Abstract
Background and Purpose:
As the profound health and cost benefits of physical activity to society are established and participation guidelines implemented, health practitioners are increasingly expected to utilize efficacious and justified injury management and prevention strategies. The complex and multifactorial nature of sports injury makes elucidation of multiple risk factors and how they may subtly and variably interact, difficult. The purpose of this case report is to discuss the differential diagnosis, acute management and rehabilitation of a case of medial tibial stress syndrome (MTSS) in a surf life‐saving athlete, in the context of sports injury prevention.
Case Description:
The subject of this case study, a 15 year old female surf life‐saving competitor, presented to the physiotherapist (PT) with recent onset, first episode, bilateral, diffuse posteromedial shin pain. Differential diagnosis, acute management, rehabilitation and preventative strategies for the subject are presented.
Discussion:
Emerging injury surveillance research in surf life‐saving suggests minor and major trauma as primary causative factors, however, the significance of high training volumes is likely underestimated. The influence of biomechanical, and subtle arthrokinematic dysfunctions on established risk factors for MTSS injury and prevention of re‐injury for this subject, are also discussed. Furthermore, the concept of preventing tibial stress fracture (TSF) by successfully managing acute MTSS, is presented. Lastly, a critical analysis of reliability of clinical assessment methodologies utilised with the subject is provided.
Level of Evidence:
Level 5; Single case report
Keywords: Bone stress injury, differential diagnosis, medial tibial stress syndrome, sports injury prevention, tibial stress fracture
BACKGROUND AND PURPOSE
The health and cost benefits of physical activity and sport are well accepted with physical activity now accepted as potent medicine.1‐7 However, the costs associated with sports related injury is not insignificant, both at recreational and professional levels.8‐10 As physical activity implementation strategies evolve, significance of sports injury prevention is likely to further increase, with a growing number of health disciplines expected to demonstrate efficacious management, in an ever increasingly competitive market.10‐14
Sports injury is complex, multifactorial and variable, with a myriad of risk factors, both intrinsic and extrinsic, modifiable and non‐modifiable, likely precipitating a single injury during an ‘inciting event.’15 This has led research methodology to adopt a multivariate analytical approach to sports injury surveillance, however, as the number of interrelated risk factors increases, the strength of their associations likely decreases.15 This renders authors of prospective injury risk factor studies often unable to identify small to moderate associations, due insufficient injury numbers.16 Nonetheless, sports injury prevention practice is also evolving towards establishing efficacy.11‐12,17
Surf lifesaving is an international sport/movement aimed at reducing injury and death around beaches, supported by a comprehensive competitive program.18In Australia, it is largely an amateur, multi‐discipline sport involving athletes from 15 years of age to “open” age, underpinned by a comprehensive junior or ‘nippers’ development program.19 Athletes are eligible for ‘Masters’ competition once they are over 30 years of age. Surf Life Saving Australia (SLSA) is the major organiser of surf sport competition in Australia, with over 310 affiliated surf lifesaving clubs and over 158,000 members nationwide.20 Club, regional, state, national and international competitions, typically called ‘carnivals,’ are held throughout the year, with the domestic Australian season spanning September through March. Carnivals are typically held on weekends, increase in frequency throughout the season and culminate in State and National Championships. Athletes typically train and compete in club squads. Surf sport disciplines include beach and flag sprints, swimming based events, surf craft (surf board and surf ski), surf boat racing, inflatable rescue boat (IRB) racing or other events such as ironman and ironwoman, a combined swim, ski and board event.19‐21 Many events involve short, unshod, beach sprints for transitions and finishes, effecting high impact and torsional loads on athlete's lower limbs, likely potentiating medial tibial stress syndrome (MTSS). A description of events relevant to the case study is presented in Table 1, however, for a complete description of surf life‐ saving events the reader is directed to www.sls.com.au/members/surf‐sport/disciplines.
Table 1.
Description of the subject's surf sport events
| Event & Description | Illustration |
|---|---|
| Swim Surf Race – the Surf Race involves swimmers starting on the beach and then running, wading and swimming about 170metres to sea around a set of buoys and then returning to the beach. The event concludes with a run finish to flags placed on the beach. |  |
| Single surf ski race – from a floating start, competitors paddle their surf ski around three buoys and return to the finish line. The finish is judged when any part of the surf ski crosses the finish line with the competitor and their paddle all in contact. |  |
| Surf board race – Standing start from the beach, each competitor enters the water with their surf board, paddles around all buoys and returns to the beach. The winner is judged by the first competitor to cross the finish line on their feet and in contact with their board. |  |
| Ironwoman‐ The Ironwoman event is conducted over a course consisting of three components, including a swim, a surf ski, and a surf board. The race concludes with a beach sprint to the finish line. The order of the legs may vary and is decided by draw prior to the event. |  |
The accepted definition of MTSS is pain along the posteromedial border of the tibia, typically in the distal third, worse during or just after exercise, with tenderness on palpation of at least 5cm and absence of stress fracture or ischaemic symptoms.22‐24 Likely perpetuating factors for MTSS symptoms in this subject, including potential associations between ankle/foot arthrokinematics, sub‐optimal kinetic chain function and excessive foot pronation, are described. The current understanding of the pathophysiology of MTSS, as well as the potential of preventing tibial stress fracture (TSF) through ‘successful’ management of MTSS, on a bone stress injury (BSI) continuum, with respect to the current scientific body of evidence, is also discussed.22‐23
The purpose of this case report is to discuss the differential diagnosis, acute management, and rehabilitation of a case of medial tibial stress syndrome (MTSS) in a surf life‐saving athlete, in the context of sports injury prevention.
CASE DESCRIPTION
The subject of this case report is 15 year old female surf lifesaving competitor who presented with bilateral MTSS. The subject participated in the swimming surf race, single surf ski, surf board, and ironwoman competitions. Common to many junior surf sport athletes, she participates in individual age and open categories, plus relays, potentially competing in 20 events in one day. Mid‐week training is bi‐daily including strength and conditioning and running‐based fitness work. All beach training and competition is conducted barefoot, whereas road/grass/hill running is carried out shod. The athlete's weekly training schedule is presented in Table 2. The subject approached the physiotherapist (PT) during a carnival near the start of the season, reporting insidious onset, first episode, bilateral, distal third posteromedial shin pain, which started two days earlier after her second hill running session of the season. She did not present to staff for assessment during these two days, retrospectively reporting mild symptoms only, noticeable after running or prolonged walking. She reported a significant worsening of symptoms during the carnival with successive events, until she determined that she was unable to compete effectively. At that time she presented to the PT for this injury. An injury timeline is presented in Appendix1.
Table 2.
