Abstract
Background
Primary care providers (PCP) are the entry point for public sector depression treatment for many Latino patients. However, many Latino patients do not initiate their PCPs’ recommended treatment, which likely contributes to ethnic disparities in depression treatment. This study examined factors related to Latino patients’ uptake of their PCPs’ recommendations for depression treatment.
Method
Ninety Latino primary care patients who received a depression treatment recommendation from their PCP participated in a telephone interview. Patients rated their working alliance with their PCPs and their PCPs’ cultural competence. They also reported their treatment preference, the type of recommendation, and their intended and actual uptake of the recommendation. Patients were contacted at two time points (Time 1: M = 14 days after PCP appointment; Time 2: M = 84 days after PCP appointment) to report their uptake status.
Results
At Time 1, 23% of patients had initiated uptake of the treatment recommendation, increasing to 53% at Time 2. Patients who received a medication recommendation were more likely to have followed though on the recommendation, compared to patients who received a psychotherapy recommendation. The working alliance was positively associated with intention to follow up on a treatment recommendation, and also mediated the relationship between cultural competence and intention of following up on the recommendation.
Conclusion
PCP’s treatment recommendation and the PCP – patient alliance play a role in Latino primary care patients intention to follow a treatment recommendation for depression. An improved understanding of this role could enhance efforts to improve depression treatment uptake.
Keywords: Latino/Hispanic, Depression Treatment, Primary Care, Treatment Disparities
Introduction
Depression is the fourth leading cause of disability in the United States (Michaud et al., 2006), and is projected to become the leading cause of disability within 15 years (McKenna, Michaud, Murray & Marks, 2005), with sixteen per cent of the general population expected to experience a major depressive episode during their lifetime (Kessler et al., 2003). Despite the availability of numerous efficacious treatments for depression (Arroll et al., 2005; Cuijpers et al., 2011; Cuijpers et al., 2010), only slightly more than 50% of those who are depressed receive treatment (Kessler et al., 2003).
The underutilization of depression treatment is of particular concern among Latinos, because Latinos comprise a significant proportion of the United States population, and because the Latino population faces disproportionate economic disadvantage, a known risk factor for depression (Muntaner, 2004). Latinos comprise 16% of the U.S. population today, and are expected to comprise 30% of the population by 2060 (U.S. Census Bureau, 2012). They are among the most socioeconomically disadvantaged groups in the United States, with 23% of Latinos living in poverty, compared with 11.6% of non-Hispanic whites (U.S. Census Bureau, 2013), and a declining median income (Taylor, Kochhar, Fry, Velasco, & Motel, 2011).
Overall, Latinos exhibit rates of depression comparable to those found among non-Latino whites (H. González et al., 2010; Mendelson, Rehkopf, & Kubzansky, 2008), but they utilize depression treatment far less frequently than the general population, with only 36% receiving treatment for past-year depression (Alegría et al., 2008a). This low rate persists despite evidence that various depression treatments are effective for Latinos (Miranda et al., 2003; Sanchez-Lacay et al., 2001; Wells, et al., 2004).
There are likely numerous explanations for this underutilization, including poverty, lack of access or insurance, underdiagnosis, stigma, negative attitudes toward treatment, and preference for informal support services among some Latinos groups (Alegria, Perez, & Williams, 2003; Cardemil et al., 2007; Cooper et al., 2003; Interian, Martinez, Guarnaccia, Vega, & Escobar, 2007; Ortega & Alegría, 2002; Sclar, Robison, & Skaer, 2008). An additional, unexamined explanation for this unmet need may be found by looking at potential disruptions to the depression referral pathways. Many patients experiencing symptoms of depression seek treatment from their primary care provider (PCP), rather than a mental health specialist (Uebelacker, Wang, Berglund, & Kessler, 2006; Wang et al., 2006; Wells, Klap, Koike, & Sherbourne, 2001). As the provider who frequently diagnoses, prescribes, and recommends treatment for depression, the PCP is thus instrumental in connecting patients with the necessary care.
Depression Treatment and Primary Care
There are a number of compelling reasons to investigate the uptake of depression treatment recommended by PCPs. First, as many as 22% of Latino primary care patients meet criteria for major depressive disorder (Olfson, Marcus, & Druss, 2000). PCPs are frequently called upon to assess depression and provide psychopharmacologic treatment for their depressed patients. In fact, they are the most common prescribers of antidepressant medications, providing 80% of all prescriptions for antidepressants (Moitabai & Olfson, 2008).
Second, despite increased screening and attention to depression in primary care (O’Connor, Whitlock, Bell, & Gaynes, 2009), many Latino patients who are referred from primary care to specialty mental health care do not follow up on the referral (De Figueiredo, Boerstler, & Doros, 2009; Miranda & Cooper, 2004). Lack of uptake may be due to a number of factors, including logistical difficulties such as transportation or scheduling around multiple jobs (Sánchez-Lacay et al., 2001), attitudinal factors such as discomfort with the diagnosis (Byrne, Regan, & Livingston, 2006), stigma about antidepressants (Interian et al., 2007), and inadequate provider supply (U.S. Department of Health and Human Services, 2011).
Third, cultural factors may affect how Latino patients perceive the PCP recommendation for depression treatment. For example, many Latinos view their PCPs as authority figures who deserve respect and should also reciprocate this respect to the patient (Flores, Abreu, Olivar & Kastner, 1998). Because of this perceived authority, PCPs’ treatment recommendations may be particularly influential for Latino patients. When treatment recommendations are made in a way that honors cultural values, it is possible that even reluctant patients may be willing to try depression treatment (Ishikawa, Cardemil, & Falmagne, 2010). Finally, emerging research has suggested that aspects related to the PCP-patient relationship, including perceived competence, trustworthiness, and openness of the PCP (Cabassa & Zayas, 2007; Kravitz et al., 2011), and effective communication between patient and PCP (Alegría et al., 2008b), may also positively influence referral uptake among Latinos.
The PCP – Patient Working Alliance and PCP Cultural Competence
This paper examines two relational variables: the PCP – patient working alliance, and PCP cultural competence. Bordin (1979) defined the working alliance as (1) agreement on treatment goals, (2) agreement on tasks, and (3) the bonds of trust and liking between clinician and patient. Research has shown that a positive working alliance predicts a range of positive outcomes in mental health care, among which treatment adherence is the most relevant to the current study (Horvath & Symonds, 1991; Julius, Novitsky, & Dubin, 2009; Martin, Garske, & Davis, 2000). For example, in Fuertes’ (2007) research among patients with chronic medical illness, the PCP – patient working alliance was significantly correlated with perceived treatment utility and treatment adherence. Julius and colleagues (2009), in a meta-analysis of the medication adherence research, identified strengthening the working alliance as one of the critical strategies for increasing adherence rates.
Cultural competence has been defined as “the ability to engage in actions or create conditions that maximize the optimal development of the client and client systems‖achieved by the counselor’s acquisition of awareness, knowledge, and skills needed to function effectively in a pluralistic democratic society” (Sue & Torino, 2005; p. 8). Bhui and colleagues (2007) showed that most models for culturally competent mental healthcare delivery do in fact share a number of features, including the development of knowledge of other cultures, awareness of the impact of culture on attitudes, expressions of distress, and help-seeking, and skills to manage language differences and interact within different belief systems. It may be that when treatment is administered in a culturally appropriate way, ethnic minority patients are more likely to stay in treatment. The treatment adherence literature suggests that culturally competent care may be associated with patients’ decisions to remain in treatment. There is evidence of this association both from mental health settings (La Roche, D'Angelo, Gualdron, & Leavell, 2006; Lieu et al., 2004) and medical settings (Fuertes et al., 2009), supporting the notion that culturally competent care may increase the likelihood of patient adherence to treatment recommendations.
