Abstract
Background
Life course theory emphasizes the need to examine a wide variety of distal factors along with proximal factors, longitudinally. Yet research on who obtains substance use treatment is generally cross-sectional and limited to examining developmentally proximal factors (e.g., substance use severity) and demographic factors.
Methods
To investigate treatment within a life-course framework, we studied 522 drug and/or alcohol users from a community cohort of African Americans followed prospectively from age 6. Developmentally distal factors of childhood and adolescent social behavior, family environment, academic achievement, mental health, and substance use along with the key proximal factors of substance use severity and socioeconomic status were examined using regression analyses to assess their impact on obtaining adult substance use treatment.
Results
One-fifth of the study population obtained treatment for substance use by age 32 (20.5%). Although adult socioeconomic status was not associated with substance use treatment in adulthood in the multivariable model, the proximal factor of substance use severity was a strong predictor of obtaining substance use treatment, as expected. After including several developmentally distal factors in the model, childhood aggression also had an independent effect on adult substance use treatment, above and beyond substance use severity.
Conclusions
These findings emphasize the importance of using a life course framework when exploring predictors of treatment; early life characteristics are important influences beyond the more proximal factors in adulthood. Research should continue to take a life course approach to better understand pathways to substance use treatment.
Keywords: substance use, life course, risk factors, substance abuse treatment
1. Introduction
Substance use treatment has been shown to be effective at reducing drug and alcohol use and the problems associated with it (Institute of Medicine, 2006; McLellan et al., 2000a; Miller et al., 2001). Yet, despite this, treatment is vastly underutilized by substance users; approximately 4.3 million individuals in the U. S. received treatment in 2009, yet 24 million, a six fold difference, were in need of substance use treatment (Substance Abuse and Mental Health Services Administration, 2010).
Numerous cross-sectional studies, which have focused on concurrent or proximal predictors, find that the most consistent predictor of obtaining treatment is substance use severity (Finney and Moos, 1995; Kessler et al., 2001; Oleski et al. 2010; Perron et al., 2009; Wang et al, 2004). Other key proximal predictors include income and treatment accessibility (Mark et al., 2007; Compton et al., 2007).
What has been lacking in the extant literature is the application of a life course perspective, which considers an individual's present and past circumstances acknowledging that receiving treatment may be influenced by historical and developmental factors as well as current severity or income. This perspective considers an actor's accumulation of risk or protection rather than at one point in time (Elder, 1985). Using a life course framework to examine substance use treatment across multiple periods of adulthood, rather than a snapshot of who may be in treatment at a single point in time, provides a more comprehensive view of who obtains treatment (Hser et al., 2007). Past experiences, relationships, and circumstances may be particularly important in considering who enters treatment beyond severity and financial costs as there are multiple avenues to obtaining treatment (Pescosolido et al., 1998). The life course framework can help identify key factors throughout the life course important for treatment, broadening our understanding of treatment and facilitating the targeting of efforts to increase substance use treatment utilization.
Historically, research focused on who receives substance use treatment has faced two challenges: first, the preponderance of cross-sectional studies and second, a limited set of predictors of obtaining treatment. A prospective research design that draws on a life course framework encourages examination of the influence of early and developmental factors on receipt of substance use treatment in adulthood.
While studies have used the life course framework to examine predictors of substance use and abuse across the life course (e.g., Fothergill and Ensminger, 2006; Doherty et al., 2008), these studies have not examined early life influences on substance use treatment. This may be due to the assumption that any effect of childhood influences on treatment is explained by substance use severity in adulthood or other proximal factors such as socioeconomic status (SES). However, whether early life factors work solely through need (e.g., substance use severity) or resources (e.g., SES), or whether they exert a direct influence on obtaining substance use treatment has not been examined empirically.
This line of research is crucial given longitudinal research that suggests numerous pathways to mental health treatment. For instance, family life, social behavior, and severity of mental health conditions distinguish which children receive mental health services in childhood and adolescence (Herrenkohl et al., 2010; Poduska et al., 2008; Temcheff et al., 2011). For substance use treatment, in particular, Gayman et al. (2011) found family background and severity of substance use were related to obtaining substance use treatment in childhood and adolescence. They did not examine if these factors continued to be important for adult substance use treatment. Also, the sample had a small number of African Americans, leaving it unclear if their findings may be particularly salient for African-American populations.
Understanding what influences receipt of substance use treatment among African-American populations is important for several reasons. First, African Americans are more likely than Whites to report problems from their use, including loss of control and health problems (Harrison, 1992; Herd, 1994, 1997). Second, African Americans suffer twice as many deaths due to substance use-related causes as do Whites (National Institute on Drug Abuse, 2003). Third, African-Americans have similar or higher rates of obtaining substance use treatment compared to Whites (Grella et al. 2009; Kessler et al., 2001; Perron et al., 2009; Mulvaney-Day et al., 2012), yet African-American substance users continue to use through adulthood when their White counterparts are more likely to cease using (French et al., 2002).
Moreover, some research suggests that pathways into treatment may differ for African Americans compared to Whites regardless of severity of use. Interactions with the criminal justice system (Swanson et al., 2009; LeCook and Alegria, 2011) and other public services such as Medicaid are possible mechanisms by which African Americans are more likely to obtain treatment than other groups. One study found African Americans were more likely to be referred to treatment when reporting alcohol use to social services systems, regardless of the individual's alcohol consumption (Dobscha et al., 2009). Understanding the antecedents of obtaining substance use treatment in this population more fully will inform efforts to increase treatment, potentially alleviating some public health burden in this population.
In this paper we pose two research questions, (1) Do distal factors during childhood and adolescence (e.g., family background, early childhood behavior) matter in obtaining treatment as an adult? (2) If so, are these distal factors important for obtaining treatment above and beyond the well-known proximal factors (e.g., drug use severity) that influence receipt of substance use treatment? Importantly, this study overcomes the challenges of previous studies by using a prospective longitudinal design that extends into adulthood and by taking a life course approach to allow for the explicit consideration of a wide variety of distal factors along with key proximal factors related to substance use treatment.
