Abstract
Objectives
The purpose of this study was to quantify within The National Dental Practice-Based Research Network current utilization of dental hygienists and assistants with expanded functions and quantify network dentists’ attitudes toward a new non-dentist provider model - the dental therapist.
Methods
Dental practice-based research network practitioner-investigators participated in a single, cross-sectional administration of a questionnaire.
Results
Current non-dentist providers are not being utilized by network practitioner-investigators to the fullest extent allowed by law. Minnesota practitioners, practitioners in large group practices, and those with prior experience with expanded function non-dentist providers delegate at a higher rate and had more-positive perceptions of the new dental therapist model.
Conclusions
Expanding scopes of practice for dental hygienists and assistants has not translated to the maximal delegation allowed by law among network practices. This finding may provide insight into dentists’ acceptance of newer non-dentist provider models.
Keywords: dental practice patterns, dental auxiliaries, delivery of dental care, dental group practices
INTRODUCTION
The Surgeon General’s report, Oral Health in America, documented the lack of access to oral health care by many Americans (1). The report identified many barriers to adequate access to care, including inadequacy in the number of dentists and/or their distribution (1). This led some to advocate for diversifying the types of providers (e.g., dental therapists, community dental health coordinators) or expanding the scopes of existing non-dentist providers (dental assistants, dental hygienists) as a solution (2). Expanding the scope of practice for dental auxiliaries is not new; expansion emerged in the 1960’s in an effort to increase dental access (3).
Since the 1970’s, states have continued to expand allied scopes of practice via their respective dental practice acts. Whether these changes in law resulted in an actual change in the utilization of non-dentist providers has not been widely studied, and our review of the literature revealed that most of our knowledge about allied dental provider utilization is decades old. Given the current debate over new non-dentist provider models, it should be helpful first to understand the current utilization of allied dental providers within dental practice, as this information could provide insight into the potential acceptance or rejection of the newest non-dentist provider – the dental therapist.
Dental therapy is relatively new to the United States. However, dental therapists have played a critical role in delivering dental care in fifty-four countries (4). Studies in the United Kingdom have shown that dental therapists can play an important role in delivery of care in a dental practice and that their role may vary according to the composition of the dental team in a practice (5, 6). The first dental therapy program in the United States, the Dental Health Aide Therapist (DHAT), was created in Alaska in 2003 by the Alaska Native Tribal Health Consortium. Dental therapists in Alaska are deployed for Native American populations under federal jurisdiction and are delivering quality dental care within their scope of training (7). In 2009, the Minnesota legislature, signed into law groundbreaking legislation authorizing two new dental providers, the dental therapist and the advanced dental therapist (8). Soon,dental therapy may expand to other states (9, 10).
The purpose of this study was to: 1) quantify current utilization of dental hygienists and dental assistants with expanded functions; 2) quantify dentists’ attitudes toward expanding functions via a new non-dentist provider model (the dental therapist), as well as Minnesota dentists’ attitudes toward the dental therapist model; 3) ascertain whether dentist and practice characteristics are associated with current utilization and dentists’ perceptions and attitudes towards expanded functions, and investigate the association between current utilization and perceptions and attitudes.
METHODS
The research setting is The National Dental Practice-Based Research Network. Many details about the network are publicly available at its web site (11); briefly, it comprises practitioner-investigators and staff in outpatient dental practices from the United States and Scandinavia (12, 13, 14). The network has a wide representation of practice types, treatment philosophies, and patient populations, including diversity with regard to the race, ethnicity, geography and rural/urban area of residence of both its practitioner-investigators and their patients. Analyses of these characteristics confirm that network dentists have much in common with dentists at large, while at the same time offering substantial diversity with regard to these characteristics (15, 16). However, a distinguishing characteristic of dentists in the network is their active participation in research, which may indicate a predilection for embracing new developments in dentistry. The network includes six regions, two of which include large group practice preferred provider organizations, the HealthPartners Dental Group (HP) located in the Midwest region and the Permanente Dental Association (PDA) located in the Western region. Until recently, most of the dentists were located in the southeast because it was the region of origin for the network (12).
The design for this study was cross-sectional, consisting of a single administration of a questionnaire to all network practitioner-investigators who had participated in one or more network studies of any type previously, and who were in current practice with an active practice address. This project was approved by the human participants institutional review boards (IRBs) at the University of Alabama at Birmingham and applicable regional IRBs of the network. The informed consent of all human subjects who participated in this investigation was obtained. Questions were taken from a larger questionnaire (“Infrastructure Update Survey”), the intent of which was to update certain practice characteristics of DPBRN practitioner-investigators. The full questionnaire is publicly available at the network’s Publications page (17).