Treatment Preference and Recommendation Type
This study also examined associations among patient treatment preference, the type of treatment recommendation (i.e., medication, psychotherapy, or combined medication and psychotherapy), and uptake of the treatment recommendation. A salient question is whether the type of referral provided by the PCP influences patient uptake of the treatment recommendation. A large body of research has shown a general preference among Latinos for psychotherapy, compared with medication (Cabassa, 2007; Dwight-Johnson et al., 2010; Fernandez Y Garcia, Franks, Jerant, Bell, & Kravitz, 2011; Interian et al., 2007). Research has shown that matching treatment type to patient preference improves treatment outcomes (Lin et al., 2005). It would follow that patients who prefer a certain modality and receive a treatment recommendation for that modality might have higher rates of uptake than patients who prefer one modality but receive a recommendation for a different type of treatment. Thus, when considering whether treatment preference would correlate with treatment uptake among Latinos, the research would imply greater uptake of psychotherapy, compared with antidepressant medication.
However, whether the type of referral influences patient uptake of the treatment recommendation involves consideration not only of treatment preference but of treatment access. That is, utilization demands a sufficient availability and accessibility of the preferred treatment. While psychotherapy may be the preferred treatment for many patients, logistical barriers might make psychotherapy more difficult to access, compared with obtaining a prescription for antidepressants. Difficulty accessing specialty mental health services is a well-known barrier to care for Latino patients, particularly Latinos with limited English proficiency (Biever, Gómez, González, & Patrizio, 2011). Problems accessing specialty mental health care may partially explain the finding that Latinos prefer to be treated in primary care, as opposed to specialty care (Dwight-Johnson et al., 2010). Treatment in primary care provides readily available treatment, most commonly in the form of antidepressant medication. Thus, compared with psychotherapy, medication may be more accessible for many Latinos seen in primary care, making it a “default” treatment, even when psychotherapy might in theory be preferable. Understanding patterns of actual treatment uptake therefore requires awareness of the logistic constraints of the particular clinical setting that may supersede consideration of a hypothetical query into patient preference. To better understand the influence of treatment preference and recommendation type, this study examined how these two variables are associated with uptake of the treatment recommendation.
Study Objectives
The purpose of this research was to examine factors that contribute to the intended and actual uptake of depression treatment recommendations among Latino primary care patients with elevated depression symptoms. In this study, “treatment recommendation” refers to either referral from the PCP for psychotherapy or psychopharmacologic treatment.
Four hypotheses were investigated: (1) the PCP-patient working alliance and PCP cultural competence will be positively associated with the patient’s intention of following up on a referral; (2) working alliance, cultural competence, and intention of following up on a referral will be directly and positively associated with uptake of the PCP’s treatment recommendation; (3) match between treatment preference and treatment recommendation will be positively associated with uptake of the treatment recommendation; and (4) patients prescribed medication will be more likely to initiate uptake of the recommendation, compared with patients referred to psychotherapy.
Method
Participants and Recruitment
Participants were recruited between March 2010 and June 2011 at a community health clinic in Cambridge, Massachusetts that is part of a public safety net hospital serving a largely low-income and ethnic minority population. Participants were drawn from the pool of primary care patients who had completed the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001) depression screening at an annual physical or new patient visit, per standard clinic protocol. A form requesting consent to be contacted by phone about the study was attached to all English and Spanish language PHQ-9 forms handed out at annual and new patient visits. This form stated that the study was open only to Latino patients. To be eligible for the initial screening call, participants had to have signed the consent to be contacted by phone, and had to have scored at or above the clinical threshold of 10 (range 0–27) on the PHQ-9. A score of 10 corresponds to the lower cut-off for major depressive disorder on the PHQ-9 and is the threshold at which this clinic’s PCPs are advised to consider active therapies. The first author, a fluent Spanish speaker and native English speaker with extensive research interview experience in both English and Spanish, and prior experience working in research and direct social service in the U.S., Mexico, Central, and South America, conducted all of the interviews. During the screening call, patients were evaluated for full study eligibility. In addition to the above criteria, additional eligibility criteria included Latino/Hispanic self-identity, and a recommendation either to begin new depression treatment (medication, psychotherapy, or combined treatment) or to change or supplement an existing treatment (e.g., to switch from psychotherapy to medication, or to add medication to psychotherapy), received from the PCP at the visit at which they filled out the PHQ-9.
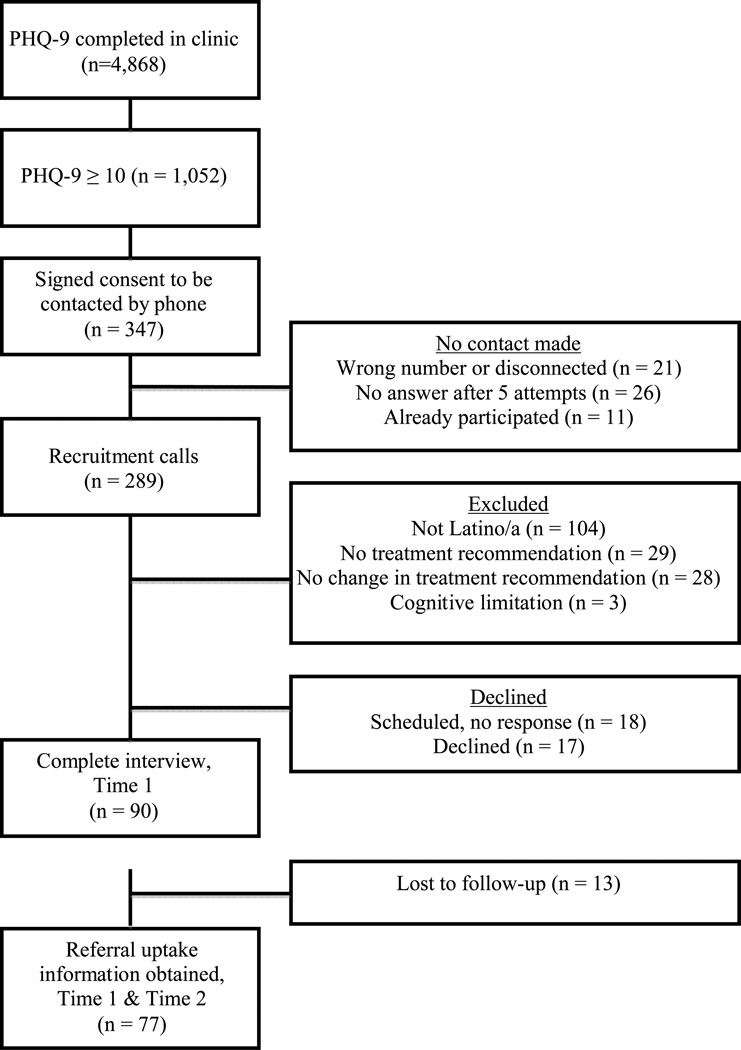
Figure 1 shows the recruitment flow. Of 4,868 patients of any ethnicity who completed the PHQ-9 form, 1,052 (22%) scored 10 or higher. Of these, 347 signed the consent to be contacted by phone, (a 33% overall response rate, although the consent form stipulated only Latino patients were eligible to participate). Of 347 recruitment call attempts, 289 patients were successfully reached, and 90 of these patients agreed to participate and were eligible based on the criteria listed above. Ninety interviews were completed at Time 1 (31% of 289 calls made; M = 14 days after PCP appointment). Of the 90 participants, 21 had completed uptake of the treatment recommendation by the Time 1 interview. Follow-up calls were attempted to the remaining 69 participants at Time 2, resulting in 56 successful calls, (86% follow-up rate; M = 84 days after PCP visit). Thus, Time 2 information was available for a total of 77 participants, with 13 (14%) lost to follow-up.
Figure 1.
Recruitment Flow
Table 1 describes the demographic characteristics of the sample (N = 90). Most of the participants were female and predominantly immigrants, with an average of 16 years living in the United States. The interview was conducted in the language of the participants’ preference, and 71% requested that the interview be conducted in Spanish. The most common places of origin were Central America and Puerto Rico. Nearly half of the sample had obtained less than a high school education. The sample was recruited in Massachusetts, where state law required that all residents have health insurance, and 86% of this sample was insured.
Table 1.