2. Methods
2.1 Study Population
Study participants are part of the Woodlawn Study, a longitudinal prospective study of 1242 African Americans growing up in a community on Chicago's South Side. Individuals entered the study in 1966-67 when they were in first grade. During this cohort's childhood and adolescence, Woodlawn was a poor, virtually all African-American community with high levels of poverty and unemployment. All first graders in the Woodlawn community, attending one of the nine public or three parochial schools, were invited to participate; only 13 families (1%) declined. The current study used data collected at three time points: childhood (age-6-7; n=1242), adolescence (age 16-17; n=705), and young adulthood (age 32-34, n=952).
Since we were interested in substance use treatment, the sample was limited to those individuals interviewed in young adulthood who had a history of significant substance use (i.e., had a history of heavy episodic drinking (4 or more drinks for women and 5 or more drinks for men on a single occasion) or used other substances 50 times or more by age 32 (n=522)). In order to capitalize on the strength of having a non-clinical population of substance users, the sample was not limited to those with a substance use disorder (SUD). Alcohol and use of other substances were examined together as research has not consistently shown predictors of treatment to differ significantly by substance (Perron et al., 2009; Wang et al., 2005). Figure 1 provides a description of study inclusion criteria.
Figure 1.
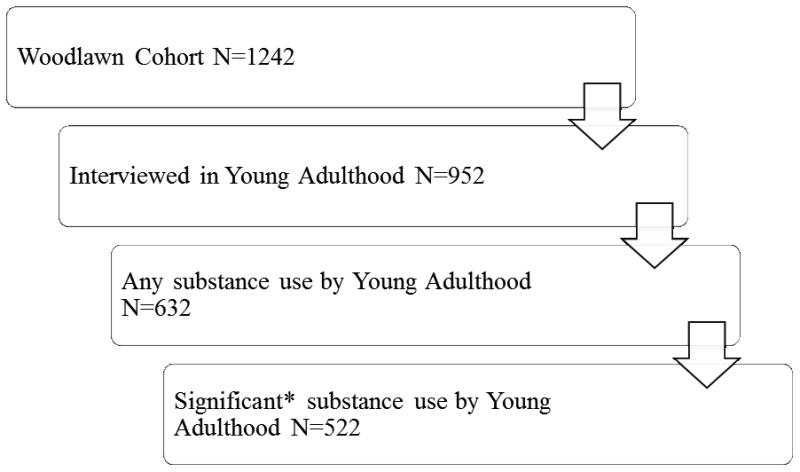
Selection of study sample.
*Significant substance use = Lifetime history of binge drinking OR any lifetime use of other substances greater than 50 times.
Self-report questions: Alcohol: Have you ever used alcohol? What is the most drinks you have ever had on a single occasion?
Other substance use: How many times in your life have you taken (for non-medical purposes): barbiturates, tranquilizers, stimulants/amphetamines, analgesics, inhalants, marijuana/hashish, cocaine/crack, LSD and other hallucinogens, heroin?
In first grade, data were collected from teachers regarding each child's classroom behavior and from mothers regarding the child's behavior and family environment. In adolescence, both mothers and children were interviewed regarding a variety of domains including: substance use, mental and physical health, family environment, and school achievement. At age 32, participants were re-interviewed regarding myriad social and psychological factors, including: health behaviors, employment, family structure, social relationships, and substance use behaviors. The initial assessment in 1966-67 occurred before institutional review boards evaluated study protocols. However, during the adolescent assessment the University of Chicago, and for later assessments the Johns Hopkins School of Public Health, reviewed and approved all study procedures. Because of significant attrition in the adolescent interview, we tested for potential attrition biases comparing those who were interviewed in adolescence to those who were not. With one exception (those interviewed were more likely to have ever used heroin and marijuana by adulthood), no differences were found with regard to any childhood or young adulthood characteristics.
2.2 Measures
2.2.1 Dependent Variable: Adult substance use treatment
Substance use treatment was measured at age 32 by two self-report indicators of lifetime treatment:
Have you ever been hospitalized or stayed overnight in a treatment center for your use of alcohol or drugs? (yes/no)
Did you ever go to a self-help group such as Alcoholics Anonymous for your use of alcohol or drugs? (yes/no)
These two were combined to create a dichotomous measure of any adult substance use treatment. Individuals who endorsed at least one of the two items were considered to have received treatment. If the last treatment occurred before age 18 (the case for two individuals) they were considered not to have received treatment as an adult because receiving treatment as an adolescent is categorically different than as an adult (Brown et al., 1994; Winters, 1999). Approximately one-fifth (20.5%, n=107) received treatment between ages 18 and 32 for their substance use according to the above criteria. Of the 107 receiving treatment, 86.0% (n=92) attended a self-help group and 71.0% (n=76) were hospitalized. Over half (57%, n=61) received both types of treatment.
To check predictive validity of the treatment measure and determine whether we should examine the two indicators separately or together, we examined how childhood and adolescent predictors compared for the two items. Table 1 provides the sample size and number of lifetime SUD symptoms for those who were hospitalized, attended a self-help group, or received both. All 3 groups had approximately the same number of symptoms. Predictors of attending a self-help group and being hospitalized were virtually the same with regard to all distal and proximal predictors. With respect to reliability, the correlation coefficient for the two items was 0.80. The kappa, measuring the degree of agreement between the two items (Cohen, 1960) was 0.65, indicating excellent agreement (Landis and Koch, 1977). Taken together this suggested combining the two indicators was appropriate.
Table 1. Comparison of Treatment Indicators, N=522.
| N % | # of SUD symptoms M(SD) | |
|---|---|---|
| No Treatment | 415 (79.5%) | 0.6 (1.3) |
| Any Treatment | 107 (20.5%) | 3.8 (2.7) |
| Inpatient/Hospitalization | 76 (14.6%) | 4.1 (2.8) |
| Self-help | 92 (17.6%) | 3.8 (2.6) |
| Both Self-help and Inpatient/Hospitalization | 61 (11.7%) | 4.2 (2.7) |
2.2.2 Independent Variables
2.2.2.1 Gender
Although most national epidemiologic studies have found no difference in treatment by gender (Grella et al., 2009; Kessler et al., 2001; Perron et al., 2009; Siegal et al., 2002), some research shows men are more likely to obtain treatment for an alcohol use disorder than women (Oleski et al., 2010; Schober and Annis, 1996). Further, studies among minority populations have found men more likely to obtain treatment than women (Beals et al., 2006). Therefore, gender was included as a control variable.
