Abstract
Objectives
To compare the cesarean delivery rates over the last decade and to examine the indications contributing to changed trends, if any.
Methods
To compare the rate and indications of cesarean delivery over the last decade, the data were collected in a retrospective manner from all the deliveries that occurred between January 1 and December 31 in 2001, 2006, and 2011, in the department of obstetrics and gynecology, Seth G.S. Medical College and K.E.M. Hospital, a large tertiary care municipal hospital in Western India. A cohort of 20853 delivered women was studied. The rates and indications of primary and repeat cesarean sections were analyzed among the live births to estimate the relative contribution of each indication to the overall increase in rate.
Results
The cesarean delivery rate increased from 171.70 to 289.30 per 1,000 live births, with an increase in primary cesarean delivery rate from 118.53 (69.03 %) in 2001 to 210.09 (72.62 %) in 2011 per 1,000 live births. Fetal distress, arrest of descent, multiple gestations, and fetal indications contributed to this increase.
Conclusions
There is a significant increase in the total cesarean rate with primary cesarean accounting for most of the increase.
Keywords: Cesarean rate, Primary cesarean birth, Repeat cesarean birth, Indications
Introduction
Cesarean section is one of the commonly performed surgical procedures in obstetrics and is certainly one of the oldest operations in surgery. One of the most dramatic features of modern obstetrics is the increase in the cesarean section rate [1, 2]. In recent years, the cesarean section rate has increased in different parts of the world, both in developed and developing countries. There is an increase in trend in both primary and repeat cesarean rates. The reasons for the increase are multifaceted. Fetal distress, especially its detection by continuous electronic fetal monitoring, more liberal use of cesarean section for breech presentation, abdominal delivery of growth-retarded infant, delayed childbearing, increasing maternal body mass, multiple gestation, prematurity, and improved safety of cesarean section are commonly cited causes [3]. This study aimed to compare the rate of primary and repeat cesarean delivery and to find out the relative contribution of various indications.
Materials and Methods
To compare the cesarean delivery rates over the last decade, the data were collected in a retrospective manner from all the deliveries that occurred in 2001, 2006, and 2011 for the interval between January 1 and December 31 in the department of Obstetrics and Gynecology, Seth G.S. Medical College and K.E.M. Hospital, a large tertiary care municipal hospital in western India. Data on all live births were collected, including type of delivery, and indication was recorded if cesarean section was done. Total, primary, and repeat cesarean section rates were calculated for each year. The cesarean rate was calculated as the number of cesarean births divided by total live births. The rate for each indication was calculated annually as the number of cesarean births performed for each indication per 1,000 live births. The categories of indication of cesarean section included fetal distress, multiple gestation, malpresentation, arrest of labor [arrest of dilatation or arrest of descent] (including failed forceps or vacuum extraction), cephalopelvic disproportion, maternal indications, and fetal indications. In our study, the category of fetal distress includes fetal distress during labor, non-reassuring and abnormal cardiotocogram when not in labor and abnormal umbilical artery doppler study. Maternal indications are the maternal conditions predating the pregnancy that could complicate delivery like vesicovaginal fistula repair, previous uterine surgery, and medical causes. Obstetric indications are the conditions brought about by the current pregnancy like placenta previa, abruptio placentae, placenta accreta, and cord prolapse. Fetal indications included intrauterine growth restriction, prematurity, and congenital malformations in which vaginal delivery was not possible. For repeat sections, cesarean was performed without trial for vaginal delivery in patients with history of 2 or more previous cesarean sections, with cephalopelvic disproportion and for those who presented with scar tenderness. Also, patients with previous cesarean section were counseled about vaginal birth after cesarean delivery. Cesarean section was electively performed for those who did not opt for vaginal birth.