Demographic characteristics of the sample (N = 90)
| % | N | |
|---|---|---|
| Female | 83% | 75 |
| Age (M, SD) | 38.9 (11.2) | |
| Immigrant1 | 93% | 84 |
| If immigrant, years since immigration (M, SD) | 16.3 (9.6) | |
| Region of Origin | ||
| Central America (not including Mexico) | 48% | 43 |
| South America | 20% | 18 |
| Puerto Rico | 20% | 18 |
| Other | 12% | 11 |
| Marital status | ||
| Single | 33% | 30 |
| Married or Civil Union | 44% | 39 |
| Separated or Divorced | 22% | 20 |
| Widowed | 1% | 1 |
| Years of Education | ||
| Less than high school graduate | 48% | 44 |
| Up to high school graduate | 26% | 23 |
| More than high school | 26% | 23 |
| Health insurance | ||
| Insured | 86% | 77 |
| Not insured | 5% | 5 |
| Free care recipient2 | 9% | 8 |
| Spanish language preference for interview | 71% | 64 |
“Immigrant” refers to both immigrant and migrant participants, including Puerto Ricans, who were born outside of the Continental United States.
Free care patients are uninsured but due to inability to pay medical expenses, expenses are paid by the healthcare facility.
Participants were seen by one of 9 PCPs in this group practice, with about 1/3 of the sample seen by one long-term, bilingual PCP. Most of the visits were conducted in Spanish. Sixty-two percent (n = 56) of the participants spoke Spanish directly with their PCP, and 3.3% (n = 3) spoke Spanish through an interpreter. Thirty-one percent (n = 28) spoke English with their PCP, and 7% (n = 6) spoke a mixture of English and Spanish. Of note only 4 of the participants who conducted their PCP appointment in English would have liked to have done so in Spanish, indicating that the language needs of this patient population were largely being met.
Procedures
Participants completed the Time 1, 45-minute telephone baseline interview in English or Spanish, according to their preference. During the interview, participants provided demographic information, information about their recent PCP visit, including the treatment recommendations received, and responded to 8 questionnaires, which were either available in Spanish or translated by a professional translator and native Spanish speaker specializing in Latino healthcare. Participants were compensated with $401. At the conclusion of the interview, participants who had not yet completed uptake of their recommended treatment (n = 69 of the total sample of 90) were asked for verbal permission to contact them at a later date with follow-up questions at Time 2. During the follow-up interview, participants reported whether they had or had not completed uptake of the recommended treatment. All participants provided verbal consent to an Institutional Review Board (IRB)-approved consent form, and the study was approved by the IRBs at Clark University and the Cambridge Health Alliance.
Measures
Primary outcome variable
Uptake of the treatment recommendation. At Time 1 and Time 2, if relevant, patients were asked whether they had completed the treatment recommended to them by their PCP. Participants’ responses were coded as “initiated,” “not initiated,” or “partially initiated.” “Partially initiated” referred to those patients who received a treatment recommendation for combined medication and psychotherapy, but had only initiated either medication or psychotherapy, but not both. Those patients who had received a recommendation for combined treatment and had completed uptake of both medication and psychotherapy were coded as “initiated.” Uptake was only coded as “initiated” if the patient had seen a provider for services, not merely made an appointment.
Intermediate variable
Intention to follow up on a referral for mental health care. This variable was considered an “intermediate” variable, because it was analyzed both as a dependent variable with working alliance and cultural competence as the independent variables, and also as an independent variable with uptake of the treatment recommendation as the dependent variable. An abbreviated version of the Help-Seeking Behavior Scale (HSBS; Addis, 2007), a face-valid measure that assesses help-seeking behavior and intention, was used to assess participants’ intentions of following up on a referral for depression treatment. The original HSBS assesses retrospective behavior as well as prospective expectations about help-seeking to formal and informal sources of support, and is measured on a 4-point Likert scale, ranging from strongly unlikely to strongly likely to seek help. For this study, only the prospective items were included, and the measure was limited to inquiry about intention to seek treatment from four types of health professional (PCP, psychiatrist, psychologist, and social worker/counselor). In addition, the introduction was adapted to inquire about intention to seek treatment in response to a referral provided by the patient’s PCP (e.g., “If your PCP recommended you seek treatment for an emotional, psychological, or interpersonal problem, and recommended you receive that treatment from a psychologist, how likely would you be to seek help from a psychologist?”) The total score for the measure was the sum of the likelihood scores for seeking treatment from each provider. Cronbach’s alpha for this sample was .77.
Predictor variables
Patient ratings of the PCP-patient working alliance. The Physician-Patient Working Alliance Scale (PPWA; Fuertes et al., 2007) is a 12-item measure that assesses patients’ report of the strength of the working alliance between their PCP and themselves (e.g., “My doctor and I agree on the things I need to do to improve my health”). It is scored on a 5-point Likert scale from “strongly disagree” to “strongly agree.” Higher scores indicate patient rating of a stronger working alliance. The PPWA was available in Spanish. Chronbach’s alpha was .90 for this sample.
Patient ratings of PCP cultural competence. The Physician Multicultural Competence Scale (PMCS, Fuertes et al., 2009) is a 9-item measure that assesses participant ratings of their PCP’s cultural competence. It is scored on a 5-point Likert scale from “strongly disagree” to “strongly agree.” This scale measures a patient’s report of the extent to which the PCP who provided them with the treatment recommendation for depression considers how the patient’s and their own beliefs, values, and attitudes inform their communication, clinical presentation, and level of understanding and respect (e.g., “My doctor seems to perceive my problems within the context of my cultural experience, values, and/or lifestyle.”) Higher scores indicate patient rating of higher PCP cultural competence. The PMCS was available in Spanish. For this sample, Chronbach’s alpha was .86.
Additional variables
Participants responded to additional questionnaires to assess a number of additional patient variables shown in the literature to be associated with utilization of depression treatment. These were depression symptomatology (Patient Health Questionnaire (PHQ-9); Kroenke, Spitzer, & Williams, 2001), acculturation (Brief Acculturation Scale for Hispanics (BASH); Norris, Ford, & Bova, 1996), depression self-stigma (Depression Self-Stigma Scale (DSSS); Kanter, Rusch, & Brondino, 2008), and attitudes about depression treatment (Attitudes Towards Seeking Professional Psychological Help – Short Form (ATSPPH-SF); Fischer & Farina, 1995). The PHQ-9, BASH, and ATSPPH-SF were available in Spanish.
In addition, participants were also asked for their age, sex, country of origin, immigrant status (yes/no), years since immigration, marital and educational status, insurance status (yes/no), treatment preference (antidepressant medication or counseling/psychotherapy), treatment uptake status (uptake initiated, uptake not initiated, uptake partially initiated), and language used with their PCP (English/Spanish).
Results
Sample Characteristics
Mean PHQ-9 scores at the Time 1 interview (M = 14 days after PCP appointment) indicated the moderate-severe range of major depression (M = 14.4, SD = 5.6; 10 – 14 = moderate range; 15 – 19 = severe range). Nearly ten times the number of the participants stated a preference for therapy or counseling (72%) over medication for treating depression (7%; X2 (1, n = 71) = 49.02, p < .001); the remaining 11% stated that they had no preference for one treatment over the other. PCP recommendations did not mirror patient preference, with new treatment recommendations being nearly evenly distributed among medication (36%), psychotherapy (41%), and combination therapy (23%; X2(2, n = 90) = 4.47, p = .11).
Uptake of the Treatment Recommendation
At Time 1 (M = 14 days after the PCP appointment) 21 patients (23%) had fully initiated the treatment recommended to them by their PCP. This number included 19 patients who initiated uptake for a single type of treatment and 2 patients who had been recommended combined treatment and who had initiated both psychotherapy and medication. An additional 12 patients (13%) who had been referred to combined treatment had partially initiated uptake, having initiated medication treatment but not psychotherapy. At Time 2 (M = 84 days after the PCP appointment) the sample was 77 patients, with 13 patients having been lost to follow up. By Time 2, a total of 41 patients (53% of the sample of 77) had fully initiated the treatment recommended to them by their PCP. This included 32 patients who had initiated uptake for a single type of treatment and 9 patients who had been referred to combined treatment and had initiated both psychotherapy and medication. An additional 4 patients (5%) who had been referred to combined treatment had partially initiated uptake, having initiated medication treatment but not psychotherapy. This represents a significant increase in full initiation of treatment uptake from Time 1 to Time 2, X2(1, n = 90) = 14.65, p < .001.