2.2.2.2 Distal factors
As described in Table 2, five domains in childhood and adolescence were included as distal factors to examine their association with substance use treatment: 1.Childhood and adolescent behavior includes measures of childhood classroom behavior and adolescent delinquency; 2 Early family environment includes measures of family poverty (childhood and adolescence combined), parental education, family involvement, and family conflict in adolescence; 3.Academic achievement includes measures of first grade readiness to learn, adolescent school bonds, and educational attainment; 4.Early mental health includes measures of mother's report of childhood psychological wellbeing, adolescent mental health and mental health help received in adolescence; and 5. Adolescent substance use includes self-report measures of alcohol use, substance use, and adolescent-onset of a SUD.
Table 2. Measurement of distal and proximal factors.
| Variable | Description |
|---|---|
| Gender | Gender of child was measured via mother's self-report at age 6. |
| Distal Factors | |
| Child and adolescent behavior | |
| Classroom behavior | Measured in first grade. Teacher reported using the Teacher Observation of Classroom Adaptation (TOCA) of any maladaptive classroom behavior in five behavioral domains: shyness (e.g. timid, alone too much, friendless), aggressiveness (e.g. fights, lies, resists authority, disobedient), underachievement (e.g. does not work as well as assessment of ability indicates), restlessness (fidgets, is unable to sit still in class), and immaturity (e.g. acts too young physically and/or emotionally, cries too much, seeks too much attention). The TOCA measure has been shown to be valid and reliable (Kellam, Branch, Agrawal, & Ensminger, 1975). |
| Delinquency | Measured in adolescence. The sum of 18, 4-point self-reported indicators. Range 0-72, α = 0.83. Items were adapted from a scale by Gold and colleagues (1970). |
| Early family environment | |
| Family poverty | Measured in first grade and adolescence. Using poverty guidelines from the Office of Economic Opportunity for 1967 and 1976 (Department of Health, Education and Welfare, 1977), categories of no poverty, poverty at either childhood or adolescence, or persistent poverty (poverty in childhood and adolescence) created from primary caregiver's self-report of income and household size. |
| Parental education | Measured in first grade. Self-reported education level of primary caregiver: dichotomized into 0-11 years vs. 12+ years of education. |
| Family involvement | Measured in adolescence. Sum of five indicators (e.g., how often family members did things together such as work on homework and do community activities) ranging from 5=less than every few months to 1= several times a week. These were summed into a single construct. Range: 5-30; α=0.69. |
| Family conflict | Measured in adolescence. Sum of five indicators (e.g., how often family members said mean things to each other, how often family members yelled at each other) ranging from 5=less than every few months to 1= several times a week. These were summed into a single construct, Range: 5-30; α = 0.94. |
| Academic achievement | |
| Readiness to learn | Measured in first grade. Metropolitan Readiness to Learn, a standardized test administered in schools in 1st grade as a measure of a child's readiness for school (Anastasi, 1968). Range 0 (i.e., not ready) to 100 (i.e., very ready). |
| School bonds | Measured in adolescence. Sum of five, 5 and 6 point self-report indicators (e.g., “how far do you think you will go in school?,” “how often do you skip school?”). Range: 5-28; α= 0.67. |
| Educational attainment | Measured at age 32. Dichotomized into obtained high school diploma vs. did not obtain high school diploma. |
| Early mental health | |
| Childhood psychological wellbeing | Measured in first grade. Using the Mother Symptom Inventory (validity previously demonstrated; Conners, 1967), the mother (or primary care giver) self-reported a 4 point 38-item inventory of symptoms of depression and anxiety in children. Tertiles were created of low, moderate, high scores, α= 0.79. |
| Adolescent mental health | Measured in adolescence. A self-report of anxiety and depression symptoms: six depression questions and seven anxiety items. Response choices were on a scale of 1 to 6, ranging from “not at all” to “very, very much.” Each scale was standardized. Psychometric examination of these original measures is published elsewhere and shows a moderate degree of internal consistency for both depression (α=0.69) and anxiety (α=0.68) and construct validity is also demonstrated (Petersen & Kellam, 1977). |
| Help received in adolescence | Measured in adolescence. Mother's report of whether child received any help for emotional, learning, behavioral, or drug problems from a youth agency since childhood assessment. Dichotomized to any help vs. no help. |
| Adolescent substance use | |
| Alcohol use | Measured in adolescence. Self-report of whether ever used and frequency of beer, wine, liquor. Categorized into no use, experimental use (1-19 times), and regular use (20+ times). |
| Early substance use | Measured in adolescence. Self-report of any substance use (marijuana, cocaine, LSD/psychedelics, amphetamines/uppers, barbiturates/downers, tranquilizers, opiates, inhalants, and cough syrup/codeine use) before age 14. |
| Adolescent-onset substance use disorder | Measured at age 32. The Composite International Diagnostic Interview (CIDI), a structured diagnostic interview developed by the University of Michigan for the National Comorbidity Survey (Kessler et al., 1994) was used to construct the age of onset of a substance use disorder. Responses were then categorized into adolescent-onset (≤18 years) vs. no adolescent-onset. |
| Proximal Factors | |
| Substance use severity | Substance use disorder symptoms were measured at age 32. The number of substance use disorder symptoms endorsed on the CIDI was used as a continuous measure of substance use severity. (Range 0-11). |
| Socioeconomic status at age 32 | |
| Health insurance | Measured in young adulthood (age 32). Self-report of current receipt of any health insurance. |
| Poverty | Measured in young adulthood (age 32). Using 1992 Federal guidelines from the Department of Health and Human Services, individuals were dichotomized into below or above the poverty threshold based on self-reported income and household size. |
| Unemployment | Measured in young adulthood (age 32). Self-report of current unemployment. |
2.2.2.3 Proximal Factors
Table 2 also outlines the two proximal factors examined in this study. The first is substance use severity measured by the number of substance use disorder symptoms endorsed by the cohort member by age 32, using the Composite International Diagnostic Interview (Kessler, 1994). We used the number of substance use disorder symptoms here rather than the presence of a SUD diagnosis because it allows severity to be measured on a continuum rather than using a cut off, providing a more thorough examination of level of severity (Dawson et al., 2010). Second, we examine socioeconomic status, which includes measures of health insurance status, poverty, and unemployment at age 32. These resource measures have been found to impact treatment but not universally. Some have found lifetime prevalence of treatment to be greater among those with lower income (Compton et al., 2007), while others have found no differences in past year treatment seeking by education and employment (Davey et al. 2007; Grella et al. 2009; Perron et al., 2009; Wang et al. 2004).
