Abstract
Objective
Clinical study to determine the acceptability and feasibility of acupuncture for acute postoperative pain control in hospitalized children.
Design
Nonrandomized clinical trial.
Setting
A single, tertiary referral pediatric intensive care unit.
Patients
A total of 20 patients aged 7 months to 18 years. Eleven of the patients had posterior spinal fusion surgery and the remaining nine patients had other surgical diagnoses.
Interventions
Two 10- to 15-minute sessions of acupuncture 24–48 hours apart.
Outcome Measures and Results
The treatment was highly accepted (27 patients were approached and 4 patients refused; of the 23 patients enrolled, 20 patients completed the study). Acupuncture was well tolerated by patients without adverse events related to treatment. In follow-up interviews, 70% of both parents and patients believed acupuncture helped the child's pain. Eighty-five percent of the parents said they would pay out of pocket for acupuncture if not covered by insurance. The pain scores, vital signs, and narcotic usage were recorded before and several times after acupuncture. In posterior spinal fusion patients, the mean pain scores (0–10) immediately before and 4 and 24 hours after acupuncture were: 3.7, 1.7, and 3.1, respectively, after the first acupuncture session and 3.7, 2.2, and 3.1, respectively, after the second session. In the other surgical cohort, the mean pain scores immediately before and 4 and 24 hours after the first session of acupuncture were 2.5, 0.3, and 1.6, respectively.
Conclusions
Our results support that acupuncture is highly accepted and feasible in critically ill, postoperative pediatric patients with acute pain. Our findings suggest that acupuncture may be a potentially useful adjunctive tool for acute pediatric postoperative pain management. A randomized, controlled clinical trial is warranted to confirm these findings.
Keywords: pain, postoperative pain, acupuncture, child, complementary therapies, pediatric intensive care unit
There has been a nationwide increase in attention to the assessment and management of pediatric pain (1, 2). Despite the increased knowledge and advances in pediatric pain, acute pain in hospitalized children remains a significant problem (1, 3–5) that is difficult to manage in everyday clinical practice (6). Children admitted to the pediatric intensive care unit are especially at risk for pain (7) and its associated adverse physiologic responses (8, 9), including increased oxygen consumption, atelectasis, increased work of breathing, hypertension, and tachyarrhythmias (10).
Management of acute pain is best accomplished using a multifaceted approach involving both pharmacologic and nonpharmacologic therapies (6, 11). Using nonpharmacologic treatments may be beneficial by reducing the need for opioids or other analgesics and subsequent drug-induced side effects, such as nausea and vomiting, respiratory depression, and ileus (12). Recently, complementary and alternative medical therapies, such as acupuncture, have become widely accepted (13–15). In fact, as of 2005, about a one-third of pediatric pain management services affiliated with major universities offer acupuncture, primarily for chronic pain management (16).
Acupuncture was developed >2500 years ago in China according to the theory that energy, or qi, flows although pathways, or meridians, within the body (17). In the Chinese medical model, blockages along the meridians of energy result in pain and disease. Acupuncture needles placed at identifiable acupuncture points close to the skin may restore the flow of energy (17, 18). The biomedical explanation is that placing acupuncture needles at specific pain points releases endogenous opioid peptides, such as beta-endorphin, and perhaps other neurotransmitters and neurohormones in the brain (17, 18).
Clinically, acupuncture can help with adult postoperative and chemotherapy nausea and vomiting as well as postoperative dental pain (18). Although most studies of acupuncture for pain control are in adults (19, 20), there are some studies in pediatric chronic pain (21–23), such as in migraine headaches (24) and cystic fibrosis (25). However, there are limited data on the use of acupuncture for acute pain in hospitalized children.
Therefore, the objectives of the study were to primarily determine the feasibility and acceptability of acupuncture as an adjunctive treatment for acute pain in critically ill, postoperative children in the hospital setting and secondarily collect important preliminary data required to design future randomized controlled trials.
MATERIALS AND METHODS
Patients were enrolled from September 27, 2005, to March 22, 2006, at the pediatric intensive care unit at Children's Hospital and Research Center Oakland.
The Committee of Human Research and Institutional Review Board approved the research protocol. We obtained written, informed consent from the parent or legal guardian of each patient and/or from the patient when appropriate. A Data Safety and Monitoring Board reviewed the interventions and their effects.