Twenty-two patients had been receiving prior mental health treatment when they received their new treatment recommendation from their PCP. Of these, 4 had been receiving therapy and were recommended to begin supplemental medication, and 18 had been receiving medication and were recommended to begin supplemental therapy. Because uptake rates among those receiving a recommendation for supplemental treatment did not differ statistically from the sample receiving a recommendation for new treatment at Time 1 or Time 2, patients receiving a recommendation for supplemental treatment were included in the overall sample.
Preliminary Analyses
Preliminary analyses showed that participant’s age was positively correlated with ratings of their provider’s cultural competence (r = 0.33, p < .05), and immigrants were shown to have significantly higher mean ratings of working alliance (t = 2.37, p < .05) and of cultural competence (r = 2.04, p < .05). Acculturation was negatively correlated with working alliance (r = −0.24, p < .05) indicating that patients more oriented toward Latino culture had higher ratings of the working alliance. Ratings of working alliance and cultural competence were highly correlated with each other (r = .77, p < .01), and ordinal regression analysis showed that attitude toward depression treatment was positively associated with intention to follow up on a referral (Est = 1.15 (0.05), Wald = 0.97, p < .01). No other associations were found between demographic variables, other patient variables, and the study variables. Thus, age, immigrant status, acculturation, and attitudes toward depression treatment were entered into all subsequent regression models. The conservative strategy of controlling for covariates associated with independent as well as dependent variables is used to better control for bias in the analysis (Yzerbyt, Muller, & Judd, 2004).
Hypothesis 1: Working alliance and cultural competence will be positively associated with intention of following up on a referral
To test Hypothesis 1, which predicted that working alliance and provider cultural competence would be associated with the patient’s intention of following up on the PCP’s referral, ordinal regressions were conducted, with intention to follow up on a referral as the outcome variable. Working alliance and cultural competence were the predictor variables, controlling for relevant covariates. The summed scores for the 4 items (ranging from 6 – 16) were transformed into a 4-point ordinal scale that corresponded to the individual 4-point scale for each item, as follows: 6 – 7 = 1; 8 – 10 = 2; 11 – 13 = 3; 14 – 16 = 4.
Results of the ordinal regressions are shown in Table 2. Immigration status, age, acculturation, and attitude toward treatment were entered as covariates in Step 1. In Step 2, cultural competence was added to the model, and working alliance was added in Step 3. Among the covariates, only attitude toward treatment was significantly associated with intention of following up on a referral. When controlling for immigration status, age, acculturation, and attitudes about depression treatment, cultural competence and working alliance were each positively associated with intention to follow up on a depression treatment referral.
Table 2.
Ordinal regression showing the association between cultural competence, working alliance, and intention of following up on a referral from the PCP (N = 891)
| Est (SE) | Wald | 95% CI | OR | Pseudo R2 (range of 3 values) |
|||
|---|---|---|---|---|---|---|---|
| Upper | Lower | ||||||
| Step 1: | Age | 0.01 (0.02) | 0.13 | −0.03 | 0.04 | ||
| Immigrant status | 0.40 (0.74) | 0.29 | −1.05 | 1.85 | |||
| Acculturation | 0.03 (0.04) | 0.47 | −0.06 | 0.12 | |||
| Attitudes to treatment | 0.15 (0.05) | 10.89** | 0.06 | 0.24 | 1.16 | 0.06 – 0.13 | |
| Step 2: | Cultural competence | 0.10 (0.04) | 6.00* | 0.02 | 0.02 | 1.11 | 0.09 – 0.22 |
| Step 3: | Working alliance | 0.19 (0.06) | 8.49** | 0.06 | 0.31 | 1.20 | 0.14 – 0.30 |
N =89 for this variable because one questionnaire was incomplete
p < .05.
p < .01.
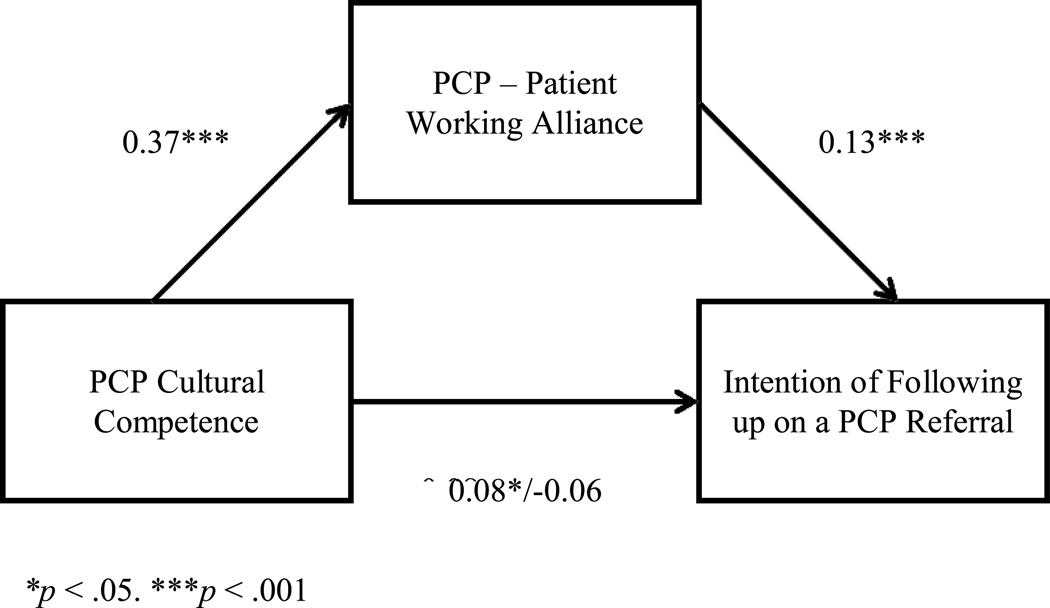
Although cultural competence was significantly associated with intention to follow up on a referral in Step 2, without working alliance in the model, when working alliance was added to the model in Step 3, cultural competence no longer showed a significant association with intention of following up on a referral (Est = −0.055 (0.06), Wald = 0.74, p = .39). To better understand this finding, a mediational analysis was conducted following Baron and Kenny’s (1986) procedure to assess whether working alliance mediated the effect of cultural competence on intention to follow up on a referral from the PCP. As shown in Figure 2, there is strong evidence for the mediating role of working alliance in the relationship between cultural competence and intention to follow up on a referral from the PCP. A partial mediation effect was supported by the Sobel test (Preacher and Leonardelli, 2001; z = 2.79, p < .01), suggesting that the association between cultural competence and intention to follow up on a referral to ones’ own PCP is partially accounted for by the working alliance (Kenny, 2012).
Figure 2.
Mediational model showing PCP – patient working alliance as a partial mediator of the association between PCP cultural competence and intention of following up on a referral from the PCP.
Hypothesis 2: Working alliance, cultural competence, and intention of following up on a referral will be positively associated with uptake of the PCP’s treatment recommendation at Time 1 and Time 2
Since working alliance and cultural competence were shown to be significantly associated with intention to follow up on a referral from the PCP, the next analyses examined whether intention to follow up on a referral was associated with actual uptake of the treatment recommendation, and whether working alliance and cultural competence were directly associated with actual uptake. Hypothesis 2 predicted that the working alliance, cultural competence, and intention of following up on a referral would be associated with uptake of the treatment recommendation at Time 1 and Time 2. Multivariate logistic regressions were conducted, with uptake of the treatment recommendation at Time 1 and Time 2 as the dependent variable, and intention to follow up on a referral, working alliance, and cultural competence as the independent variables. The model controlled for relevant covariates (i.e. age, immigration status, acculturation, and attitudes toward treatment).
Possible response categories for uptake of the treatment recommendation were “initiated,” “not initiated,” or “partially initiated.” “Not initiated” was the reference category. Age, immigration status, acculturation, and attitudes toward treatment were entered in Step 1, cultural competency was entered in Step 2, and working alliance was entered in Step 3. Intention to follow up on a referral from the PCP, the outcome variable from the previous analysis, was entered as an independent variable in Step 4. Working alliance and cultural competence were not directly associated with uptake in Steps 2 and 3, and the overall fit of the model was not significant at Time 1, X2(14, n = 90) = 17.04, p = .25 or Time 2, X2(14, n = 77) = 11.38, p = .60.