2.3 Analysis
All analyses were conducted using Stata 10.0. Bivariate logistic regression analyses were conducted to assess the relationship between each theoretically and empirically-derived factor, and substance use treatment. Multivariable logistic regression analyses were then run to examine if the distal (early life) characteristics were predictive of obtaining treatment after controlling for proximal factors (i.e., substance use severity and socioeconomic status at age 32). Along with theory and previous research, we used Hosmer and Lemeshow's (2000) recommendation of a p<0.20 inclusion criteria to select variables that are suggestive of a relationship for the final model, as the p<0.05 criteria “often fails to identify important variables” (pg. 91). This also allowed us to include variables that may only be significant in concert with others even if not statistically significant in bivariate analyses. Given the number of related variables in the multivariable model, we examined multicollinearity using the Variance Inflation Factor. All variables were less than five, well below the recommended maximum of 10 (Hair et al., 1995).
2.3.1 Multiple Imputation
Multiple imputation is one of the best methods for dealing with missing data greater than 5% (Graham, 2009; Stuart et al., 2009) and has been shown to produce valid standard errors and estimates. The variables used in this study had missing data ranging from 1% to 40%. This study used Multivariate Imputation by Chained Equations to create 20 imputed datasets. All regression analyses were performed using these multiply imputed data.
3. Results
3.1 Sample Characteristics
Table 3 describes the sample with respect to background and substance use. By design, all individuals used at least one substance by age 32, however, the type of substances used varied. Alcohol (92%) and marijuana (87%) were used by most individuals. Cocaine was also fairly common (42%), while heroin use was less frequent (11%). The proportion in poverty increased from early life, when approximately 32% were persistently living below the poverty threshold, to almost 45% at age 32. While a large proportion was unemployed at age 32 (35%), the majority had some form of health insurance (76%).
Table 3.
Cohort Characteristics of Woodlawn Study Substance Users by age 32 (N=522).
| Variables | Percent or Mean(SD) |
|---|---|
| Female | 43.49 |
| Early Social Behavior | |
| First Grade Classroom Behavior | |
| Aggressive | 33.89 |
| Shy | 31.67 |
| Underachieving | 43.19 |
| Restless | 33.82 |
| Immature | 35.53 |
| Adolescent Delinquency (0-72) | 17.87 (15.61) |
| Early Family Environment | |
| Poverty | |
| No Poverty | 31.81 |
| Poverty at 1 Time Point | 36.60 |
| Persistent Poverty | 31.59 |
| Parent Education | |
| <HS Diploma | 57.57 |
| HS Diploma | 42.43 |
| Family Involvement (5-30) | 16.37 (15.59) |
| Family Conflict (5-30) | 20.78 (16.34) |
| Academic Achievement | |
| Readiness to Learn (0-100) | 58.38 (19.62) |
| School Bonds (5-28) | 12.66 (7.82) |
| High school diploma | 74.52 |
| Mental Health | |
| Mother's Symptom Inventory (1st grade) | |
| Low | 39.20 |
| Medium | 33.41 |
| High | 27.39 |
| Help Received in Adolescence | 29.48 |
| Adolescent Mental Health | |
| Anxious | 21.83 (14.46) |
| Depressed | 19.54 (13.40) |
| Adolescent Substance Use | |
| Other substance use by age 14 | 22.80 |
| Alcohol Use | |
| No Use | 9.62 |
| Experimental Use | 35.20 |
| Regular Use | 55.28 |
| Adolescent-onset of SUD (by age 18) | 15.71 |
| Lifetime substance use by age 32 | |
| Alcohol use | 91.95 |
| Illegal substance use | 89.08 |
| Marijuana use | 86.78 |
| Cocaine use | 48.47 |
| Heroin use | 10.73 |
| Substance use severity (# of SUD symptoms) | 1.44 (2.36) |
| Socioeconomic status at age 32 | |
| Health insurance | 76.44 |
| Poverty | 44.26 |
| Unemployment | 35.06 |
3.2 Bivariate Analyses
Table 4, Column A, presents the bivariate logistic regression models of the relationship of distal and proximal factors with adult substance use treatment.
Table 4.