Two patient cohorts were enrolled in the study. The inclusion criteria for the first cohort (group 1) were patients aged 7 to 18 years who were postoperative from spinal fusion surgery, spontaneously breathing, and developmentally able to use patient-controlled analgesia (PCA). The inclusion criteria for the second cohort (group 2) were patients aged 6 months to 18 years admitted to the pediatric intensive care unit who required intravenous pain medication. Exclusion criteria were age <6 months, prior acupuncture treatment, hemodynamic instability, immunodeficiency, increased intracranial pressure, inability to react to painful stimuli, moderate or severe developmental delay, severe dermatologic conditions, extensive burns, use of cardiopulmonary bypass within last 24 hours, therapeutic anticoagulant medication (excluding aspirin, nonsteroidal anti-inflammatory drugs, and/or prophylactic heparin), chronic steroid use, neutropenia (absolute neutrophil count <1000), thrombocytopenia (platelets <100,000), excessive pain/sedation medication inducing deep sedation, or muscle relaxant medication. Patients younger than 3 years of age were not treated with acupuncture needles (see below) so were still eligible if they were on therapeutic anticoagulant therapy.
As a part of patient screening, we contacted eligible patients who were scheduled for posterior spinal fusion or other surgeries. Whenever possible, we obtained consent preoperatively to allow more time for anticipatory guidance regarding acupuncture. We reassured parents and patients it was common to have anxiety or fear about the idea of having needles inserted. We explained that acupuncture needles, unlike thick and hollow needles used for injection or phlebotomy, are extremely thin, fine, and solid. We also offered to show a sterile acupuncture needle to the children and families so they could look at it and touch them if they so desired. We stated that although some children did not feel the needle insertion, others feel a little pinch or prick that might last a second. It was also explained that most children do not feel the needles after placement but if any needle should cause pain for longer than a couple of seconds, then the acupuncturist would either adjust or remove the needle so there would be no further pain (22).
Eligible patients meeting study criteria underwent two 10- to 15-minute acupuncture sessions. For postoperative patients, the first session was performed on the first postoperative day to minimize the impact of the clinical effects of anesthesia and intraoperative medication as a confounding factor. The second acupuncture session was performed approximately 24–48 hours after the first session, when there was likely minimal residual effect of the first acupuncture treatment (26, 27).
A licensed acupuncturist (MAS) performed acupuncture on all the patients using the Japanese method of acupuncture (26). The patients received 3–6 needles and individually tailored acupuncture treatment depending on their diagnosis. All points were needled using Seirin number 3 (0.20) 30-mm needles. The needles were inserted and manipulated by hand at insertion and then again after 10 minutes. Needles were removed after 15 minutes.
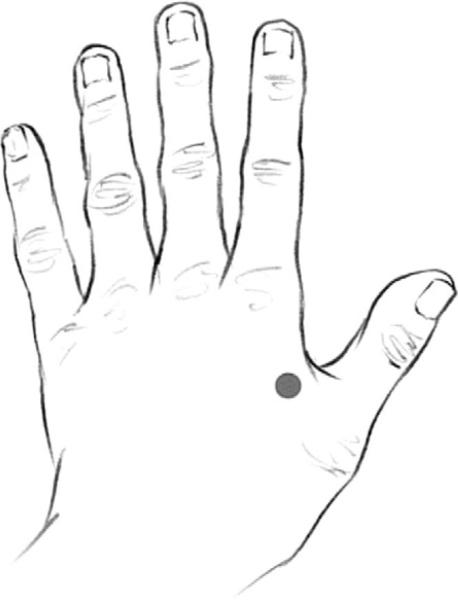
Acupuncture was done at the following points for patients after posterior spinal fusion surgery (Figs. 1–4):
Large Intestine 4 (Hegu). Located on the dorsum of the hand between the first and second metacarpal bones, at the midpoint of the second metacarpal bone and close to its radial border.
Liver 3 (Taichong). Located on the dorsum of the foot in the hollow distal to the junction of the first and second metatarsal bones.
Urinary Bladder 60 (Kunlun). Located between the prominence of the lateral malleolus and the Achilles tendon.
Kidney 3 (Taixi). Located in the depression between the medial malleolus and the Achilles tendon, level with the prominence of the medial malleolus.
All four points are located on the extremities. They were chosen for their effectiveness primarily and ease of access secondarily.
Figure 1.
Large intestine 4 (Hegu).
Figure 4.
Kidney 3 (Taixi).