In order to eliminate the possible confounding effects of access to care, which would be more pronounced for psychotherapy compared with medication, a bivariate regression was conducted among only those referred to medication. The association was not significant, but there was a positive trend associating higher ratings of intention with greater odds of completing treatment uptake, among those prescribed medication, X2(1, n = 32) = 2.95, p = .09.
Hypothesis 3: Match between treatment preference and recommendation type will be positively associated with uptake of the treatment recommendation
The next set of analyses examined the associations between treatment preference match and type of treatment recommendations and uptake of the treatment recommendation. Hypothesis 3 predicted that when patients’ treatment preference (psychotherapy or medication) matched the treatment recommended to them by their PCP, they would be more likely to initiate treatment uptake compared to patients for whom treatment preference did not match the recommendation type. Only patients who indicated a definitive treatment preference (i.e., medication or psychotherapy, excluding those who selected “no preference”) and who received a recommendation for a single treatment (i.e., medication or psychotherapy, but not combined treatment) were included in the analysis, giving n = 53 at Time 1 and n = 44 at Time 2. A dummy variable, “preference match” was computed for this analysis. This variable was coded as “1” if a patient who preferred therapy was referred to therapy, or if a patient who preferred medication was referred to medication. The variable was coded as “0” if the patient preferred therapy and was referred to medication, or vice versa.
Fisher’s exact tests were conducted for preference match and uptake of the treatment recommendation at Time 1 and Time 2. There was a significant association between the preference match and uptake at Time 1, p < .01 and Time 2, p < .05. However, this association was not in the expected direction. As shown in Table 3, a greater proportion of non-matched treatment recommendations initiated uptake, compared with treatment recommendations that matched treatment preference. This is due to the fact that there was proportionally greater uptake among medication recommendations, nearly all of which fell into the “non-match” category.
Table 3.
Uptake of the treatment recommendation by preference match and type of recommendation
| Time 1 uptake (n = 53; M = 14 days after PCP appointment) |
Time 2 uptake (n = 44: M = 84 days after PCP appointment) |
Time 2 uptake (%) |
|||
|---|---|---|---|---|---|
| Initiated (n) |
Not initiated (n) |
Initiated (n) |
Not initiated (n) |
||
| Preference match | |||||
| Medication | 2 | 0 | 2 | 0 | 100% |
| Psychotherapy | 0 | 26 | 8 | 15 | 53% |
| No preference match | |||||
| Medication | 11 | 12 | 14 | 3 | 82% |
| Psychotherapy | 0 | 2 | 0 | 2 | 0% |
Nearly all of the psychotherapy referrals fell into the “match” category, but there were proportionally fewer psychotherapy uptakes compared with medication uptakes. This indicates that patients who preferred psychotherapy and were recommended psychotherapy were less likely to access treatment, compared to patients recommended medication.
Hypothesis 4: Patients prescribed medication will be more likely to initiate uptake of the recommendation, compared with patients referred to psychotherapy
The final hypothesis predicted that, despite the overwhelming preference for psychotherapy in this sample, patients referred to medication would have greater uptake rates due to the greater ease of access in obtaining medication prescriptions. Table 4 shows referral uptake at Time 1 and Time 2, grouped by referral type. First, frequencies of uptake initiation were assessed by referral type, and comparisons among groups conducted with chi-square tests. Because medication and psychotherapy have only two possible uptake options – “initiated” or “not initiated” – analytic consistency for the chi-squares required that combined treatment also have two options, so uptake for these patients was counted as initiated only if both medication and psychotherapy had been initiated. If combined treatment was only partially initiated, (i.e., medication, but not psychotherapy) the outcome was counted as “not initiated.” Data about partial completion is provided in the Table 4 footnote.
Table 4.
Uptake of the treatment recommendation by type of treatment recommendation, Time 1 and Time 2
| Time 1 N = 90 M = 14 days after PCP visit |
Time 2 N = 77 M = 84 days after PCP visit |
||||||
|---|---|---|---|---|---|---|---|
| Type of treatment recommended |
n (%) | Initiated n = 21 (23%) |
Not initiated n = 69 (77%) |
Complete uptake at Time 1 (%) |
Initiated n = 41 (53%) |
Not initiated n = 36 (47%) |
Complete uptake at Time 2 (%) |
| Medication | 32 (36%) | 19 | 13 | (59%) | 20 | 6 | (77%) |
| Psychotherapy | 37 (41%) | 0 | 37 | (0%) | 12 | 21 | (36%) |
| Combined treatment | 21 (23%) | 2 | 191 | (9.5%) | 9 | 92 | (50%) |
12 of the 19 patients included in the Time 1 combined treatment “not initiated” category had initiated medication, but not psychotherapy.
5 of the 9 patients included in the Time 2 combined treatment “not initiated” category had initiated medication, but not psychotherapy.
The greatest proportion of uptakes at Time 1 was found among those who had been prescribed medication by their PCP, with 59% of those prescribed medication having initiated treatment by Time 1, 10.5% of those referred to combined treatment having fully initiated uptake, and 0% of those who had been referred to psychotherapy receiving treatment, X2(2, n = 90) = 36.76, p < .001, Cramer’s V = .64 (indicating a strong effect size; Cohen, 1988). At Time 2 (M = 87 days after initial interview), chi-square tests still show significant differences, though only a medium effect size, in uptake among the three groups, X2(2, n = 77) = 9.70, p < .01, Cramer’s V = .35. Although the Time 2 uptake rate was lowest among those recommended psychotherapy (36%, compared to 77% uptake among medication recommendations and 50% among those recommended combined treatment) there was a significant increase in uptake of psychotherapy referrals between Time 1 and Time 2, (from 0% to 36%, X2(1, n = 70) = 16.24, p < .001. There was also a significant increase in uptake among those recommended combined treatment X2(1, n = 96) = 6.70, p < .01, but no statistically significant increase in uptake among those recommended medication, X2(1, n = 58) = 2.01, p = ns.
Discussion
Over one in five Latino primary care patients presented to their PCP with symptoms indicating depression, but despite receiving a treatment recommendation from their PCP, almost half of the patients interviewed had not begun treatment by Time 2, nearly 3 months after their PCP visit. These findings are consistent with reports of Latino care, and point to the urgent need to improve follow-up rates for depressed Latino patients seen in public primary care settings. To that end, this study examined PCP-patient relational factors, treatment preference, and referral type to better understand what makes Latino patients more likely to consider following up on a referral, and more likely to actually initiate uptake of the treatment recommendation.
The analyses showed that patient ratings of the PCP – patient working alliance and PCP cultural competence were positively related to patients’ intention of following up on a referral to mental health care, but that neither working alliance, cultural competency, nor intention of following up on a referral were significantly related to actual uptake of a treatment recommendation. Thus, while associations between PCP – patient variables and patients’ intention of engaging in treatment behavior were found, there was no association between these variables and patients’ actual uptake behavior, or between intention and behavior.
The associations found between the PCP – patient variables and intention to seek treatment confirmed that when patients experience a good working alliance with their PCP and experience their PCP as having high cultural competence, they are more likely to report a strong intention to follow their PCP’s referral for mental health care. This finding is consistent with research maintaining that the working alliance plays a paramount role in patients’ treatment decisions (Fuertes, 2007; Horvath & Symonds, 1991; Julius et al., 2009; Martin, Garske & Davis, 2000), and also extends the relevance of Bordin’s concept of the working alliance (1979) to the question of intention to follow up on a referral. When the patient and the PCP are allied in shared decision-making around their wish to help the patient to change, and the strategies they will employ to enable that change, and when this alliance occurs in the context of a strong bond, the patient may be more likely to be engaged with the treatment plan.
