk of rupture uterus. The risk of rupture uterus varies from 0.5 to 1 % but has a significant morbidity and mortality. It was noted that this potentially fatal event occurred mostly in those trying for VBAC section. Hence, it becomes imperative for obstetricians to be able to predict the factors governing the success of trial of labor.
The purpose of this study was to identify the obstetrical parameters that influence the success of vaginal delivery in women with previous cesarean section and to compare the maternal and fetal outcomes with the control group.
Materials and Methods
This prospective observational study was carried out on women attending the antenatal clinics of our hospital from May 2007 to April 2009. This study included 100 women with one prior cesarean section in the study group and 100 primigravida in the control group. Approval was obtained from the ethical committee of the hospital.
Inclusion criteria for the study were gestational age >36 weeks, singleton pregnancy, vertex presentation, and a documented transverse lower uterine segment scar. Complete history including age, pre-pregnancy BMI, indication of previous cesarean section, intra and postoperative complications of previous cesarean section, etc., was recorded. Patients who presented with intrauterine fetal death, two previous cesarean sections, a previous vertical uterine scar or a scar of other uterine surgery (myomectomy), clinically contracted pelvis, breech presentation at term in the current pregnancy, or any other contraindications to vaginal delivery like cephalopelvic disproportion, major degree placenta previa, transverse lie, etc., were excluded from the study.
All women were admitted in the hospital on their due date or earlier if they went into spontaneous labor. Those who failed to go into labor on their own were induced at 40 weeks of gestation. At the time of admission, a detailed examination was done for all women including the cervical examination. In patients with previous cesarean section for trial of labor, an informed consent was taken and 1 unit of cross-matched blood was kept arranged for emergency cesarean section, if the need should arise. In cases with unfavorable cervix (Bishop’s score <6), 0.5 mg of PGE2 gel was instilled in the cervical canal and repeated after 6 h, if required. Augmentation of labor was done, if required, with oxytocin. The progress of labor, whether spontaneous or induced, was monitored by:
Hourly recording of vital parameters—temperature, pulse, respiration, and blood pressure
Continuous electronic fetal monitoring
Monitoring of uterine contractions
Partograph
A close watch for early recognition of the scar dehiscence, by identifying maternal tachycardia in the absence of fever, vaginal bleeding, scars’ tenderness, and fetal heart rate alterations.
Attempt at vaginal delivery was abandoned if there was any suspicion of scar dehiscence or signs of fetal distress or unsatisfactory progress of labor. The duration of labor and also the maternofetal outcomes were recorded for all patients.
Maternal complications included third degree perineal tears, cervical tears, hematomas, post-op infection, scar dehiscence, need for internal iliac artery ligation, and need of blood transfusion.
Statistical analysis was performed with student t test for continuous variables, Pearson χ2 test for categorical variables, Mann–Whitney U test for ordinal variables, and binomial test of significance (two-tailed). A p value of 0.05 was chosen to represent statistical significance.
Results
Of 100 women with prior cesarean Sect. 65 had successful trial of labor, while 35 underwent a repeat cesarean section. Among 100 primigravidas, 77 had vaginal delivery and 23 had cesarean delivery.
The demographic characteristics of the study group and the control group were compared, and we observed that the two groups were comparable except that primigravidas were younger compared to the women with previous cesarean section. The two groups were also comparable with respect to onset of labor (i.e., whether spontaneous or induced) and the Bishop’s score at the time of admission.
Women with previous low transverse cesarean scar attempting VBAC were further subdivided in two groups, on the basis of success or failure of trial of labor, and the predictors of success of VBAC were then analyzed.
Of the 100 women with previous cesarean delivery, the rate of success of VBAC in the age group less than 30 years, 30–34 years, and more than 35 years was 60.7, 68.6, and 77.8 %, respectively. As seen, the rate of success of VBAC in our study appeared to improve with the increasing age, but the p value was only 0.524, suggesting the correlation between maternal age and success of VBAC to be statistically insignificant.
In our study, all the 10 women with BMI below 19.8 had a successful trial of labor (Table 1). Out of 49 women who had a pre-pregnancy BMI within the range of 19.8–26, 37 (75.5 %) delivered vaginally after a previous cesarean delivery while 12 (24.5 %) of them underwent a repeat cesarean section. Eighteen women were overweight, with a BMI value in the range of 26.1–29, and of these only 8 (44.4 %) delivered vaginally while 10 (55.6 %) had a repeat cesarean delivery. Of 23 obese women with a BMI more than 29, only 10 (43.5 %) women delivered vaginally. This observation suggested that as the pre-pregnancy BMI increased, the chances of successful VBAC decreased. A p value of 0.001 supports this and suggests a highly significant relation between BMI and success of trial of labor after previous cesarean delivery.
Table 1.
