Abstract
Background
Combined pulmonary fibrosis and emphysema (CPFE) have different pulmonary function tests (PFTs) and outcomes than idiopathic pulmonary fibrosis (IPF). The intention of this study was to identify unknown differences between CPFE and IPF by a retrospective comparison of clinical data including baseline and annual changes in pulmonary function, comorbidities, laboratory findings, clinical characteristics and cause of hospitalization.
Methods
This study retrospectively enrolled patients with CPFE and IPF who had undergone PFTs once or several times per year during a follow-up period of three years. Baseline clinical characteristics and the annual changes in the pulmonary function during the follow-up period were compared between 26 with CPFE and 42 patients with IPF.
Results
The baseline ratio of forced expiratory volume in one second to forced vital capacity (FEV1/FVC%) in patients with CPFE was lower than that in patients with IPF (78.6±1.7 vs. 82.9±1.1, p=0.041). The annual decrease in FEV1/FVC in the CPFE was significantly higher than in the IPF. The annual decreases in diffusion capacity of carbon monoxide and FVC showed no significant differences between the two groups. The symptom durations of cough and sputum were in the CPFE significantly lower than in the IPF. The serum erythrocyte sedimentation rate level at the acute stage was significantly higher than in the IPF. There were no significant differences in the hospitalization rate and pneumonia was the most common cause of hospitalization in both study groups.
Conclusion
The annual decrease of FEV1/FVC was in patients with CPFE significantly higher than in the patients with IPF.
Keywords: Pulmonary Emphysema, Pulmonary Fibrosis, Idiopathic Pulmonary Fibrosis, Respiratory Function Tests
Introduction
Combined pulmonary fibrosis and emphysema (CPFE) is defined as concurrent emphysema and pulmonary fibrosis in a patient. This disease may have a different clinical outcome and pulmonary function compared to idiopathic pulmonary fibrosis (IPF). But the difference and magnitude have not been completely elucidated. CPFE experience mildly expiratory flow limitation and overexpansion, as well as significantly compromised gas exchange during exercise1,2,3,4,5,6,7,8,9. Notably, CPFE have a relatively normal lung volume compared to those with IPF2,3,4,10. Pulmonary emphysema increases lung compliance and volume, while pulmonary fibrosis decreases compliance and volume. Thus, ventilatory function appears relatively normal because of these two opposing conditions in CPFE4,11. Emphysema associated with CPFE is localized to the upper pulmonary lobes and pulmonary fibrosis to the lower lobes4. CPFE is often concomitant with numerous complications including pulmonary hypertension, acute lung injury, and lung cancer4,5,12,13,14. The condition occurs primarily in male smokers, and these co-morbidities are known to impact the survival rate4,5,6,12. Generally, pulmonary function is comparatively normal in CPFE than in IPF. In a prior study evaluating the long term pulmonary function in CPFE and IPF, the reduction in vital capacity and total lung capacity was less in CPFE patients than in IPF; the diffusion capacity of carbon monoxide (DLco) was also lower in the CPFE than the IPF11. At present, there are few long-term studies comparing the change in pulmonary function between CPFE and IPF3,6,11,15. Comparative studies focused on other clinical parameters such as acute exacerbation are similarly inadequate. We hypothesized that CPFE present distinct clinical characteristics and disease progression than IPF in pulmonary function and acute exacerbation. We investigated the correlation to several clinical parameters including concomitant diseases, pulmonary function, laboratory findings, symptoms, and hospitalization to discern potential differences between the two diseases that have not been revealed.
This protocol was screened and approved by the Committee of Clinical Research Ethics of Gachon University's Gil Medical Center.
Materials and Methods
1. Patient characteristics
CPFE and IPF patients receiving pulmonary function test (PFT) over 3 years at the Division of Pulmonology at Gachon University Gil Medical Center from 1 January 2000 to 31 June 2013 were retrospectively reviewed. In total, 68 records of 26 patients with CPFE and 42 patients with IPF were analyzed for sex, age, smoking status, laboratory findings, and pulmonary function. IPF was diagnosed based on the American Thoracic Society (ATS) and European Respiratory Society (ERS) 2012 guidelines16. CPFE was diagnosed in patients showing well-demarcated areas of low attenuation typical of emphysema located predominantly in the upper lung zones and patterns compatible with IPF11.