Patient ratings of PCP cultural competence were also found to be associated with intention to follow up on a referral, but this association was non-significant when working alliance was added to the model. A meditational analysis confirmed that working alliance acts as a mediator of the association between cultural competence and intention to follow up on a referral. Thus, the working alliance appears to be the primary mechanism influencing ratings of follow-up intention. These findings support the model proposed by Constantine and Ladany (2001), whereby the working alliance is posited to enable the effectiveness of multicultural competencies. Thus, when considering following up on a referral from their PCP, it may be that a strong working alliance is a necessary precondition for enabling patients to consider whether their provider is sufficiently culturally competent to understand and appropriately respond to their treatment needs. Or, it may be that cultural competence is best understood as the ability to develop a working alliance with culturally different patients. This finding has important implications for our understanding of the mechanisms by which cultural competence influences patients’ intentions of engaging in treatment. Given the primacy of the working alliance in this association, the working alliance may be the most appropriate target for interventions to improve patients’ willingness to consider treatment.
Working alliance, cultural competence, and intention to follow up on a referral were not associated with actual treatment uptake. There are at least two possible explanations for the lack of significant association between these variables. One perspective originates in the health behavior literature, which acknowledges difficulties in predicting health behaviors from psychological variables or treatment intention. According to Ajzen and Fishbein’s Theory of Reasoned Action (Ajzen and Fishbein, 1975), intention is seen as a strong predictor of actual behavior; however, this is true only when certain conditions are met, including that the individual must possess a high degree of volitional control in carrying out the intention. Uptake of the treatment recommendation is thus a problematic behavior to predict based on intention to follow up, and, by extension, on the variables associated with intention. Uptake of a treatment recommendation, particularly psychotherapy, is highly dependent on other people and factors. In particular, lack of access to services and the lack of availability of Spanish-speaking therapists are considerable impediments to accessing care for Latino patients (U.S. Department of Health and Human Services, 2001). The possibility that access and availability complicate the relationship between intention and treatment uptake is partially supported by the findings showing a positive trend between intention and uptake among a sub-sample of patients who had been recommended medication treatment, and who therefore would face fewer access and availability barriers. It is possible that a larger sample size may have shown a significant effect in this analysis.
The second possibility is that social desirability bias or leniency bias played a role in inflating participants’ report of the PCP – patient factors, or their stated intention of following up on a referral from their PCP. Social desirability bias refers to the tendency of individuals to present themselves in a positive light, regardless of their true feelings, whereas leniency bias occurs when an individual rates a close acquaintance, or someone with whom he or she is highly invested, more highly than that individual’s true feelings would indicate (Podsakoff, MacKenzie, Lee, & Podsakoff, 2003). Social desirability bias might therefore inflate a patient’s reported intention of following up on a referral, whereas leniency bias could inflate their report of their PCP – patient working alliance or their PCP’s cultural competence. Both types of bias could potentially have caused an artificial increase in mean working alliance, cultural competence, or intention scores.
Sample size limitations and an imbalance of treatment preference contributed to unexpected results of the prediction that treatment preference match would be associated with a higher uptake rate. Among this sample, type of treatment recommendation was strongly associated with treatment uptake, with people recommended medication more likely to have completed treatment uptake. Given that the sample overwhelmingly preferred psychotherapy to medication, it is possible that this finding represents the difference in access between medication and psychotherapy, and does not necessarily indicate that treatment preference is an unimportant consideration when recommending depression treatment. That is, patients were able to obtain a medication prescription at their PCP visit, and to fill the prescription immediately. Although access was not directly assessed, it appears that access to psychotherapy was more difficult than access to medication, with many patients reporting anecdotally at Time 2 that they were still waiting for a psychotherapy appointment. Access to psychotherapy was likely particularly difficult for patients with limited English proficiency. The possible confounding effect of initial difficulties accessing psychotherapy is supported by the fact that between Time 1 and Time 2, uptake of psychotherapy recommendations increased 36%, while the increase between Time 1 and Time 2 uptake was insignificant for medication recommendations. Thus, although treatment preference match did not appear to be a significant correlate of treatment uptake in this sample, this should not be taken as a generalizable finding. It should also be noted, however, that PCP preference may have played a role. Given that they were likely aware of the delay in accessing psychotherapy, PCPs may have chosen to recommend medication in order to ensure immediate care for their patients, and to avoid leaving patients’ depression untreated for an indefinite period. Again, the lack of a direct access variable means that these inferences are conjectural only.
Barriers to accessing psychotherapy might contribute to the lack of significant association between intention and uptake, as well as the significantly greater uptake of medication recommendations, compared with psychotherapy, despite patient preference for psychotherapy. Indeed, the data suggest that barriers could prevent uptake, even in the presence of a strong intention and when there is preference match. This possibility is a likely one, particularly for Latinos, who have considerable barriers in accessing treatment (i.e., language barriers, higher rates of poverty than the general population, and a lower likelihood of having comprehensive insurance; Pew Hispanic Center, 2010). Were these barriers to be reduced, the working alliance, treatment intentions, and patient preference might emerge as more relevant to patients’ treatment uptake behaviors.
Thus, despite a lack of association between working alliance and treatment uptake, this study’s finding of a strong association between the working alliance and intention to follow up on a referral is still relevant. As mental health systems evolve in response to an increasing awareness of mental health treatment disparities (e.g., through the emphasis on Accountable Care Organizations), the instrumental barriers that complicate the intention – uptake relationship may well decrease in potency. The PCP – patient working alliance may therefore assume greater primacy in influencing treatment uptake. Developing PCPs’ awareness of this association and helping them maximize the working alliance would then become a pragmatic approach to increasing the likelihood that patients would consider and ultimately access depression treatment.
Limitations
This study was constrained by a number of factors. The questions raised by the analysis about effects such as potential bias and access difficulties would have been measureable had the study included the relevant assessment tools. Mental health treatment access is a complicated behavior involving personal, interpersonal, organizational, social, and policy aspects, and was beyond the scope of this study to measure. A related limitation is the fact that interviews were conducted by phone, which, though beneficial to participants in terms of logistics, comfort with disclosure, and literacy burden, has been shown to exacerbate response bias and social desirability bias (Paris, Añez, Bedregal, Andrés-Hyman, & Davidson, 2005).
In addition, there are unique characteristics about the recruitment site that may affect the generalizability of these results. First, recruitment took place at a public primary care clinic that serves a largely ethnic minority population, and which is committed to providing culturally and linguistically competent care. Indeed, several of the European American providers are fluent Spanish speakers. In addition, there is a Latino Mental Health clinic directly upstairs from the primary care clinic, staffed by bilingual and bicultural clinicians. Although the wait at the clinic could be several months, its location and familiarity likely had a facilitative impact on treatment access. Therefore, patients at this primary care clinic may enjoy a level of attention to culture and equity not experienced in other settings, a possibility supported by the high mean cultural competence scores. The treatment rates presented here may therefore be even higher than they may have been elsewhere. Nonetheless, the clinic is a public, urban clinic that serves low-income Latinos from many different nationalities, and thus the results have relevance for similar settings.
Lastly, while the mediational analysis raises important questions about the mechanisms of change of cultural competence and working alliance, the cross-sectional nature of the analysis precludes a firm inference about the mediational role of working alliance on the relationship between cultural competence and intention to follow up on a referral. Longitudinal research could more closely evaluate whether there is a true mediational relationship among the three variables.
Implications
The association between the working alliance and intention to follow up on a referral suggests that the PCP – patient relationship merits attention insofar as it relates to the treatment of depression among Latinos. Efforts to maximize PCPs’ attention to this relationship while simultaneously working to reduce the barriers to accessing treatment may serve well to increase the rates of depression treatment uptake.
One such approach, mentioned above, is the shift to integrated and collaborative treatment models, which are already being shown to improve treatment utilization and access among Latinos (Cabassa & Hansen, 2007; Dwight-Johnson et al., 2010; Ell et al., 2011). Such models may be successful at least in part because they build on the working alliance with the PCP while simultaneously improving access to specialty mental health providers and incorporating a care manager who is responsible for actively pursuing the patient and addressing barriers to treatment. When the PCP and mental health specialists collaborate on patient care, both the patient and the providers stand to benefit. The PCP, the most familiar and trusted health care provider, together with the mental health specialist facilitate access and de-mystify mental health care, and the patient receives both continuity of care and as well as guideline-adherent mental health care. At the same time, PCPs are relieved of the burden of being the sole treaters for their many patients with mental health needs. Indeed, though not a panacea (Bower & Sibbald, 2000), integrated care has been shown to improve the perception that members of minority groups have about mental health care and to improve treatment initiation rates (Chapa, 2004). Understanding the role of the working alliance and cultural competence in treatment uptake could help PCPs to formulate depression treatment and goals in collaboration with their patients.
