Abstract
One key component in HIV prevention is serostatus disclosure. Until recently, many studies have focused on interpersonal factors and minimally considered meeting venues as they pertain to disclosure. Using data (N=3309) from an online survey conducted across 16 US metropolitan statistical areas, we examined whether HIV serodisclosure varies by online/offline meeting venues in both protected and unprotected anal intercourse encounters. Most of the sample (76.9%) reported meeting men for sex (last 90 days) both online and offline, versus 12.7% offline only and 10.4% online only. After controlling for other variables, we found that the men who meet partners in both online and offline were 20~30% more likely to report disclosing their HIV status prior to sex than men who met their partners exclusively either offline or online. While previous studies have identified the Internet as a risk environment, our findings suggest bi-environmental partner seeking may also have beneficial effects.
Keywords: Men who have sex with men, HIV disclosure, Meeting venue, SILAS, Online, Offline
Introduction
The Centers for Disease Control and Prevention (CDC) estimates that approximately 1.2 million people in the United States are living with HIV/AIDS and an estimated one in five people are unaware that they have the infection [1]. The majority of the new cases in the US are occurring in men who have sex with men (MSM). While MSM comprise only 4% of the general population, they account for 78% of new HIV diagnoses among men and 63% of all new infections [1]. Disclosure of HIV status to sexual partners may reduce risk of transmission in sero-discordant partnerships [2] and has been promoted as a sexual risk reduction strategy to appraise risk in sexual partnerships [3], screen potential partners for the same HIV status as oneself (i.e., serosorting) [4], and negotiate sexual practices that may reduce the risk of HIV transmission (i.e., strategic positioning) [5].
HIV status disclosure among sexual partners is a complex process characterized by several attributes, including age [6], race/ethnicity [6,7], income [2] relationship status [8,9], sexual identity (i.e., bisexual men vs. gay men) [10], openness as gay/homosexual [11], and sexual partner meeting environment [12]. In addition, disclosure among men varies by an individual’s own serostatus. HIV-positive men may seek out same HIV status partners for many reasons, including limiting the risk of transmission to a HIV-negative partner, legal concerns regarding laws requiring HIV disclosure, and psycho-social factors such as stigma, fear of rejection and safe sex fatigue [5,13,14]. By contrast, HIV-negative men may be motivated to seek out same serostatus partners to avert risk of infection to themselves [14].
HIV disclosure can also vary by type of sexual behavior; either unprotected anal intercourse (UAI) or protected anal intercourse (PAI). Engaging in either UAI or PAI is a choice that is not always “rational” [15]. The intent to use protection in a sexual encounter can vary from what actually ends up happening when the opportunity presents itself [15,16]. HIV serodisclosure discussions prior to sex enable both individuals to make healthier and informed choices regarding their choice of partners, the type of sex engaged in, and whether protection is necessary [17]. Many MSM believe that provided they use protection during their sexual encounters, no disclosure of HIV is necessary [18–21]. This is also a defense in some states which otherwise require HIV-positive persons to serodisclosure prior to sex. HIV disclosure is also important in terms of individuals who participate in UAI and the potential legal implications of non-disclosure if one is infected with the disease [22].
The environment where an individual meets a potential partner has been significantly associated with either safer sex or unsafe sexual decision-making as well as subsequent behaviors [11,15,19,23,24]. In the last two decades, the popularity of using the Internet to locate sexual partners has skyrocketed due to the medium’s accessibility, affordability, anonymity and acceptability [25–27]. Websites and smart phone/mobile apps such as Manhunt.net, Adam4Adam.com, Grindr, Gay.com, Craigslist, and many others have now become very popular for sexual and social networking among MSM both in the US and internationally. The Internet provides a unique opportunity for easier disclosure of HIV serostatus than standard “offline or physical” meeting venues (such as, bar/club, party, school, work, bathhouse, park, gym, etc) as individuals can simply write or check their serostatus on their online profiles [13,25,28,29]. However, researchers have noted that there is a high level of inaccurate serodisclosure in “online or virtual” environments [30]. In addition, men who use the Internet to seek sex with men report more sexual partners and a higher frequency of unprotected anal intercourse (UAI) than men who only seek partners offline [26,31].
Despite the popularity of Internet-based meeting environments, the use of “offline or physical” meeting venues still remains quite common [15]. Offline or physical venue environments include private parties, bars, bathhouses, through friends, work, community events, support groups, school, gyms, public restrooms, parks, and countless other places [23]. It is debatable whether offline or online environments are more conducive to HIV disclosure. In at least some offline environments, verbal communication is considered inappropriate or awkward (e.g. parks, public restrooms, bathhouses) and can impede HIV serostatus disclosure. Other offline environments, such as meeting through mutual friends or at a party may introduce additional challenges to disclosure if there is concern about mutual friends overhearing or learning of one’s HIV status. MSM-themed community events may facilitate HIV disclosure due to a higher perceived comfort level among individuals. Online, the way profiles are set up may facilitate or impede HIV disclosure, and whether or how much a reader reads and adequately comprehends the profile likely varies across MSM.
Several studies which have examined the role of the meeting venue on HIV disclosure, have typically compared ‘online’ and ‘offline’ settings by treating them as mutually exclusive [23,25,32]. Today, many if not most, MSM use a combination of environments to meet their potential sexual partners [33,34]. In this study, our primary purpose is to compare how MSM who meet partners for sex, online, offline or both online and offline environments, vary in their HIV serodisclsoure. In addition, given the lack of prior studies studying “both online and offline” environment, we sought to identify personal and behavioral variables that might affect disclosure of HIV status. “Online only” refers to MSM who report first meeting partners only “virtually,” such as through the use of various dating or “hookup” websites and mobile apps, (e.g., Grindr, Adam4Adam, Manhunt, Dudesnude, Bigmuscle) and then hooking up for sex. “Offline only” refers to MSM who report first meeting partners only in physical (non-virtual) locales, whether it would be at a gay bar/club, party, school, work, bathhouse, park, gym, or any type of environment not preceded by initial online contact. “Online-offline” refers to MSM who report meeting men for sex in both environments.
Within the Social Cognitive Theory framework, Bandura [35] explained human behavior in terms of a triadic, dynamic and reciprocal model in which personal factors, behavior and environmental influences all interact. Following Bandura’s typology we model our analysis to examine personal, behavioral, and environmental factors potentially associated with HIV disclosure. Since online environments have more ways of serodisclosing, we hypothesize that MSM who meet partners for sex only online or in virtual environment should have the highest rates of HIV serodisclosure; men who meet partners offline or in physical environment, the lowest rates, with MSM who meet partners in both environments reporting rates in between.
Methods
Study Participants
In 2008, we began a four-wave prospective, matched-sample study of MSM in 16 U.S. metropolitan statistical areas (MSAs). Defined by the U.S. Office of Management and Budget (OMB) [36], and used by the U.S. Census, an MSA is a geographical region with relatively high population density, and close social and economic ties throughout the area. A typical MSA is centered on a single large city that wields substantial influence over the region (e.g., the greater Chicago, or Atlanta area, as distinct from the city limits). The purpose of the Structural Interventions to Lower STI/HIV risk (SILAS) study [29,37] was to assess the extent to which legislation about homosexuality influenced alcohol use and risky sexual behavior among MSM. Data for this analysis came from the fourth wave of data collection. We recruited 5,047 MSM into wave four between May 20, 2011, and December 26, 2011. The eligibility criteria were being a biological male, having prior sexual experience with a man, being 18 years or older, and reporting a residential zip code in a MSA under study. This analysis was restricted to participants (N=3309, 65.6%) with complete data on meeting venue and at least one sex partner in the past three months prior to the survey.