The combination of liver 3 and large intestine 4 is known for its ability “to vigorously activate the qi and blood and ensure their smooth passage throughout the body” (28). Trauma, such as surgery, directly disrupts the free flow of qi and blood. When qi and blood are not moving freely, pain is felt. This combination of points has a general effect on all the qi and blood of the body. It is often used to treat pain anywhere in the body.
Urinary bladder 60 was chosen because it activates the entire bladder channel and clears obstructions—i.e., qi and blood flow disrupted by surgery—all down the back. It is “vital in the treatment of disorders of the back and spine from the neck right down to the coccyx” (28). It is often referred to as the aspirin point for back pain (29).
Kidney 3 was chosen for its effect of nourishing the kidneys, which control the low back, including the lumbar area, and support the bones. For the patients with spinal surgery, the fact that their spines had formed improperly and required surgery implied a kidney disharmony. The kidney channel also connects with the bladder channel and can be used to treat the back.
For each patient who had posterior spinal fusion surgery, all four points were used. There were a total of six needles used. Large intestine 4 and liver 3 were needled bilaterally. Urinary bladder 60 and kidney 3 were each needled only on one side, contralateral to each other. Patients were always able to move around easily and accessibility to the needling site determined the side on which these latter two points were needled.
All other surgical patients seen were treated according to the particular surgery/pain they experienced. Most received treatment at the points liver 3 and large intestine 4 described above.
Children younger than 2 years of age were treated with Shonishin, a Japanese needling technique that stimulates the meridian system with small tools made for that purpose (30). Young children's meridian system is not developed fully, and therefore, it is more effective to treat the whole area or affected meridian (30). A spring-loaded noninsertion probe was gently bounced on particular point areas and a smooth scraper was lightly rubbed along the meridian(s).
We measured the following clinical parameters at different intervals before and after each acupuncture session: heart rate, blood pressure, pain score, amount of pain and sedation medication, and number of PCA attempts if applicable. Patient self-reported pain scores using a standard numeric scale ranging from 0 to 10 whenever possible (31). Otherwise, other validated pain scales, such as the Face, Legs, Activity, Cry, Consolability scale, were used (31). In assessing narcotic usage, we focused on morphine PCA in group 1 because this was the most common form of intravenous analgesic administered. The data were collected at 2 hours before and immediately pretreatment, and at 2, 4, 8, and 24 hours posttreatment.
We asked the parent and child (if older than 7 years) to answer four questions after both sessions of acupuncture. First, we asked if they thought the acupuncture helped the child's pain and if they would consider acupuncture for the child in the future. Then, we asked parents who would consider future acupuncture for their child if they were willing to pay out of pocket for acupuncture (if not covered by insurance) and if so, the amount they would pay per treatment. Finally, we also collected general comments about the acupuncture treatment.
Statistical Analysis
The results are expressed as mean ± sd or range. Values at baseline and at 4 hours after treatment were compared using the Wilcoxon's signed rank test. Summary statistics are provided. This is a preliminary study for the purposes of determining feasibility and obtaining data for sample size estimation in future trials rather than determining statistically significant differences in effects due to acupuncture. Therefore, p values were not intended for interpretation as they would in randomized, controlled clinical trials.
RESULTS
Of the 27 patients invited to participate, 86% (23) of patients accepted and 14% (4) declined (two patients had fear of needles and two patients were below age 5 and their parents did not think they would tolerate the treatment). Eighty-seven percent of participants (n = 20) completed the study and 13% (n = 3) did not. The following reasons were given for dropping out of the study: lack of significant postoperative pain (one patient), excessive anxiety regarding treatment (one patient), and excessive stranger anxiety (one patient). Of the 20 patients who completed the treatment, two patients from group 2 were excluded from the statistical analysis because the planned surgical intervention was not carried out or the patient had received acupuncture preoperatively. However, they are still included in the interview results because they received acupuncture for pain related to their underlying condition. One of these patients had perforated appendicitis with small bowel obstruction and received two acupuncture treatments for the associated pain but did not require surgery. The other patient had a resection of a perforated Meckel's diverticulum and received non-needling acupuncture both before and after surgery for pain. The remaining 18 received acupuncture postoperatively. No adverse events reported were related to acupuncture. One patient from group 1 developed transient hypotension approximately 7 minutes after acupuncture. Both the primary physician and the Data Safety and Monitoring Board reviewed the event. Both parties independently concluded that the hypotension was not related to acupuncture but rather to postoperative hypovolemia.