Conclusions
This study has the potential to contribute to efforts to improve Latino patients’ access to depression treatment, by identifying factors that increase the likelihood that Latino patients will consider treatment. The data show that the alliance that PCPs share with their patients – the bond they develop, the degree to which they and their patients are allied in identifying the patient’s desire for change and the strategies to be employed in creating that change – is associated with patients’ intention to follow up on a treatment recommendation to mental health care. The data further show a mediational effect of working alliance on the relationship between cultural competence and intention to follow up on a referral, thereby contributing to our understanding of the role of cultural competence on treatment intention. Understanding the role of the working alliance and cultural competence in intended and actual treatment uptake could help providers ensure treatment for their depressed patients.
Nonetheless, despite the evidence of an association between working alliance and intention, this study strongly suggests that problems accessing treatment may prevent uptake, even in the presence of a strong intention and treatment preference match. Further examination of treatment access barriers faced by primary care patients could contribute to our understanding of how patient preference and recommendation type affect treatment uptake.
Acknowledgments
Preparation of this article was supported by National Institute of Mental Health grant F31MH091874.
Footnotes
The first eleven participants received $15. Subsequent funding enabled an increase in compensation.
References
- Ajzen I, Fishbein M. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Alegría M, Chatterji P, Wells K, Cao Z, Chen C-N, Takeuchi D, Jackson J, Meng X-L. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric services (Washington, DC) 2008a;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Polo A, Gao S, Santana L, Rothstein D, Jimenez A, Hunter ML, Mendieta F, et al. Evaluation of a patient activation and empowerment intervention in mental health care. Medical Care. 2008b;46(3):247–256. doi: 10.1097/MLR.0b013e318158af52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arredondo P, Toporek R, Brown SP, Jones J, et al. Operationalization of the multicultural counseling competencies. Journal of Multicultural Counseling and Development. 1996;24:42–78. [Google Scholar]
- Arroll B, Macgillivray S, Ogston S, Reid I, Sullivan F, Williams B, Crombie I. Efficacy and tolerability of tricyclic antidepressants and SSRIs compared with placebo for treatment of depression in primary care: A meta-analysis. Annals of Family Medicine. 2005;3:449–456. doi: 10.1370/afm.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhui K, Warfa N, Edonya P, McKenzie K, Bhugra D. Cultural competence in mental health care: A review of model evaluations. BMC Health Services Research. 2007;7:1–10. doi: 10.1186/1472-6963-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biever JL, Gómez JP, González CG, Patrizio N. Psychological services to Spanish-speaking populations: A model curriculum for training competent professionals. Training and Education in Professional Psychology. 2011;5:81. [Google Scholar]
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice. 1979;16:252–260. [Google Scholar]
- Bower P, Sibbald B. Systematic review of the effect of on-site mental health professionals on the clinical behaviour of general practitioners. BMJ. 2000;320:614–617. doi: 10.1136/bmj.320.7235.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne N, Regan C, Livingston G. Adherence to treatment in mood disorders. Current opinion in psychiatry. 2006;19:44–49. doi: 10.1097/01.yco.0000191501.54034.7c. [DOI] [PubMed] [Google Scholar]
- Cabassa LJ. Latino immigrant men's perceptions of depression and attitudes toward help seeking. Hispanic Journal of Behavioral Sciences. 2007;29(4):492–509. [Google Scholar]
- Cabassa LJ, Hansen MC. A systematic review of depression treatments in primary care for Latino adults. Research on Social Work Practice, Research on Social Work Practice. 2007;17:494–503. [Google Scholar]
- Cabassa LJ, Zayas LH. Latino immigrants' intentions to seek depression care. The American journal of orthopsychiatry. 2007;77:231–242. doi: 10.1037/0002-9432.77.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapa T. Mental Health Services in Primary Care Settings for Racial and Ethnic Minority Populations. Rockville, M.D: U.S. Department of Health and Human Services, Office of Minority Health; 2004. pp. 1–30. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Constantine MG, Ladany N. New visions for defining and assessing multicultural counseling competence. In: Ponterotto JG, Casas JM, Suzuki LA, Alexander CM, editors. Handbook of Multicultural Counseling. 2nd ed. Thousand Oaks: Sage; 2001. pp. 482–498. [Google Scholar]
- Cuijpers P, Geraedts A, van Oppen P, Andersson G, Markowitz JC, van Straten A. Interpersonal psychotherapy for depression: A meta-analysis. The American Journal of Psychiatry. 2011;168:581–592. doi: 10.1176/appi.ajp.2010.10101411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Schuurmans J, van Oppen P, Hollon SD, Andersson G. Psychotherapy for chronic major depression and dysthymia: A meta-analysis. Clinical Psychology Review. 2010;30:51–62. doi: 10.1016/j.cpr.2009.09.003. [DOI] [PubMed] [Google Scholar]
- De Figueiredo JM, Boerstler H, Doros G. Failure of high-risk minority patients to show up for outpatient psychiatric treatment. International Journal of Mental Health, International Journal of Mental Health. 2009;38:91–105. [Google Scholar]
- Dwight-Johnson M, Lagomasino I, Hay MJ, Zhang PL, Tang M, et al. Effectiveness of collaborative care in addressing depression treatment preferences among low-income Latinos. Psychiatric Services. 2010;61:1112–1118. doi: 10.1176/ps.2010.61.11.1112. [DOI] [PubMed] [Google Scholar]
- Ell K, Xie B, Kapetanovic S, Quinn DI, Lee PJ, Wells A, Chou CP. One-year follow-up of collaborative depression care for low-income, predominantly Hispanic patients with cancer. Psychiatric Services. 2011;62:162–170. doi: 10.1176/ps.62.2.pss6202_0162. [DOI] [PubMed] [Google Scholar]
- Fernandez Y, Garcia E, Franks P, Jerant A, Bell RA, Kravitz RL. Depression treatment preferences of Hispanic individuals: exploring the influence of ethnicity, language, and explanatory models. Journal of the American Board of Family Medicine : JABFM. 2011;24:39–50. doi: 10.3122/jabfm.2011.01.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer EH, Farina A. Attitudes toward seeking professional psychological help: A shortened form and considerations for research. Journal of College Student Development. 1995;36:368–373. [Google Scholar]
- Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Archives of Pediatric Adolescent Medicine. 1998;152:1119–1125. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- Fuertes JN, Boylan LS, Fontanella JA. Behavioral indices in medical care outcome: the working alliance, adherence, and related factors. Journal of General Internal Medicine. 2009;24:80–85. doi: 10.1007/s11606-008-0841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuertes JN, Mislowack A, Bennett J, Paul L, Gilbert TC, Fontan G, Boylan LS. The physician-patient working alliance. Patient education and counseling. 2007;66:29–36. doi: 10.1016/j.pec.2006.09.013. [DOI] [PubMed] [Google Scholar]
- González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Archives of general psychiatry. 1. Vol. 67. Am Med Assoc.; 2010. Depression care in the United States: too little for too few; p. 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology. 1991;38(2):139–149. [Google Scholar]
- Interian A, Martinez IE, Guarnaccia PJ, Vega WA, Escobar JI. A qualitative analysis of the perception of stigma among Latinos receiving antidepressants. Psychiatric services (Washington, DC) 2007;58(12):1591–1594. doi: 10.1176/appi.ps.58.12.1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa RZ, Cardemil EV, Falmagne RF. Help seeking and help receiving for emotional distress among Latino men and women. Qualitative Health Research. 2010;20:1558–1572. doi: 10.1177/1049732310369140. [DOI] [PubMed] [Google Scholar]