Bivariate and Multivariable Logistic Regression Models of Childhood and Adolescent Predictors of Treatment for Substance Use (N=522).
| Column A | Column B | |||
|---|---|---|---|---|
|
| ||||
| Bivariate | Multivariable | |||
| OR | 95% CI | aOR | 95% CI | |
| Female | 0.54* | (0.34, 0.84) | 0.76 | (0.36,1.58) |
| Proximal Factors | ||||
| Substance use severity | 2.28* | (1.97, 2.64) | 2.45* | (2.04, 2.96) |
| Socioeconomic status at age 32 | ||||
| Health insurance | 0.40* | (0.25, 0.67) | 0.77 | (0.36, 1.67) |
| Poverty | 1.74* | (1.11, 2.71) | 0.79 | (0.38, 1.65) |
| Unemployment | 2.26* | (1.47, 3.48) | 1.43 | (0.71, 2.88) |
| Distal Factors | ||||
| Early Social Behavior | ||||
| First Grade Classroom Behavior | ||||
| Aggressive | 2.09* | (1.35, 3.23) | 2.17* | (1.10,4.28) |
| Shy | 1.06 | (0.67, 1.67) | ||
| Underachieving | 1.26 | (0.82, 1.92) | ||
| Restless | 1.49+ | (0.96, 2.30) | ||
| Immature | 1.28 | (0.83, 1.99) | ||
| Adolescent Delinquency | 1.01 | (0.99, 1.03) | ||
| Early Family Environment | ||||
| Parent education | ||||
| <HS diploma | Ref. | Ref. | ||
| HS diploma | 0.73+ | (0.47, 1.13) | 0.67 | (0.33, 1.33) |
| Poverty | ||||
| None | Ref. | |||
| At 1 Time Point | 1.07 | (0.60, 1.90) | ||
| Persistent Poverty | 1.17 | (0.67, 2.07) | ||
| Family Involvement | 1.01 | (0.99, 1.04) | ||
| Family Conflict | 1.00 | (0.98, 1.02) | ||
| Academic Achievement | ||||
| 1st grade Readiness to Learn (MRT) | 1.00 | (0.99, 1.01) | ||
| School Bonds | 1.01 | (0.97, 1.06) | ||
| Educational Attainment | ||||
| <HS diploma | Ref. | |||
| HS diploma | 0.64+ | (0.40, 1.01) | 1.11 | (0.52, 2.38) |
| Mental Health | ||||
| Mother's Symptom Inventory | ||||
| Low | Ref. | Ref. | ||
| Moderate | 1.12 | (0.69, 1.81) | 0.90 | (0.43, 1.86) |
| High | 0.64· | (0.36, 1.13) | 0.64 | (0.27, 1.51) |
| Adolescent Help Received | 1.11 | (0.65, 1.90) | ||
| Adolescent Anxiety (standardized) | 0.87 | (0.62, 1.22) | ||
| Adolescent Depression (standardized) | 0.94 | (0.68, 1.29) | ||
| Adolescent Substance Use | ||||
| Early Substance Use | ||||
| No use ≤14 | Ref. | Ref. | ||
| Use ≤14 | 3.00* | (1.89, 4.75) | 1.55 | (0.74, 3.25) |
| Adolescent Alcohol Use | ||||
| No Use | 0.43· | (0.12, 1.54) | 0.27 | (0.03, 2.32) |
| Experimental Use | Ref. | Ref. | ||
| Regular Use | 1.22 | (0.75, 2.00) | 1.10 | (0.50, 2.42) |
| Adolescent-onset of SUD | 4.96* | (2.99, 8.22) | 0.42 | (0.18, 1.01) |
p<0.20,
p < 0.10,
p < 0.05 (For multivariable analyses, only p<0.05 denoted)
3.2.1 Gender
While the sample was fairly evenly split by gender (43.5% female), less than one-third of those who received treatment were female (31.8%).
3.2.2 Proximal factors
As expected, substance use severity, measured by the number of SUD symptoms, was a significant predictor of obtaining treatment with each additional SUD symptom being associated with greater than two times the odds of obtaining treatment. Moreover, all three measures of SES at age 32: health insurance, poverty, and unemployment were significantly associated with obtaining treatment. In line with Compton et al. (2007), higher SES was associated with lower odds of obtaining treatment. Those with health insurance were less likely to obtain treatment than those without (OR: 0.40; 95% CI: 0.25, 0.67) and those below the poverty threshold and unemployed were approximately two times more likely to obtain treatment (OR: 1.74 and 2.26, respectively).
3.2.3 Distal Factors
Three of the twenty childhood factors were significantly associated with obtaining substance use treatment in adulthood. Those who were rated as aggressive by their teachers in first grade had twice the odds of receiving substance use treatment in adulthood (OR: 2.09; 95% CI: 1.35, 2.23) compared to those not rated as aggressive in first grade. Additionally, those who started using substances at an early age (≤ 14) had three times greater odds of obtaining treatment than those who did not (OR: 3.00; 95% CI: 1.89, 4.75) and those who had an adolescent-onset of a substance use disorder (SUD) had almost five times the odds of obtaining treatment than those who did not (OR: 4.96; 95% CI: 2.99, 8.22).
3.3 Multivariable Analyses
Table 4, Column B, presents the adjusted odds ratios from the multivariable analyses, which includes all variables with a p value <0.20 in the bivariate analysis, with one exception. We did not include restlessness in the final model for two reasons; previous research reveals considerable overlap in children who are restless and children who are aggressive, with aggression showing a stronger relationship with negative health outcomes (Kellam et al., 1980). Indeed, there was considerable correlation between aggression and restlessness (r=0.62, p<0.001). Second, when restlessness is included in the multivariable model, results are not substantively different and restlessness is not associated with obtaining treatment.
These multivariable analyses show a continued significant two-fold association between substance use severity and substance use treatment in adulthood. This association remained strong and rendered many other key factors non-significant, including each measures of SES. It is important to note that this lack of relationship between SES and substance use treatment remained when each measure of SES was included in the multivariable model separately, suggesting that substance use severity is largely responsible for the attenuation of this effect. Being male was also attenuated in the multivariable analyses, likely due to males' higher SUD symptoms. Moreover, in the multivariable model, neither early substance use nor adolescent-onset of a SUD was significantly associated with obtaining treatment.
Although most factors associated with substance use treatment fell to non-significance when substance use severity was included in the model, first grade aggressive behavior remained significantly associated with treatment. Moreover, the strength of the association was not attenuated with those rated as aggressive still having twice the odds of receiving substance use treatment in adulthood compared to those who were not rated as aggressive in first grade (OR: 2.17; 95% CI: 1.10, 4.28).