Success of VBAC in relation to pre-pregnancy BMI
| (Cases) previous CS | BMI in Kg/m2 | |||
|---|---|---|---|---|
| <19.8 | 19.8–26 | 26–29 | >29 | |
| Successful | 10 100 % |
37 75.5 % |
8 44.4 % |
10 43.5 % |
| Failed | 0 0 % |
12 24.5 % |
10 55.6 % |
13 56.5 % |
We further classified our 100 women with previous cesarean scar on the basis of the neonatal birth weight into four groups (<2, 2–3, 3–4, and >4 kg). The VBAC success rates in the subgroups were 100, 74.5, and 48.8 %, respectively. The p value of 0.017 suggested that this observed difference was statistically significant. Hence, suggesting that with increasing neonatal birth weight, the chances of successful vaginal delivery after previous cesarean delivery reduced.
In our study, 7 women gave history of post-op infection following their first cesarean section. The success rate of VBAC in these women did not differ from those who had no such history (71.4 vs. 64.5 %, respectively, p = 0.72).
In our study, while analyzing the indication of previous cesarean section as a predictor of success of VBAC (Table 2), we found that in patients where primary cesarean was done for fetal malpresentation or fetal distress, the chances of having a successful VBAC were better in comparison with those in whom primary cesarean was done for non-progress of labor or failed induction. Binominal test of significance(two-tailed) revealed that the difference was statistically significant in groups with previous cesarean done for breech and fetal distress(0.019 and 0.011, respectively) but not in those where previous cesarean was done for failed induction, non-progress of labor, or others like severe PIH (0.344, 1.0, and 0.263, respectively).
Table 2.
Indication of previous CS as predictor of VBAC
| Group | Indication of previous cesarean section | ||||
|---|---|---|---|---|---|
| Breech | Fetal distress | Failed induction | NPOL | Others | |
| Successful | 15 78.9 % |
26 72.2 % |
3 30 % |
8 53.3 % |
13 65 % |
| Failed | 4 21.1 % |
10 27.8 % |
7 70 % |
7 46.7 % |
7 35 % |
| Total | 19 | 36 | 10 | 15 | 20 |
| P value | 0.019 | 0.011 | 0.344 | 1.000 | 0.263 |
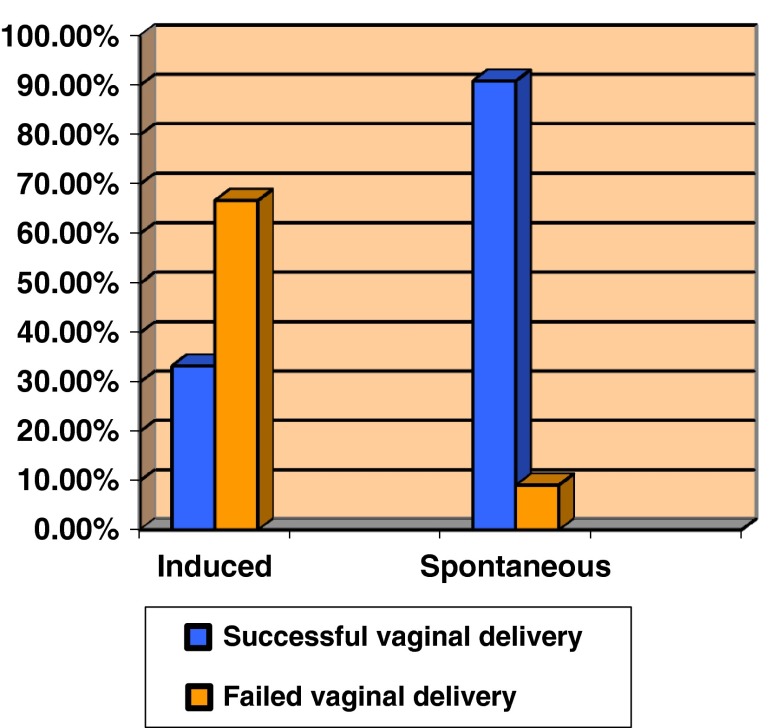
Of 100 women with previous cesarean section, 55 presented to hospital in spontaneous labor while 45 had to be induced. Of 55 patients who had spontaneous onset of labor, 50 (90.9 %) delivered vaginally and only 5 (9.1 %) had to be operated upon. Among 45 women who were induced for onset of labor, only 15 (33.3 %) had successful VBAC and rest of them i.e., 30 (66.7 %) underwent repeat cesarean section (Fig. 1). P value by χ2 test was 0.000, suggesting that the difference is highly significant. This depicts that the women with previous cesarean section who presented in spontaneous labor as compared to those who had to be induced for labor had higher number of successful VBAC.
Fig. 1.