Weekly training schedule
| Day | Training |
|---|---|
| Mon: | 0500‐0645 Swim, 1630‐1700 Run, 1700‐1800 Board. |
| Tue: | 0500‐0645 Swim, 1615‐1745 S&C, Run |
| Wed: | Rest AM, 1630‐1700 Run, 1700‐1800 Board |
| Thu: | 0500‐0645 Swim, 1630‐1730 Ski, 1730‐1800 Run |
| Fri: | 0500‐0645 Swim, 1200‐1300 Gym, 1630‐1700 Run, 1700‐1800 Board |
| Sat: | Iron: Ski, Swim & Board, most of the day. |
| Sun: | Rest Day. |
| Other training: | No. |
INITIAL EXAMINATION
Assessment revealed moderate diffuse tenderness in the distal third of both left and right tibias postero‐medially, pain reported with a simple numerical rating scale (SNRS) was 6‐7/10 bilaterally on light palpation, utilizing an adapted 3 point force of palpation scale of light, moderate, and firm.25‐30 The soft tissues adjacent to the implicated area of the distal posteromedial tibia were also tender to palpation, however, this was deduced to be substantially less for the soft tissue compared to the bony tissue (2‐3/10 on moderate palpation). Tibial traction periostitis (TTP) through the soleus, tibialis posterior or flexor digitorum longus, is a popular inflammatory based pathophysiological theory for MTSS, however, this is not supported by studies showing absence of attachment of these muscles in the distal tibia, the most common site for MTSS.22‐23,31‐32 An in‐vitro examinatioin of three cadaveric shanks demonstrated TTP through the deep crural fascia, however, histological and imaging studies are largely unsupportive as fascial or periosteal inflammation are seldom identified.33‐35 This potentially identifies a separate and less common pathophysiological process or transitory state between muscle fatigue and BSI.23,36‐38 Conversely, evidence suggesting MTSS as a non‐focal BSI is stronger, including evidence of diffuse periosteal and bone marrow stress, and local osteopenia which has been shown to resolve concurrently with symptom resolution.35,37,39‐43 The subject showed no signs of significant inflammation, her symptoms were local to the distal third of tibia, and muscle length and resistance testing were unprovocative, suggesting MTSS rather than TTP.22,44
Concomitant subjective examination revealed no significant medical history, no reports of non‐mechanical symptoms such as night or resting pain, no current or previous history of low back pain, nor altered sensation or muscular weakness, indicating that systemic or proximal lumbar causes were highly unlikely and neurological examination unnecessary at that point in time.45 Given absence of resting or night pain, and lack of focal tenderness usually associated with TSF, it was not highly suspected.22‐23.46 Differential diagnosis of early chronic exertional compartment syndrome was provisionally excluded as symptoms were worse rather than better immediately post exercise, and lacked the typical characteristics of muscular tightness, burning sensation or neurological symptoms.22‐23,47 Similarly, popliteal artery entrapment syndrome was not strongly suspected at this time.46‐48 Provisional diagnosis of MTSS was made utilising ‘decision analyses’ in calculating post‐test probabilities of the conditions in this subject's differential diagnoses, by factoring pre‐test probabilities in the clinical demographic factored by estimated likelihood ratios of subjective and physical examination findings.49‐50 A discussion of this process is presented in subsequent sections and is consistent with literature reporting careful history taking and physical examination as the current gold standard for the identification of MTSS.22‐23
Radiographs were not requested as they are unreliable in detecting MTSS.22‐23 Magnetic resonance imaging (MRI), Computerised Tomography (CT) or Three Phase Bone Scan (TPBS) are of limited value in diagnosing MTSS, due to large variability between sensitivity and specificity (Table 3), and currently undetermined relevance to clinical and functional outcomes.22‐23,51 Exception to this is where differential diagnosis is relatively uncertain and imaging may alter the management.22,49 For example, MRI and TPBS can be used to exclude TSF, inter‐compartmental pressure testing is utilized for assessment of exertional compartment syndrome, and indirect or direct angiography utilized for suspected popliteal artery entrapment syndrome.22,37,47
Table 3.
| Imaging Modality | Sensitivity | Specificity |
|---|---|---|
| TPBS | 74‐90% | 33‐100% |
| MRI | 57‐100% | 33‐100% |
| CT | 42‐100% | 88‐100% |
TPBS= Three‐phase bone scan; MRI=Magnetic Resonance Imaging; CT=Computerized Tomography
INITIAL INTERVENTION
As the provisional diagnosis was MTSS rather than TTP, cryotherapy was prescribed to help attenuate symptoms through hypoalgesic effects.52‐54 Advice on application was ice bag with moist cloth for 15 minutes up to every two hours.55 Acetaminophen was permitted as required, however, non‐steroidal anti‐inflammatory drugs were actively discouraged due apparent absence of inflammation, increased side effect profile, and potential to hinder tissue healing.56
The subject was known to have a high weekly training volume (Table 2). She was instructed to rest from further competition that weekend so as not to further exacerbate symptoms and advised she could participate in swim and surf craft training during the week but to avoid any running until formal PT assessment at the weekly strength and conditioning/physiotherapy session midweek. Training volume and activity modification have been shown to be the most effective interventions in MTSS.22‐23,57 This episode led directly to the PT and coaching staff developing a sport specific, rehabilitative staged running guidelines (Table 4). Due to the relative low running component in surf sports (excluding beach and flag sprints), these guidelines potentially allow athletes to safely participate in full competition or maintain high level sport specific training, whilst impact loads with running are diminished.58‐59
Table 4.
Staged Running Guidelines
|
Level 1: Unrestricted |
Unrestricted running at training and competition. |
|
Level 2A: Training restricted |
May compete fully but running restricted at training under direction coach/physio/doctor. |
|
Level 2B: Competition restricted |
Restricted sprinting. May compete but effort of sprint restricted under guidance from coach/physio/doctor (set as a percentage of maximum effort or limited number of repetitions or sets). |
|
Level 3: No running with squad |
Full weight bearing, no running in competition or squad training. May have separate staged running program under direction of PT separate to squad. May train other disciplines under guidance coach/physio/doctor. |
|
Level 4: Protected weight bearing: |
On crutches plus or minus protective orthosis/cast. Training other disciplines to be discussed with coach/physio/doctor. |
Notes: Level 4 for restricted weight bearing. Progress to level 3 when full weight bearing but NO running with squad.Progression to 2A when full surf sport competition is allowed, but running impact loading in training is restricted. 2B is special category where athlete may be allowed to compete but running impact loads are restricted during beach transitions. Level 1, unrestricted. All progressions should be made with full consultation of the multidisciplinary team.
Examination #2 (0.5 weeks after initial examination)
The subject reported being compliant with management advice, had not run and only felt mild symptoms (SNRS VAS 1‐2/10) after walking for approximately 1 hour. Symptom progression throughout management course is presented in Table‐5. She again reported no neurovascular symptoms, resting or night pain, consistent with the initial examination. A quick lumbar screen of active range of movement, combined movement, passive straight leg raise, and passive accessory intervertebral motion was normal, therefore further neurological examination was not deemed necessary at that time. Palpation to the distal posteromedial tibias produced verbal SNRS of 1‐2/10 with light palpation and 5‐6/10 with moderate palpation.
Table 5.
Symptom progression throughout management.course
| Examination | Subjective complaints (SNRS/function) | Objective measure (SNRS/palpation) |
|---|---|---|
| Initial | 3–4/10 immediate with walking, increased attempts to run during carnival | 6–7/10 on light palpation of bony tissue 2–3/10 on moderate palpation of adjacent soft tissue |
| 2 | 1–2/10 with walking approximately 1 hour | 1–2/10 on light palpation 5–6/10 on moderate palpation |
| 3 | 1–2/10 with walking > 1 hour | 0–1/10 on light palpation 2–3/10 on firm palpation |
| 4 | Initial flare up post run 1–2/10 with walk > 15 minutes Resolved within 3 days to 1–2/10 with walk > 1 hour |
0–1/10 on light palpation 2–3/10 on firm palpation |
Muscle length assessments of the lower limb were within normal limits.60‐64 However, despite a normal active and passive physiological ankle dorsiflexion range of motion of approximately 20 degrees bilaterally, talocrural dorsiflexion in knee extension and subtalar neutral was restricted by soft tissue to approximately 20 degrees short of neutral/plantar grade, bilaterally.65‐68 The range approached neutral when the knee was allowed to flex thus the gastrocnemius was primarily implicated. This was likely perpetuating excessive compensatory pronation to achieve adequate segmental dorsiflexion between shank and foot.66‐69 Excessive pronation is a cited risk factor for MTSS, potentially through increased tibial bending or torsion.24,70 All muscle length range assessments by the PT were made using visual estimates of successive midpoints between the horizontal and vertical planes.71 Although instrumented joint angle assessment is advocated wherever possible and practical, particularly for inter‐rater measures, very good intra‐rater reliability of visual estimate of joint range of motion has been demonstrated by experienced clinicians.71‐73
Utilising elements of the Foot Posture Index in standing and calcaneus to tibial alignment during jogging, the subject was classified as an overpronator in static and dynamic weight bearing, respectively, (Table 6).24,74‐77 The subject reported she had previously been prescribed the use of foot orthoses, while shod, by a PT and podiatrist for a previous bout of anterior knee pain (AKP), but had discontinued their use for the previous six months. Not utilising these during shod walking and running was a possible contributor to her developing MTSS symptoms.22‐23,78
Table 6.