3.4. Post Hoc Analyses
Although we were not able to conduct proper mediation analyses to test the pathway of early aggressive behavior and receipt of other health and public services, due to temporal ordering issues, we conducted post hoc analysis to investigate this relationship. Analyses revealed that those rated as aggressive were almost two times more likely to receive help for emotional, learning, or behavioral problems in early life (41.3% vs. 23.4%; p<0.05), and to have a history of incarceration (39.3% vs. 22.5%; p<0.05). They were also 1.5 times more likely to receive public assistance (38.1% vs. 25.7%; p<0.05) and to receive some form of medical treatment for a serious physical condition (40.9% vs. 26.3%; p<0.05). The increased interaction with these services may, in part, explain the link between aggressive behavior and obtaining substance use treatment.
4. Discussion
Our results are consistent with earlier literature showing that substance use severity is a major predictor of obtaining treatment. However, this study also highlights the importance of early life factors in obtaining substance use treatment. Aggression, measured in first grade, was not attenuated by substance use severity in magnitude or statistical significance. Moreover, other studies of this cohort have shown aggressive behavior to be associated with using substances, developing a SUD in adulthood (Fothergill and Ensminger, 2006), and lower educational attainment (Ensminger et al., 2002); yet, when controlling for severity and SES, childhood aggressiveness remained significantly associated with obtaining treatment in adulthood. This finding reinforces the importance of adopting a life course perspective and the inclusion of distal factors when examining substance use treatment.
The post-hoc analyses lend some insight into this association between childhood aggression and substance use treatment. We found that aggressive children were more likely to obtain services in childhood than those without aggression, which is consistent with prior research on conduct problems and mental and physical health services (Poduska et al., 2008; Scott et al., 2001). While these previous studies examined general medical and mental health treatment rather than substance use treatment, they provide a plausible pathway from aggression to treatment of any type. Because we see the relationship between aggressive behavior and treatment regardless of SUD severity, these individuals may be obtaining treatment regardless of need. Previous studies have suggested African-American individuals in particular may receive treatment because of coercion through involvement with the criminal justice system (LeCook et al., 2011) and social services (Dobscha et al., 2009). However, the use of other services by aggressive individuals may also suggest that aggressive individuals have more mental health co-morbidities increasing both their odds of treatment and other services. A final explanation is that these individuals may have fewer social resources to draw upon when they experience substance use problems and are thus, more likely to turn to formal treatment services. Previous research, including previous analyses of the Woodlawn cohort, has shown early aggressive behavior to be related to a lack of supportive social connections (Sampson and Laub, 1992; Ensminger et al., 2009).
We note the limitations of examining predictors of substance use treatment in this population. First, all individuals were born around 1960 and from a single, predominately urban African-American community so generalization of the findings to other populations must be done cautiously. However, this is also a strength in the study that all individuals grew up in the same community and are the same age, allowing inherent control of many neighborhood and age-cohort factors which may otherwise confound analyses. We also relied on self-report to measure substance use, which has its limitations, yet studies have shown self-report of substance use to be valid and reliable (Babor et al., 2000; Darke, 1998), and work from the Woodlawn cohort show no systematic bias in the self-reports in these data (Ensminger et al., 2007).
Our measures of treatment are another challenge for the study. We did not extensively examine treatment options, but the high overlap of the two indicators gives some reassurance that we captured a high proportion of those who obtained treatment. Moreover, this study examined whether individuals ever obtained any substance use treatment. This required retrospection over 14 years which may have resulted in some inaccurate recall. However, because individuals did not need to provide details of the treatment episode this is less concerning. Additionally, we did not examine the treatment quality or length, thus, we can only draw conclusions about what differentiates individuals who receive treatment from those who never receive treatment. An important future direction in a study with a larger sample and information on multiple types of substance use treatment could examine differences in distal predictors by treatment modality and treatment quality.
The strengths of the study—the prospective design over a long period of the life course, the availability of information from many life domains, and the use of a community population to examine substance use treatment—enable us to add to the extant knowledge about what influences obtaining treatment. In sum, our findings suggest early identifiable life factors, even as young as first grade, influence receipt of substance use treatment. Further research is needed to understand the pathways from childhood aggressive behavior to substance use treatment using mediational analyses to examine how and whether this pathway is mediated by receipt of other services or social support and whether this relationship is specific to African-American populations. Because we found this relationship regardless of severity, research is also needed to examine how childhood aggressive behavior is related to the quality and duration of treatment and if this increased likelihood of treatment leads to improved substance use outcomes. While African Americans obtain treatment at higher rates, they are less likely to receive specialty services (Schmidt et al., 2007) and less likely to complete treatment (Blumenthal et al., 2007) which may be related to more treatment coercion among African Americans through the criminal justice system and social services (LeCook et al., 2011).
Better coordination and standards to integrate social services and the criminal justice system with quality substance use treatment programs are needed. Finally, more research is needed that examines substance use and substance use treatment longitudinally over the life course, particularly among African Americans. This type of research can enable us to better understand how individual characteristics, early life experiences, substance use, and treatment pathways interact.
Highlights for Review.
Using a life course approach we examine factors related to substance use treatment.
Children rated as aggressive were more likely to receive substance use treatment.
In post-hoc analysis aggressive children were more likely to obtain other services.
Better integration of substance use treatment and other social services is needed.
Acknowledgments
We wish to thank the Woodlawn community and the Woodlawn Project Board for their support and cooperation in this project over many years.
Role of funding source: Funding for this study was provided by NIDA grants R01 DA 022366, R01 DA 033999, T32 DA 007292, and T32DA017629. NIDA had no further role in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Contributors: Dr. Evans-Polce formulated the research question, conducted the statistical analyses, and wrote the initial draft of the manuscript. Drs. Doherty and Ensminger provided feedback on the scope of the research project and assisted in writing and editing of the manuscript. Dr. Ensminger is the Principal Investigator of the Woodlawn study. All authors have read and approved the final version of the manuscript.