Data Collection Procedures
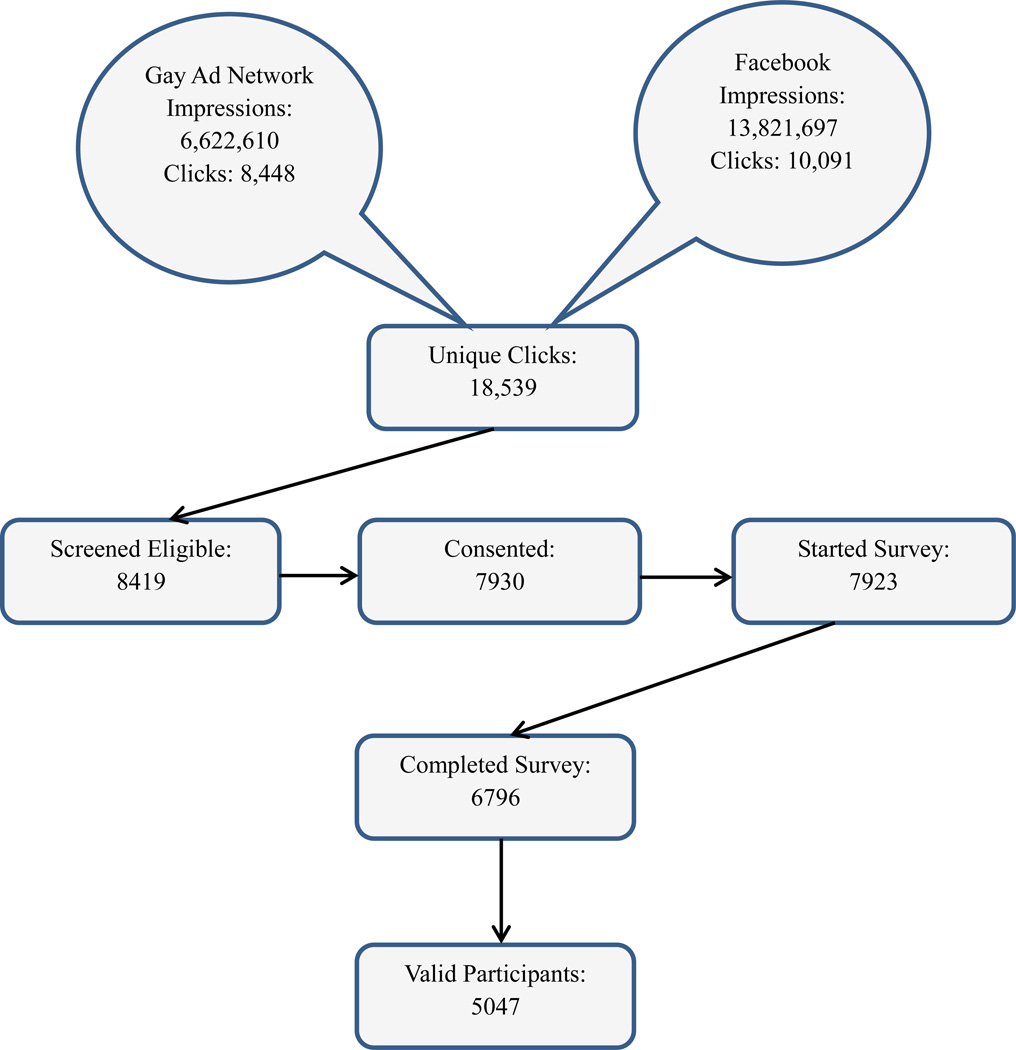
Participants were recruited with geo-targeted banner advertisements to adult male members of Facebook (http://www.facebook.com) who self-identified as attracted to men; and to men who frequented websites affiliated with the Gay Ad Network (Quantcast Corporation, n.d.). Banner advertisements and emails directed interested persons to a webpage hosted on a dedicated university server with appropriate encryption to ensure data security. The webpage included information about the study procedures and a link to the eligibility screener. Eligible respondents were invited to complete our consent protocol. Initially, 8,419 enrollees were deemed eligible, 7,930 consented to participate and 6,796 completed the survey. We adapted a standard de-duplication and cross-validation protocol developed by our team to exclude participants with duplicate or suspicious surveys [38, 39] and impossible or nonsensical data patterns [40]. This resulted in 5,047 (73.4%) completed surveys deemed to be from unique valid participants (see Figure 1).
Figure 1.
Flow diagram of participant recruitment in SILAS wave 4 (May–December 2011)
Participants were asked a variable number of items depending on responses and skip patterns (maximum of 123 questions). The mean survey completion time was 71 minutes, and participants who completed the survey were compensated with a $30 gift card. Participants could opt out of answering any question by clicking a “refuse to answer” option. A Certificate of Confidentiality was obtained from the National Institutes of Health. The institutional review board of the researchers’ home institution approved study procedures.
Measure
The survey consisted of sections about demographics; Internet use; sexual behaviors with partners from online, from bars/clubs and from other locations; rectal enema/douche use; current alcohol and drug use; sexuality and role in sex; long-term relationships (LTRs); openness as gay and bisexual men; mental health; internalized homonegativity; HIV and STI status; perception of the gay scene in the MSA; awareness of public policy in the MSA; and social climate toward gay people at work, in the family, neighborhood, MSA, and state levels. For this analysis, we grouped intrapersonal characteristics such as age, race/ethnicity, and income as personal variables; behavioral characteristics such as number of sexual partners, and unprotected anal intercourse as behavioral variables and residence in urban or rural MSA or in pro or anti-gay MSA as environmental variables. Measures relevant to this analysis are described below. HIV serostatus disclosure: In order to assess HIV serodisclosure, two questions were asked on the survey. The first was, “Thinking about the times you had protected anal sex (condom was used) in the past 3 months, how often did you tell your sex partner(s) your HIV status?” and the other was, “Thinking about the times you had unprotected anal sex (no condom used) in the past 3 months, how often did you tell your sex partner(s) your HIV status?”. The response options for both questions were “Never (0% of the time)”, “Rarely (1–24% of the time)”, “Sometimes (25–49% of the time)”, “Frequently (50–74% of the time)”, “Always or almost always (75–100% of the time)”, “Not applicable, I have not had sex in the last 3 months”, “Not applicable, I have not had sex with (or without, for UAI) a condom in the last 3 months”, and “Refuse to answer.” The answers were then coded into binary outcomes by setting any answer of “Never”, “Rarely”, “Sometimes”, and “Frequently” to “no” and “Always or almost always” as “yes.” The study participants who indicated either of the “Not applicable” answers or refused to answer the question were marked missing and were excluded from this analysis.
Sexual risk behavior: A sexual behavior battery investigated sexual risk behavior in the past three months with partners met online, at a gay bar/club, and at any other physical location(s). Data from both physical venues (“gay bar/clubs” and “other”) were combined at analysis. If participants indicated they engaged in anal sex in the past three months with a partner(s) met online or offline, they were asked to report the number of partner(s), and the number with whom they had unprotected (without condom) and protected (with condom) sex, estimated separately. Using these estimates, we created three summary variables; total number of partners (0 partner/1–2 partner/2+ partners) unprotected anal intercourse male partners (UAIMP: 0–2 partners/2+ partners) and protected anal intercourse male partners (PAIMP: 0 partner/1+ partners). Meeting Venue: Venue where participants met their sexual partners in the last three months was placed into three categories: “Online only”, “Offline only”, and “Both online and offline.” For online only, participants had to report at least one man met online and no men met offline. Conversely, participants were placed in the “offline only” group if they reported at least one man met offline and none met online. For men who reported meeting men both online and offline, they were placed in the both online and offline category.