- Julius RJ, Novitsky MA, Dubin WR. Medication adherence: a review of the literature and implications for clinical practice. Journal of psychiatric practice. 2009;15(1):34–44. doi: 10.1097/01.pra.0000344917.43780.77. [DOI] [PubMed] [Google Scholar]
- Kanter JW, Rusch LC, Brondino MJ. Depression self-stigma: A new measure and preliminary findings. Journal of Nervous and Mental Disease. 2008;196:663–670. doi: 10.1097/NMD.0b013e318183f8af. [DOI] [PubMed] [Google Scholar]
- Kenny DA. Mediation. 2012 Retrieved from http://davidakenny.net/cm/mediate.htm#COMP. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA: The Journal of the American Medical Association. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Wang P, Wells KB, Zaslavsky AM. Prevalence and Treatment of Mental Disorders, 1990 to 2003. New England Journal of Medicine. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz RL, Paterniti DA, Epstein RM, Rochlen AB, Bell RA, Cipri C, Fernandez y, Garcia E, et al. Relational barriers to depression help-seeking in primary care. Patient education and counseling. 2011;82:207–213. doi: 10.1016/j.pec.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz R, Franks P, Feldman M, Meredith L, Hinton L, Franz C, Duberstein P, et al. What drives referral from primary care physicians to mental health specialists? A randomized trial using actors portraying depressive symptoms. Journal of General Internal Medicine. 2006;21(6):584–589. doi: 10.1111/j.1525-1497.2006.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Roche MJ, D'Angelo E, Gualdron L, Leavell J. Culturally sensitive guided imagery for allocentric latinos: a pilot study. Psychotherapy: Theory, Research, Practice, Training Special Issue: Culture, Race, and Ethnicity in Psychotherapy. 2006;43:555–560. doi: 10.1037/0033-3204.43.4.555. [DOI] [PubMed] [Google Scholar]
- Lin P, Campbell DG, Chaney EF, Liu CF, Heagerty P, Felder BL, Hedrick SC. The influence of patient preference on depression treatment in primary care. Annals of Behavioral Medicine. 2005;30:164–173. doi: 10.1207/s15324796abm3002_9. [DOI] [PubMed] [Google Scholar]
- Lieu TA, Finkelstein JA, Lozano P, Capra AM, Chi FW, Jensvold N, Quesenberry CP, et al. Cultural competence policies and other predictors of asthma care. 2004 doi: 10.1542/peds.114.1.e102. [DOI] [PubMed] [Google Scholar]
- Martin D, Garske J, Davis M. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68(3):438–450. [PubMed] [Google Scholar]
- McKenna MT, Michaud CM, Murray JL, Marks JS. Assessing the burden of disease in the United States using Disability-Adjusted Life Years. American Journal of Preventive Medicine. 2005;28:415–423. doi: 10.1016/j.amepre.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Mendelson T, Rehkopf DH, Kubzansky LD. Depression among Latinos in the United States: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2008;76(3):355–366. doi: 10.1037/0022-006X.76.3.355. [DOI] [PubMed] [Google Scholar]
- Michaud CM, McKenna MT, Begg S, Tomijima N, Majmudar M, Bulzacchelli MT, Ebrahim S, et al. The burden of disease and injury in the United States 2006. Population Health Metrics. 1996;4:1–49. doi: 10.1186/1478-7954-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2003;290:57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- Miranda J, Cooper LA. Disparities in care for depression among primary care patients. Journal of General Internal Medicine. 2004;19(2):120–126. doi: 10.1111/j.1525-1497.2004.30272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moitabai R, Olfson M. National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the national comorbidity survey replication. Journal of Clinical Psychiatry. 2008;69:1064–1074. doi: 10.4088/jcp.v69n0704. [DOI] [PubMed] [Google Scholar]
- Muntaner C. Socioeconomic position and major mental disorders. Epidemiologic Reviews. 2004;26:53–62. doi: 10.1093/epirev/mxh001. [DOI] [PubMed] [Google Scholar]
- Norris AE, Ford K, Bova CA. Psychometrics of a brief acculturation scale for Hispanics in a probability sample of urban Hispanic adolescents and young adults. Hispanic Journal of Behavioral Sciences. 1996;18:29–38. [Google Scholar]
- O’Connor EA, Whitlock EP, Bell TL, Gaynes BN. Screening for depression in adult patients in primary care settings: A systematic evidence review. Annals of Internal Medicine. 2009;151:793–803. doi: 10.7326/0003-4819-151-11-200912010-00007. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus S, Druss B. National trends in the outpatient treatment of depression. JAMA. 2002;287:203–209. doi: 10.1001/jama.287.2.203. [DOI] [PubMed] [Google Scholar]
- Ortega A, Alegría M. Self-reliance, mental health need, and the use of mental healthcare among island Puerto Ricans. Mental Health Services Research. 2002;4(3):131–140. doi: 10.1023/a:1019707012403. [DOI] [PubMed] [Google Scholar]
- Paris M, Añez L, Bedregal L, Andrés-Hyman R, Davidson L. Help seeking and satisfaction among Latinas: The roles of setting, ethnic identity, and therapeutic alliance. Journal of Community Psychology. 2005;33(3):299–312. [Google Scholar]
- Pew Hispanic Center. Statistical portrait of Hispanics in the United States pewhispanic.org. [Retrieved March 3, 2012];2010 from http://www.pewhispanic.org/2012/02/21/statistical-portrait-of-hispanics-in-the-united-states-2010/ [Google Scholar]
- Pingitore D, Snowden L, Sansone RA, Klinkman M. Persons with depressive symptoms and the treatments they receive: a comparison of primary care physicians and psychiatrists. International journal of psychiatry in medicine. 2001;31(1):41–60. doi: 10.2190/6BUL-MWTQ-0M18-30GL. [DOI] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology. 2003;88:879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Leonardelli GJ. Calculation for the Sobel test: An interactive calculation tool for mediation tests. [Retrieved March 26, 2012];2001 from: http://quantpsy.org/sobel/sobel.htm. [Google Scholar]
- Sánchez-Lacay JA, Lewis-Fernandez R, Goetz D, Blanco C, Salmann E, Davies S, Liebowitz M. Open trial of nefazodone among Hispanics with major depression: Efficacy, tolerability, and adherence issues. Depression and Anxiety, Depression and Anxiety. 2001;13:118–124. doi: 10.1002/da.1027. [DOI] [PubMed] [Google Scholar]
- Sue DW, Torino GC. Racial– cultural competence: Awareness, knowledge, and skills. In: Carter RT, editor. Handbook of racial–cultural psychology and counseling: Vol. 2. Training and practice. Hoboken, NJ: Wiley; 2005. pp. 3–18. [Google Scholar]
- U.S.Census Bureau. U.S. Census Bureau projections show a slower growing, older, more diverse nation a half century from now. [December 12, 2012];U.S. Census Bureau Newsroom Release. 2012 Accessed online https://www.census.gov/newsroom/releases/archives/population/cb12-243.html. [Google Scholar]
- U.S. Census Bureau. Poverty rates for selected detailed race and Hispanic groups by state and place, 2007–2011. American Community Survey Briefs. 2013 Accessed online http://www.census.gov/prod/2013pubs/acsbr11-17.pdf. [Google Scholar]
- U.S. Department of Health and Human Services. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. Mental Health: Culture, Race, and Ethnicity, A Supplement to Mental Health: A Report of the Surgeon General surgeongeneral.gov. [Google Scholar]
- Uebelacker LA, Wang PS, Berglund P, Kessler RC. Clinical differences among patients treated for mental health problems in general medical and specialty mental health settings in the National Comorbidity Survey Replication. General hospital psychiatry. 2006;28(5):387–395. doi: 10.1016/j.genhosppsych.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S. Help seeking for mental health problems among Mexican-Americans. Journal of Immigrant Health. 2001;3:133–140. doi: 10.1023/A:1011385004913. [DOI] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. The American journal of psychiatry. 2001;158(12):2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- Wells K, Sherbourne C, Schoenbaum M, Ettner S, Duan N, Miranda J, Unũtzer J, Rubenstein L. Five-year impact of quality improvement for depression: Results of a group-level randomized controlled trial. Archives of General Psychiatry. 2004;61:378–386. doi: 10.1001/archpsyc.61.4.378. [DOI] [PubMed] [Google Scholar]
- Yzerbyt VY, Muller D, Judd CM. Adjusting researchers’ approach to adjustment: On the use of covariates when testing interactions. Journal of Experimental Social Psychology. 2004;40:424–431. [Google Scholar]