Conflict of Interest: No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anastasi A. Psychological Testing. Collier-Macmillan; London: 1968. [Google Scholar]
- Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug Alcohol Depend. 1995;40:9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]
- Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: measuring drinking outcomes in clinical trials. J Stud Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Beals J, Novins DK, Spicer P, Whitesell NR, Mitchell CM, Manson SM The American Indian Service Utilization, Psychiatric Epidemiology, Risk,and Protective Factors Project Team. Help seeking for substance use problems in two American Indian reservation populations. Psychiatr Serv. 2006;57:512–520. doi: 10.1176/ps.2006.57.4.512. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Mott MA, Vik PW. Correlates of success following treatment for adolescent substance abuse. Appl Prev Psychol. 1994:361–373. [Google Scholar]
- Carroll KM, Rounsaville BJ. Contrast of treatment-seeking and untreated cocaine abusers. Arch Gen Psychiatry. 1992;49:464–471. doi: 10.1001/archpsyc.1992.01820060044007. [DOI] [PubMed] [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Conners CK. The syndrome of minimal brain dysfunction: psychological aspects. Pediatric Clin N Am. 1967;14:749–766. doi: 10.1016/s0031-3955(16)32053-3. [DOI] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Davey MA, Latkin CA, Hua W, Tobin KE, Strathdee S. Individual and social network factors that predict entry to drug treatment. Am J Addict. 2007;16:38–45. doi: 10.1080/10601330601080057. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Saha TD, Grant BF. A multidimensional assessment of the validity and utility of alcohol use disorder severity as determined by item response theory models. Drug Alcohol Depend. 2010;107:31–38. doi: 10.1016/j.drugalcdep.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty EE, Green KM, Ensminger ME. Investigating the long-term influence of adolescent delinquency on drug use initiation. Drug Alcohol Depend. 2008;93:72–84. doi: 10.1016/j.drugalcdep.2007.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eland-Goossensen A, van de Goor IA, Garretsen HF. Heroin addicts in the community and in treatment compared for severity of problems and need for help. Subst Use Misuse. 1997;32:1313–1330. doi: 10.3109/10826089709039380. [DOI] [PubMed] [Google Scholar]
- Elder GH., Jr . Life Course Dynamics: Trajectories And Transitions. Cornell University Press; Ithaca, NY: 1985. pp. 1968–1980. [Google Scholar]
- Ensminger ME, Juon HS, Fothergill KE. Childhood and adolescent antecedents of substance use in adulthood. Addiction. 2002;97:833–844. doi: 10.1046/j.1360-0443.2002.00138.x. [DOI] [PubMed] [Google Scholar]
- Ensminger ME, Juon H, Green KM. Consistency between adolescent reports and adult retrospective reports of adolescent marijuana use: Explanations of inconsistent reporting among an African American population. Drug Alcohol Depend. 2007;89:13–23. doi: 10.1016/j.drugalcdep.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensminger ME, Juon HS, Lee RD, Lo S. Social connections in the inner city: examination across the life course. Longit Life Course Stud. 2009;1:11–26. doi: 10.14301/llcs.v1i1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing T. Substance Abuse and Mental Health Services Administration. Center for Substance Abuse Treatment; Rockville, MD: 2002. Patterns Of Substance Use Among Minority Youth And Adults In The United States: An Overview And Synthesis Of National Survey Findings. [Google Scholar]
- Finney JW, Moos RH. Entering treatment for alcohol abuse: a stress and coping model. Addiction. 1995;90:1223–1240. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- Fothergill KE, Ensminger ME. Childhood and adolescent antecedents of drug and alcohol problems: a longitudinal study. Drug Alcohol Depend. 2006;82:61–76. doi: 10.1016/j.drugalcdep.2005.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayman M, Cuddeback G, Morrissey J. Help-seeking behaviors in a community sample of young adults with substance use disorders. J Behav Health Serv Res. 2011;38:464–477. doi: 10.1007/s11414-011-9243-1. [DOI] [PubMed] [Google Scholar]
- Gold M. Delinquent Behavior In An American City. Brooks/Cole; Oxford, England: 1970. [Google Scholar]
- Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US, Moore AA, Niv N. Perceptions of need and help received for substance dependence in a national probability survey. Psychiatr Serv. 2009;60:1068–1074. doi: 10.1176/appi.ps.60.8.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair JF, Jr, Anderson RE, Tatham RL, Black WC. Multivariate Data Analysis. 3rd. Macmillan; New York: 1995. [Google Scholar]
- Harrison LD. Trends in illicit drug use in the United States: conflicting results from national surveys. Int J Addict. 1992;27:817–847. doi: 10.3109/10826089209068769. [DOI] [PubMed] [Google Scholar]
- Herd D. Predicting drinking problems among black and white men: results from a national survey. J Stud Alcohol. 1994;55:61–71. doi: 10.15288/jsa.1994.55.61. [DOI] [PubMed] [Google Scholar]
- Herd D. Sex ratios of drinking patterns and problems among blacks and whites: results from a national survey. J Stud Alcohol. 1997;58:75–82. doi: 10.15288/jsa.1997.58.75. [DOI] [PubMed] [Google Scholar]
- Herrenkohl TI, Kosterman R, Mason WA, Hawkins JD, McCarty CA, McCauley E. Effects of childhood conduct problems and family adversity on health, health behaviors, and service use in early adulthood: tests of developmental pathways involving adolescent risk taking and depression. Dev Psychopathol. 2010;22:655–665. doi: 10.1017/S0954579410000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd. Wiley & Sons; New York, NY: 2000. [Google Scholar]
- Hser Y, Longshore D, Anglin DM. The Life Course perspective on drug use: a conceptual framework for understanding drug use trajectories. Eval Rev. 2007;31:515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- Hubbard RL, Craddock SG, Anderson J. Overview of 5-year followup outcomes in the drug abuse treatment outcome studies (DATOS) J Subst Abuse Treat. 2003;25:125–134. doi: 10.1016/s0740-5472(03)00130-2. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. National Academies Press; Washington, DC: 2006. [PubMed] [Google Scholar]