Sexual orientation: Participants’ sexual identity was investigated by asking, “Do you identify as…” with response options being gay/homosexual, bisexual, heterosexual, or other (with a space to write in their response). They were also asked to report role-in-sex by identified themselves as top, top/versatile, versatile, bottom/ versatile, bottom, oral only, oral and jerking off, and jerking off only. At analysis, we categorized participants as no anal (either oral only, or oral and jerking off, or jerking off only), top only, top/versatile, versatile, bottom/ versatile, and bottom only; and treated it as continuous with higher score indicating risker role in sex. Other measures: Demographic variables included age, education, income, race/ethnicity, marital status to a man, long-term relationship status (90+ days), history of any sexually transmitted infections (STI) and HIV serostatus. “Openness,” defined in the survey as “I would say that I am open (out) as a gay, bisexual, or a man attracted to other men:” and was measured as a 5-point Likert-type item (1 = “not at all open (out)”, 5 = “open (out) to all or most people I know”). We used the shortened Center for Epidemiological Studies Depression (CES-D) 10 item scale [41] to measure depressive symptoms among participants. Cornbach’s alpha for CES-D scale in this sample was 0.85 (95% CI: 0.84–0.86). We used the revised Reaction to Homosexuality 7-item scale [42] to measure internalized homonegativity, which was treated as continuous. Alpha reliability for this scale with our sample was 0.76 (95% CI: 0.75–0.78). For all questions on SILAS, participants were given the choice of “Refuse to answer,” which was marked missing in subsequent analyses.
Statistical Analyses
Summary statistics were used to describe the study sample and to calculate the prevalence of HIV disclosure among the participants. A chi-square test was used to assess differences in serodisclosure across various demographic, behavioral and environmental factors (age, race, education, income, marital status, long term relationship status, HIV status, non-HIV STI status, number of sexual partners, UAIMP, PAIMP, sexual orientation, meeting venue); and MSA type (urban/rural) and MSA attitudes regarding homosexuality (pro/anti). A t-test was used to assess the relationship between internalized homonegativity and disclosure. These were conducted twice, once for the PAI and once for the UAI encounter.
To assess the relationship between meeting venue and HIV disclosure in UAI and PAI contexts, and the relative contribution of personal and behavioral factors as well as the block of factors on this relationship, we used a block regression strategy. Three separate multivariable (multiple) regression models were run to identify factors associated with HIV disclosure (0=did not disclose, 1=yes, did disclose). Personal characteristics that were significant (p≤0.05) at the bivariate level were entered into the first multivariable regression model. In the second multivariable regression model, we included behavioral variables that were significant (p≤0.05) at the bivariate level. Finally, in the third model we included all the variables that were significant (p≤0.05) in the first two regression models along with the meeting venue variable. We built a three-level (individual, rural/urban MSA, and pro/anti MSA) random-intercept random coefficient nested regression model using gllamm [43,44] in STATA. We calculated adjusted risk ratios and respective 95% confidence interval with a robust variance estimator correcting the standard errors. We used the likelihood ratio (LR) test to build the most parsimonious model. All statistical tests were two-tailed, and all analyses were conducted in STATA 11 software [45].
Results
Demographic, sexual, and behavioral characteristics
Personal and behavioral characteristics of the participants are presented in Table I. Of the 3,309 study participants, the majority identified themselves as White (72.6%) and gay/homosexual (90.6%). The mean age of the study participants was 33.8 years, and most indicated having a college degree (50.3%) and having an income of less than forty thousand in a year (57.4%). Over three-fourths of respondents (76.9%) reported that they used both online and offline venues to seek sexual partners, while 12.7% used exclusively offline venues and 10.4% used exclusively online venues. Reflecting the study design, most (76.4%) indicated that they resided in an urban MSA, and about half (54.5%) of the respondents evaluated their MSA as being tolerant towards homosexuality, while the other half evaluated their city as antagonistic or homonegative. Twelve percent of the respondents stated that they were HIV-positive and 12.3% reported that they had a (non-HIV) sexually transmitted infection in the past twelve months.
Table 1.
Personal and behavioral characteristics by HIV serostatus disclosure among SILAS participants (N=3,309)
| Variable | Total | HIV Disclosure before UAI (n=2358) | HIV disclosure before PAI (n=2593) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N=3309 (%) | No n=1150 (48.8%) |
Yes n=1208 (51.2%) |
χ2/t | p-value | No n=1329 (51.3%) |
Yes n=1246 (48.7%) |
χ2/t | p-value | |
| Meeting venue: | 16.16 | <0.001 | 8.70 | <0.05 | |||||
| Online-offline both | 2547 (76.9) | 887 (77.1) | 996 (82.5) | 1019 (76.7) | 1024 (81.0) | ||||
| Offline only | 419 (12.7) | 117 (10.2) | 118 (9.8) | 143 (10.8) | 123 (9.7) | ||||
| Online only | 343 (10.4) | 146 (12.7) | 94 (7.8) | 167 (12.5) | 117 (9.3) | ||||
| Personal: | |||||||||
| Age in years | 4.26 | <0.001 | 4.75 | <0.001 | |||||
| mean±SD | 32.80±12.31 | 31.18±11.05 | 33.34±12.09 | 31.04±11.38 | 33.35±12.22 | ||||
| Race/Ethnicity | 149.95 | <0.001 | 124.51 | <0.001 | |||||
| Non-Hispanic White | 2401 (72.6) | 659 (57.3) | 970 (80.3) | 797 (59.9) | 1006 (79.6) | ||||
| Non-Hispanic Black | 112 (3.4) | 71 (6.2) | 22 (1.8) | 78 (5.9) | 20 (1.6) | ||||
| Hispanic | 375 (11.3) | 191 (16.6) | 106 (8.8) | 208 (15.7) | 112 (8.9) | ||||
| Othera | 421 (12.7) | 229 (19.9) | 110 (9.1) | 246 (18.5) | 126 (9.9) | ||||
| Education | 3.63 | 0.06 | 0.46 | 0.49 | |||||
| Less than college degree | 1644 (49.7) | 547 (47.6) | 621 (51.5) | 642 (48.3) | 627 (49.6) | ||||
| College degree or greater | 1663 (50.3) | 603 (52.4) | 585 (48.5) | 687 (51.7) | 636 (50.4) | ||||
| Income | 47.92 | <0.001 | 35.63 | <0.001 | |||||