Foot Posture Index (FPI)76
| FPI | Left | Right |
|---|---|---|
| 1. Talar head palpation | +2 | +2 |
| 2. Malleolar curves | +1 | +1 |
| 3. Calcaneal position | +1 | +2 |
| 4. Prominence TNJ region | +1 | +1 |
| 5. Congruence MLA | +1 | +1 |
| 6. Ab/Ad forefoot/rearfoot | +1 | +2 |
| TOTAL Score for Subject | +7 | +9 |
Reference Values: Normal 0 to +5; Pronated +6 to +9; Highly Pronated +10 or >; Supinated −1 to −4; Highly Supinated −5 or <. Abbreviations: TNJ (talonavicular joint); MLA (Medial longitudinal arch); Ab (abduction); Ad (Adduction).
As squad athletes had already been screened with a training and vocation related injury questionnaire, created by the PT, at the beginning of the season, the subject had been identified with a history of a previous single episode of bilateral anterior knee pain associated with running, resolved with physiotherapy and podiatry intervention. Kinetic chain screening by the PT during strength and conditioning sessions, identified a tendency to display mild dynamic knee valgus (DKV) bilaterally, particularly with one leg squat, lunging and running.79‐80 The screening was an adapted three point quality of movement scale (‘good’, ‘fair’ or ‘poor’) for observed quality of movement during functional weight bearing activities such as squats, one leg squats, lunges, walking and running, with DKV correspondingly rated as ‘absent’, ‘mild’, or ‘pronounced.’81‐82 DKV likely potentiates MTSS through excessive tibial rotation resulting from excessive pronation and torque conversion at the sub‐talar joint, providing partial explanation for similarities in higher MTSS incidence in females, amongst other lower limb injuries such as patellofemoral pain syndrome, illiotibial band syndrome, and anterior cruciate ligament compromise.22,24,67,80,83‐84 Static muscle testing of muscles of the hip was 5/5 and gluteal function was rated as ‘fair,’ also utilising the PT's adapted movement quality and target muscle recruitment scale based on visual observation, palpation, and subjective reporting of sensation in muscle activation and fatigue, performed in side lying hip abduction, clamshell exercise, and single leg bridge.80‐82,85
Intervention #2
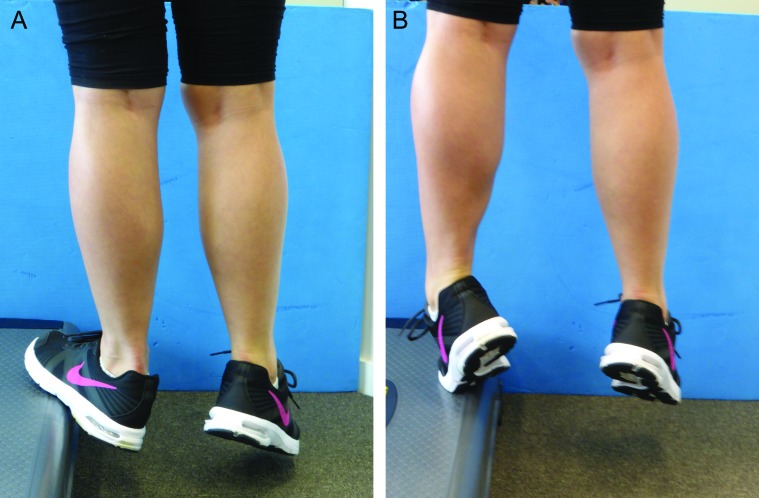
Approximately 6‐8 minutes of light to moderate pressure myofascial release interspersed with 5‐15 second bouts of moderate digital ischaemic pressure was administered to the superficial and deep posterior compartments of each leg, as illustrated by Hutchinson and colleagues,44 aiming to increase talocrural dorsiflexion range and potentially attenuate compensatory hyperpronation.67,86 A home program of calf stretches was prescribed in order to augment an increase in range of talo‐crural dorsiflexion, together with instruction to resume wearing her foot orthoses while shod.69,78,87‐88 Calf stretching was initially prescribed at four repetitions of 15 seconds, alternating sides, four times per day, utilizing a modified weight bearing stretch which is postulated to increase talocrural dorsiflexion and calf stretching by maintaining integrity of the medial longitudinal arch through preferential tension and loading of the plantar fascia (Figure‐1).67‐68,88,‐94 The same stretch but with the knee slightly flexed was prescribed but at decreased frequency, as the soleus was deemed less implicated in this case. All therapeutic exercise parameters including progressions from start point to end goal and preventative maintenance levels are presented in Appendix 2.58‐59.
Figure 1.
A. Gastrocnemius stretch, B. Soleus stretch. Shod weight at level of metatarsal heads and calcaneus utlizing a step, avoiding forefoot abduction.
Remedial gluteal retraining was begun in side lying hip abduction, clamshell exercises and during training sessions with the goal of achieving a ‘good’ rating on the quality of movement scale. Functional integration in one leg squats were introduced next but at low reps, due to the acute nature of the injury.58‐59 The above exercises aimed to improve kinetic chain biomechanics and attenuate DKV, which is a likely neuromuscular driver of foot pronation through ‘torque conversion’ at the sub‐talar joint.67,95‐96. Due to their more dynamic nature compared to single‐leg squats, lunges were withheld at this stage to avoid potentially greater impact and torsional loading forces which were deemed a greater risk for exacerbation of the subject's MTSS symptoms.49,58‐59
Discussion and agreement between PT and coaching staff initiated the subject at level 3 of the staged running guidelines at least until symptoms settled further.58‐59 This allowed full training (swim, surf ski, surf board), while restricting all running impact loads, tying in well with a natural three week break from competition, as there were no carnivals scheduled during that period.
Examination #3 (1.5 weeks after initial examination)
The subject reported she was training swim and surf craft without symptoms and complying with non‐ running status, as instructed. She resumed utilising her foot orthoses while shod, which was also emphasised as preventative maintenance.24,78 She reported pain SNRS of 1‐2/10 after walking over an hour otherwise she was symptom free. Pain on light palpation was 0‐1/10 whereas pain on firm palpation was 2‐3/10.
Whole foot dorsiflexion was unchanged on visual assessment, however, talocrural dorsiflexion in knee extension and subtalar neutral was only 5‐10 degrees from neutral/plantar grade. This represented a substantial improvement towards normalisation of this arthrokinematic index, as in the author's clinical experience, it rarely reaches neutral, without significant soft tissue resistance in non‐children.67,97 Dynamic valgus control of the knees was improved and was rated as ‘good’ in single leg squat, however, still tended to display mild DKV without the subject's conscious attention to the set task. During assessment of calf raise strength and endurance, the subject demonstrated fatigue and deterioration of form from ‘fair’ to ‘poor‘ at 8‐10 repetitions. Assessment of deep posterior compartment strength in calf raise with excursion from eversion to inversion over a step (Figure‐2) showed poor form and inability to perform more than 3‐4 repetitions.
Figure 2.