The questionnaire queried practitoners’ current utilization of non-dentist providers and their perceptions of quality and practice efficiency with regard to these providers. Given a list of dental procedures, practitioner-investigators were asked to identify what dental procedures are done by each dental team member. Additional questions quantified dentists’ attitudes and opinions regarding emerging dental providers, such as the dental therapist. Five additional questions were asked of Minnesota dentists only and queried their interest in hiring a dental therapist, important hiring factors, and barrriers to hiring. In this survey, the term “expanded functions” means activities that dental hygienists and dental assistants cannot do in all U.S. states. Examples of “expanded functions” include placing and carving complex amalgam filling, composite, and stainless steel crowns,, administering local anesthetic injections, re-cementing permanent crowns or comparable procedures.
At the time the survey was conducted (December 2010 to March 2011), there were no practicing dental therapists in Minnesota. Practitioner-investigators were asked to complete the questionnaire within three weeks; reminder letters were sent at monthly intervals to those who had not completed the questionnaire within the three week timeframe.
Analysis
All analyses were done using SAS (18). Statistical significance was assumed alpha =0.05. Chi-square tests were used to assess significance of differences in frequency distributions, including employment of dental personnel by practitioner and practice characteristics, and whether selected procedures were delegated to dental hygienists or assistants differed by geographic region (Minnesota) and practice setting (PDA/HP). Logistic regression was used to adjust for the inter-relationship of practice being in Minnesota, being in PDA or HP practice, and graduating since 2000. Outcome variables included employment and experience working with expanded function dental hygienists or assistants, delegation of expanded functions, opinions regarding and likelihood of hiring a dental therapists. Odds ratios (OR) and 95% confidence intervals (CI) were calculated from the equations.
RESULTS
Practitioner and Practice Characteristics
A response rate of 76.3% (632/828) was achieved. Response rates did not differ by gender or year graduated dental school, but were lower in the southeast than other U.S. regions. Overall, 81% of practitioners were male, 92% were general practitioners, 55% were in solo practices, of which the majority (78%) was from the southeastern U.S. Of the entire sample, almost all practices employed dental assistants ([592/624] 95%) or dental hygienists ([591/628] 94%). Fewer practitioners employed associate dentists ([195/611] 32%), expanded function dental hygienists ([89/599] 15%), expanded function dental assistants ([188/609] 31%). In general, female practitioners, more-recent graduates and group practices employed associate dentists and expanded function dental hygienists or assistants at higher rates (Table 1). In adjusted analyses, only large group practices (PDA/HP) and dentists practicing in Minnesota were associated with employment of expanded function dental hygienists or assistants at higher rates (Table 1).
Table 1.
Employment of allied dental personnel, by selected practitioner and practice characteristics
| Practitioner/practice characteristic |
Total | Employs Associate Dentist1 |
Employs an Expanded Function Dental Hygienist or Assistant2 |
||||
|---|---|---|---|---|---|---|---|
| N | Col3 % | N | Row4 % | N | Row4 % | ||
| ALL | 632 | 100.0 | 195 | 31.9 | 200 | 32.8 | |
| Gender | |||||||
| Male | 512 | 81.0 | 144 | 28.9 | 153 | 30.8 | |
| Female | 120 | 19.0 | 51 | 45.1 | 47 | 42.0 | |
| p-value= | <.001 | .02 | |||||
| Graduation Year | |||||||
| Before 1970 | 30 | 4.8 | 5 | 17.2 | 3 | 10.0 | |
| 1970 – 1979 | 171 | 27.1 | 51 | 30.9 | 46 | 28.2 | |
| 1980 – 1989 | 208 | 32.9 | 44 | 22.1 | 67 | 33.7 | |
| 1990 – 1999 | 140 | 22.2 | 47 | 34.6 | 45 | 33.1 | |
| 2000 or later | 83 | 13.1 | 48 | 58.5 | 39 | 48.2 | |
| p-value= | <.001 | .002 | |||||
| Practitioner specialty | |||||||
| General practice | 584 | 92.4 | 174 | 30.9 | 185 | 32.9 | |
| Specialist | 48 | 7.6 | 21 | 43.8 | 15 | 31.9 | |
| p-value= | .07 | 0.88 | |||||
| Practice Type | |||||||
| Solo Private | 351 | 55.5 | 16 | 4.7 | 64 | 18.9 | |