2. Clinical characteristics and PFT
The sex, age, smoking status, and laboratory findings at the first medical examination were screened, and the clinical symptoms, symptom duration, hospitalization incidence and cause, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) during stable periods, and the ESR and CRP during hospitalization periods during the follow-up period were compared between the patient groups. The follow-up period was defined as the interval between the first hospital visit and the last visit or patient death. The PFT evaluated the forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and pulmonary DLco. Data were measured as the percentage (% predicted) of the absolute (mL) and estimated values. Pulmonary function at the initial hospital visit served as the baseline respiratory function. Patients who performed a PFT at least three times during the study period.
3. Statistical analysis
Data means and magnitude of change in numerical pulmonary function and laboratory findings were compared using the t-test. Correlations between the binary variables such as sex, age, smoking, and concomitant diseases were analyzed using the chi-square test. Patients who performed a PFT at least three times during the study period were reviewed to evaluate the pulmonary function change over time using linear regression analysis. Differences were considered significant when the p-value less than 0.05.
Results
1. Clinical characteristics of CPFE and IPF (Table 1)
Table 1.
Clinical characteristics of CPFE and IPF
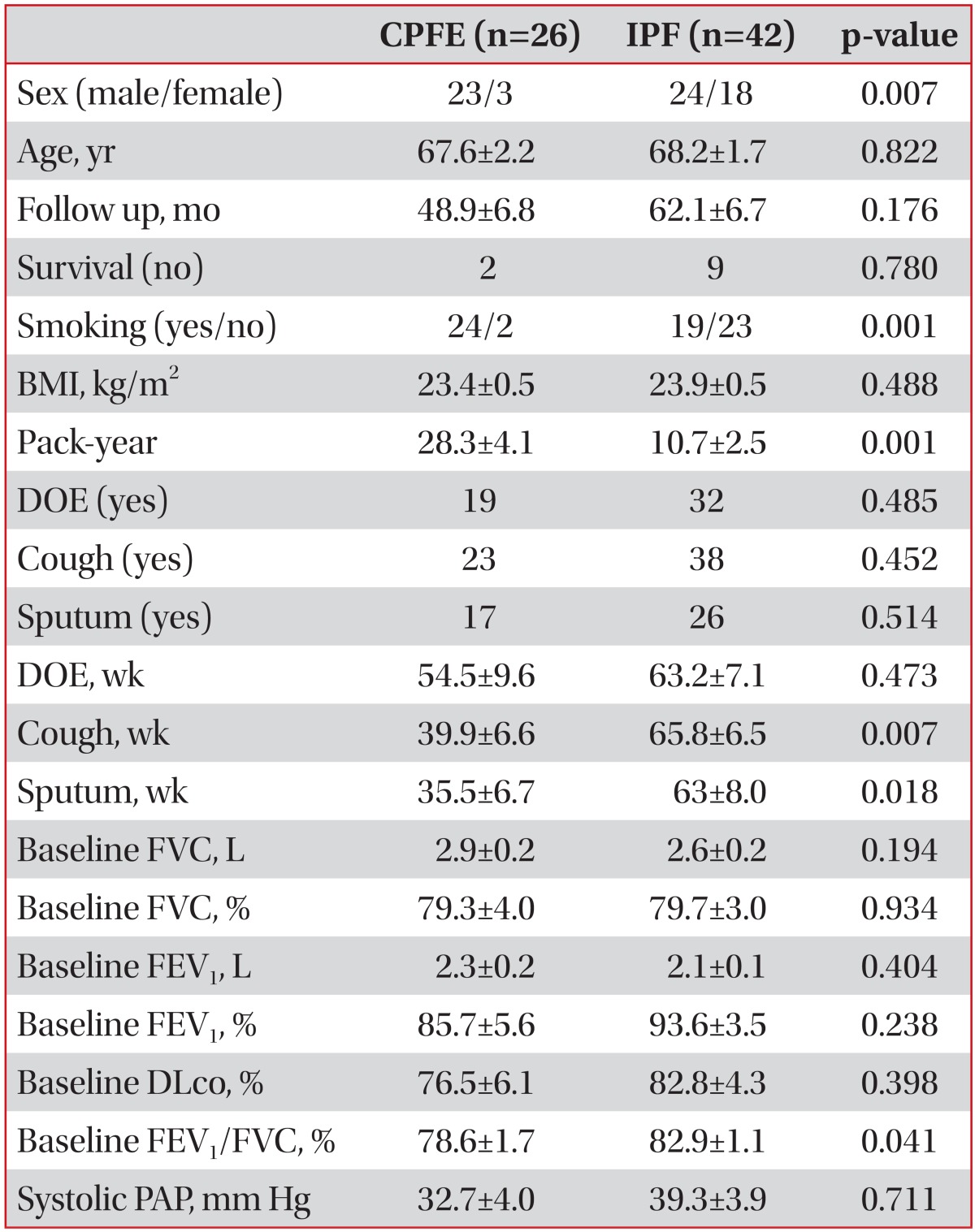
Values are presented as number or mean±SD.