| Less than $19,999 | 1114 (34.6) | 339 (29.9) | 420 (36.7) | 425 (32.4) | 422 (34.4) | ||||
| $20,000 – $39,999 | 735 (22.8) | 216 (19.1) | 301 (25.6) | 250 (19.1) | 305 (24.9) | ||||
| $40,000 – $59,999 | 580 (18.0) | 225 (19.9) | 211 (17.9) | 251 (19.1) | 214 (17.5) | ||||
| $60,000 – $79,999 | 288 (8.9) | 115 (10.2) | 94 (7.9) | 125 (9.5) | 116 (9.5) | ||||
| $80,000 – $99,999 | 205 (6.4) | 104 (9.2) | 50 (4.2) | 116 (8.9) | 56 (4.6) | ||||
| More than $100,000 | 300 (9.3) | 134 (11.8) | 101 (8.6) | 144 (10.9) | 113 (9.2) | ||||
| Marital Status to a man | 113.36 | <0.001 | 97.04 | <0.001 | |||||
| Married or in a domestic or civil union | 250 (9.1) | 93 (11.5) | 113 (10.4) | 94 (9.6) | 97 (8.5) | ||||
| Never legally married | 2337 (84.8) | 586 (72.6) | 949 (87.1) | 759 (77.2) | 1012 (89.2) | ||||
| Separated, divorced, or widowed | 169 (6.1) | 129 (15.9) | 28 (2.6) | 130 (13.2) | 25 (2.2) | ||||
| In a long-term relationship | 1.45 | 0.23 | 0.004 | 0.95 | |||||
| No | 1947 (58.9) | 633 (55.1) | 635 (52.6) | 808 (60.8) | 767 (60.7) | ||||
| Yes | 1362 (41.2) | 517 (44.9) | 573 (47.4) | 521 (39.2) | 497 (39.3) | ||||
| Self-reported HIV status | 0.81 | 0.23 | 11.34 | <0.01 | |||||
| HIV-Negative | 2905 (88.0) | 967 (84.3) | 1031 (85.6) | 1130 (85.2) | 1131 (89.6) | ||||
| HIV-Positive | 396 (12.0) | 180 (15.7) | 173 (14.4) | 196 (14.8) | 131 (10.4) | ||||
| Self-reported non-HIV STI status | 86.44 | <0.001 | 75.75 | <0.001 | |||||
| Never | 2139 (62.8) | 763 (66.7) | 696 (57.7) | 870 (65.9) | 797 (63.1) | ||||
| Yes, in last 12 months | 405 (12.3) | 210 (18.4) | 143 (11.9) | 246 (18.6) | 125 (9.8) | ||||
| Yes, not in last 12 months | 755 (22.9) | 170 (14.9) | 367 (30.4) | 205 (15.5) | 342 (27.1) | ||||
| Self-reported identity | 4.74 | 0.03 | 12.98 | <0.001 | |||||
| Non-gay | 312 (9.4) | 81 (7.1) | 115 (9.5) | 102 (7.7) | 150 (11.9) | ||||
| Gay/Homosexual | 2995 (90.6) | 1068 (92.9) | 1092 (90.5) | 1226 (92.3) | 1113 (88.1) | ||||
| Openness | 389.09 | <0.001 | 321.68 | <0.001 | |||||
| Not Open | 81 (2.4) | 36 (3.1) | 21 (1.7) | 39 (2.9) | 32 (2.5) | ||||
| Open to few people | 346 (10.5) | 190 (16.5) | 77 (6.4) | 208 (15.7) | 91 (7.2) | ||||
| Open to half the people | 419 (12.7) | 302 (26.3) | 46 (3.8) | 319 (24.0) | 59 (4.7) | ||||
| Open to most people | 670 (20.3) | 218 (18.9) | 232 (19.2) | 265 (19.9) | 228 (18.0) | ||||
| Open to all or almost all people | 1791 (54.1) | 402 (35.0) | 832 (68.9) | 496 (37.4) | 854 (67.6) | ||||
| Internal Homonegativity (as continuous scale)b | 15.17 | <0.001 | 12.94 | <0.001 | |||||
| Mean ± SD | 2.22 ±1.04 | 2.54±1.03 | 1.92±0.95 | 2.51±1.05 | 1.99±0.99 | ||||
| Depressive symptoms (CESD 10) | 151.57 | <0.001 | 111.80 | <0.001 | |||||
| Absent (score < 10) | 1643 (49.6) | 397 (34.5) | 723 (59.9) | 494 (37.2) | 732 (57.9) | ||||
| Present(score ≥ 10) | 1666 (50.4) | 753 (65.5) | 485 (40.1) | 835 (62.8) | 532 (42.1) | ||||
| Behavioral: | |||||||||
| Self-reported role-in-sex | 84.23 | <0.001 | 78.46 | <0.01 | |||||
| No anal | 151 (4.6) | 80 (7.0) | 8 (0.7) | 83 (6.3) | 8 (0.6) | ||||
| Top only | 358 (10.9) | 123 (10.8) | 125 (10.4) | 139 (10.5) | 154 (12.2) | ||||
| Top/versatile | 660 (201) | 200 (17.5) | 264 (21.9) | 227 (17.2) | 290 (22.9) | ||||
| Versatile | 718 (21.9) | 202 (17.7) | 290 (24.1) | 262 (19.9) | 293 (23.2) | ||||
| Versatile /Bottom | 823 (25.1) | 296 (25.9) | 310 (25.7) | 345 (26.2) | 304 (24.1) | ||||
| Bottom only | 574 (17.5) | 239 (20.9) | 208 (17.3) | 262 (19.9) | 213 (16.9) | ||||
| Total sex partners, last 90 days | 80.04 | <0.001 | 58.59 | <0.001 | |||||
| 1–2 partners | 1270 (38.4) | 266 (23.1) | 487 (40.3) | 321 (24.1) | 481 (38.1) | ||||
| 2+ partners | 2037 (61.6) | 884 (76.9) | 721 (59.7) | 1008 (75.9) | 783 (61.9) | ||||
| UAIMPc, last 90 days | 222.45 | <0.001 | 244.48 | <0.001 | |||||
| 0–2 partners | 1930 (69.3) | 499 (45.8) | 858 (76.7) | 684 (54.6) | 984 (84.0) | ||||
| 2+ partners | 857 (30.7) | 591 (54.2) | 261 (23.3) | 569 (45.4) | 187 (16.0) | ||||
| PAIMPd, last 90 days | 21.36 | <0.001 | 1.22 | 0.27 | |||||
| 0 PAI partner | 746 (36.9) | 302 (27.9) | 415 (37.1) | 223 (17.9) | 229 (19.6) | ||||
| 1+ PAI partner | 2032 (73.1) | 781 (72.1) | 703 (62.9) | 1025 (82.1) | 938 (80.4) | ||||
| Environmental: | |||||||||
| MSA Strata | 2.27 | 0.13 | 0.41 | 0.52 | |||||
| Pro-gay city | 1788 (54.5) | 599 (52.7) | 670 (55.8) | 730 (55.4) | 681 (54.2) | ||||
| Anti-gay city | 1493 (45.5) | 538 (47.3) | 531 (44.2) | 587 (44.6) | 576 (45.8) | ||||
| Residence in | 25.22 | <0.001 | 17.53 | <0.001 | |||||
| Rural MSA | 774 (23.6) | 415 (27.6) | 322 (20.1) | 368 (27.9) | 262 (20.8) | ||||
| Urban MSA | 2507 (76.4) | 1086 (72.4) | 1279 (79.9) | 949 (72.1) | 995 (79.2) | ||||
Note: UAI: Unprotected Anal Intercourse; PAI: Protected Anal Intercourse
Other includes American Indian, Asian, Pacific Islanders and multi-racial
Higher score indicates higher internalized homonegativity
Number of male partners who engaged in unprotected anal intercourse, last 90 days
Number of male partners who had sex involving protected anal intercourse, last 90 days
HIV disclosure in UAI and PAI context
The primary dependent variables in this study were HIV serodisclosure before UAI and PAI context. During UAI context, 51.2% of the participants reported serodisclosing before UAI, whereas in the PAI context, 48.7% reported serodisclosing before PAI. Among those who serodisclosed prior to UAI, most (82.5%) met their partners using a combination of offline and online venues, 7.8% of participants met their partners exclusively online, and 9.8% exclusively offline. For PAI, 81% met using both, 9.3% using online and 9.7% using offline venue.
To identify potential demographic and behavior correlates of serodisclosure, we examined which characteristics were statistically significant in both UAI and PAI disclosure situations (see Table I). Age, race/ethnicity, income, marital status to a man, sexual identity, openness, internalized homonegativity, depressive symptoms, and non-HIV STI status were significantly associated (p≤0.05) with those who serodisclosed all or almost all the time prior to UAI and PAI. HIV status was not associated with serodisclosure in UAI, however HIV-negative men were more likely to serodisclose before PAI. For the behavioral variables, identifying as a versatile, having more partners, and a recent history of UAI were associated with HIV serodisclosure before both UAI and PAI.