Results
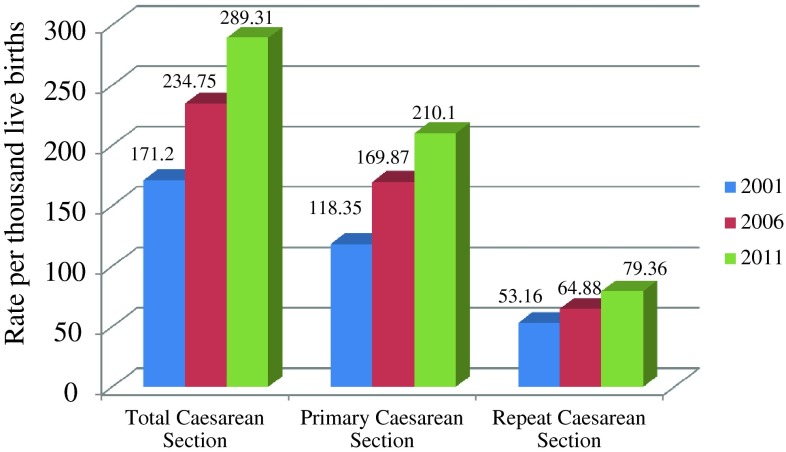
A total of 5,568, 7,706, and 6,716 live births occurred in the hospital in 2001, 2006, and 2011, respectively. The overall cesarean delivery rate and the trends in cesarean delivery were examined in relation to the total number of live births during the study period. The overall cesarean delivery rate increased from 2001 to 2006 to 2011. The average annual rate increased from 171.51 per 1,000 live births (17.15 %) in 2001 to 234.75 per 1,000 live births (23.47 %) in 2006 to 289.30 per 1,000 live births (28.93 %) in 2011. Both the primary and repeat cesarean delivery rates increased during this period (Fig. 1). The primary cesarean delivery rate increased from 118.35 per 1,000 live births (11.83 %) in 2001 to 169.86 per 1,000 live births (16.98 %) in 2006 to 210.09 per 1,000 live births (21.00 %) in 2011. The repeat cesarean delivery rate increased from 53.16 per 1,000 live births (5.31 %) in 2001 to 64.88 per 1,000 live births (6.48 %) 2006 to 79.36 per 1,000 live births (7.93 %) in 2011. The number of cases with age ≥35 years increased from 2001 to 2011. There was an increase in preterm births and multiple gestation (Table 1).
Fig. 1.
Change in cesarean section rate per 1,000 live births
Table 1.
Maternal characteristics among all live births during study period
| Percentage(absolute numbers) of total live births | |||
|---|---|---|---|
| 2001 | 2006 | 2011 | |
| Multiparous (parity ≥1) | 56.80 (3,163) | 47.91 (3,692) | 47.05 (3,160) |
| Preterm | 14.09 (785) | 15.84 (1,221) | 18.44 (1,239) |
| Age ≥35 | 2.26 (126) | 2.37 (183) | 3.40 (229) |
| Multiple gestation | 1.41 (79) | 1.69 (131) | 2.06 (139) |
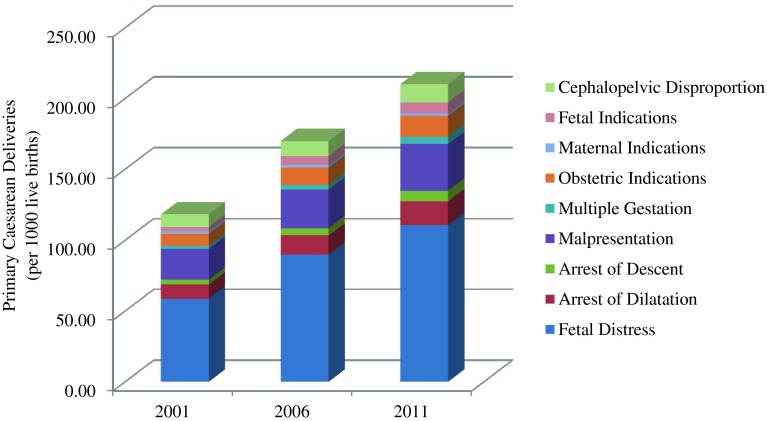
The rate of primary cesarean delivery among women with no history of cesarean birth increased from 11.83 % in 2001 to 21.00 % in 2011. The majority of increase is attributable to increase in fetal distress, arrest of descent, and fetal indications (Fig. 2; Table 2). With the exception of fetal distress that shows a progressive increase, there was no discernible trend in the other indications to possibly account for the increasing cesarean section rate.
Fig. 2.
Relative contribution of indications to primary cesarean delivery
Table 2.
Indications contributing to the increase in primary cesarean rate (per 1,000 live births)
| 2001 | 2006 | 2011 | |
|---|---|---|---|
| Fetal distress | 58.72 | 89.67 | 110.63 |
| Arrest of labor | 13.46 | 18.81 | 24.27 |
| Dilatation | 10.05 | 13.62 | 16.82 |
| Descent | 3.41 | 5.19 | 7.44 |
| Malpresentation | 21.73 | 27.12 | 32.90 |
| Multiple gestation | 2.15 | 3.37 | 5.21 |
| Obstetric indication | 8.44 | 12.06 | 14.59 |
| Maternal indication | 1.79 | 1.81 | 1.78 |
| Fetal indication | 3.05 | 6.35 | 7.74 |
| Cephalopelvic disproportion | 8.97 | 10.64 | 12.95 |
In the repeat sections, there was a rise in cases with fetal distress, scar tenderness, arrest of labor—both dilatation and descent and cephalopelvic disproportion (Table 3). Also, the number of cesarean sections performed for patients with history of two or more previous cesarean sections increased over the time period. There was also an increase in patients refusing vaginal birth after one previous cesarean section.