| Group Private | 168 | 26.6 | 108 | 66.7 | 51 | 31.9 | |
| HP or PDA5 | 82 | 13.0 | 63 | 81.8 | 76 | 92.7 | |
| Public Health | 10 | 1.6 | 4 | 40.0 | 5 | 55.6 | |
| Academic setting/other | 21 | 3.3 | 4 | 21.0 | 4 | 20.0 | |
| p-value= | <.001 | <.001 | |||||
| Region | |||||||
| Southeast | 495 | 78.3 | 105 | 21.7 | 96 | 20.2 | |
| Midwest | 80 | 12.7 | 43 | 58.9 | 53 | 68.0 | |
| Northeast | 4 | 0.6 | 1 | 33.3 | 2 | 50.0 | |
| West6 | 53 | 8.4 | 46 | 90.2 | 49 | 92.4 | |
| p-value= | <.001 | <.001 | |||||
| Minnesota7 | 77 | 12.2 | 43 | 61.4 | 52 | 69.3 | |
| Non-Minnesota | 555 | 87.8 | 152 | 28.1 | 148 | 27.7 | |
| p-value= | <.001 | <.001 | |||||
Associate dentists: Missing for 21
Expanded function: Missing for 23
Col: Column percent
Row %: Percent among the row characteristic (e.g., Male) who employed the column specified personnel (e.g., associate dentist)
HP: HealthPartners Dental Group, PDA: Permanente Dental Associates
45 (85%) 53 of practitioners from West were from PDA
37 (48%) 77 of Minnesota practitioners were from HP
Experience with and attitudes toward expanded function dental hygienist/assistant
Of 604 practitioners who answered both questions, whether practice currently employs and whether ever worked with an expanded function dental hygienist or assistant, 90 (14.9%) of network dentists reported they had worked with and/or are in a practice that currently employs an expanded function dental assistant or dental hygienist. Sixty-eight dentists (11.3%) reported they had worked with expanded function allied personnel but did NOT currently employ, and 108 (17.9%) currently employ but had NOT previously worked with an expanded function dental assistant or hygienist. The majority of dentists (n=338; 56.0%) have never worked with an expanded function dental hygienist or assistant, nor currently employ one. This distribution differed substantially for PDA/HP practices than other practices, e.g., among PDA/HP practices, 52% of practitioners reported current employment of an expanded function dental hygienist or assistant and that they have had experience working with one compared to 9% in other practice settings (Table 1).
A higher proportion of dentists from Minnesota (64% [48/75]) than elsewhere (21% [117/552], p<0.001) reported having had experience working with an expanded function dental hygienist or assistant. This difference was present when stratified by large group private practices (PDA or HP) (p<0.001 in each stratum), the largest employers of expanded function personnel [in this study population]. Overall, 54% [335/626] of dentists thought expanded function capabilities of these personnel had a positive impact on provision of quality dental care. Experience working with or being in a practice that currently employs an expanded function dental hygienist or assistant was the only characteristic that was significantly associated with agreeing that expanded function personnel had a positive impact on quality of dental care (OR=4.1; 95% CI: 2.8 – 6.0, p<0.001), while working in PDA or HP had an association of marginal statistical significance (OR=1.9; 95% CI: 1.0–3.7, p=0.06); neither practice in Minnesota nor graduation year had any association when adjusted for the former two.
Utilization
The most frequently performed procedures by dental hygienists are oral health education, radiographs, removal of supra- and sub-gingival deposits, and root curettage; for assistants, oral health education, radiographs, and impressions for diagnostic casts (See Table 3). Dental hygienists administered local anesthesia in only 17% of the dental offices even though at the time of the survey it was within the dental hygiene scope of practice in all but seven of U.S. states (19). With respect to restorative procedures performed in 621 (98%) practices, 6% percent of dentists reported that they delegate these procedures to dental assistants and less than 2% percent reported delegation to dental hygienists. Varying degrees of restorative procedures are permitted in Ohio, Minnesota, Washington, New Mexico, California, Oregon, Pennsylvania, New York, Maine, Tennessee and Mississippi. In analysis adjusted for year graduated (2000 or later), two practice settings, Minnesota practice and whether or not PDA/HP, were more likely to delegate two of the expanded function procedures: place, carve, and adjust restorations and administer local anesthetics (Figure 2).