CPFE: combined pulmonary fibrosis and emphysema; IPF: idiopathic pulmonary fibrosis; BMI: body mass index; DOE: dyspnea of exertion; FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second; DLco: diffusion capacity of carbon monoxide; PAP: pulmonary arterial pressure; SD: standard deviation.
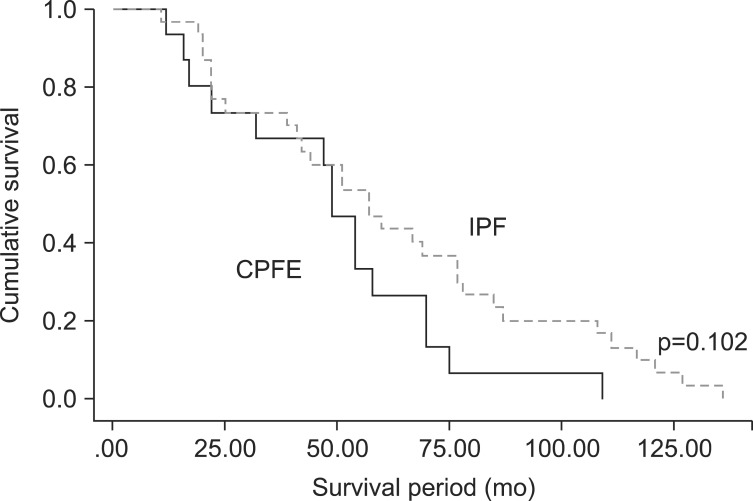
Male accounted for 23 (88.5%) of the CPFE and was significantly higher than that the IPF (p=0.007). Smoking status and pack-year were significantly higher in the CPFE (p=0.001). In the analysis of respiratory symptoms (excertional dyspnea, cough, and sputum), there were no significant differences between the two groups. The mean symptom duration for both cough and sputum were significantly longer in the IPF than in the CPFE (p=0.007 and p=0.018). There were no significant differences between the two groups in FVC and FEV1, but the FEV1/FVC ratio was significantly lower in the CPFE patient group (p=0.041). DLco (%) were lower in the CPFE compared to the IPF, but the difference was not statistically significant. Both groups exhibited an elevated pulmonary artery pressure compared with normal range, but there was no significant difference between the two groups. We observed no significant difference in survival both group (Figure 1).
Figure 1.
Kaplan-Meier survival curves. CPFE: combined pulmonary fibrosis and emphysema; IPF: idiopathic pulmonary fibrosis.
2. Annual changes in pulmonary function in the CPFE and IPF (Table 2)
Table 2.
Annual changes in pulmonary function in the groups with CPFE and IPF
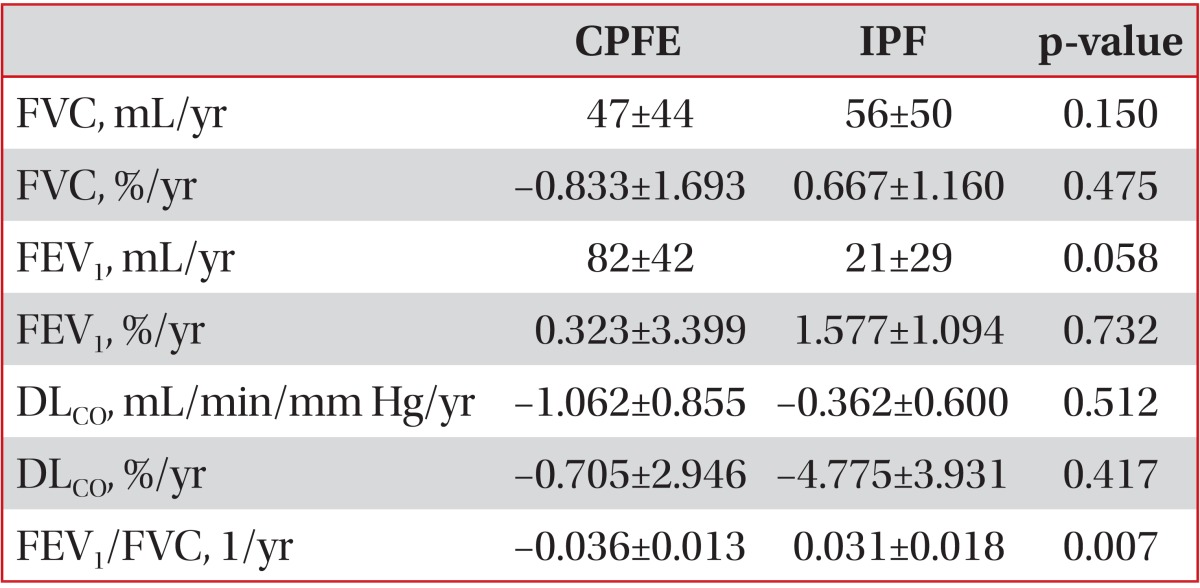
Values are presented as mean±SD or number.