Table 3.
Specific indications contributing to the increase in repeat cesarean rate (per 1,000 live births)
| 2001 | 2006 | 2011 | |
|---|---|---|---|
| Fetal distress | 12.39 | 15.18 | 18.67 |
| Arrest of labor | 4.84 | 5.96 | 7.59 |
| Dilatation | 4.31 | 5.19 | 6.55 |
| Descent | 0.53 | 0.77 | 1.042 |
| Malpresentation | 4.31 | 5.32 | 6.40 |
| Multiple gestation | 3.05 | 3.24 | 2.82 |
| Obstetric indication | 1.07 | 1.42 | 1.93 |
| Maternal indication | 0.35 | 0.38 | 0.44 |
| Fetal indication | 0.89 | 1.16 | 2.38 |
| Cephalopelvic disproportion | 14.18 | 17.12 | 16.37 |
| ≥2 Cesarean section | 7.18 | 8.69 | 13.10 |
| Scar tenderness | 4.48 | 5.96 | 7.29 |
| Refusal of Vaginal Birth | 0.35 | 0.38 | 2.38 |
The number of elective cesarean sections in 2001, 2006, and 2011 was 12.21, 21, and 20.84 per 1,000 live births, respectively. The number of emergency cesarean sections in 2001, 2006, and 2011 was 159, 213, and 268 per 1,000 live births, respectively.
Discussion
Today, there is concern over the rising cesarean delivery rates, in both developed and developing countries across the world [2, 3]. The rates of both primary and repeat cesarean delivery have been on the rise [4].
In our study, from all the deliveries, the increase in average annual cesarean delivery rate, from 17.15 % in 2001 to 23.47 % in 2006 to 28.93 % in 2011, is consistent with the findings of other investigators. Barber et al. [4] showed an increase from 26 to 36.5 % between 2003 and 2009, and it changed from 10.6 % in 1997 to 19.1 % in 2006 in the case of Ba’aqeel [5]. A study conducted by Stavrou et al. [6] in New South Wales, Australia, showed an overall increase in cesarean rate from 19.1 to 29.5 per 100 births from 1998 to 2008. In a study conducted in Singapore by Chong et al. [7], the cesarean delivery rate increased from 19.9 to 29.6 per 100 births from 2001 to 2010. The reported increase in cesarean rate in Tanzania by Litorp et al. [8] has been higher, rising from 19 % in 2000 to 49 % in 2011. As per the OECD Health data 2011, the cesarean section rates in countries like Brazil, Mexico, and Turkey have exceeded 40 %. In India, a more accelerated rise in the cesarean section rate was observed from 9 % to 16 % in less than a decade between 1987 and 1997 [9]. Recently, Saha et al. [10] reported a rate of 29 % in 2007 in Kolkata. In our study, both the primary and repeat cesarean delivery rates increased during this period and as in Barber et al.’s study [4], the primary cesarean delivery rate accounted for most of the increase, from 11.83 % in 2001 to 16.98 % in 2006 to 21.00 % in 2011. As in our study, an increase in primary and repeat cesarean rates has been reported by Stavrou et al. [6]. The largest contributor to the primary cesarean delivery rate was fetal distress, similar to other reports ([4, 11, 12]). This is in contrast to findings of a study in the Welsh population conducted by Choudhary et al. [13], where previous cesarean rather than fetal distress was the largest contributor. This finding was contrary to the findings of their own national survey report which showed fetal distress as the largest contributor to cesarean delivery rate. This variation could be because the fetal distress taken in their study was based on fetal blood sampling, while in other studies as well in our study, non-reassuring fetal heart pattern before and during labor and abnormal umbilical artery doppler were taken as signs of fetal distress. The present study also shows an increase in labor arrest disorders, due to an increase in arrest of dilatation as well as descent. The change in the labor arrest due to an arrest of dilatation [4, 9] and due to arrest of descent [9, 11] has also been shown earlier. This increase in arrest of descent is possibly because of a decrease in difficult instrumental delivery over a period of time. The increase in fetal indication in our study is also similar to the study by Barber et al. [4], probably because of good antenatal care and good-sized fetuses. The higher contribution by fetal indications to increased cesarean rate also reflects better neonatal care with improved survival of intrauterine growth-retarded babies. Similarly, there has also been an increase in preterm live birth rates in this period. The obstetric characteristics of the study population show a decrease in parity. There were more patients with age ≥35 years in 2011 compared to 2006 and 2001, reflective of increased maternal age with time, also found by other investigators. In a study by Liu et al. [11], approximately 15 % of the increase in overall cesarean delivery rates was explained by increase in maternal age. Women with increased age are at a higher risk of cesarean section, which has also been highlighted in the systematic review conducted by Bayrampour et al. [14]. Multiple pregnancy rates increased in our study, a finding also reported earlier by Choudhary et al. [13].The findings of increased maternal age and multiple pregnancy rates may be because of increasing infertility and use of ovulation induction drugs.