Correlates of HIV disclosure in UAI context
Table II shows the results of both univariate and multivariable regressions, with serostatus disclosure as the outcome variable in UAI and PAI situations. In the final model controlling for other variables, meeting environment was associated with HIV disclosure before UAI. Participants were significantly less likely to report serodisclosing before UAI if they met their partners either exclusively offline (RR=0.78, 95% CI: 0.71–0.86, p<0.001) or exclusively online (RR=0.70, 95% CI: 0.66–0.73; p<0.001) compared to participants who met their sexual partners in both environments. Gay identified participants (RR=0.84, 95% CI: 0.81–0.87; p<0.001) and those who were separated/ widowed/divorced (RR=0.57, 95% CI: 0.42–0.78; p<0.001) were less likely of serodisclosing before UAI than their counterparts. Participants who reported being more out as gay (RR=1.15, 95% CI: 1.13–1.16; p<0.001) were more likely of disclosing before UAI. Participants with more depressive symptoms (RR=0.86, 95% CI: 0.85–0.86; p<0.001) and with more than two unprotected anal intercourse male partners (RR=0.85, 95% CI: 0.84–0.85; p<0.001) were less likely of serodisclosing their HIV status than other participants.
Table 2.
Bivariate and multivariable regression analysis of HIV serodisclosure in UAI and PAI encounters among SILAS participants
| Variable | UAI Disclosure (n=2358) | PAI Disclosure (n=2593) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Final Model c |
Model 1d | Model 2e | Final Model f |
|||||
| Crude RR (95% CI) |
Adj. RR (95% CI) |
Adj. RR (95% CI) |
Adj. RR (95% CI) |
p-value | Crude RR (95% CI) |
Adj. RR (95% CI) |
Adj. RR (95% CI) |
Adj. RR (95% CI) |
p-value | |
| Meeting venue: | ||||||||||
| Online- offline both |
Ref. | Ref. | Ref. | Ref. | ||||||
| Offline only |
1.02 (0.90–1.15) |
0.78*** (0.71–0.86) |
<0.001 | 0.95 (0.90–1.01) |
0.79*** (0.78–0.80) |
<0.001 | ||||
| Online only | 0.73*** (0.71–0.74) |
0.70*** (0.66–0.73) |
<0.001 | 0.81** (0.76–0.85) |
0.77*** (0.74–0.80) |
<0.001 | ||||
| Personal: | ||||||||||
| Age | 1.01*** (1.00–1.01) |
1.00 (0.99–1.01) |
1.01*** (1.00–1.01) |
1.01*** (1.00–1.01) |
1.00 (0.99–1.01) |
0.56 | ||||
| Race/Ethnicity | ||||||||||
| N-H White | Ref. | Ref. | Ref. | Ref. | Ref. | |||||
| N-H Black | 0.40** (0.23–0.71) |
1.01 (0.82–1.24) |
0.37*** (0.27–0.51) |
0.88** (0.81–0.95) |
0.90*** (0.86–0.93) |
<0.001 | ||||
| Hispanic | 0.60 (0.27–1.33) |
1.04 (0.66–1.65) |
0.64 (0.41–1.01) |
1.07 (0.85–1.33) |
1.02 (0.76–1.38) |
0.88 | ||||
| Other f | 0.55*** (0.43–0.72) |
0.87 (0.55–1.37) |
0.62*** (0.60–0.63) |
0.96 (0.85–1.08) |
0.91 (0.82–1.01) |
0.07 | ||||
| Income | 0.92*** (0.88–0.95) |
0.95** (0.92–0.98) |
0.98 (0.93–1.03) |
0.49 | 0.96 (0.92–1.01) |
|||||
| Marital Status to a man | ||||||||||
| Married | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||
| Never married | 1.13*** (1.09–1.16) |
0.98 (0.90–1.07) |
1.05* (1.01–1.11) |
0.02 | 1.11*** (1.08–1.14) |
0.96* (0.93–0.99) |
0.99 (0.94–1.04) |
0.64 | ||
| Separated, divorced or widowed | 0.34*** (0.30–0.39) |
0.77* (0.62–0.94) |
0.57*** (0.42–0.78) |
<0.001 | 0.32*** (0.29–0.36) |
0.75*** (0.70–0.80) |
0.79** (0.67–0.93) |
0.005 | ||
| Self-reported HIV status | ||||||||||
| HIV- Negative |
Ref. | |||||||||
| HIV- Positive |
0.80 (0.53–1.20) |
|||||||||
| Self-reported non-HIV STI | ||||||||||
| Never | Ref. | Ref. | Ref. | Ref. | ||||||
| Yes, in last 12 months |
0.86 (0.55–1.33) |
1.11 (0.95–1.28) |
0.71 (0.43–1.15) |
0.91 (0.76–1.09) |
||||||
| Yes, not in last 12 months |
1.38*** (1.19–1.61) |
1.14 (0.99–1.33) |
1.28*** (1.23–1.34) |
1.06 (0.94–1.19) |
||||||
| Self-reported identity | ||||||||||
| Non-gay | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||
| Gay/Homo sexual |
0.83** (0.74–0.94) |
0.84*** (0.81–0.87) |
0.84*** (0.81–0.87) |
<0.001 | 0.79** (0.67–0.92) |
0.77*** (0.76–0.79) |
0.79*** (0.75–0.84) |
<0.001 | ||
| Openness g | 1.49*** (1.48–1.50) |
1.10*** (1.05–1.16) |
1.15*** (1.13–1.16) |
<0.001 | 1.42*** (1.40–1.44) |
1.12*** (1.09–1.16) |
1.10*** (1.07–1.12) |
<0.001 | ||
| IH h | 0.71*** (0.69–0.73) |
0.96 (0.90–1.01) |
0.74*** (0.71–0.76) |
0.94* (0.88–0.99) |
0.92** (0.87–0.98) |
0.007 | ||||
| Depressive symptoms (CES-D 10) |
||||||||||
| Absent (score <10) |
Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||
| Present (score ≥ 10) |
0.62*** (0.61–0.63) |
0.87*** (0.86–0.87) |
0.86*** (0.85–0.86) |
<0.001 | 0.66*** (0.63–0.68) |
0.92*** (0.90–0.95) |
0.95*** (0.92–0.97) |
<0.001 | ||
| Behavioral: | ||||||||||
| Self- reported role-in-sexi |
1.02** (1.01–1.03) |
1.01 (0.99–1.03) |
1.00 (0.99–1.01) |
|||||||
| UAIMP j, last 90 days | ||||||||||
| 0–2 partners | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||
| 2+ partners | 0.49*** (0.28–0.50) |
0.50*** (0.49–0.51) |
0.85*** (0.84–0.85) |
<0.001 | 0.42*** (0.41–0.44) |
0.43*** (0.42–0.44) |
0.83*** (0.79–0.87) |
<0.001 | ||
| PAIMP k, last 90 days | ||||||||||
| 0 PAI partner |
Ref. | Ref. | Ref. | |||||||
| 1+ PAI partner |
0.83* (0.69–1.00) |
0.95 (0.80–1.12) |
0.97 (0.93–1.01) |
|||||||
p≤0.05;
p≤0.01;
p≤0.001
Note: RR: Relative Risk; Adj. RR: Adjusted Relative Risk; N-H: Non-Hispanic; IH: Internal Homonegativity; UAI: Unprotected Anal Intercourse; PAI: Protected Anal Intercourse
Adjusted for age, race/ethnicity, income, marital status,, non-HIV STI status, sexual identity, openness, internalized homonegativity and depressive symptoms
Adjusted for self-reported role in sex, number of unprotected anal intercourse male partner and number of protected anal intercourse male partner
Adjusted for meeting venue, income marital status, sexual identity, openness, internalized homonegativity depressive symptoms and number of unprotected anal intercourse male partner; variances of random effects-level 2 (SE)=0.001 (0.001) and level 3 (SE)=0.003 (0.002)
Adjusted for age, race/ethnicity, marital status, non-HIV STI status, sexual identity, openness, internalized homonegativity and depressive symptoms
Adjusted for meeting venue, age, race/ethnicity, marital status, sexual identity, openness, internalized homonegativity, depressive symptoms and number of unprotected anal intercourse male partner; variances of random effects-level 2 (SE)=0.001 (0.001) and level 3 (SE)=0.001 (0.001)
Other includes American Indian, Asian, Pacific Islanders and multi-racial
Higher score indicates more open as gay
Higher score indicates higher internalized homonegativity
Higher score indicates riskier role in sex
Number of male partners who engaged in unprotected anal intercourse, last 90 days
Number of male partners who had sex involving protected anal intercourse, last 90 days
Correlates of HIV disclosure in PAI context
As for HIV serodisclosure before PAI, meeting environment was associated with HIV disclosure. Participants meeting their partners exclusively offline (RR=0.79, 95% CI: 0.78–0.80; p<0.001) or exclusively online (RR=0.77, 95% CI: 0.74–0.80; p<0.001) were less likely to HIV serodisclose compared to participants who met their sexual partners both online and offline. Non-Hispanic Black participants (RR=0.90, 95% CI: 0.86–0.93; p<0.001); gay identified participants (RR=0.79, 95% CI: 0.75–0.84; p<0.001) and those who were separated/ widowed/divorced (RR=0.79, 95% CI: 0.67–0.93; p=0.005) were less likely to serodosclose than their counterparts. Participants who reported being more out as gay (RR=1.10, 95% CI: 1.07–1.12; p<0.001) were more likely of HIV disclosing before PAI whereas participants with higher internalized homonegativity (RR=0.92, 95% CI: 0.87–0.98; p=0.007); more depressive symptoms (RR=0.95, 95% CI: 0.92–0.97; p<0.001) and with more than two unprotected anal intercourse male partners (RR=0.83, 95% CI: 0.79–0.87; p<0.001) were less likely to serodisclose in the PAI context.