CPFE: combined pulmonary fibrosis and emphysema; IPF: idiopathic pulmonary fibrosis; FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second; DLCO: diffusion capacity of carbon monoxide; SD: standard deviation.
Notably, the FEV1/FVC did significantly decrease over time in the CPFE compared with the IPF (p=0.007). In the CPFE, the mean FVC increased over time, while the mean FEV1 decreased. In the IPF, FVC decreased, and the FEV1 slightly increased over time. However, there were no significant differences in FVC or FEV1 change over time between the two groups. DLco decreased in both groups over, but to a greater extent in CPFE; however, there was no significant difference between the groups.
3. Co-morbidities of CPFE and IPF (Table 3)
Table 3.
Comorbidity of CPFE and IPF
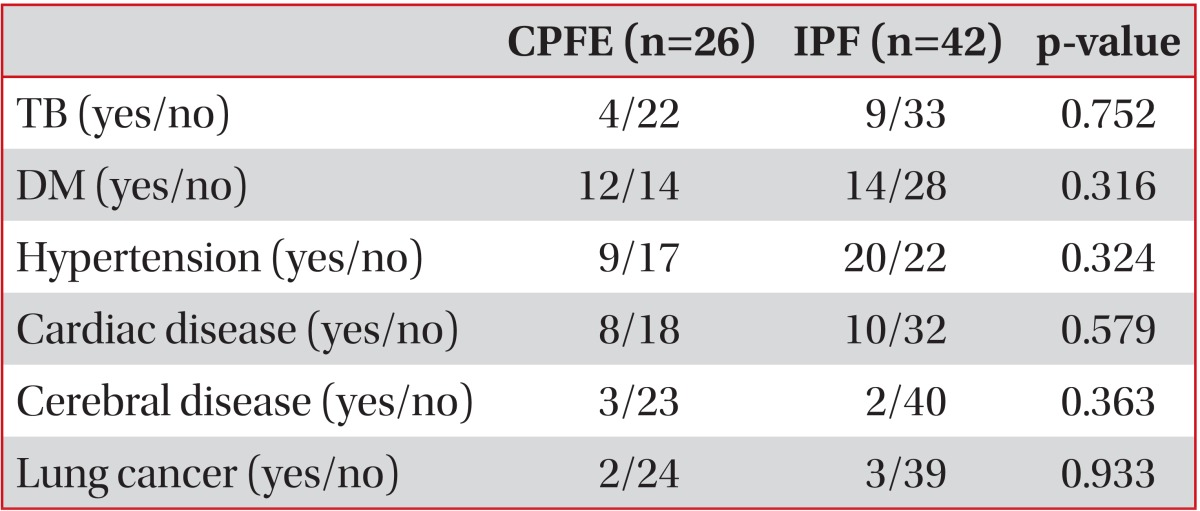
CPFE: combined pulmonary fibrosis and emphysema; IPF: idiopathic pulmonary fibrosis; TB: Mycobacterium tuberculosis history; DM: diabetes mellitus.
In the analysis of co-morbidities such as tuberculosis, diabetes, hypertension, heart disease, cerebral disease, and lung cancer to survival rate, there were no significant differences in any of the variables between the two groups.
4. Laboratory finding of CPFE and IPF (Table 4)
Table 4.