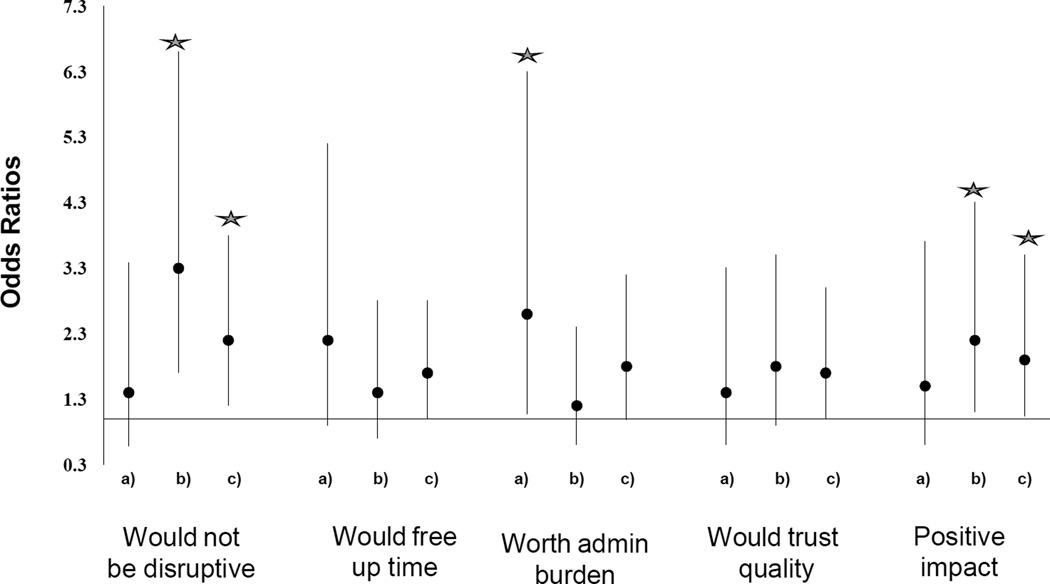
Figure 2.
Associations (a,b,c below) with positive attitudes towards dental therapists
a) PDA/HP b) MN c) Ever work with or currently employ expanded function dental hygienist/assistant – all 3 in models, as is graduation year. Vertical lines represent 95% confidence intervals.
 P<0.05
P<0.05
Attitudes Toward New Non-Dentist Provider, Dental Therapist
When asked about the newest non-dentist provider, the dental therapist (excluding Minnesota dentists): 27% [N=149] had never heard of a dental therapist, 27% [N=151] reported being “a little” familiar, 19% were “somewhat” [N=103], 18% [N=97] were moderately, and 9% were very [N=51] familiar with the dental therapist. Among the non-Minnesota dentists who were at least somewhat informed, a majority felt that having a dental therapist would disrupt their relationship with their patients (67%) and add an administrative burden (63%). However, 39% of the respondents reported that having a dental therapist would free up time to focus on more complex and interesting dental procedures and 27% would trust the quality of the dental therapist’s work. Minnesota dentists in the network had more positive opinions on all four aspects of the dental therapist model that were queried (Figure 2).
Out of the entire sample, 25% of dentists thought that dental therapists would have a positive or somewhat positive impact on quality of dental care, 51% thought that dental therapists would increase access to care, 45% thought they would have no impact on access, and 4% thought they would decrease access to care in their state. In analysis adjusted for year graduated (2000 or later), state, and practice setting (PDA/HP or not), in general, Minnesota dentists in the network, dentists practicing in PDA/HP, and dentists with prior experience working with expanded function personnel had more positive attitudes towards dental therapists (Figure 2).
Minnesota Dentists’ Perceptions/Attitudes, Dental Therapist
Twice the proportion of Minnesota dentists compared to non-Minnesota dentists (49% [37/76] vs. 20% [112/551], P<0.001) were at least somewhat likely to hire a dental therapist. Similarly, twice the proportion of Minnesota dentists compared to non-Minnesota dentists (62% [48/77] vs. 37% [206/552], P<0.001) thought dental therapists would at least somewhat increase access to dental care, and would have a positive impact on quality of dental care provided. These differences remained present and significant when adjusted for practice setting (PDA or HP) and graduation year, also when adjusted for whether ever worked with or currently employs an expanded function dental hygienist or assistant (Figure 2).
DISCUSSION
Although the scopes of practice have expanded during the past four decades for both dental assistants and hygienists, results from this study suggest that the procedures delegated to these providers have remained aligned with conventional roles. It appears that changes to the law have not resulted in non-dentist providers being utilized to the fullest extent in the NDPBRN. With the exception of oral health education, radiographs, deposit removal and root curretage, the dentist is performing all procedures at a much higher percentage of the time even though a dental assistant or hygienist legally can perform these tasks in most states.
The majority of respondents feel that non-dentist providers with expanded functions have a positive impact on dental practice. This sentiment has not changed as previous studies have confirmed that dentists support delegation to allied personnel as a means to increase dental services (20, 21, 22). Yet, expanding the scopes of practice for allied providers has not dramatically changed dental delivery (23). Since the 1960s, studies have demonstrated that non-dentist providers can reduce cost, provide high quality care and do not put patients at risk (24–31). These findings have motivated policy makers in many states to consider expanding the workforce via non-dentist providers.