- Kellam SG, Branch JD, Agrawal KC, Ensminger ME. Mental Health And Going To School: The Woodlawn Program Of Assessment, Early Intervention And Evaluation. The University of Chicago Press; Chicago: 1975. [Google Scholar]
- Kellam SG, Ensminger ME, Simon MB. Mental health in first grade and teenage drug, alcohol, and cigarette use. Drug Alcohol Depend. 1980;5:273–304. doi: 10.1016/0376-8716(80)90003-4. [DOI] [PubMed] [Google Scholar]
- Kellam SG, Branch JD, Brown CH, Russell G. Paths leading to teenage psychiatric symptoms and substance use: developmental epidemiological studies in Woodlawn. J Am Acad Child Psychiatry. 1982;20:477–495. doi: 10.1016/s0002-7138(09)61641-1. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Berglund PA, Caraveo-Anduaga JJ, DeWit DJ, Greenfield SF, Vega WA. Patterns and predictors of treatment seeking after onset of a substance use disorder. Arch Gen Psychiatry. 2001;58:1065–1071. doi: 10.1001/archpsyc.58.11.1065. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the national comorbidity survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol. 2001;62:211–220. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- Mulvaney-Day N, DeAngelo D, Chen C, Cook BL, Alegria M. Unmet need for treatment for substance use disorders across race and ethnicity. Drug Alcohol Depend. 2012;125:S44–S50. doi: 10.1016/j.drugalcdep.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Drug Use Among Racial/Ethnicminorities. National Institute on Drug Abuse; Rockville, MD: 2003. DHHS Publication No. NIH 03-3888. [Google Scholar]
- Oleski J, Mota N, Cox BJ, Sareen J. Perceived need for care, help seeking, and perceived barriers to care for alcohol use disorders in a national sample. Psychiatr Serv. 2010;61:1223–1231. doi: 10.1176/ps.2010.61.12.1223. [DOI] [PubMed] [Google Scholar]
- Perron BE, Alexander-Eitzman B, Watkins D, Taylor RJ, Baser R, Neighbors HW, Jackson JS. Ethnic differences in delays to treatment for substance use disorders: African Americans, black Caribbeans and non-hispanic whites. J Psychoactive Drugs. 2009;41:369–377. doi: 10.1080/02791072.2009.10399775. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Gardner CB, Lubell KM. How people get into mental health services: stories of choice, coercion and “muddling through” from “first-timers”. Soc Sci Med. 1998;46:275–286. doi: 10.1016/s0277-9536(97)00160-3. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Kellam SG. Measurement of the psychological well-being of adolescents: the psychometric properties and assessment procedures of the how I feel. J Youth Adolesc. 1977;6:229–247. doi: 10.1007/BF02138937. [DOI] [PubMed] [Google Scholar]
- Poduska JM, Kellam SG, Wang W, Brown CH, Ialongo NS, Toyinbo P. Impact of the good behavior game, a universal classroom-based behavior intervention, on young adult service use for problems with emotions, behavior, or drugs or alcohol. Drug Alcohol Depend. 2008;95:S29–S44. doi: 10.1016/j.drugalcdep.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcohol Clin Exp Res. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Putnam I. Poverty thresholds: their history and future development. In: Orshansky M, editor. Documentation of Background Information and Rationale for Current Poverty Matrix (Technical Paper I of The Measure of Poverty) Washington, D.C.: U.S. Department of Health, Education, and Welfare; 1970. 1977. [Google Scholar]
- Sampson RJ, Laub JH. Crime and deviance in the life course. Ann Rev Sociol. 1992;18:63–84. [Google Scholar]
- Schmidt L, Greenfield T, Mulia N. Unequal treatment: racial and ethnic disparities in alcoholism treatment services. Alcohol Res Health. 2006;29:49–54. [PMC free article] [PubMed] [Google Scholar]
- Schober R, Annis HM. Barriers to help-seeking for change in drinking: a gender-focused review of the literature. Addict Behav. 1996;21:81–92. doi: 10.1016/0306-4603(95)00041-0. [DOI] [PubMed] [Google Scholar]
- Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001;323:191. doi: 10.1136/bmj.323.7306.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegal HA, Falck RS, Wang J, Carlson RG. Predictors of drug abuse treatment entry among crack-cocaine smokers. Drug Alcohol Depend. 2002;68:159–166. doi: 10.1016/s0376-8716(02)00192-8. [DOI] [PubMed] [Google Scholar]
- Stuart EA, Azur M, Frangakis C, Leaf P. Multiple imputation with large data sets: a case study of the children's mental health initiative. Am J Epidemiol. 2009;169:1133–1139. doi: 10.1093/aje/kwp026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 national survey on drug use and health: Volume I Summary of National Findings (No HHS Publication No SMA 10-4586) Rockville, MD: 2010. [Google Scholar]
- Swanson J, Swartz M, Van Dorn RA, Monahan J, McGuire TG, Steadman HJ, Robbins PC. Racial disparities in involuntary outpatient commitment: are they real? Health Aff (Millwood) 2009;28:816–826. doi: 10.1377/hlthaff.28.3.816. [DOI] [PubMed] [Google Scholar]
- Temcheff C, Serbin L, Martin-Storey A, Stack D, Ledingham J, Schwartzman A. Predicting adult physical health outcomes from childhood aggression, social withdrawal and likeability: a 30-year prospective, longitudinal study. Int J Behavl Med. 2011;18:5–12. doi: 10.1007/s12529-010-9082-0. [DOI] [PubMed] [Google Scholar]
- Wang P, Berglund PA, Olfson M, Kessler RC. Delays in initial treatment contact after first onset of a mental disorder. Health Serv Res. 2004;39:393–416. doi: 10.1111/j.1475-6773.2004.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Winters KC. Treating adolescents with substance use disorders: an overview of practice issues and treatment outcome. Subst Abuse. 1999;20:203–224. doi: 10.1080/08897079909511407. [DOI] [PubMed] [Google Scholar]
- Yu J, Williford WR. The age of alcohol onset and alcohol, cigarette, and marijuana use patterns: an analysis of drug use progression of young adults in New York state. Subst Use Misuse. 1992;27:1313–1323. doi: 10.3109/10826089209047353. [DOI] [PubMed] [Google Scholar]