Individual patient characteristics and diagnoses are described in Tables 1 and 2. The ethnic background of the patients were as follows: 35% whites (7), 50% Latinos (10), 10% Asians (2), and 5% African American (1). In group 1, all patients received two sessions of needling acupuncture postoperatively. One patient in group 1 had a history of chronic pain due to metastatic osteosarcoma to the spine requiring home narcotic medications. In group 2, four patients received non-needling acupuncture or Shonishin (patients 1, 2, 4, and 9). Also, two patients in group 2 (patients 3 and 6) only had one acupuncture session because they were discharged before the second session. Of the patients who completed two sessions of acupuncture, 61% of the patients received the second session of acupuncture in the inpatient ward after they were transferred out of the pediatric intensive care unit.
Table 1.
Patient characteristics
| Characteristic | Number (Percent/Range) |
|---|---|
| Group 1 | |
| Number of patients | 11 |
| Male | 4 (36%) |
| Median age (range, in yrs) | 13 yr (8–18) |
| Mean age (sd, in yrs) | 13.2 yr ± 3.1 |
| Use of morphine patient controlled analgesia | 11 (100%) |
| Days in the intensive care unit (median, range) | 2 d (1–6) |
| Days in the hospital (median, range) | 7 d (6–63) |
| Group 2 | |
| Number of patients | 9 |
| Male | 6 (67%) |
| Median age (range, in mos/yrs) | 2.7 yr (7 mo–16 yr) |
| Mean age (sd, in yrs) | 7.6 yr ± 6.9 |
| Days in the intensive care unit (median, range, in days) | 3 d (1–21) |
| Days in the hospital (median, range, in days) | 5 d (2–24) |
Table 2.
Diagnoses of group 2 patients
| Group 2 Patients | Type of Surgery/Diagnosis |
|---|---|
| Patient 1 | Cranial remodeling for craniosynostosis |
| Patient 2 | Atrioventricular canal repair |
| Patient 3 | Cervical laminoplasty for cervical stenosis |
| Patient 4 | Atrioventricular valve repair and patch repair of supravalvular pulmonic stenosis, history of transposition of great arteries |
| Patient 5 | Pulmonary band removal, pulmonary artery and atrioventricular valve repair |
| Patient 6 | Third ventriculostomy and shunt revision |
| Patient 7 | Thoracotomy for benign thymoma resection |
| Patient 8a | Perforated appendicitis with small bowel obstruction |
| Patient 9a | Resection of perforated Meckel's diverticulum |
Excluded from statistical analysis.
Vitals Signs and Pain Scores
The purpose of obtaining the vital signs and pain scores at different intervals was to collect standard deviations of the outcome measures to calculate sample sizes for future randomized controlled trials.
We observed general trends of decrease in heart rate, systolic blood pressure, and pain scores after acupuncture, especially at 4 hours posttreatment, with a return toward baseline by 24 hours for some measures (Tables 3 and 4). Four hours after the first treatment in group 1, seven patients (64%) had decreases in pain scores, three had no change (27%), and one had an increase in pain score (9%). In group 2, five patients (71%) had a decrease in pain scores and two had no change (29%). Four hours after the first treatment, group 1 had a decrease in pain scores (p < 0.05) and a decrease in heart rates (p < 0.05). Group 2 had a decrease in pain scores (p < 0.05) 4 hours after the first treatment and a decrease in systolic blood pressures (p < 0.05) 4 hours after the second treatment.
Table 3.
Vital signs and pain scores before and after the first treatment
| Baseline | 2 Hours After Treatment | 4 Hours After Treatment | 8 Hours After Treatment | 24 Hours After Treatment | |
|---|---|---|---|---|---|
| Group 1 (n = 11) | |||||
| Heart rate | 125 ± 10 | 122 ± 16 | 113 ± 19 | 118 ± 18 | 116 ± 25 |
| Systolic BP | 114 ± 13 | 107 ± 12 | 107 ± 12 | 111 ± 10 | 107±8 |
| Diastolic BP | 62 ± 8 | 56 ± 9 | 59 ± 5 | 62 ± 12 | 58 ± 13 |
| Pain score | 3.7 ± 3.2 | 3.4 ± 3.1 | 1.7 ± 2.1 | 2.9 ± 2.2 | 3.1 ± 2.8 |
| Group 2 (n = 7) | |||||
| Heart rate | 120 ± 39 | 115 ± 38 | 115 ± 42 | 112 ± 35 | 118 ± 26 |
| Systolic BP | 117 ± 24 | 109 ± 12 | 115 ± 16 | 110 ± 11 | 118 ± 25 |
| Diastolic BP | 63 ± 20 | 55 ± 8 | 58 ± 10 | 54 ± 18 | 59 ± 14 |
| Pain score | 2.5 ± 1.9 | 0.3 ± 0.8 | 0.3 ± 0.5 | 0.9 ± 1.5 | 1.6 ± 2.6 |
BP, blood pressure.
aData presented as mean ± SD.