A. Plantarflexion/inversion strengthening exercise, start position. B. End position
Treatment #3
Due to apparent efficacy in improved talocrural dorsiflexion in subtalar neutral and knee extension, manual soft tissue release and digital ischaemic pressure therapy of the superficial and deep posterior compartments was again administered at 8‐10 minutes per leg with moderate to firm pressure. The subject was instructed to continue gastrocnemius stretching at least bi‐daily. Furthermore, strength and endurance training of the deep and superficial posterior compartments were begun, to offset and prevent muscle fatigue related bone stress, and potentially attenuate overpronation through their actions over the sub‐talar and mid‐tarsal joints.38,46,67,,98 Kinetic chain retraining was progressed to include lunging but was initially restricted to two sets of 5 repetitions on each leg, every other day.58‐59
As the next carnival was two weeks away, coaching staff and the athlete agreed to maintain the subject on 3 of the staged running protocol.58‐59 This ensured she would not run with the squad, however, was able to start running under the strict guidance of the PT. This was begun as 5 minutes of shod light jogging on a grass surface, every other day, with a 2 minute progression each day. At that point in time the injury was considered in the sub‐acute stage, with some potential to irritate symptoms, hence the subject was instructed to cease the running program immediately if symptoms were at all more noticeable than prior to starting running.49,58‐59 This is consistent with treating symptoms of MTSS symptomatically unless symptoms are significant and persistent, or TSF is suspected, whereby a minimum rest period irrespective of symptoms should be enforced.46,49,58‐59
Examination #4 (2.5 weeks after initial examination)
The subject reported ceasing the graduated running program after the first jogging session due to resulting mild symptom provocation. This was reported as 1‐2/10 pain with walking longer than 10‐15 minutes (Previously 1‐2/10 pain with walking for an hour) which resolved to previous level within two to three days. Palpation of the posteromedial tibias again revealed diffuse tenderness in the distal third, rated on SNRS as 0‐1 on light palpation and 2‐3/10 on firm palpation. Talocrural dorsiflexion in knee extension and sub‐talar neutral was also in status quo to Examination #3. Static and through range resisted muscle tests were again unprovocative. Diagnosis of MTSS was unchanged and the subject was considered to have sustained a mild flare up resulting from running, which appeared to have settled to previous levels within a week.
Intervention #4
Soft tissue release and digital ischaemic pressure were repeated as per previous session. Remedial gluteal retraining, one leg squats and lunges were reviewed and progressed. Remedial core exercises such as single leg bridging, planking, and side planking were introduced as trunk stability likely plays an important role in lower limb biomechanics and injury.80,99‐103
Due to low suspicion of TSF and only minor running elements to the subject's surf sport disciplines, the PT, coach and athlete agreed to progress her status to Level 2A in the staged running protocol.58‐59 This would limit the overwhelming majority of impact loading related to running, however, would allow the subject to compete and prepare for State and National Titles. In order to maintain athlete safety, she was given strict instruction that she was able to compete only if her MTSS symptoms were gradually improving from week to week, and if symptoms were not improving she must report it to staff.49,58‐59
Subsequent Interventions and Outcomes
The subject competed the following week with symptoms remaining in status quo. MTSS symptoms gradually abated and were fully resolved at approximately 8 weeks after initial onset. She competed in at least another two carnivals during this period. The subject gradually resumed running with the squad at 10 weeks and was upgraded to Level 1 of the staged running guidelines at 12 weeks post injury, and thereafter trained and competed asymptomatically for the rest of the season.
DISCUSSION
Not until recently have surf lifesaving injury incidence patterns been reported.20 A list of the most commonly reported injuries and primary contributing factors are presented in Tables 7&8, respectively.20 The overwhelming majority of injuries reported appear related to minor or major trauma, however, this may be somewhat skewed by the nature of the injury reporting methods utilised.11,20,104 Many athletes training for multiple disciplines or endurance events, where overuse symptoms may affect training or competition performance, often will not present to formal first aid stations, thus underestimating the incidence and prevalence of injury. Furthermore, traumatic injuries reported may merely represent the inciting event or the interplay of a myriad of preceding risk factors, including overuse.15‐16 This potentially provides a future injury research agenda for the sport.11
Table 7.
Five most common primary contributing factors reported as associated with injury occurrence during Surf Life-saving competition and training20
| Nature of Injury | %Incidence Competition | %Incidence Training |
|---|---|---|
| 1.Bruise/Contusion | 15.2 | 14.9 |
| 2.Strain | 14.8 | 11.2 |
| 3.Inflammation/Swelling | 12.3 | 12.1 |
| 4.Sprain | 11.9 | 11.0 |
| 5.Open wound/laceration | 9.7 | 10.9 |
Table 8.
Five most common primary contributing factors reported as associated with injury occurrence during Surf Life‐saving competition and training20
| Contributing Factor | % Reported Competition | % Reported Training |
|---|---|---|
| 1.Returning to shore | 19.5 | 15.1 |
| 2.Negotiating the break | 17.5 | 24.7 |
| 3.Collision with | 9.8 | 4.5 |
| 4.Lost control own craft | 7.0 | 8.1 |
| 5.Other person lost control of craft | 5.5 | 3.9 |
Propositional risk factors for MTSS identified with this subject were female sex and excessive foot pronation.22‐23 Although presently not propositionally supported as risk factors for MTSS, decreased talocrural dorsiflexion in sub‐talar neutral and DKV were considered relevant to injury onset, successful rehabilitation and future prevention of re‐injury in this subject, likely thorough their effects on pronation.80,83 It is difficult to ascertain whether temporally the primary driver is DKV causing excessive pronation and subsequently perpetuating calf tightness, or, vice versa.67,69,80,84,101 The two mechanisms may be synergistic or part of the same biomechanical dysfunction in certain individuals, increasing tissue loading and potentiating injury.15 However, once the calf musculature is restricting talocrural dorsiflexion in the neutral sub‐talar joint position, the likely ‘path of least resistance’ to achieve adequate dorsiflexion between shank and foot is compensatory excessive foot pronation.67,69,91 Prospective research has not identified calf tightness as a risk factor for MTSS, however, measuring whole foot dorsiflexion may not fully elucidate these subtle arthrokinematic relationships.15‐16,105 Similarly, the inter‐relationships between potential MTSS risk factors such as training parameters and footwear, are yet to be propositionally elucidated.15‐16,22‐23
Outcome in this case was full resolution of symptoms at eight weeks post injury, resumption of unrestricted running with squad training at 12 weeks, and uninterrupted participation throughout the entire competitive season. It could be argued that the symptom resolution rate in this case of MTSS was rather modest, however, it may at least be partially explained by maintenance of this subject's competitive status throughout, while restricting her running impact loads during training, due to mild residual symptoms, prolonging their course. There were several focal lower limb BSI amongst the female squad members, thus club wide preventative educational strategies on stress fractures and female athlete triad were undertaken. But how relevant was this to MTSS? MTSS is a form of diffuse or non‐focal BSI, which has been shown to progress to linear micro crack formation with progressive loading in animal and a limited number studies of human subjects.106‐107 These stress responses likely vary with age and loading direction, and are probably confounded by factors such as gender, bone microstructure, nutrition, biomechanics, training terrain, footwear and pain perception.70,108‐110 Combined with research showing abnormal imaging in asymptomatic subjects, this suggests current difficulty in predicting if any one individual with MTSS will progress to TSF.22,40‐41,111 However, amongst populations and sports where numbers of cases presenting with MTSS is high, such as running and the military, it is not improbable that successful management of acute MTSS could prevent progression to TSF in some of these cases.22
Finally, a critical discussion on the methodology in the differential diagnosis of MTSS in this case study is warranted. The use of ‘decision analysis’ in estimating post‐test probabilities of the conditions in the differential diagnoses by factoring pre‐test probability of the clinical demographic with likelihood ratios of subjective and objective examination tests, requires elaboration. For example, utilizing a Nomogram and a conservative estimate of pre‐test probability of MTSS in this subject (50%), and a positive likelihood ratio for positive diffuse, distal third posteromedial tibial tenderness on palpation (2.0), the post‐test probability of MTSS being present is approximately 7 in 10.49‐50,78,112‐113 Conversely, utilising the same methods with a liberal pre‐test probability estimate for TSF in this clinical demographic (20%), factored by the same magnitude but negative likelihood ratio, (‐2.0), for absence of focal tenderness, yields a post‐test probability of less than 1 in 10 that TSF is present.49‐50,78,112 Furthermore, there is moderate evidence to suggest a thorough subjective examination should provide larger positive and negative values for likelihood ratios than the physical examination.44,50,114‐116 This becomes a form of diagnostic test clustering which is likely to accentuate post‐test probabilities.49,117‐118 However, it must be acknowledged that pre‐test probabilities are often estimated conservatively based on clinical experience rather than propositional data, and likelihood ratios, in this case, were estimated from the limited data available.50,78,113.