Discussion
The primary purpose of this analysis was to compare HIV serodisclosure across three separate types of environments for meeting sexual partners – online only, offline only, and both online/offline. A secondary purpose was to identify demographic and behavioral variables that might affect disclosure of HIV status. Because HIV serodisclosure can reasonably be expected to differ before UAI and PAI, each was investigated separately. For both UAI and PAI, HIV disclosure varied by meeting environment. More than three-fourths of the sample reported meeting men for sex (last 90 days) using both online and offline methods, versus 12.7% who used offline only and 10.4% who used online only. Thus, the key finding of this study is that the MSM who meet their sexual partners exclusively either offline or online were about 20~30% less likely to report disclosing their HIV status prior to sex than men who met their partners both online-offline (after controlling for all other variables). Our findings contradict with other studies [13,23,25,26] which found that MSM who meet their sexual partners online are more likely to disclose their serostatus than men who meet their partners offline. However, this analysis is the first, to our knowledge, to show that MSM who use a combination of environments to meet sexual partners are more likely to serodisclose than MSM who use only one environment. There are at least two possible interpretations of this key finding. First, men who seek partners “bi-environmentally” versus “mono-environmentally” may be analogous to linguistic students (bilingual versus monolingual), race/ethnicity (biracial versus monoracial), sexuality (bisexual versus monosexual) and travelers (bicultural versus monocultural). In each case, exposure to more than one language, race, sexuality, culture or other life dimension provides a potential strength that builds perspective and insight. Etymologically-speaking the comparison of “sophisticated” (from sophizesthai meaning “to become wise, learned or clever”) versus “inexperienced” (meaning lacking experiment, proof or experience) may best describe the benefit from seeking partners bi-environmentally versus mono-environmentally. Because HIV disclosure is expressed very differently in the two environments, those who navigate both environments are likely to learn multiple skills and ways to serodisclose versus those who seek partners in only one environment. Future research could test this hypothesis by examining HIV serodisclosure self-efficacy between those seeking partners bi-environmentally versus mono-environmentally. Our results lead us to hypothesize that HIV serodisclosure self-efficacy will be greater in MSM seeking partners bi-environmentally versus mono-environmentally. A second possible interpretation is that this finding is a statistical artifact. Because so many more MSM report findings partners bi-environmentally, they represent the norm, relegating uni-environmental partner seekers as statistical outliers. Our findings also suggest a potential bias in prior studies. Because most MSM use both environments to meet partners, our own and others’ prior analyses that compared any online sex-seeking with exclusively offline sex seeking were in fact comparing men who use only mono-environments We recommend future researchers employ the trichotic (offline only, online only, and both online-offline) comparison to avoid this bias.
Using Bandura’s typology, personal characteristics associated with non-disclosure in both UAI and PAI context include being previously married, self-identified gay/homosexual, being depressed, and being less open as gay/homosexual. In addition, Black MSM (vs. White MSM), and MSM who expressed more internalized homonegativity were each significantly less likely to disclose their HIV serostatus to sexual partners before PAI. Consistent with other studies [6,7], race/ethnicity remained a factor to consider in disclosure, with all racial/ethnic minorities less likely to disclose than White MSM. Carballo-Dieguez et al., [13] attributes this finding to cultural factors. For example, Harawa et al., [46] in their study of HIV positive African American MSM state that serodisclosure is influenced by the fear of exclusion. They also noted, “HIV prevention among non-gay identified African American men is complicated by issues of secrecy, racism, and a lack of identification with gay communities and norms” (p. 683). In the Positive Connections study of 675 HIV positive MSM, Rosser et al. [11] reported that participants who were most out as gay were also more likely to serodisclose before sex. Similarly, in our current sample, openness as gay/homosexual was associated with HIV serodisclosure before PAI as well as UAI. However, our findings also contradict several previous findings. Contrary to Eustace & Ilagan’s [12] findings, MSM who do not identify as gay in this study remained more likely to disclose their HIV serostatus (after controlling for other variables). As the two key differences between the prior studies and this study are: 1) in this study we controlled for online-offline environment, and 2) this study was conducted in the era of web 2.0 and smart technology, we speculate that individual differences around gay identification are being erased by technology which makes it easier to serodisclose online. Most study participants (88.0%) identified their HIV status as HIV negative and most (62.8%) have never been diagnosed with a non-HIV STI. In contrast to previous studies which report a relationship [5,13,14], in our study HIV serostatus was not associated with HIV disclosure either before UAI or PAI.
More than sixty percent of the participants reported having more than two sexual partners in the last ninety days with nearly one-third reporting UAI with at least two male partners. Among participants with more than two partners, 45% (721/1605) disclosed their serostatus before UAI and 44% (783/1791) before PAI. However, among participants who reported more than two UAI male sexual partners in last ninety days, only 31% (261/852) and 25% (187/756) disclosed in UAI setting and in PAI setting respectively. In multivariable analysis, participants with multiple unprotected anal male sexual partners in last ninety days (2+ vs. 0–2 partners) were less likely of serodisclosing in both settings.
A strength of this analysis is that serostatus disclosure both before PAI and before UAI were assessed separately, allowing us to identify what factors may be common to HIV serodisclosure, and what factors may be specific to using or not using protection. Interestingly, in the final model, while disclosure before PAI and UAI had six variables in common, our analysis identified two additional variables which were significant only in disclosure before PAI. This supports our a priori assumption that HIV serodisclosure before UAI and PAI should be investigated separately. It also suggests that serodisclosure is a complex, sophisticated process.