Relation of onset of labor with success of VBAC
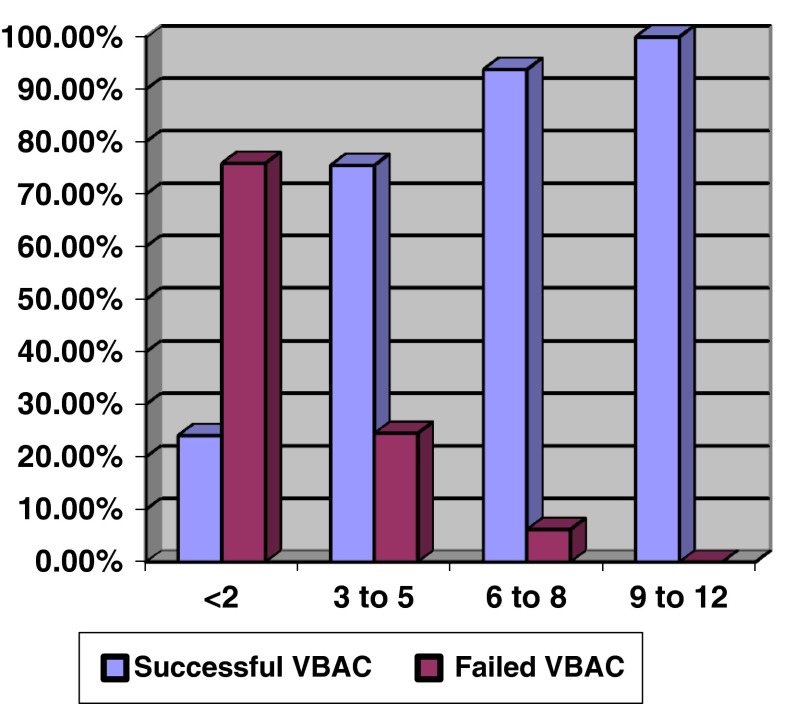
At the time of admission, all women with previous cesarean section underwent a detailed examination including Bishop’s score calculation (Fig. 2). These women were then classified into four groups according to the Bishop’s score (<2, 3–5, 6–8, and 9–12). Twenty-nine women had Bishop’s score below 2, 49 women had Bishop’ score in the range of 3–5, and 16 women had it in the range of 6–8. Six women presented in advanced labor, with a Bishop’s score above 9. Of 29 women who presented with Bishop’s score below 2, only 7 (24.1 %) had VBAC while majority of them (i.e., 75.9 %) had a repeat cesarean section. Thirty-seven (75.5 %) of the 49 women with Bishop’s score in the range of 3–5 delivered vaginally. Majority of the women (15/16 i.e., 93.8 %) with Bishop’s score in the range of 6–8 and all of the women with Bishop’s score above 9 had vaginal delivery. P value by χ2 was highly significant (p = 0.000). This, hence, suggests that the chances of vaginal delivery after previous cesarean section improve as the Bishop’s score at the time of admission increases.
Fig. 2.
Relation of Bishop’s score at admission and success of VBAC
Of 100 women with prior cesarean delivery, only 5 (5 %) babies needed NICU stay comparable to 4 (4 %) babies of primigravidas. P value by χ2 test was 0.733, indicating that this difference was not statistically significant. Also, the p value by χ2 test was 0.810, suggesting that the difference of perinatal morbidity in the two groups (successful and failed trial of labor) was statistically not significant.
Among 100 women with previous cesarean section, maternal morbidity in the form of scar dehiscence, postpartum hemorrhage, postpartum infection, need for blood transfusion, need for ligation of uterine arteries or internal iliac arteries, etc., was seen in 15 % as compared to only 2 % in the control group (Table 3). P value by Pearson χ2 test was 0.001, suggesting this difference to be statistically significant. Among 100 women with previous cesarean section, the morbidity was more commonly found in those who failed their trial of labor and underwent a repeat cesarean section as compared to the group who had a successful VBAC (p = 0.028) as seen in Table 3. Among 9 women who failed their trial of VBAC, 3 had scar dehiscence, 4 developed post-op infection, and 2 had atonic PPH. There were no cases of uterine rupture in this study.
Table 3.
Maternal morbidity
| Groups | Maternal morbidity | |
|---|---|---|
| No | Yes | |
| Cases | 85 | 15 |
| Successful VBAC | 59 | 6 |
| Failed VBAC | 26 | 9 |
| Controls | 98 | 2 |
Discussion
Vaginal birth after cesarean section was generally believed to be “safe.” Numerous studies have been reported detailing the success of safety of a trial of labor after a previous transverse lower uterine segment scar. In analyzing these trials of labor, investigators have sought to identify the conditions that may influence or inhibit a successful outcome.