Secondly, a limitation of the case report was that physical examination was primarily dependent on subjective reporting on a SNRS whilst the PT administered conventional manual palpation of an estimated force magnitude of mild, moderate or firm. Bendtsen & Co‐workers (1996) demonstrated good intra‐rater reliability for constant force conventional muscular palpation compared with instrumented palpometry, however, they utilised a modified Total Tenderness Scoring system rather than a SNRS.25 Similarly, a recent study by Kothari & colleagues found no significant differences in variability between with manual palpation with left or right hands, middle or index fingers, soft or hard surface, and 2 versus 10 second palpation.30 These authors did consistently demonstrate significantly lower coefficients of variation (CV) for all instrumented test conditions utilising a palpometer (Mean CV: 4.8%; Range: 2.7%‐5.8%), compared to standard manual palpation (Mean CV 13.0%; Range: 10.0‐17.8%).27 However, applying their highest CV for manual palpation (17.8%) to their outer range and median palpation pressures of 0.5kg, 1.75 kg and 3kg, as representing a light, moderate or firm palpation rating, respectively, is unlikely to affect reliability.30 The above data is consistent with the premise that objective instrumented palpation may be required for constructs where inter‐rater reliability is necessitated, for example, research, or atypically formal assessment, whereas astute manual palpation by the same clinician is likely sufficient for day to day clinical practice.25,27,30 Lastly, the limitations of goniometric assessment of ankle dorsiflexion range of motion has been described above, and visual estimates of joint range of motion are generally not accepted in research literature.
CONCLUSIONS
Sports injury is multifactorial, complex, and variable, which presents a challenge to health practitioners in establishing efficacious and propositionally justified sports injury management prevention strategies. This case describes the differential diagnosis, acute management and rehabilitation of MTSS in a 15 year old female surf life‐saving athlete, in the context of sports injury prevention. Concurrently, a case supporting the notion of some MTSS cases as precursors of TSF is presented.
Acknowledgements
Maroochydore Surf Life Saving Club, Surf Life Saving Australia, MyPhysio GESAC, Melbourne, Australia, Review and editorial staff, International Journal of Sports Physical Therapy.
Appendix 1.
Injury Timeline
| Examination | Days from Initial examination | Progress/Management |
|---|---|---|
| Initial | 0 days | Symptoms at their worst. Cease further competition that weekend, no running at least until mid‐week full assessment, Able train swim and surf craft, cryotherapy, simple analgesics prn |
| Exam #2 | 3 Days | Significantly improved, mild symptoms. Soft tissue release, calf stretching, remedial gluteal work begun, advised to resume wearing foot orthoses, Level 3 on staged running proforma (no running with squad, able to train surf craft), no carnivals scheduled for 3.5 weeks, cryotherapy prn |
| Exam #3 | 10 Days | Significantly improved, symptoms minimal. Continue soft tissue work, stretching, foot orthoses, progress hip stability exercises, add lunges. Maintain Level 3 running proforma: no squad running but prescribed 5 minute light jog on grass. Next carnival 2.5 weeks away. |
| Exam #4 | 17 Days | Mild flare up with initial session of graduated jogging program, settled within the week. Next carnival 1.5 weeks away. Due to subjects low running demands during competition, athlete, coach & PT agree to place on 2A of running proforma (full competition, no running at training) Gradually progress above exercises, add trunk stability. |
| Subsequent Exams | Weekly throughout season | Symptoms gradually abated. All exercises progressed. Competes in subsequent weeks with nil ill effect. Asymptomatic at 8 weeks, running at training gradually re‐introduced from week 10, upgraded to Level 1 of running proforma at 12 weeks. Competes asymptomatically for the rest of season. Preventative maintenance strategies. |
Note: PT exams and treatment were scheduled weekly during strength and conditioning sessions, PT was available on call between scheduled sessions, as required.
Appendix 2.
Details of therapeutic exercise interventions
| Exercise | Start dose | Progression (as tolerated) | End goal | Preventative maintenance |
|---|---|---|---|---|
| Gastrocnemius stretch | 4 × 20secs each leg, alternating, 4×/day plus after activity | 4 × 20secs each leg alternating 2/day plus after activity | Neutral talocrural dorsiflexion in subtalar neutral | 4× 20secs after activity. Allowed pre‐ activity as part of sport specific warm‐up |
| Hip abduction side‐lye | 2 sets, 6‐8 reps, daily | 2‐3 reps per session, daily unless fatigued | 2‐3 sets, 20 reps | 1‐2/week |
| Clams in side lye | 2 sets, 6‐8 reps, daily | 2‐3 reps per session, daily unless fatigued | 2‐3 sets, 20 reps | 1‐2/week |
| One leg squats | 2 sets, 5reps each leg, daily | 2‐3 reps each session, every other day when reps >10 or if fatigued | 2‐3 sets, 20 reps | 1‐2/week |
| Calf raise (straight and bent knee) | 2 sets, 6 reps, each leg, daily | 2‐3 reps each session, every other day when reps > 10 or fatigued | 2‐3 sets, 20 reps | 1‐2/week |
| Eversion to inversion calf raise for deep posterior compartment | 2 sets, 2‐3 reps, each leg, daily unless fatigued | 1‐2 reps each session, every other day when reps >10 or fatigued | 2 sets, 15‐20 reps | 1/week |
| Lunges | 2×5 | 2‐3 reps per | 2‐3 sets 20 | 1‐2 per week |
| each leg every other day, unless fatigued or increased symptoms | session | repetitions | ||
| 1 Leg Bridge | 10secs (L) then (R) = 1 rep, start 4‐5 reps, daily | 1‐2 reps per session | 10 reps | 1‐2/week |
| Plank (elbow feet) | 5 × 20secs, daily unless fatigued | 5secs per session up to 5×45secs then elbow/1foot | 5 × 45secs | 1‐2/week |
| Side plank (elbow/leg) | 5×20 secs, daily unless fatigued | 5secs/session up to 5× 45 secs, then elbow/leg | 5 × 45secs | 1‐2/week |
References
- 1.Booth F. Gordon S Carlson C. Hamilton M. (2000). Waging the war on modern chronic diseases: primary prevention through exercise biology. J Appl Physiol. 2000; 88 (2): 774‐787 [DOI] [PubMed] [Google Scholar]
- 2.Blair S. (2009). Physical inactivity: The biggest public health problem of the 21st century. Br J Sports Med. 2009; 43 (1): 1‐2 [PubMed] [Google Scholar]
- 3.Davis J. Marra C. Robertson M. Khan K. et al. Economic evaluation of dose‐ response resistance training in older women: a cost‐effectiveness and cost‐utility analysis. Osteoporos Int, 2011; 22 (5): 1355‐1366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis J. Blair S. Sports and exercise medicine: Addressing the world's greatest public health problem. In: Brukner P Khan K; Clinical Sports Medicine. (2013); McGraw Hill [Google Scholar]
- 5.Katzmarzyk P. T. Janssen I. (2004). The economic costs associated with physical inactivity and obesity in Canada: An update. Can J Appl Physiol. 2004; 29(1), 90‐115 [DOI] [PubMed] [Google Scholar]