Laboratory findings of CPFE and IPF
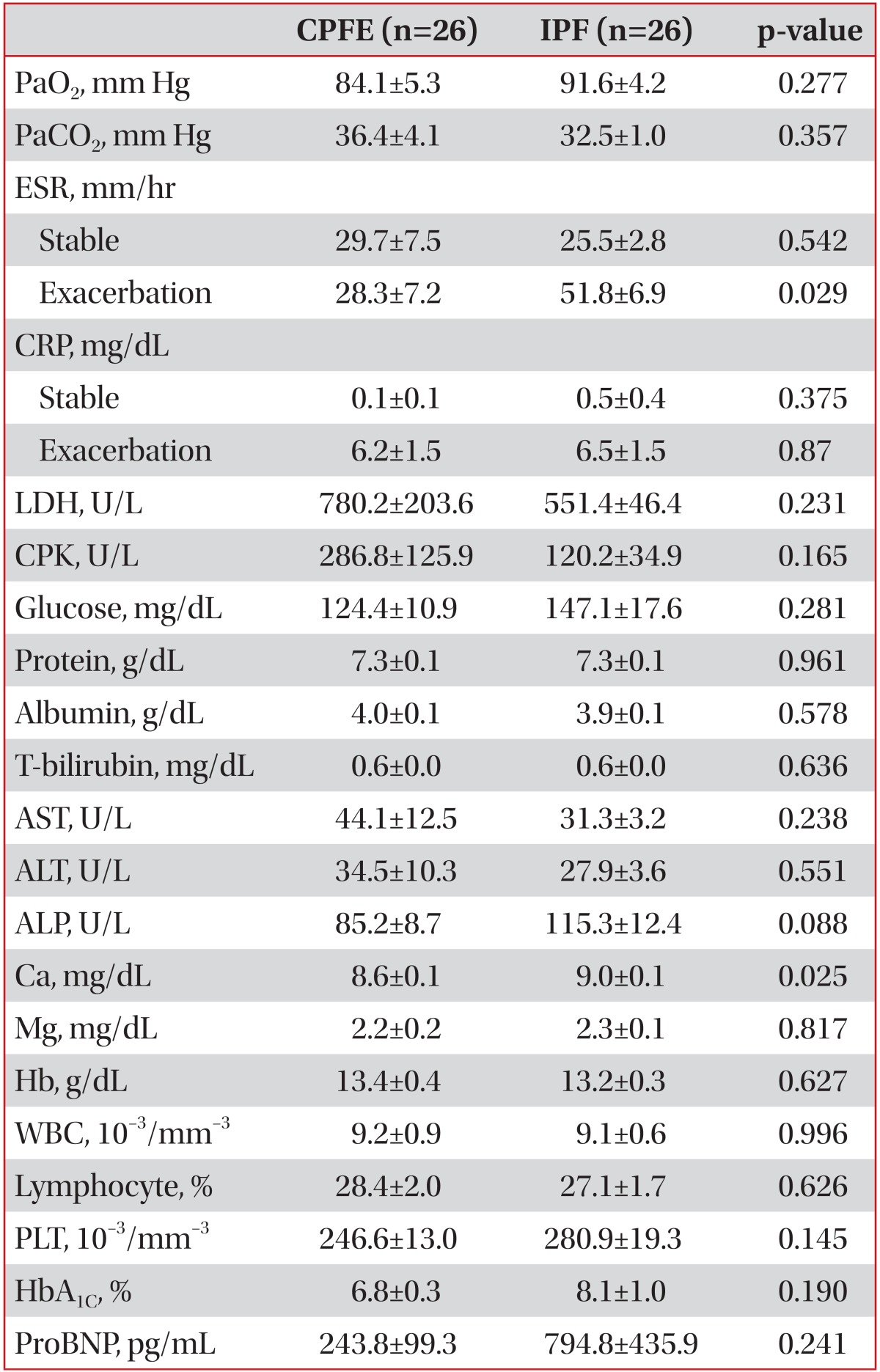
Values are presented as mean±SD or number.
CPFE: combined pulmonary fibrosis and emphysema; IPF: idiopathic pulmonary fibrosis; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; LDH: lactate dehydrogenase; CPK: creatine kinase; T-bilirubin: total bilirubin; AST: aspartate aminotransferase; ALT: alanine transaminase; ALP: alkaline phosphatase; WBC: white blood cell; PLT: platelet; HbA1C: hemoglobinA1C; ProBNP: pro-brain natriuretic peptide; SD: standard deviation.
The mean ESR during hospital period was significantly higher in the IPF (p=0.029). The mean ESR during stable periods and the mean CRP during hospital period and stable period were not significantly different between the two groups. The mean baseline serum calcium concentration at stable was higher in the IPF than the CPFE but was within the normal range (p=0.025). There was no significant difference between the two groups in the other laboratory findings.