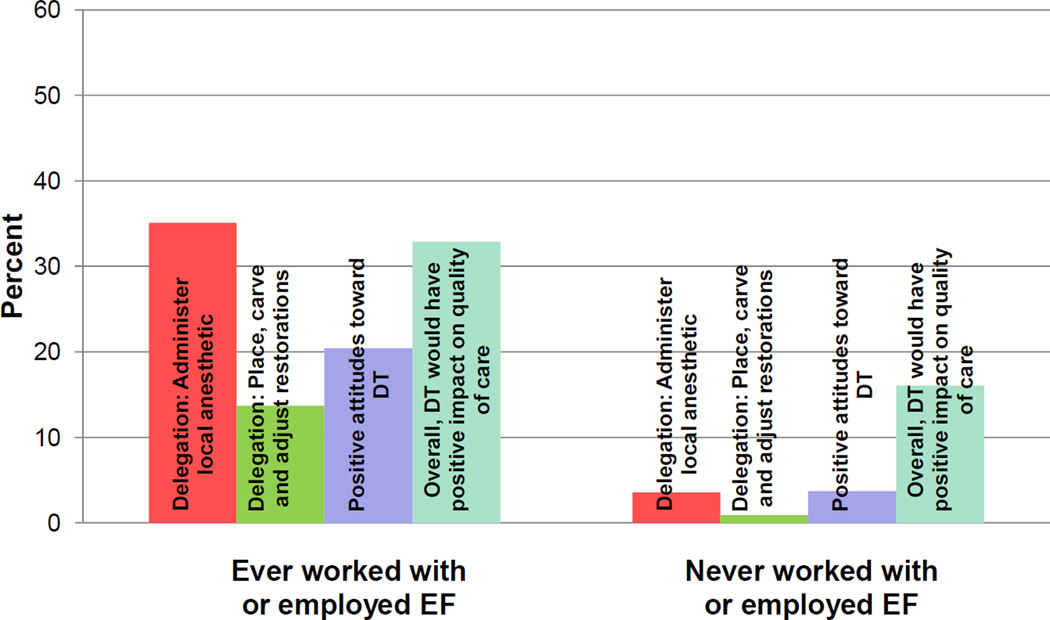
Dentists in this study indicated dental hygienists and assistants with expanded functions have a positive impact on the quality of dental care yet underutilize them in comparison to what is allowed by law. Similarily, nearly one quarter of respondents indicated that they would trust the quality of a dental therapist’s work, and felt that employing a dental therapist would free up their time for more complex and interesting dental procedures; however, the majority indicated that it is unlikely that they will consider hiring a therapist. Therefore, dentists appear to embrace the concept of utilizing non-dentist providers; nonetheless, they have not changed their practice delivery models. It is clear from the results of this study that exposure to and utilization of expanded function allied providers is associated with higher delegation of procedures and more positive attitudes toward these providers and toward dental therapy (Figure 1). Ever working with or being in a practice that currently employs an expanded function dental hygienist or assistant was the only characteristic that was significantly associated with agreeing that expanded function personnel had a positive impact on quality of dental care. A higher proportion of Minnesota dentists and larger group practices (HP and PDA) were more likely to delegate procedures and had more positive views of dental therapy than did solo practitioners. Minnesota dentists in the network supported the passage of the dental therapy law, so it is not surprising that that they would have more positive views of dental therapy than dentists in other network regions.
Figure 1.
Distribution (%) of practitioners’ delegation to expanded function allied providers and attitudes* toward dental therapy (DT) and its potential impact on quality of care according to experience with expanded function (EF) allied providers
* Agree with all 4 aspects of attitudes towards DT assessed: would free up time, would trust quality of their work, they would NOT disrupt relationships nor increase administrative burden
Limited experience integrating and utilizing non-dentist providers in a team delivery model may explain why the roles of dental assistants and hygienists have remained largely unchanged. Early research on delegation to non-dentist providers is consistent with the notion that lack of knowledge on how to optimally integrate and utilize allied providers can be a barrier to maximum delegation and teamwork (21, 33). A recent study by Beazoglou found that general dental practices could substantially increase their capacity to see more patients with the effective use of expanded function allied dental personnel (32). Investigators have recommended that dental students have opportunitues to work with allied providers to learn how to utilize their team members more effectively and be comfortable in the role of delegator (23). The socialization to this role is central to the success of the new dental therapist workforce model (33).