- 6.O'Donovan G. Blazevich A. J. Boreham C. Cooper A. R., et al. (2010). The ABC of Physical Activity for Health: A consensus statement from the British Association of Sport and Exercise Sciences. J Sports Sci.. 2010; 28(6), 573‐591 [DOI] [PubMed] [Google Scholar]
- 7.Zheng H. Ehrlich F. Amin J. (2010). Economic evaluation of the direct healthcare cost savings resulting from the use of walking interventions to prevent coronary heart disease in Australia. Int J Health Care Finance Econ. 2010; 10(2), 187‐201 [DOI] [PubMed] [Google Scholar]
- 8.Finch C. Cassell E. The public health impact of injury during sport and active recreation. J Sci Med Sport. 2006; 9(6), 490‐497 [DOI] [PubMed] [Google Scholar]
- 9.Hagglund M Walden M Magnusson H Kristenson K et al. Injuries affect team performance negatively in professional football: an 11 year follow‐up of the UEFA Champions League injury study. Br J Sports Med. 2013; 47, 807‐808 [DOI] [PubMed] [Google Scholar]
- 10.Lyons R. Finch C. Mclure R Van Beek E., et al. The injury list of all deficits (LOAD) framework‐ conceptualising the full range of deficits and adverse outcomes following injury and violence. International Journal of Injury Control and Safety Promotion. 2010; 17 (3): 145‐159 [DOI] [PubMed] [Google Scholar]
- 11.Finch C. A new framework for research leading to sports injury prevention. J Sci Med Sport. 2006; 9: 3‐9 [DOI] [PubMed] [Google Scholar]
- 12.Mahler P Donaldson A. (2010). The limits of prevention‐sports injury as an example. International Journal of Injury Control and Safety Promotion. 2010; 17(1), 69‐72 [DOI] [PubMed] [Google Scholar]
- 13.Morrow J. Defina L. Leonard D. Trudell‐Jackson E., et al. Meeting physical activity guidelines and musculoskeletal injury: The WIN study. Med Sci Sports Exerc. 2012; 44 (10): 1986‐1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shepphard L. Analysis of the physiotherapy industry: Challenges for marketing. Health Marketing Quarterly. 1991; 14 (2): 35‐42 [DOI] [PubMed] [Google Scholar]
- 15.Meeuwisse W. Assessing causation in sports injury: A multifactorial model. Clin J Sports Med. 1994; 4: 166‐170 [Google Scholar]
- 16.Bahr R. Holme I. Risk factors for sports injuries‐A methodological approach. Br J Sports Med. 2003; 37: 384‐392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Mechelen W. Hlobil H Kemper HCG. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. 1992; 14 (2): 82‐99 [DOI] [PubMed] [Google Scholar]
- 18.International Life Saving Federation. (2014) www.ilsf.org
- 19.Surf Life Saving Australia. (2014). www.slsa.com.au
- 20.Mitchell R. Brighton B. Sherker S. (2013). The epidemiology of competition and training‐based surf sport‐related injury in Australia, 2003‐2011. J Sci Med Sport. 2013; 16:18‐21 [DOI] [PubMed] [Google Scholar]
- 21.Surf Life Saving Australia. Australian surf sports manual. 2008; No 3, 33rd ed. Sydney, Surf Life Saving Australia [Google Scholar]
- 22.Moen M. Tol J. Weir A. Steunebrink M., et al. Medial tibial stress syndrome. A critical review. Sports Med. 2009; 39(7), 523‐546 [DOI] [PubMed] [Google Scholar]
- 23.Reshef N. Guelich D. Medial Tibial Stress Syndrome. Clin Sports Med. 2012; 31: 273‐290 [DOI] [PubMed] [Google Scholar]
- 24.Yates B. White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med. 2004; 32 (3): 772‐780 [DOI] [PubMed] [Google Scholar]
- 25.Bendtsen L. Jensen R. Jensen N. Olesen J. Pressure‐controlled palpation: a new technique which increases the reliability of manual palpation. Cephalgia. 1995; 15:205‐210 [DOI] [PubMed] [Google Scholar]
- 26.Ferreira‐Valente M. Pais‐Ribeiro J. Jensen M (2011). The validity of four pain rating scales. Pain. 2011; 152:2399‐2404 [DOI] [PubMed] [Google Scholar]
- 27.Kothari S. Kothari M. Zambra R. Baad‐Hansen L., et al. Standardisation of muscle palpation‐Methodological considerations. Clin J Pain. 2014; 30 (2):174‐182 [DOI] [PubMed] [Google Scholar]
- 28.Price D. McGrath P. Rafii A Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983; 45‐56 [DOI] [PubMed] [Google Scholar]
- 29.Price D. Bush F. Long S. (1994). A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994; 56: 217‐226 [DOI] [PubMed] [Google Scholar]
- 30.Langemark M. Jensen K. Jensen T. Olesen J. Pressure pain thresholds and thermal nociceptive thresholds in chronic tension‐type headache. Pain. 1989; 38:203‐210 [DOI] [PubMed] [Google Scholar]
- 31.Bradshaw C. Hislop M. Hutchinson M. Shin Pain. In: Brukner P. Khan. K. Clinical Sports Medicine. 2006; 3rd Edition, McGraw‐Hill, Australia [Google Scholar]
- 32.Stickley C. Hetzler R. Kimura I. Lozanoff S. Crural fascia and muscle origins related to medial tibial stress syndrome symptom location. Med Sci Sports Exerc. 2009; 41(11), 1991‐1996 [DOI] [PubMed] [Google Scholar]
- 33.Bhatt R. Lauder I. Finlay D. B. Allen M. J. Belton I. P. Correlation of bone scintigraphy and histological findings in medial tibial syndrome. Br J Sports Med. 2000; 34(1), 49‐53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bouche R. Johnson C. Medial tibial stress syndrome (tibial fasciitis) ‐ A proposed pathomechanical model involving fascial traction. Journal of the American Podiatric Medical Association. 2007; 97(1), 31‐36 [DOI] [PubMed] [Google Scholar]
- 35.Johnell O. Rausing A. Wendeberg B. Westlin N. Morphological bone changes in shin splints. Clin Orthop and Rel Res. 1082; (167), 180‐184 [PubMed] [Google Scholar]
- 36.Aoki Y. Yasuda K. Tohyama H. Ito H. Minami A. Magnetic resonance imaging in stress fractures and shin splints. Clin Orthop Rel Res. 2004; 421, 260‐267 [DOI] [PubMed] [Google Scholar]
- 37.Gaeta M. Minutoli F. Scribano E. Ascenti G., et al. CT and MR imaging findings in athletes with early tibial stress injuries: Comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005; 235(2), 553‐561 [DOI] [PubMed] [Google Scholar]
- 38.Milgrom C Radeva‐Petrova D. Finestone A. Nyska M, et al. The effect of muscle fatigue on in vivo tibial strains. J Biomech.. 2007; 40(4), 845‐850 [DOI] [PubMed] [Google Scholar]
- 39.Batt M. Ugalde V. Anderson M Shelton D. A prospective controlled study of diagnostic imaging for acute shin splints. Med Sci Sports Exerc. 1998; 30 (11), 1564‐1571 [DOI] [PubMed] [Google Scholar]
- 40.Chisin R. Milgrom C. Giladi M. Stein M., et al. Clinical‐significance of nonfocal scintigraphic findings in suspected tibial stress‐fractures. Clin Orthop Rel Res. 1987; (220), 200‐205 [PubMed] [Google Scholar]
- 41.Gaeta M. Minutoli F. Vinci S. Salamone I., et al. High‐resolution CT grading of tibial stress reactions in distance runners. Am J Roentgenol. 2006; 187(3), 789‐793 [DOI] [PubMed] [Google Scholar]
- 42.Magnusson H. Westlin N. Nyqvist F. Gardsell P., et al. Abnormally decreased regional bone density in athletes with medial tibial stress syndrome. Am J Sports Med. 2001; 29(6), 712‐715 [DOI] [PubMed] [Google Scholar]
- 43.Magnusson H. Ahlborg H. Karlsson C. Nyquist F., et al. Low regional tibial bone density in athletes with medial tibial stress syndrome normalizes after recovery from symptoms. Am J Sports Med.. 2003; 31(4), 596‐600 [DOI] [PubMed] [Google Scholar]
- 44.Hutchinson M. Bradshaw C. Hislop M. Leg Pain. In: Brukner P. Khan K. Clinical Sports Medicine. 2013; 4th edition, McGraw‐Hill, Australia [Google Scholar]