5. Cause of hospitalization (Table 5)
Table 5.
Causes of hospitalization
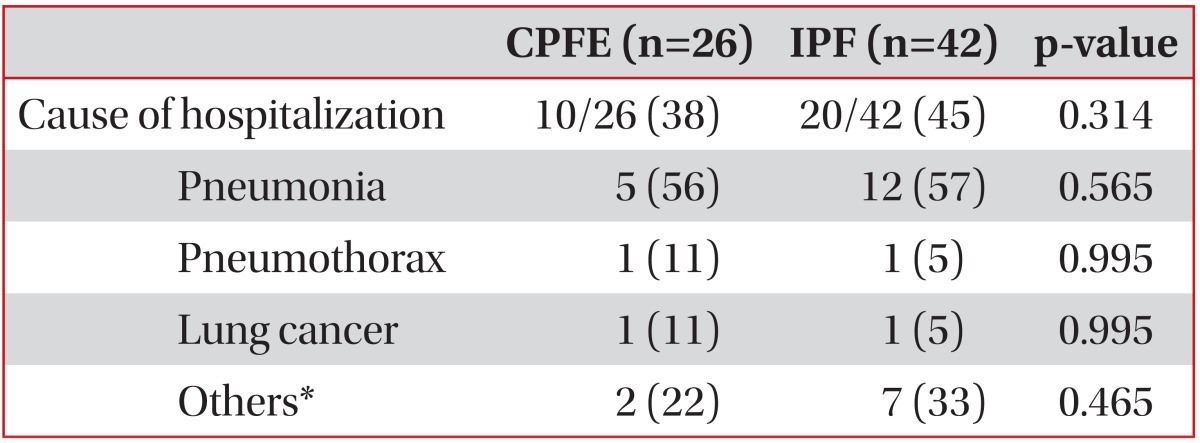
Values are presented as number (%).
*Upper airway infection, pulmonary thromboembolism, Still's disease, acute exacerbation of IPF.
CPFE: combined pulmonary fibrosis and emphysema; IPF: idiopathic pulmonary fibrosis.
The rate of hospitalization was 38% in the CPFE and 45% in the IPF, indicating no significant difference between the two groups. Pneumonia, which occurred at the highest frequency of hospitalization, accounted for 56% of CPFE and 56% of IPF, which was a high incidence in both groups.
6. Treatment of CPFE and IPF (Table 6)
Table 6.
Treatments of CPFE and IPF
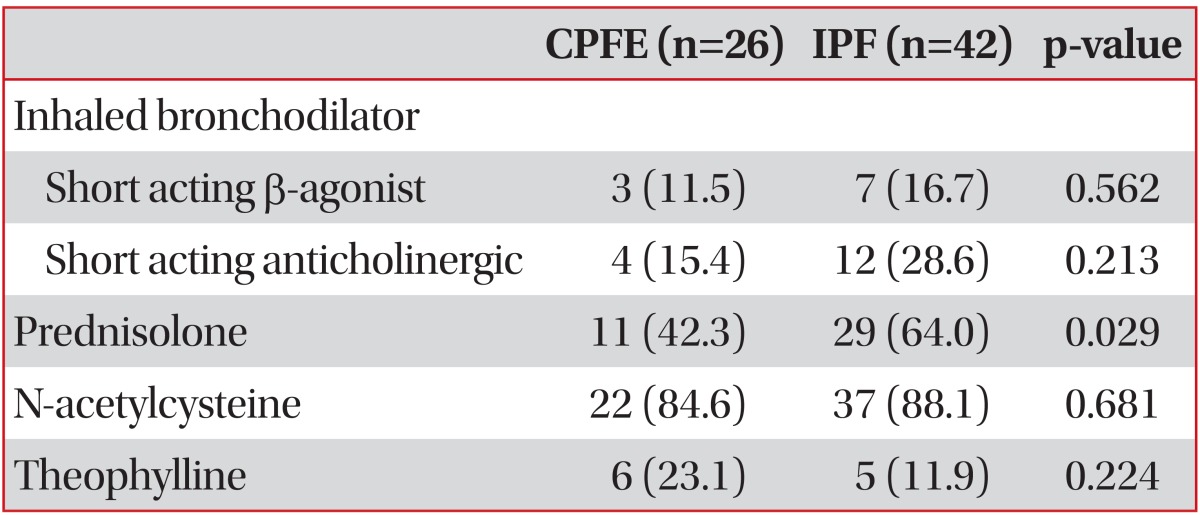
Values are presented as number (%).