A limitation of this study is the varying degrees of expanded functions that exist among states in the network. All states in the network permit some form of expanded functions for either dental assistants or dental hygienists. However, states in the southeast region, the largest region in the network, have the most restrictive scopes of practice for allied dental providers. The only states in the network that allow dental hygienists and/or dental assistants to perform a full range of restorative procedures are Oregon, Washington and Minnesota. Delegation of the EF procedures are presented separately in Figure 1 for these regions/type of practice. In addition, the study sample is not a representative sample of dentists in the US and therefore the results cannot be generalized to all U.S. dentists.
CONCLUSION
This study informs the practicing dental community about the duties that are actually being performed by non-dentist providers in a U.S.practice-based research network. The results of this study indicate that changes to the law have not resulted in expanded function allied personnel being utilized to the fullest extent. This study found that dentists who have previously worked with or currently employ expanded function dental hygienists or assistants in their practices view them more positively and are more likely to delegate procedures to these providers. In addition, they have more positive views of dental therapists and believe they have the potential to increase access to care. Effective use of expanded function allied dental personnel has the potential to expand the capacity of general dental practices to treat more patients, yet these providers are under-utilized. Limited experience integrating and utilizing non-dentist providers in a team delivery model may explain why the roles of dental assistants and hygienists have remained largely unchanged. This finding poses a challenge for dental education and should be addressed in light of the oral health disparities that exist in our nation.
Table 2.
Delegation of procedures1 to dental assistants and hygienists
| Performed by Dentist |
Hygienist | Assistant | Hygienist or Assistant |
||
|---|---|---|---|---|---|
| Procedure | N | % | % | % | % |
| Remove supra-gingival deposits | 621 | 63.4 | 93.4 | 14.5 | 95.3 |
| Take radiographs | 631 | 53.7 | 87.8 | 89.2 | 93.7 |
| Oral health education and prevention | 627 | 78.5 | 90.3 | 75.1 | 93.3 |
| Remove sub-gingival deposits | 618 | 68.8 | 91.8 | 2.3 | 93.0 |
| Applying topical medications | 621 | 70.8 | 87.4 | 62.6 | 91.1 |
| Taking impressions | 621 | 69.9 | 55.1 | 87.6 | 90.7 |
| Perform root curettage | 610 | 63.9 | 84.4 | 1.3 | 85.7 |
| Remove excess cement | 628 | 85.4 | 62.9 | 71.2 | 84.6 |
| Etch enamel surfaces, apply sealants | 614 | 79.0 | 76.2 | 36.6 | 80.6 |
| Cement/adjust temporary restorations | 621 | 81.8 | 23.7 | 61.7 | 66.2 |
| Place/remove rubber dams | 541 | 86.9 | 13.9 | 57.9 | 60.6 |
| Fabricate athletic mouth guards | 488 | 73.6 | 23.2 | 53.9 | 59.6 |
| Place temporary fillings | 619 | 94.4 | 27.8 | 48.6 | 54.3 |
| Suture removal | 622 | 78.0 | 24.1 | 42.8 | 46.1 |
| Denture soft relines | 567 | 95.6 | 4.1 | 12.7 | 15.2 |
| Re-cement permanent crowns | 622 | 85.7 | 3.0 | 2.9 | 5.1 |
| Extract primary teeth | 617 | 83.8 | 1.5 | 0.2 | 1.5 |
| Cavity excavation/preparation for simple permanent filling | 622 | 85.7 | 0.6 | 0.2 | 0.8 |
| Expanded function procedures | |||||
| Place, carve, adjust restorations | 621 | 84.4 | 1.8 | 6.0 | 6.6 |
| Administer local anesthetics | 629 | 82.8 | 17.5 | 0.2 | 17.6 |
| Administer nitrous oxide inhalation | 535 | 76.1 | 35.7 | 22.2 | 39.4 |
Procedures may be performed by more than one member of dental team/staff. All procedures listed are within the scope of practice of dental therapists. Procedures not quieried about that are within the scope of practice of dental therapists include charting of the oral cavity, pulp vitality testing, atraumatic restorative therapy, administration of local anesthetics, preparation and restoration of decidous and permanent teeth with complex amalgam fillings and stainless steel crowns, pulpotomy, simple extraction of decidous and permanent teeth, dressing changes, reimplantation of avulsed teeth.
Number of practices (of total of 632) that indicated the procedure was performed there by either dentist, dental hygienist, or assistant.
ACKNOWLEDGEMENTS
This investigation was supported by NIH grants U01-DE-16746, U01-DE-16747 and U19-DE-22516. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health.