Table 4.
Vital signs and pain scores before and after the second treatment
| Baseline | 2 Hours After Treatment | 4 Hours After Treatment | 8 Hours After Treatment | 24 Hours After Treatment | |
|---|---|---|---|---|---|
| Group 1 (n = 11) | |||||
| Heart rate | 120 ± 16 | 119 ± 14 | 115 ± 16 | 113 ± 18 | 109 ± 17 |
| Systolic BP | 115 ± 9 | 107 ± 11 | 107 ± 11 | 113 ± 9 | 113 ± 10 |
| Diastolic BP | 69 ± 13 | 59 ± 14 | 65 ± 12 | 65 ± 13 | 69 ± 11 |
| Pain score | 3.6 ± 2.7 | 2.0 ± 1.9 | 2.2 ± 2.0 | 2.1 ± 1.7 | 3.2 ± 2.5 |
| Group 2 (n = 5) | |||||
| Heart rate | 118 ± 29 | 118 ± 38 | 119 ± 44 | 125 ± 36 | 123 ± 38 |
| Systolic BP | 114 ± 18 | 105 ± 7 | 104 ± 17 | 97 ± 12 | 111 ± 16 |
| Diastolic BP | 59 ± 13 | 65 ± 10 | 57 ± 13 | 60 ± 12 | 71 ± 7 |
| Pain score | 0.2 ± 0.4 | 0.68 ± 1.1 | 0.8 ± 1.8 | 0.4 ± 0.9 | 1.8 ± 2.5 |
BP, blood pressure.
aData presented as mean ± SD.
Narcotic Usage
Data are presented for morphine PCA usage for group 1 before and after the first acupuncture treatment only because most patients were transitioned from the PCA to oral narcotics by the second acupuncture treatment. We observed the maximal decrease in morphine usage during the time interval 4–8 hours after acupuncture treatment (Table 5).
Table 5.
Morphine use (mg/kg/hr) before and after acupuncture the first session in group 1a
| 2 Hours Before Treatment (Baseline) | 0–4 Hours After Treatment | 4–8 Hours After Treatment | 8–12 Hours After Treatment | 12–24 Hours After Treatment | |
|---|---|---|---|---|---|
| Mean | 0.04 ± 0.02 | 0.03 ± 0.02 | 0.02 ± 0.02 | 0.03 ± 0.02 | 0.03 ± 0.01 |
| Difference from baseline | −0.01 ± 0.01 | −0.01 ± 0.02 | −0.01 ± 0.01 | −0.00 ± 0.01 |
Data presented as mean ± SD.
For Future Randomized Clinical Trials
We used the data from group 1, session 1 for the following estimates because group 1 was comprised of similar surgical patients and because pain was more likely to be greater before session 1 than before session 2. Here, the descriptive data (mean ± sd) were –2.0 ± 3.29 for the 0–4 hours change in pain score and –0.011 ± 0.017 for the baseline to 4–8 hours change in morphine use (mg/kg/ hr). Using these data and assuming a 5% type I error rate, a randomized controlled trial with 43 subjects per group would have 80% power to detect a two-point decrease in pain score 4 hours after acupuncture and a 0.01 mg/kg/hr decrease in morphine usage 4–8 hours after acupuncture.
Interview Results
All parents completed follow-up interviews. Fourteen parents (70%) and 11 patients (69%) said they thought the acupuncture helped the child's pain. Only one parent and one child (of the same family) said that the acupuncture did not help the pain but believed it to be beneficial in other ways. In addition, 18 parents (90%) and 11 patients (60%) said they would consider getting future acupuncture treatment. None of the respondents said they would refuse acupuncture treatment in the future. Seventeen parents (85%) would pay out of pocket for acupuncture if not covered by insurance. Two parents said the reason they would not pay out pocket for acupuncture was because they could not afford it. When asked how much they would be willing to pay per treatment, eight (47%) would pay $20–$40, six (35%) would pay $41–$60, two (12%) would pay $61–80, and one (6%) would pay $81–100.