There are four principal limitations in this study. First, this is a cross-sectional study and, as such, causality cannot be assumed. Second, all the data are retrospective self-report for the last ninety days. Because of the socially-sensitive nature of the topic, we caution that rates are likely underestimates or possibly overly-optimistic assessments of the true incidence of serodisclosure. Third, this sample was a convenience sample recruited online from 16 MSAs and their surrounding areas. Hence, the generalizability of findings is not known. Fourth, we don’t actually know where and when the person sero-disclosed. Particularly for those who met online, the participant may have concluded he disclosed because he put something in his profile online (and assumed the partner read it), serodisclosed while organizing a meeting by email or phone, and/or serodisclosed in person prior to, during or after sex. We recommend future studies use event level investigations to explore this further.
This study has some interesting implications for HIV prevention practice. Should our “bi-environmental hypothesis” prove accurate, then HIV prevention counsellors could assess for mono-environmental sex seeking MSM, and where an association with risk is observed, engage in serodisclosure skills building across both environments. For example, those having challenges serodisclosing in offline environments could go through the exercise of setting up an online profile including the field of HIV status; while those who non-disclose in online environments could practice disclosing in person. Both can build skills by being exposed to the multiple different ways that serodisclosure occurs in both environments. Second, consistent with our findings, health professionals working with MSM should explicitly ask about serodisclosure across both environments as they may differ. Third, the assumptions that MSM who are out, gay-identified, and of higher SES are more sexually healthy (and especially have less internalized homonegativity and symptoms of depression) were not supported by this study. While this study could be an anomaly, we speculate that the lack of HIV prevention and decreasing services focused on gay-identified MSM for over a decade, increasing social acceptance of homosexuality, and pressure on same-sex attracted MSM to identify as gay, may be changing a long-established relationship between coming out, gay identity, and sexual health. If so, health professionals should be cautioned not to assume that a “gay identity” equates with self-acceptance and lower internalized homonegativity. These findings support the recent Institute of Medicine’s finding that more research is needed to address the chronic health disparities faced by gay/bisexual/MSM, and a new generation of MSM health programming, which addresses the reality of gay-identified MSM’s sexual and mental health challenges in the 21st century, will likely be needed.
The dynamics of sexual risk taking, disclosure, and safer sex negotiation among MSM are complex, intertwined in individual, behavioral and environmental level factors. While HIV prevention for MSM has focused on individual and behavioral risk factors, this study highlights the importance also of considering the environment. While previous studies have focused on the Internet as a risk environment, our findings suggest bi-environmental partner seeking may also have beneficial effects.
Acknowledgments
This study was undertaken as part of the “Structural Interventions to Lower Alcohol-Related STI/HIV Risk,” Grant number R01AA01627001, funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
References
- 1.Centers for Disease Control and Prevention (CDC) HIV Surveillance Report, 2011. [Accessed Jun 10, 2013];2013 Vol.23 http://www.cdc.gov/hiv/topics/surveillance/resources/reports/.Published February 2013. [Google Scholar]
- 2.Simoni JM, Pantalone DW. Secrets and safety in the age of AIDS: does HIV disclosure lead to safer sex? Top HIV Med. 2004 Oct-Nov;12(4):109–118. [PubMed] [Google Scholar]
- 3.Horvath KJ, Nygaard K, Rosser BRS. Ascertaining partner HIV status and its association with sexual risk behavior among internet-using men who have sex with men. AIDS Behav. 2010 Dec;14(6):1376–1383. doi: 10.1007/s10461-009-9633-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xia Q, Molitor F, Osmond DH, Tholandi M, Pollack LM, Ruiz JD, et al. Knowledge of sexual partner's HIV serostatus and serosorting practices in a California population-based sample of men who have sex with men. AIDS. 2006 Oct 24;20(16):2081–2089. doi: 10.1097/01.aids.0000247566.57762.b2. [DOI] [PubMed] [Google Scholar]
- 5.Parsons JT, Schrimshaw EW, Bimbi DS, Wolitski RJ, Gomez CA, Halkitis PN. Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. AIDS. 2005 Apr;19(Suppl 1):S87–S97. doi: 10.1097/01.aids.0000167355.87041.63. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan KM. Male self-disclosure of HIV-positive serostatus to sex partners: a review of the literature. J Assoc Nurses AIDS Care. 2005 Nov-Dec;16(6):33–47. doi: 10.1016/j.jana.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Rice E, Comulada S, Green S, Arnold EM, Rotheram-Borus MJ. Differential disclosure across social network ties among women living with HIV. AIDS Behav. 2009 Dec;13(6):1253–1261. doi: 10.1007/s10461-009-9554-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Batterham P, Rice E, Rotheram-Borus MJ. Predictors of serostatus disclosure to partners among young people living with HIV in the pre- and post-HAART eras. AIDS Behav. 2005 Sep;9(3):281–287. doi: 10.1007/s10461-005-9002-5. [DOI] [PubMed] [Google Scholar]
- 9.Rutledge SE. Enacting personal HIV disclosure policies for sexual situations: HIV-positive gay men's experiences. Qual Health Res. 2007 Oct;17(8):1040–1059. doi: 10.1177/1049732307306931. [DOI] [PubMed] [Google Scholar]
- 10.Mutchler MG, Bogart LM, Elliott MN, McKay T, Suttorp MJ, Schuster MA. Psychosocial correlates of unprotected sex without disclosure of HIV-positivity among African-American, Latino, and White men who have sex with men and women. Arch Sex Behav. 2008 Oct;37(5):736–747. doi: 10.1007/s10508-008-9363-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosser BRS, Horvath KJ, Hatfield LA, Peterson JL, Jacoby S, Stately A, et al. Predictors of HIV disclosure to secondary partners and sexual risk behavior among a high-risk sample of HIV-positive MSM: results from six epicenters in the US. AIDS Care. 2008 Sep;20(8):925–930. doi: 10.1080/09540120701767265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eustace RW, Ilagan PR. HIV disclosure among HIV positive individuals: a concept analysis. J Adv Nurs. 2010 Sep;66(9):2094–2103. doi: 10.1111/j.1365-2648.2010.05354.x. [DOI] [PubMed] [Google Scholar]
- 13.Carballo-Dieguez A, Miner M, Dolezal C, Rosser BRS, Jacoby S. Sexual negotiation, HIV-status disclosure, and sexual risk behavior among Latino men who use the internet to seek sex with other men. Arch Sex Behav. 2006 Aug;35(4):473–481. doi: 10.1007/s10508-006-9078-7. [DOI] [PubMed] [Google Scholar]
- 14.Eaton LA, Kalichman SC, O'Connell DA, Karchner WD. A strategy for selecting sexual partners believed to pose little/no risks for HIV: serosorting and its implications for HIV transmission. AIDS Care. 2009 Oct;21(10):1279–1288. doi: 10.1080/09540120902803208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pollock JA, Halkitis PN. Environmental factors in relation to unprotected sexual behavior among gay, bisexual, and other MSM. AIDS Educ Prev. 2009 Aug;21(4):340–355. doi: 10.1521/aeap.2009.21.4.340. [DOI] [PubMed] [Google Scholar]