Emmanuel Bujold et al. [1] and Srinivas et al. [2] analyzed the relation between maternal age and VBAC success. Both the studies concluded that women ≥35 years age were more likely to experience unsuccessful trial of labor. In our study, rate of success of vaginal delivery after previous cesarean delivery appeared to improve with increasing age (60.7 % vs. 68.6 vs. 77.8 %, respectively) but when p value was calculated (p = 0.524) this difference was found to be not significant.
As was seen in studies conducted by Carroll et al. [3] and Chauhan et al. [4] and Juhasz et al. [5], obese women were less likely to have successful VBAC, similar to the results found in our study wherein the chances of success of VBAC decreased from 100 to 43.5 % with increasing BMI.
Contrary to the popular belief, in our study we found no correlation between the history of previous vaginal delivery and the success of VBAC. But, the data for such a comparison were very small in the present study and may be a larger group should be recruited in future study.
As was also concluded in the study by Emmanuel et al. [6], the VBAC success rates in our study improved as the Bishop’s score at admission increased implying that modified Bishop’s score is an important predictor of success of VBAC.
Various studies (Peaceman et al. [7], Hoskins and Gomez [8], Shipp et al. [9], etc.) were done to study the influence of indication of previous cesarean section on the success of VBAC. In our study, we concluded that indication of previous CS is an important predictor of success of trial of labor. Women who underwent primary cesarean section for fetal malpresentation or fetal distress had more chances of having a successful VBAC as compared to those who underwent their primary cesarean for non-progress of labor or failure of induction. Also, women with spontaneous onset of labor and those with better Bishop’s score had more VBAC success rates than their counterparts.
In our study, we concluded that maternal pre-pregnancy BMI, neonatal birth weight, non-recurring indications of previous cesarean section, good Bishop’s score, and spontaneous onset of labor are predictors of success of vaginal birth after previous cesarean section. Also, there is no significant increase in perinatal morbidity though maternal morbidity was more common in women who failed their trial of labor. Hence, we recommend that it is very important to be able to accurately predict those whose trial of labor is likely to be a failure.
References
- 1.Bujold E, Hammoud AO, Hendler I, et al. Trial of labour in patients with a previous cesarean section: does maternal age influence the outcome? Am J Obstet Gynecol. 2004;190:1113–1118. doi: 10.1016/j.ajog.2003.09.055. [DOI] [PubMed] [Google Scholar]
- 2.Srinivas SK, Stamilio DM, Sammel MD, et al. Vaginal birth after caesarean delivery: does maternal age affect safety and success? Paediatr Perinatal Epidemiol. 2007;21(2):114–120. doi: 10.1111/j.1365-3016.2007.00794.x. [DOI] [PubMed] [Google Scholar]
- 3.Caroll CS, Magann EF, Chauhan SP, et al. Vaginal birth after caesarean versus elective repeat caesarean delivery, weight based outcome. Am J Obstet Gynecol. 2003;188:1516–1522. doi: 10.1067/mob.2003.472. [DOI] [PubMed] [Google Scholar]
- 4.Chauhan SP, Magann EF, Charroll CS, et al. Mode of delivery for morbidly obese with prior caesarean delivery vaginal versus repeat caesarean section. Am J Obstet Gynecol. 2001;185:349–354. doi: 10.1067/mob.2001.116729. [DOI] [PubMed] [Google Scholar]
- 5.Juhasz G, Gyamfi C, Gyamfi P, et al. Effect of body mass index and excessive weight gain on success of vaginal birth after cesarean delivery. Obstet Gynecol. 2005;106(4):741–746. doi: 10.1097/01.AOG.0000177972.32941.65. [DOI] [PubMed] [Google Scholar]
- 6.Bujold E, Blackwell SC, Hendler I, et al. Modified Bishop’s score and induction of labour in patients with previous caesarean delivery. Am J Obstet Gynecol. 2004;191:1644–1648. doi: 10.1016/j.ajog.2004.03.075. [DOI] [PubMed] [Google Scholar]
- 7.Peaceman AM, Gersnoviez R, Landon MB, et al. The MFMU cesarean registry: impact of fetal size on trial of labor success for patients with previous cesarean for dystocia. Am J Obstet Gynecol. 2006;195(4):1127–1131. doi: 10.1016/j.ajog.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Hoskins IA, Gomez JL. Correlation between maximum cervical dilatation at caesarean delivery and subsequent vaginal birth after caesarean delivery. Obstet Gynecol. 1997;89(4):591–593. doi: 10.1016/S0029-7844(97)00046-X. [DOI] [PubMed] [Google Scholar]
- 9.Shipp TD, Zelop CM, Repke JT, et al. Labour after previous caesarean: influence of prior indication and party. Obstet Gynecol. 2000;95:913–916. doi: 10.1016/S0029-7844(00)00790-0. [DOI] [PubMed] [Google Scholar]