Footnotes
This manuscript contains original material that has not been submitted for publication or has previously been published elsewhere.
Contributors
Christine Blue contributed to the development of the survey questions used in the study; interpretation of all aspects of the study; analysis and writing the article. Ellen Funkhouser contributed to the statistical analysis of data; interpretation of all aspects of the study and to the writing of the article. Sheila Riggs and Brad Rindal contributed to the development of the survey questions, interpretation of the results, and to the writing of the article. Don Worley, Dan Pihlstrom, and Paul Benjamin contributed to the interpretation of the results and to the writing of the article. Gregg Gilbert contributed to obtaining the funding, originating the study, the conduct, design, interpretation of all aspects of the study; and writing the article.
References
- 1.US Department of Health and Human Services. Oral health in America: a report of the surgeon general. Rockville: Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- 2.McKinnon M, Luke G, Bresch J, Moss M, Valecovic RW. Emerging Allied Dental Workforce Models: Considerations for Academic Institutions. J Dent Ed. 2007;71:1476–1491. [PubMed] [Google Scholar]
- 3.American Dental Association. House of Delegates responsibility for meeting manpower needs. ADA Transactions. 1966:370. [Google Scholar]
- 4.Nash DA, Friedman JW, Kardos TB, Kardos RL, Schwarz E, Satur J, et al. Dental therapists: a global perspective. Int Dent J. 2008;58:61–70. doi: 10.1111/j.1875-595x.2008.tb00177.x. [DOI] [PubMed] [Google Scholar]
- 5.Ward P. The changing skill mix: experiences on the introduction of the dental therapist into general dental practice. Br Dent J. 2006;200:193–197. doi: 10.1038/sj.bdj.4813251. [DOI] [PubMed] [Google Scholar]
- 6.Harris R, Burnside G. The role of dental therapists working in four personal dental service pilots: type of patients seen, work undertaken, and cost-effectiveness within the context of the dental practice. Br Dent J. 2004;197:491–496. doi: 10.1038/sj.bdj.4811749. [DOI] [PubMed] [Google Scholar]
- 7.Bolin KA. Assessment of treatment provided by dental health aide therapists in Alaska. J Am Dent Assoc. 2008;139(11):1530–1535. doi: 10.14219/jada.archive.2008.0080. [DOI] [PubMed] [Google Scholar]
- 8.Minnesota Board of Dentistry Statutes. The Office of Revisor of Statutes. 2010. [cited 2012 July 2]. Chapter 150A & 319B. [Google Scholar]
- 9.Kellogg WK. [cited 2011 May 17];Foundation supports community-led efforts in five states to increase oral health care access by adding dental therapist to the dental team. 2010 Available from: www.wkkf.org.news/articles/2010/11/wk-kellogg-foundation-supports-community-led-efforts.aspx.
- 10.Pew Center on the States. [cited 2010 June 6];It takes a team: how new dental providers can benefit patients and practices. 2010 Available from: http://www.pewcenteronthestates.org/report_detail.aspx?id=61628, 2010.
- 11. [cited 2012 July 8];National Dental Practice-Based Research Network. 2012 Available from: www.NationalDentalPBRN.org.
- 12.Gilbert GH, Williams OD, Rindal DB, Pihlstrom DJ, Benjamin PL, Wallace MA for The DPBRN Collaborative Group. The creation and development of The Dental Practice-Based Research Network. J Am Dent Assoc. 2008;139(1):74–81. doi: 10.14219/jada.archive.2008.0024. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert GH, Qvist V, Moore SD, Rindal DB, Fellows JL, Gordan VV, et al. for The DPBRN Collaborative Group. Institutional Review Board and regulatory solutions in The Dental PBRN. J Public Health Dent. 2010;70(1):19–27. doi: 10.1111/j.1752-7325.2009.00139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilbert GH, Richman JS, Gordan VV, Rindal DB, Fellows JL, Benjamin PL, et al. for The DPBRN Collaborative Group. Lessons learned during the conduct of clinical studies in the Dental PBRN. J Dent Educ. 2011;75(4):453–465. [PMC free article] [PubMed] [Google Scholar]
- 15.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, et al. for The DPBRN Collaborative Group. Dentists in practice-based research networks have much in common with dentists at large: evidence from The Dental PBRN. Gen Dent. 2009;57(3):270–275. [PMC free article] [PubMed] [Google Scholar]
- 16.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, et al. for The DPBRN Collaborative Group. Practices participating in a dental PBRN have substantial and advantageous diversity even though as a group they have much in common with dentists at large. BMC Oral Health. 2009;1:26–35. doi: 10.1186/1472-6831-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Dental Practice-Based Research Network. [cited 2013 January 8];Peer-reviewed Publications page. 2013 Available from: http://nationaldentalpbrn.org/peer-reviewed-publications.phpPlease see the citation for this publication and access the Infrastructure Update Survey link.