- 45.Refshauge K. M. Maher C. G. Low back pain investigations and prognosis: a review. Br J Sports Med. 2006; 40(6), 494‐498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ng J. Grady M. Shin and lower pain. In: Koutres C. Wong V. Pediatric Sports Medicine: Essentials for Office Evaluation. 2013; Thorofare, NJ, USA: SLACK Incorporated [Google Scholar]
- 47.Brewer R. Gregory A. Chronic lower leg pain in athletes: A guide for the differential diagnosis, evaluation and treatment. Sports Health. 2012; 4 (2): 121‐127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gallo R. Plakke M. Silvis M. Common leg injuries of long distance runners: Anatomical and biomechanical approach. Sports Health. 2012; 4 (6)., 485‐495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fritz J. M. Wainner R. S. Examining diagnostic tests: An evidence‐based perspective. Phys Ther. 2001; 81(9), 1546‐1564 [DOI] [PubMed] [Google Scholar]
- 50.Bernstein J. Decision analysis. J Bone Joint Surg Am. 1997; 79 (9):1404‐1414 [DOI] [PubMed] [Google Scholar]
- 51.Moen M. Schmikli S. Weir A. Steeneken V. Stapper G. De Slegte R. Tol J. Backx F. A prospective study on MRI findings and prognostic factors in athletes with MTSS. Scand J Med Sci Sports. 2014; 24:204‐210 [DOI] [PubMed] [Google Scholar]
- 52.Andrish J. Bergfeld J Walheim J. Prospective study on management of shin splints. J Bone Joint Surg Am. 1974; 56 (8), 1697‐1700 [PubMed] [Google Scholar]
- 53.Bizzini M. Ice and modern sports physiotherapy: Still cool? Br J Sports Med, 2012; 46 (4), 218‐219 [Google Scholar]
- 54.Bleakley C. Glasgow P. Webb M. Cooling an acute muscle injury: Can basic scientific theory translate into the clinical setting? Br J Sports Med. 2012; 46:496‐498 [DOI] [PubMed] [Google Scholar]
- 55.http://e-firstaid.stjohn.org.au/text_alt/topic_08/index.html
- 56.Paoloni J. A. Milne C. Orchard J. Hamilton B. Non‐steroidal anti‐inflammatory drugs in sports medicine: guidelines for practical but sensible use. Br J Sports Med. 2009; 43(11), 863‐865 [DOI] [PubMed] [Google Scholar]
- 57.Winters M. Eskes M. Weir A. Moen M., et al. Treatment of medial tibial stress syndrome: A systematic review. Sports Med. 2013; 43: 1315‐1344 [DOI] [PubMed] [Google Scholar]
- 58.Brody L. Effective therapeutic exercise prescription: The right exercise at the right dose. J Hand Ther. 2012; 25:220‐232 [DOI] [PubMed] [Google Scholar]
- 59.Marr D. Care of the multisport athlete: Lessons from Goldilocks. Br J Sports Med. 2011; 45 (14):1086‐1087 [DOI] [PubMed] [Google Scholar]
- 60.Bohannon R. Gajdosik R. LeVeau B. Contribution of pelvic rotation and lower limb motion to increases in the angle of passive straight leg raising. Phys Ther. 1985; 65(4): 474‐476 [DOI] [PubMed] [Google Scholar]
- 61.Corkery M. Briscoe H. Ciccone N. Foglia G., et al. Establishing normal values for lower extremity muscle length. Phys Ther Sport. 2007; 8: 66‐74 [Google Scholar]
- 62.Ferber R. Kendal K. McElroy L. Normative and critical criteria for iliotibial band and iliopsoas muscle flexibility. Journal of Athletic Training. 2010; 45(4):344‐348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Toppenberg R. Bullock M. Normal lumbo‐pelvic muscle lengths and their interrelationships in adolescent females. Australian Journal of Physiotherapy. 1990; 36:105‐109 [DOI] [PubMed] [Google Scholar]
- 64.Youdas J. Krause D. Hollman J. Harmsen W., et al. The influence of gender and age on hamstring muscle length in healthy adults. J Orthop Sports Phys Ther. 2005; 35: 246‐252 [DOI] [PubMed] [Google Scholar]
- 65.Elveru R. Rothstein J. Lamb R. Goniometric reliability in a clinical setting: Subtalar and ankle joint measurements. Phys Ther. 1988; 68: 672‐677 [DOI] [PubMed] [Google Scholar]
- 66.Moseley A. Crosbie J. Adams R. Normative data for passive ankle plantar flexion‐dorsiflexion flexibility. Clinical Biomechanics. 2001; 16:514‐521 [DOI] [PubMed] [Google Scholar]
- 67.Tiberio D. Evaluation of functional ankle dorsiflexion using subtalar neutral position ‐ a clinical report. Phys Ther. 1987; 67(6), 955‐957 [DOI] [PubMed] [Google Scholar]
- 68.Tiberio D. Bohannon R. Zito M. Effect of subtalar joint position on the measurement of maximal ankle dorsiflexion. Clinical Biomechanics. 1989; 4:189‐191 [DOI] [PubMed] [Google Scholar]
- 69.Jung D. Koh E. Kwon O. Yi C., et al. Effect of medial arch support on displacement of the myotendinous junction of the gastrocnemius during standing wall stretching. J Orthop Sports Phys Ther. 2009; 39(12), 867‐874 [DOI] [PubMed] [Google Scholar]
- 70.Diab T. Vashishth D. Effects of damage morphology on cortical bone fragility. Bone. 2005; 37(1), 96‐102 [DOI] [PubMed] [Google Scholar]
- 71.Blonna D. Zarkadas P. Fitzsimmons J. O'Driscoll S. Accuracy and inter‐observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Sury, Sports Traumatol, Arthrosc.. 2012; 20:1378‐1385 [DOI] [PubMed] [Google Scholar]
- 72.Youdas J. Bogard C. Suman V. Reliability of goniometric measurements and visual estimates of ankle joint active range of motion obtained in a clinical setting. Arch Phys Med Rehabil. 1993; 74:113‐118 [DOI] [PubMed] [Google Scholar]
- 73.Watkins M. Riddle D. Lamb R. Personius W. Reliability of goniometric measurements and visual estimates of knee range of motion in a clinical setting. Phys Ther. 1991; 71:90‐96 [DOI] [PubMed] [Google Scholar]
- 74.Gehlsen G. Seger A. Selected measures of angular displacement, strength, and flexibility in subjects with and without shin splints. Res Q Exerc Sport. 1980; 51 (3), 478‐485 [DOI] [PubMed] [Google Scholar]
- 75.Keenan A. Redmond A. Horton M. Conaghan P., et al. The Foot Posture Index: Rasch analysis of a novel, foot specific outcome measure. Arch Phys Med Rehabil. 2007; 88 (1):88‐93 [DOI] [PubMed] [Google Scholar]
- 76.Redmond A. Crosbie J. Ouvier A. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clinical Biomechanics (Bristol, Avon). 2006; 21 (1):89‐98 [DOI] [PubMed] [Google Scholar]
- 77.Viitasalo J. Kvist M. Some biomechanical aspects of the foot and ankle in athletes with and without shin splints. Am J Sports Med. 1983; 11 (3):125‐130 [DOI] [PubMed] [Google Scholar]
- 78.Franklyn‐Miller A. Wilson C. Bilzon J. McRory P. Foot orthoses in the prevention of injury in initial military training: A randomized controlled trial. Am J Sports Med. 2011; 39: 30‐37 [DOI] [PubMed] [Google Scholar]
- 79.Karandikar N. Vargas O. Kinetic chains. A review of the concept and it's clinical implications. Physical Medicine and Rehabilitation. 2011; 3:739‐745 [DOI] [PubMed] [Google Scholar]
- 80.Powers C. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J Orthop Sports Phys Ther. 2010; 40(2), 42‐51 [DOI] [PubMed] [Google Scholar]
- 81.Crossley K. Zhang W. Schache A. Bryant A. Cowan S. Performance on the single‐leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011; 39, 866‐873 [DOI] [PubMed] [Google Scholar]