Parental Comments
Positive Comments
In addition to answering follow-up interview questions, parents said, “acupuncture was very relaxing” for the child, and “it helped her (the child) so much, calmed her down, and made her relax a bit. It helped her with pain substantially, helped her sleep, it was soothing.” Other parents said, “(acupuncture) relaxed him. It knocked him out,” “she was relaxed, it seemed soothing to her,” and “it helped her to relax and be more content . . . she was laying there calm.” Two parents commented on the “calming effect” of the licensed acupuncturist.
One parent commented that her child slept better on the days she received acupuncture and that she had “bad nights” on days she did not. Two parents reported that their children were “confused” and “had hallucinations” with the analgesic/ sedative medications but were “coherent” and “relaxed” after acupuncture. The parent of a patient who received the non-needling form of acupuncture said that he continued to stroke his son along the same meridians as the acupuncturist and said it helped his son to relax.
One parent said “before the first session, she did not sleep for more than 15 minutes at a time but by the third needle, she was sound asleep for 2½ hours straight. When she woke up, she felt calm and so much better. She slept better that night than she slept any other night. She was excited about acupuncture. She liked it a lot and did not feel the needles. She kept asking ‘Am I going to get more acupuncture?’ It was the best part of the hospital experience. It helped her more than anything anybody did. It bothers me that they stick drugs onto kids when there are other things that work. It helped more than morphine. I think if she had a choice between pushing the (PCA) button or acupuncture, she would have chosen acupuncture.”
Unequivocal/Negative Comments
Parents suggested “more and longer sessions,” “three sessions instead of two,” and one said, “a longer session would have probably felt better.” Parents also commented on the timing of acupuncture with suggestions to have acupuncture “later after surgery, instead of immediately after surgery,” “when (our child) was transitioning to oral pain medicines,” and “a few days after surgery.”
Patient Comments
All the patients who were verbal said that they felt minimal to no discomfort with acupuncture needling. Some patients said, “it did not hurt” or “it did not hurt at all” whereas others said they felt a little “poke” but it did not hurt overall. One child said, “it felt weird when the needles went in . . . it felt good and relaxing . . . if other kids do not try it, they're babies because it doesn't hurt.” Patients said acupuncture “helped the pain a lot” and “made the pain go away.” They also said the treatment was “relaxing,” “very relaxing,” “it really works and it makes you really relaxed. It is different from pain medicine because it's relaxing, too,” and “it is definitely relaxing and other kids should definitely try it.” Others said, “it made me calm and sleepy. It works really well” and “it was calming and nice. It is relaxing and calms you down. It's cool.” The only patient who said that the acupuncture did not help the pain said, “It did not help the headache but helped me relax and feel better about the hospitalization. It gave me a tingling, relaxing feeling all over my body, especially on the arms and legs. It was nice.”
Patients suggested “longer and more sessions,” sessions to last “20 minutes instead of 15 minutes” and “10–15 minutes longer,” and to have three, four, and seven instead of two acupuncture sessions.
DISCUSSION
The study shows that acupuncture is highly accepted and well tolerated by children and parents for acute postoperative pediatric pain control in the hospital setting. Earlier studies found that acupuncture may be an effective adjunctive therapy for chronic pain in pediatric patients (21, 22, 24, 32). To date, there are few studies on acupuncture in acute postoperative pain in children in the hospital setting. To our knowledge, this is the first published study to evaluate the role of acupuncture in postoperative pain management in children in the intensive care unit. We observed no adverse side effects. Only one patient withdrew because of possible needle discomfort. We also observed decreasing trends in heart rate, blood pressure, pain score, and narcotic usage posttreatment that may indicate acupuncture has a maximal therapeutic effect at 4 hours that wanes by 24 hours.
Although our study focused on the role of acupuncture in acute pediatric pain control, we found that acupuncture may have other beneficial effects. On the basis of our interviews, acupuncture may encourage relaxation, promote sleep, and help children cope positively with the hospitalization. These effects need to be studied further in future clinical trials.
Our study is limited by the small sample size and the lack of control group. Therefore, we could not control for confounding factors, such analgesic and sedative medication. Patients were treated with analgesic and sedative medications on an individualized basis instead of a standardized treatment protocol. The implementation of a standardized pain management protocol in future studies would include an algorithm for determining the type and amount of analgesic, as well as if acupuncture is needed, based on the patient's pain score. For example, patients with pain scores of 3 or lower may not require narcotic medication. However, it is crucial to complete a preliminary study such as ours to determine acceptability and feasibility of acupuncture in hospitalized children with acute pain before designing a randomized, controlled clinical trial.