- 16.Grov C, Rendina HJ, Ventuneac A, Parsons JT. HIV Risk in Group Sexual Encounters: An Event-Level Analysis from a National Online Survey of MSM in the U.S. J Sex Med. 2013 Sep;10(9):2285–2294. doi: 10.1111/jsm.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paxton S. The paradox of public HIV disclosure. AIDS Care. 2002 Aug;14(4):559–567. doi: 10.1080/09540120208629674. [DOI] [PubMed] [Google Scholar]
- 18.Gorbach PM, Galea JT, Amani B, Shin A, Celum C, Kerndt P, et al. Don't ask, don't tell: patterns of HIV disclosure among HIV positive men who have sex with men with recent STI practising high risk behaviour in Los Angeles and Seattle. Sex Transm Infect. 2004 Dec;80(6):512–517. doi: 10.1136/sti.2004.010918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grov C, Parsons JT, Bimbi DS. Sexual risk behavior and venues for meeting sex partners: an intercept survey of gay and bisexual men in LA and NYC. AIDS Behav. 2007 Nov;11(6):915–926. doi: 10.1007/s10461-006-9199-y. [DOI] [PubMed] [Google Scholar]
- 20.Grov C, DeBusk JA, Bimbi DS, Golub SA, Nanin JE, Parsons JT. Barebacking, the Internet, and harm reduction: an intercept survey with gay and bisexual men in Los Angeles and New York City. AIDS Behav. 2007 Jul;11(4):527–536. doi: 10.1007/s10461-007-9234-7. [DOI] [PubMed] [Google Scholar]
- 21.Parsons JT, Schrimshaw EW, Wolitski RJ, Halkitis PN, Purcell DW, Hoff CC, et al. Sexual harm reduction practices of HIV-seropositive gay and bisexual men: serosorting, strategic positioning, and withdrawal before ejaculation. AIDS. 2005 Apr;19(Suppl 1):S13–S25. doi: 10.1097/01.aids.0000167348.15750.9a. [DOI] [PubMed] [Google Scholar]
- 22.Horvath KJ, Weinmeyer R, Rosser BRS. Should it be illegal for HIV-positive persons to have unprotected sex without disclosure? An examination of attitudes among US men who have sex with men and the impact of state law. AIDS Care. 2010 Oct;22(10):1221–1228. doi: 10.1080/09540121003668078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grov C, Hirshfield S, Remien RH, Humberstone M, Chiasson MA. Exploring the venue's role in risky sexual behavior among gay and bisexual men: an event-level analysis from a national online survey in the U.S. Arch Sex Behav. 2013 Feb;42(2):291–302. doi: 10.1007/s10508-011-9854-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horvath KJ, Bowen AM, Williams ML. Virtual and physical venues as contexts for HIV risk among rural men who have sex with men. Health Psychol. 2006;25(2):237–242. doi: 10.1037/0278-6133.25.2.237. [DOI] [PubMed] [Google Scholar]
- 25.Horvath KJ, Oakes JM, Rosser BRS. Sexual negotiation and HIV serodisclosure among men who have sex with men with their online and offline partners. J Urban Health. 2008 Sep;85(5):744–758. doi: 10.1007/s11524-008-9299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. J Acquir Immune Defic Syndr. 2007 Feb 1;44(2):235–243. doi: 10.1097/QAI.0b013e31802e298c. [DOI] [PubMed] [Google Scholar]
- 27.Tikkanen R, Ross MW. Technological tearoom trade: characteristics of Swedish men visiting gay Internet chat rooms. AIDS Educ Prev. 2003 Apr;15(2):122–132. doi: 10.1521/aeap.15.3.122.23833. [DOI] [PubMed] [Google Scholar]
- 28.Bolding G, Davis M, Hart G, Sherr L, Elford J. Where young MSM meet their first sexual partner: the role of the Internet. AIDS Behav. 2007 Jul;11(4):522–526. doi: 10.1007/s10461-007-9224-9. [DOI] [PubMed] [Google Scholar]
- 29.Horvath KJ, Weinmeyer R, Rosser BRS. Should it be illegal for HIV-positive persons to have unprotected sex without disclosure? An examination of attitudes among US men who have sex with men and the impact of state law. AIDS Care. 2010 Oct;22(10):1221–1228. doi: 10.1080/09540121003668078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ross MW, Rosser BRS, Coleman E, Mazin R. Misrepresentation on the Internet and in real life about sex and HIV: A study of Latino men who have sex with men. Cult Health Sex. 2006 Mar-Apr;8(2):133–144. doi: 10.1080/13691050500485604. [DOI] [PubMed] [Google Scholar]
- 31.Mustanski BS. Are sexual partners met online associated with HIV/STI risk behaviours? Retrospective and daily diary data in conflict. AIDS Care. 2007 Jul;19(6):822–827. doi: 10.1080/09540120701237244. [DOI] [PubMed] [Google Scholar]
- 32.Ostergren JE, Rosser BRS, Horvath KJ. Reasons for non-use of condoms among men who have sex with men: a comparison of receptive and insertive role in sex and online and offline meeting venue. Cult Health Sex. 2011 Feb;13(2):123–140. doi: 10.1080/13691058.2010.520168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grov C, Crow T. Attitudes about and HIV risk related to the "most common place" MSM meet their sex partners: comparing men from bathhouses, bars/clubs, and Craigslist.org. AIDS Educ Prev. 2012 Apr;24(2):102–116. doi: 10.1521/aeap.2012.24.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Leary A, Horvath KJ, Rosser BRS. Associations between partner-venue specific personal responsibility beliefs and transmission risk behavior by HIV-positive men who have sex with men (MSM) AIDS Behav. 2013 Jun;17(5):1855–1861. doi: 10.1007/s10461-012-0291-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 36.Office of Management and Budget. Standards for defining metropolitan and micropolitan statistical areas. Federal Register. 2000;65(249):82228–82238. [Google Scholar]
- 37.Jones-Webb R, Smolenski D, Brady S, Wilkerson M, Rosser BRS. Drinking settings, alcohol consumption, and sexual risk behavior among gay men. Addict Behav. 2013 Mar;38(3):1824–1830. doi: 10.1016/j.addbeh.2012.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Konstan JA, Rosser BRS, Ross MW, Stanton J, Edwards WM. The story of Subject Naught: A cautionary but optimistic tale of Internet survey research. J Comput Mediat Commun. 2005;10(2) [Google Scholar]
- 39.Rosser BRS, Miner M, Bockting W, Ross MW, Konstan J, Gurak L, et al. HIV Risk and the Internet: Results of the Men's INTernet Sex (MINTS) Study. AIDS Behav. 2009 Aug;13(4):746–756. doi: 10.1007/s10461-008-9399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pequegnat W, Rosser BRS, Bowen A, Bull S, DiClemente R, Bockting W, et al. Conducting Internet-Based HIV/STD Prevention Survey Research: Considerations in Design and Evaluation. AIDS Behav. 2007 Jul;11(4):505–521. doi: 10.1007/s10461-006-9172-9. [DOI] [PubMed] [Google Scholar]
- 41.Zhang W, O'Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, et al. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012 Jul;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smolenski DJ, Diamond PM, Ross MW, Rosser BRS. Revision, criterion validity, and multigroup assessment of the Reactions to Homosexuality scale. J Pers Assess. 2010 Nov;92(6):568–576. doi: 10.1080/00223891.2010.513300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rabe-Hesketh S, Skrondal A, Pickles A. Maximum likelihood estimation of limited and discrete dependent variable models with nested random effects. J Econ. 2005 Oct;128(2):301–323. [Google Scholar]
- 44.Rabe-Hesketh S, Skrondal A, Pickles A. Generalized multilevel structural equation modeling. Psychometrika. 2004 Jun;69(2):167–190. [Google Scholar]
- 45.StataCorp. Stata Statistical Software: Release 11. 2010; 11.0 [Google Scholar]
- 46.Harawa NT, Williams JK, Ramamurthi HC, Bingham TA. Perceptions towards condom use, sexual activity, and HIV disclosure among HIV-positive African American men who have sex with men: implications for heterosexual transmission. J Urban Health. 2006 Jul;83(4):682–694. doi: 10.1007/s11524-006-9067-0. [DOI] [PMC free article] [PubMed] [Google Scholar]