- 18.SAS/STAT version 9.2, 2009. Cary, NC: SAS Publishing; 2009. [cited 2011 July 8]. SAS Institut. Available from: www.sas.com/apps/pubscat/complete.jsp. [Google Scholar]
- 19.American Dental Hygienists’ Association. [cited 2012 April 5];States where dental hygienists can administer local anesthesia. 2012 Available from: www.adha.org/governmental-affairs/downloads/localanesthesiamap.pdf.
- 20.Koerner KR, Osterholt DA. Student survey report: Washington dentists questioned on expanded duties. J Am Dent Assoc. 1973;86:995–1000. doi: 10.14219/jada.archive.1973.0227. [DOI] [PubMed] [Google Scholar]
- 21.Leske GS, Leverett DH. Variables of affecting attitudes of dentists toward the use of expanded function auxiliaries. J Dent Educ. 1976;40(2):79–85. [PubMed] [Google Scholar]
- 22.Domer LR, Bauer JC, Bomberg TJ. Attitudes toward the use of expanded function dental auxiliaries as a function of provider characteristics and participation in expanded-function training. J Pub H Dent. 1977;37(1):9–22. doi: 10.1111/j.1752-7325.1977.tb02872.x. [DOI] [PubMed] [Google Scholar]
- 23.Chapko MK, Milgrom P, Bergner MB, Conrad D, Skalabrin N. Delegation of expanded functions to dental assistants and hygienists. Am J Public Healt. 1985;75:61–65. doi: 10.2105/ajph.75.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hammons PE, Jamison HC, Wilson LL. Quality of service by dental therapists in an experimental program at the University of Alabama. J Am Dent Assoc. 1971;82:1060–1066. doi: 10.14219/jada.archive.1971.0171. [DOI] [PubMed] [Google Scholar]
- 25.Lotzar S, Johnson DW, Thompson MB. Experimental program in expanded functions for dental assistants: phase 3 experiment with dental teams. J Am Dent Assoc. 1971;82:1067–1081. doi: 10.14219/jada.archive.1971.0196. [DOI] [PubMed] [Google Scholar]
- 26.Brearley LJ, Rosenblum FN. Two-year evaluation of auxiliaries trained in expanded duties. J Am Dent Assoc. 1972;84:600–610. doi: 10.14219/jada.archive.1972.0094. [DOI] [PubMed] [Google Scholar]
- 27.Abramowitz J, Berg LE. A four-year study of the utilization of dental assistance with expanded functions. J Am Dent Assoc. 1973;87:623–635. doi: 10.14219/jada.archive.1973.0462. [DOI] [PubMed] [Google Scholar]
- 28.Lobene R, Kerr A. The Forsyth experiment: an alternative for dental care. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 29.Bolin KA. Assessment of treatment provided by dental health aide therapists in Alaska: a pilot study. J Am Dent Assoc. 2008;139:1530–1535. doi: 10.14219/jada.archive.2008.0080. [DOI] [PubMed] [Google Scholar]
- 30.Bader JD, Lee JY, Shugers DA, Burrus BB, Wetterhall S. Clinical technical performance of dental therapists in Alaska. J Am Dent Assoc. 2011;142:322–329. doi: 10.14219/jada.archive.2011.0171. [DOI] [PubMed] [Google Scholar]
- 31.Worley DC, Thoke MJK, Asche SE, Godlevsky OV, Schmidt AM, Yardic RL, et al. A comparison of dental restoration outcomes after placement by restorative function auxiliaries versus dentists. Health Partners Dental Group, Bloomington, MN. Public Health Dent. 2012;72:122–127. doi: 10.1111/j.1752-7325.2011.00291.x. 2012. [DOI] [PubMed] [Google Scholar]
- 32.Beazoglou TJ, Chen L, Lazar VF, L. Brown J, Ray SC, Heffley DR, Berg R, Bailit HL. Expanded Function Allied Dental Personnel and Dental Practice Productivity and Efficiency. J Dent Educ. 2012;76:1054–1060. [PubMed] [Google Scholar]
- 33.Blue C, Phillips R, Born D, Lopez N. Beginning the socialization to a new workforce model: dental students’ preliminary knowledge of and attitudes about the role of the dental therapist. J Dent Educ. 2011;75:1465–1475. [PubMed] [Google Scholar]