CPFE: combined pulmonary fibrosis and emphysema; IPF: idiopathic pulmonary fibrosis.
Prednisolone was significantly difference compared with the CPFE and IPF (p=0.029). At a 64% prescription rate in IPF, which was significantly higher than that of CPFE at 42%. There were no significant differences between the two groups in the prescription rate of other medications such as short acting β-agonists, short acting anticholinergics, theophylline, and N-acetylcysteine.
Discussion
Compared to the baseline PFT, the FEV1/FVC ratio was significantly different between the two groups and was lower in CPFE than in IPF, which is consistent with previous reports2,11,15. Cottin et al.2 reported that the FEV1/FVC in CPFE was lower than the normal range. Mura et al.3 asserted that the existence and range level are important factors promoting decline in pulmonary function including FEV1/FVC. Akagi et al.11 also observed that the baseline FEV1/FVC in CPFE was decreased compared to FEV1/FVC in IPF. Also, they found that the baseline DLco and DLco was decreased to a significantly higher in the CPFE than in the IPF11. But this study report did not reveal a significant difference in the baseline DLco of either group. Moreover, there was no statistically significant difference in the FVC decrease. Over the study follow-up period, change in the FEV1/FVC was disparate between the two groups, a finding similar to that reported by previous study11,15. The FEV1/FVC in IPF remained mostly consistent over the follow-up period, but the ratio significantly decreased in the CPFE during the follow-up period11. Distinct from IPF, CPFE was associated with a progressively obstructive pattern over time, which highlights the importance of bronchodilator therapy in CPFE. In a study comparing CPFE and COPD executed by Kitaguchi et al.15, the FEV1/FVC in CPFE tended to decreased during the follow-up period, like the our study. Patients with CPFE are commonly men with smoking history. It seems most likely that emphysema affected FEV1/FVC decline by the effect of the fibrosis. While Akagi et al.11 reported a significant yearly decline in DLco between the two groups, our data did not show such a trend, indicating the need for additional research. Notably, this study revealed a significantly long duration of cough and sputum in the IPF compared to the CPFE. Moreover, the mean ESR during hospitalization was higher in the IPF. Previous studies reported that CPFE and IPF have similar mortality8,17. But Kurashima et al.6 reported CPFE had better survival compared with IPF. ESR and CRP might show as systemic inflammatory marker in chronic obstructive pulmonary disease18. CRP increases as FEV1% worsens19. It is still uncertain the role of inflammation in IPF. But Mura et al.20 suggested inflammatory activity in IPF is relavant. CPFE have different clinical features such as relation with emphysema and smoking history compared with IPF. So the mean ESR during hospitalization was higher in the IPF. ESR might show as a marker of systemic inflammation in CPFE and IPF. Further study needed whether ESR and the symptom duration may be prognostic indicator. Both groups had a pulmonary artery pressure higher than the normal range, but there was no significant difference between the groups. This result is similar to previous reports showing that the pulmonary hypertension incidence is higher in CPFE patients5,17. Additional prospective studies are needed to clarify the relationship between pulmonary hypertension and CPFE. There are several limitations in this study. First, this is single-center and retrospective study. Second, the assessment of emphysema did not use scoring method of emphysema. Third, we did not measure the exact areas of fibrosis. But, this study showed that the presence of concurrent emphysema in IPF is important factor about prognosis and PFT changes of patient. Further studies investigating the relationship between the obstructive change and short symptom duration in CPFE and prognosis are needed. The study of inflammatory mediators and biomarker in CPFE also merits evaluation through prospective studies.