A further limitation was that pretreatment measurements of physiologic parameters used were done immediately before acupuncture. Children, especially before the first treatment, may have elevated heart rate and blood pressure from anticipatory anxiety that is not reflective of their underlying pain. Although we measured the vital signs and pain scores at 2 hours pretreatment, they are not truly baseline measurements because they lack adequate proximity to the intervention. For future studies, it may be prudent to take baseline measurements less than an hour before acupuncture.
There are few studies regarding the use of acupuncture for acute pain control in children (11) and on the utility of this therapy in the hospitalized pediatric population. Widespread acceptance of acupuncture as an adjunctive therapy to treat acute pain in children requires well-designed randomized controlled trials. Here, we provide valuable data to design such future studies in hospitalized children with acute pain.
CONCLUSIONS
Acupuncture may be a potentially useful adjunctive treatment for acute pediatric pain management. Our study showed that acupuncture is both feasible and highly accepted by parents and children for the treatment of acute pain, particularly postoperative pain, in hospitalized pediatric patients. There is a probable therapeutic effect at approximately 2–8 hours after acupuncture that wanes by 24 hours after the intervention, and it may be reproducible with subsequent acupuncture sessions. Adequately powered randomized controlled studies are necessary to evaluate the role of repeated and prolonged acupuncture sessions as a complementary therapy for acute pain control in hospitalized children.
Figure 2.
Liver 3 (Taichong).
Figure 3.
Urinary bladder 60 (Kunlun).
ACKNOWLEDGMENT
We would like to thank Kenneth X. Probst for his illustrations.
Supported, in part, by NIH grant M01-RR01271, Children's Hospital and Research Center Oakland, Pediatric Clinical Research Center. This study was performed at Children's Hospital and Research Center Oakland.
Footnotes
The authors have not disclosed any potential conflicts of interest.
REFERENCES
- 1.Ellis JA, O'Connor BV, Cappelli M, et al. Pain in hospitalized pediatric patients: How are we doing? Clin J Pain. 2002;18:262–269. doi: 10.1097/00002508-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 2.McClain BC. Measurement of pain in children: State-of-the-art considerations. Anesthesiology. 2002;96:523–526. doi: 10.1097/00000542-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Johnston CC, Abbott FV, Gray-Donald K, et al. A survey of pain in hospitalized patients aged 4–14 years. Clin J Pain. 1992;8:154–163. doi: 10.1097/00002508-199206000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Cummings EA, Reid GJ, Finley GA, et al. Prevalence and source of pain in pediatric inpatients. Pain. 1996;68:25–31. doi: 10.1016/S0304-3959(96)03163-6. [DOI] [PubMed] [Google Scholar]
- 5.Palermo TM, Drotar DD, Lambert S. Psychosocial predictors of children's postoperative pain. Clin Nurs Res. 1998;7:275–291. doi: 10.1177/105477389800700305. [DOI] [PubMed] [Google Scholar]
- 6.Howard RF. Current status of pain management in children. JAMA. 2003;290:2464–2469. doi: 10.1001/jama.290.18.2464. [DOI] [PubMed] [Google Scholar]
- 7.Chambliss CR, Anand KJ. Pain management in the pediatric intensive care unit. Curr Opin Pediatr. 1997;9:246–253. doi: 10.1097/00008480-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Schechter NL. The undertreatment of pain in children: An overview. Pediatr Clin North Am. 1989;36:781–794. doi: 10.1016/s0031-3955(16)36721-9. [DOI] [PubMed] [Google Scholar]
- 9.Anand KJ, Carr DB. The neuroanatomy, neurophysiology, and neurochemistry of pain, stress, and analgesia in newborns and children. Pediatr Clin North Am. 1989;36:795–822. doi: 10.1016/s0031-3955(16)36722-0. [DOI] [PubMed] [Google Scholar]