- 82.Piva S. Fitzgerald K. Irrgang J Jones S., et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskeletal Disorders. 2006; 7:33‐. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Burne S. Khan K. Boudville P. Newman P., et al. Risk factors associated with exertional tibial pain: a twelve months prospective clinical study. Br J Sports Med. 2004; 38(4), 441‐445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Myer G. Brent J. Ford K. Hewett T. Real‐time assessment and neuromuscular training feedback techniques to prevent anterior cruciate ligament injury in female athletes. Strength and Conditioning Journal. 2011; 33(3), 21‐35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Grimaldi A. Assessing lateral stability of the hip and pelvis. Manual Therapy. 2011; 16: 26‐32 [DOI] [PubMed] [Google Scholar]
- 86.Grieve R. Clark J. Pearson E. Bullock S., et al. The immediate effect of soleus trigger point pressure release on restricted ankle joint dorsiflexion: A pilot randomised controlled trial. Journal of Bodywork and Movement Therapies. 2011; 15(1), 42‐49 [DOI] [PubMed] [Google Scholar]
- 87.Loudon J. Dolphino M. Use of foot orthoses and calf stretching for individuals with medial tibial stress syndrome. Foot & ankle specialist. 2010; 3(1), 15‐20 [DOI] [PubMed] [Google Scholar]
- 88.Nakamura M. Ikezoe T. Takeno Y. Ichihashi N. Effects of a 4‐week static stretch training program on passive stiffness of human gastrocnemius muscle‐tendon unit in vivo. Eur J Appl Physiol. 2012; 112:2749‐2755 [DOI] [PubMed] [Google Scholar]
- 89.Ayala F. Sainz de Baranda P, Effect of 3 different active stretch durations on hip flexion range of motion. Journal of Strength and Conditioning Research. 2010; 24 (2), 430‐436 [DOI] [PubMed] [Google Scholar]
- 90.Fuller E. The windlass mechanism of the foot: A mechanical model to explain pathology. Journal of the American Podiatric Medical Association. 2000; 70 (1): 35‐46 [DOI] [PubMed] [Google Scholar]
- 91.Kasuyama T. Sakamoto M. Kato K. Comparing changes in the calf muscle during weight‐bearing and non‐weight‐bearing stretching. J Phys Ther Sci. 2011; 23: 395‐399 [Google Scholar]
- 92.Sainz de Baranda F. Ayala P. Chronic flexibility improvements after 12 week of stretching program utilising the ACSM recommendations: Hamstring flexibility. Int J Sports Med. 2010; 38: 389‐396 [DOI] [PubMed] [Google Scholar]
- 93.Weppler C. Magnusson S. Increasing muscle extensibility: A matter of increasing length or modifying sensation. Phys Ther. 2010; 90 (3): 438‐449 [DOI] [PubMed] [Google Scholar]
- 94.Yamaguchi S. Sasho T. Kato H. Kuroyanagi Y. Banks S. Ankle and sub‐talar kinematics during dorsiflexion‐plantar flexion activities. Foot Ankle Int. 2009; 30: 361‐366 [DOI] [PubMed] [Google Scholar]
- 95.Nawoczenski D. A. Saltzman C. L. Cook T. M. The effect of foot structure on the three‐dimensional kinematic coupling behavior of the leg and rear foot. Phys Ther. 1998; 78(4), 404‐416 [DOI] [PubMed] [Google Scholar]
- 96.Perry J. Anatomy and biomechanics of the hindfoot. Clin Orthop Rel Res. 1983; (177), 9‐15 [PubMed] [Google Scholar]
- 97.Sahrmann S. Moving precisely? Or taking the path of least resistance? Phys Ther. 1998; 78 (11): 1208. [DOI] [PubMed] [Google Scholar]
- 98.Madeley L. Munteanu S. Bonanno D. Endurance of the ankle joint plantar flexor muscles in athletes with medial tibial stress syndrome: A case‐control study. J Sci Med Sport. 2007; 10 (6): 356‐362 [DOI] [PubMed] [Google Scholar]
- 99.Baldon R. Moreira D. Carvalho L. Lam Wun P, et al. Effect of functional stabilization training on lower limb biomechanics in women. Med Sci Sports Exerc. 2012; 44(1), [DOI] [PubMed] [Google Scholar]
- 100.Ekstrom R. Donatelli R. Carp K. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther. 2007; 37(12), 754‐762 [DOI] [PubMed] [Google Scholar]
- 101.Hewett T. E. Myer G. D. The Mechanistic Connection Between the Trunk, Hip Knee, and Anterior Cruciate Ligament Injury. Exerc Sport Sci Rev.. 2011; 39(4), 161‐166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Okubo Y. Kaneoka K. Imai A. Shiina I., et al. (2010). Electromyographic analysis of transversus abdominis and lumbar multifidus using wire electrodes during lumbar stabilization exercises. J Orthop Sports Phys Ther. 2010; 40(11), 743‐750 [DOI] [PubMed] [Google Scholar]
- 103.Zazulak B. T. Hewett T. E. Reeves N. P. Goldberg B., et al. Deficits in neuromuscular control of the trunk predict knee injury risk ‐ A prospective biomechanical‐epidemiologic study. Am J Sports Med. 2007; 35(7), 1123‐1130 [DOI] [PubMed] [Google Scholar]
- 104.Erby R. Heard R. O'Loughlin K. (2010). Trial of an injury reporting system for surf lifesavers in Australia. Work‐ A Journal of Prevention Assessment & Rehabilitation. 2010; 36(2), 181‐192 [DOI] [PubMed] [Google Scholar]
- 105.Burne S. Khan K. Boudville P. Mallet R., et al. Risk factors associated with exertional medial tibial pain: A 12 month prospective clinical study. Br J Sports Med. 2004; 38: 441‐445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Burr D. Milgrom C. Boyd R. Higgins W., et al. Experimental stress‐fractures of the tibia ‐ biological and mechanical etiology in rabbits. J Bone Joint Surg Br. 1990; 72(3), 370‐375 [DOI] [PubMed] [Google Scholar]
- 107.Chisin R. Milgrom C. Giladi M. Stein M., et al. Clinical‐significance of nonfocal scintigraphic findings in suspected tibial stress‐fractures. Clin Orthop Rel Res. 1987; (220), 200‐205 [PubMed] [Google Scholar]
- 108.Diab T. Condon K. Burr D. Vashishth D. Age‐related change in the damage morphology of human cortical bone and its role in bone fragility. Bone. 2006; 38(3), 427‐431 [DOI] [PubMed] [Google Scholar]
- 109.Diab T. Vashishth D. (2007). Morphology, localization and accumulation of in vivo microdamage in human cortical bone. Bone. 2007; 40(3), 612‐618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Melzack R. Evolution of the neuromatrix theory of pain. Pain Practice. 2005; 5 (2), 85‐94 [DOI] [PubMed] [Google Scholar]
- 111.Navas A. Kassarjian A. Bone marrow changes in stress injuries. Seminars in Musculoskeletal Radiology. 2011; 15(3), 183‐197 [DOI] [PubMed] [Google Scholar]
- 112.Fagan T. Nomogram for Bayes's Theorem. N Engl J Med. 1975; 293:257. [DOI] [PubMed] [Google Scholar]
- 113.Newman P. Adams R. Waddington G. Two simple clinical tests for predicting onset of medial tibial stress syndrome: shin palpation test and shin oedema test. Br J Sports Med. 2012; 46: 861‐864 [DOI] [PubMed] [Google Scholar]
- 114.Brukner P. Khan K. (2013). Principles of diagnosis: Clinical assessment. In: Clinical Sports Medicine. 2013; McGraw Hill [Google Scholar]
- 115.Hampton J. Harrison M. Mitchell R. Prichard S., et al. Relative contributions of history taking, physical exaqmination, and laboratory investigations to diagnosis and management of medical outpatients. Br Med J. 1975; 2:486‐489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sandler G. The importance of the history in the medical clinic and the cost of unnecessary tests. Heart Journal. 1980; 100 (6): 928‐931 [DOI] [PubMed] [Google Scholar]
- 117.Kerry R. Maddocks M. Mumford S. Philosophy of science and physiotherapy: An insight into practice. Physiotherapy Theory and Practice. 2008; 24(6), 397‐407 [DOI] [PubMed] [Google Scholar]
- 118.Wainner R. Fritz J. Irrgang J. Boninger M., et al. Reliability and diagnostic accuracy of the clinical examination and patient self‐ report measures for cervical radiculopathy. Spine. 2003; 28 (1): 52‐62 [DOI] [PubMed] [Google Scholar]