For the repeat cesareans, the number of cases with ≥2 cesarean sections has increased as with Choudhary et al. [13]. There is an increase in the number of cases with arrest of dilatation and scar tenderness. These findings are similar to earlier reported studies [15].
Conclusions
The rate of cesarean section has increased from 2001 to 2011 with primary and repeat cesareans both showing an increase. In the primary cesarean section rate, indications like labor arrest disorders and fetal distress show an increase more than the objective indications like malpresentation. In repeat cesarean sections, history of two or more previous sections and scar tenderness contributed more than the fetal distress.
References
- 1.Turner MJ. Delivery after one previous caesarean section. Am J Obstet Gynaecol. 1997;176:741–744. doi: 10.1016/S0002-9378(97)70596-9. [DOI] [PubMed] [Google Scholar]
- 2.Oladapo OT, Sotunsu JO, Sule-Odu AO. The rise in caesarean birth rate in Sagamu, Nigeria: reflection of changes in obstetrics practice. J Obstet Gynaecol. 2004;24:377–381. doi: 10.1080/01443610410001685484. [DOI] [PubMed] [Google Scholar]
- 3.Tollånes MC. Increased rate of Caesarean sections—causes and consequences. Tidsskr Nor Laegeforen. 2009;129(13):1329–1331. doi: 10.4045/tidsskr.08.0453. [DOI] [PubMed] [Google Scholar]
- 4.Barber EL, Lundsberg LS, Belanger K, et al. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ba’aqeel Cesarean delivery rates in Saudi Arabia: a ten-year review. Ann Saudi Med. 2009;29(3):179–183. doi: 10.4103/0256-4947.51773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stavrou EP, Ford JB, Shand AW, et al. Epidemiology and trends for Caesarean section births in New South Wales, Australia: a population-based study. BMC Pregnancy Childbirth. 2011;20(11):8. doi: 10.1186/1471-2393-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chong C, Su LL, Biswas A. Changing trends of cesarean section births by the Robson Ten Group Classification in a tertiary teaching hospital. Acta Obstet Gynecol Scand. 2012;91(12):1422–1427. doi: 10.1111/j.1600-0412.2012.01529.x. [DOI] [PubMed] [Google Scholar]
- 8.Litorp H, Kidanto HL, Nystrom L, et al. Increasing caesarean section rates among low-risk groups: a panel study classifying deliveries according to Robson at a university hospital in Tanzania. BMC Pregnancy Childbirth. 2013;8(13):107. doi: 10.1186/1471-2393-13-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta A, Apers L, Verstraelen H, et al. Trends in caesarean section rates at a maternity hospital in Mumbai. India J Health Popul Nutr. 2001;19(4):306–312. [PubMed] [Google Scholar]
- 10.Saha S, Saha S, Das R, et al. A paradigm shift to check the increasing trend of cesarean delivery is the need of hour: but how? J Obstet Gynaecol India. 2012;62(4):391–397. doi: 10.1007/s13224-012-0288-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu S, Rusen ID, Joseph KS, et al. Recent trends in caesarean delivery rates and indications for caesarean delivery in Canada. J Obstet Gynaecol Can. 2004;26(8):735–742. doi: 10.1016/s1701-2163(16)30645-4. [DOI] [PubMed] [Google Scholar]
- 12.Krychowska A, Kosińska K, Karwan-Płońska A. Comparison of indications for caesarean section in 1985–86 and 2000–01: analysis of changes. Ginekol Pol. 2004;75(12):926–931. [PubMed] [Google Scholar]
- 13.Choudhary AP, Dawson AJ. Trends in indications for caesarean sections over 7 years in a Welsh district general hospital. J Obstet Gynaecol. 2009;29(8):714–717. doi: 10.3109/01443610903191269. [DOI] [PubMed] [Google Scholar]
- 14.Bayrampour H, Heaman M. Advanced maternal age and the risk of cesarean birth: a systematic review. Birth. 2010;37(3):219–226. doi: 10.1111/j.1523-536X.2010.00409.x. [DOI] [PubMed] [Google Scholar]
- 15.Abu-Heija A, Zayed F. Primary and repeat caesarean sections: comparison of indications. J Obstet Gynaecol. 1998;18(5):432–434. doi: 10.1080/01443619866723. [DOI] [PubMed] [Google Scholar]