In conclusion, Annual decrease in FEV1/FVC in CPFE was significantly more than IPF. In addition, this is the report showing the yearly dynamics changes of pulmonary function parameters, and analysis of the frequency and causes of hospitalization in CPFE compared with IPF.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002;165:277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 2.Cottin V, Nunes H, Brillet PY, Delaval P, Devouassoux G, Tillie-Leblond I, et al. Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur Respir J. 2005;26:586–593. doi: 10.1183/09031936.05.00021005. [DOI] [PubMed] [Google Scholar]
- 3.Mura M, Zompatori M, Pacilli AM, Fasano L, Schiavina M, Fabbri M. The presence of emphysema further impairs physiologic function in patients with idiopathic pulmonary fibrosis. Respir Care. 2006;51:257–265. [PubMed] [Google Scholar]
- 4.Jankowich MD, Rounds SI. Combined pulmonary fibrosis and emphysema syndrome: a review. Chest. 2012;141:222–231. doi: 10.1378/chest.11-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grubstein A, Bendayan D, Schactman I, Cohen M, Shitrit D, Kramer MR. Concomitant upper-lobe bullous emphysema, lower-lobe interstitial fibrosis and pulmonary hypertension in heavy smokers: report of eight cases and review of the literature. Respir Med. 2005;99:948–954. doi: 10.1016/j.rmed.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Kurashima K, Takayanagi N, Tsuchiya N, Kanauchi T, Ueda M, Hoshi T, et al. The effect of emphysema on lung function and survival in patients with idiopathic pulmonary fibrosis. Respirology. 2010;15:843–848. doi: 10.1111/j.1440-1843.2010.01778.x. [DOI] [PubMed] [Google Scholar]
- 7.Collard HR, King TE, Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2003;168:538–542. doi: 10.1164/rccm.200211-1311OC. [DOI] [PubMed] [Google Scholar]
- 8.Jankowich MD, Rounds S. Combined pulmonary fibrosis and emphysema alters physiology but has similar mortality to pulmonary fibrosis without emphysema. Lung. 2010;188:365–373. doi: 10.1007/s00408-010-9251-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kitaguchi Y, Fujimoto K, Hanaoka M, Kawakami S, Honda T, Kubo K. Clinical characteristics of combined pulmonary fibrosis and emphysema. Respirology. 2010;15:265–271. doi: 10.1111/j.1440-1843.2009.01676.x. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt SL, Nambiar AM, Tayob N, Sundaram B, Han MK, Gross BH, et al. Pulmonary function measures predict mortality differently in IPF versus combined pulmonary fibrosis and emphysema. Eur Respir J. 2011;38:176–183. doi: 10.1183/09031936.00114010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akagi T, Matsumoto T, Harada T, Tanaka M, Kuraki T, Fujita M, et al. Coexistent emphysema delays the decrease of vital capacity in idiopathic pulmonary fibrosis. Respir Med. 2009;103:1209–1215. doi: 10.1016/j.rmed.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Mejia M, Carrillo G, Rojas-Serrano J, Estrada A, Suarez T, Alonso D, et al. Idiopathic pulmonary fibrosis and emphysema: decreased survival associated with severe pulmonary arterial hypertension. Chest. 2009;136:10–15. doi: 10.1378/chest.08-2306. [DOI] [PubMed] [Google Scholar]
- 13.Usui K, Tanai C, Tanaka Y, Noda H, Ishihara T. The prevalence of pulmonary fibrosis combined with emphysema in patients with lung cancer. Respirology. 2011;16:326–331. doi: 10.1111/j.1440-1843.2010.01907.x. [DOI] [PubMed] [Google Scholar]
- 14.Lim TK. Respiratory failure from combined emphysema and pulmonary fibrosis. Singapore Med J. 1993;34:169–171. [PubMed] [Google Scholar]
- 15.Kitaguchi Y, Fujimoto K, Hayashi R, Hanaoka M, Honda T, Kubo K. Annual changes in pulmonary function in combined pulmonary fibrosis and emphysema: over a 5-year follow-up. Respir Med. 2013;107:1986–1992. doi: 10.1016/j.rmed.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryerson CJ, Hartman T, Elicker BM, Ley B, Lee JS, Abbritti M, et al. Clinical features and outcomes in combined pulmonary fibrosis and emphysema in idiopathic pulmonary fibrosis. Chest. 2013;144:234–240. doi: 10.1378/chest.12-2403. [DOI] [PubMed] [Google Scholar]
- 18.Corsonello A, Pedone C, Battaglia S, Paglino G, Bellia V, Incalzi RA. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) as inflammation markers in elderly patients with stable chronic obstructive pulmonary disease (COPD) Arch Gerontol Geriatr. 2011;53:190–195. doi: 10.1016/j.archger.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 19.Tkacova R, Kluchova Z, Joppa P, Petrasova D, Molcanyiova A. Systemic inflammation and systemic oxidative stress in patients with acute exacerbations of COPD. Respir Med. 2007;101:1670–1676. doi: 10.1016/j.rmed.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 20.Mura M, Belmonte G, Fanti S, Contini P, Pacilli AM, Fasano L, et al. Inflammatory activity is still present in the advanced stages of idiopathic pulmonary fibrosis. Respirology. 2005;10:609–614. doi: 10.1111/j.1440-1843.2005.00757.x. [DOI] [PubMed] [Google Scholar]