- 10.Anand KS. Relationships between stress responses and clinical outcome in newborns, infants, and children. Crit Care Med. 1993;21(Suppl 9):S358–S359. doi: 10.1097/00003246-199309001-00035. [DOI] [PubMed] [Google Scholar]
- 11.Rusy LM, Weisman SJ. Complementary therapies for acute pediatric pain management. Pediatr Clin North Am. 2000;47:589–599. doi: 10.1016/s0031-3955(05)70227-3. [DOI] [PubMed] [Google Scholar]
- 12.Golianu B, Krane EJ, Galloway KS, et al. Pediatric acute pain management. Pediatr Clin North Am. 2000;47:559–587. doi: 10.1016/s0031-3955(05)70226-1. [DOI] [PubMed] [Google Scholar]
- 13.Lee AC, Highfield ES, Berde CB, et al. Survey of acupuncturists: Practice characteristics and pediatric care. West J Med. 1999;171:153–157. [PMC free article] [PubMed] [Google Scholar]
- 14.Kemper KJ. Complementary and alternative medicine for children: Does it work? Arch Dis Child. 2001;84:6–9. doi: 10.1136/adc.84.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kemper KJ, Cassileth B, Ferris T. Holistic pediatrics: A research agenda. Pediatrics. 1999;103(4 Pt 2):902–909. [PubMed] [Google Scholar]
- 16.Lin Y, Lee A, Kemper K, et al. Integrating complementary and alternative medicine in pediatric pain management. Anesthesiology. 1999;91:939. [Google Scholar]
- 17.Helms JM. Acupuncture Energetics: A Clinical Approach for Physicians. First Edition Medical Acupuncture Publishers; Berkeley, CA: 1995. [Google Scholar]
- 18.NIH Consensus Conference. Acupuncture. JAMA. 1998;280:1518–1524. [PubMed] [Google Scholar]
- 19.Ernst E. Acupuncture—A critical analysis. J Intern Med. 2006;259:125–137. doi: 10.1111/j.1365-2796.2005.01584.x. [DOI] [PubMed] [Google Scholar]
- 20.Nasir LS. Acupuncture. Prim Care. 2002;29:393–405. doi: 10.1016/s0095-4543(01)00007-0. [DOI] [PubMed] [Google Scholar]
- 21.Kemper KJ, Sarah R, Silver-Highfield E, et al. On pins and needles? Pediatric pain patients’ experience with acupuncture. Pediatrics. 2000;105(4 Pt 2):941–947. [PubMed] [Google Scholar]
- 22.Zeltzer LK, Tsao JC, Stelling C, et al. A phase I study on the feasibility and acceptability of an acupuncture/hypnosis intervention for chronic pediatric pain. J Pain Symptom Manage. 2002;24:437–446. doi: 10.1016/s0885-3924(02)00506-7. [DOI] [PubMed] [Google Scholar]
- 23.Lin YC, Ly H. Acupuncture and needlephobia: The pediatric patient's perspective. Acupunct Med. 2003;14:15–16. [Google Scholar]
- 24.Pintov S, Lahat E, Alstein M, et al. Acupuncture and the opioid system: Implications in management of migraine. Pediatr Neurol. 1997;17:129–133. doi: 10.1016/s0887-8994(97)00086-6. [DOI] [PubMed] [Google Scholar]
- 25.Lin YC, Ly H, Golianu B. Acupuncture pain management for patients with cystic fibrosis: A pilot study. Am J Chin Med. 2005;33:151–156. doi: 10.1142/S0192415X05002758. [DOI] [PubMed] [Google Scholar]
- 26.Ida B. Japanese Acupuncture, A Clinical Guide. Paradigm Publications; Brookline: 1998. [Google Scholar]
- 27.Fukishima K. Meridian Therapy. Toyo Hari Medical Association; Toyko: 1991. [Google Scholar]
- 28.Deadman P, Al-Khafaji M, Baker K. A Manual of Acupuncture. East Sussex, England, Journal of Chinese Medicine Publications. 2001 [Google Scholar]
- 29.Delaney C, Leonard D, Kitsch L. The Acupuncture Point Book. Roast Duck Production; Santa Cruz, CA: 1988. [Google Scholar]
- 30.Birch S. Shonishin: Japanese pediatric acupuncture. Eur J Orient Med. 2002;3(Part 6):4–10. [Google Scholar]
- 31.Brislin RP, Rose JB. Pediatric acute pain management. Anesthesiol Clin North Am. 2005;23:789–814. doi: 10.1016/j.atc.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 32.Lin YC, Bioteau AB. Pediatric medical acupuncture service.. 55th Annual Meeting of the American Society of Anesthesiologists.; Orlando, FL. 2002 October 16. [Google Scholar]