Abstract
Introduction and Background:
Lateral ankle sprains (LAS) are common in sports medicine and can result in a high rate of re‐injury and chronic ankle instability (CAI). Recent evidence supports the use on mobilizations directed at the ankle in patients who have suffered a LAS. The Mulligan Concept of Mobilization‐with‐Movement (MWM) provides an intervention strategy for LASs, but requires pain‐free mobilization application and little literature exists on modifications of these techniques.
Purpose:
To present the use of a modified MWM to treat LASs when the traditional MWM technique could not be performed due to patient reported pain and to assess outcomes of the treatment.
Case Description:
The subject of this case report is a 23 year‐old female collegiate basketball player who had failed to respond to initial conservative treatments after being diagnosed with a lateral ankle sprain. The initial management and subsequent interventions are presented. After re‐examination, the addition of a modification of a MWM technique produced immediate and clinically significant changes in patient symptoms. The use of the modified‐MWM resulted in full resolution of symptoms and a rapid return to full athletic participation.
Outcomes:
After the initial application of the modified‐MWM, the patient reported immediate pain‐free ankle motion and ambulation. Following a total of 5 treatments, using only the modified MWM and taping technique, the patient was discharged with equal range of motion (ROM) bilaterally, a decreased Disablement in the Physically Active (DPA) Scale score, and an asymptomatic physical exam. Follow‐up exam 6 weeks later indicated a full maintenance of these results.
Discussion:
Recent evidence has been presented to support the use of mobilization techniques to treat patient limitations following ankle injury; however, the majority of evidence is associated with addressing the talar and dorsiflexion limitations. Currently, little evidence is available regarding the use of the MWM technique designed for LASs and the expected outcomes. This case adds to the emerging evidence supporting the use for MWMs to treat ankle pathology and introduces a modification that may be applied in cases where patient reported pain prevents traditional application.
Level of Evidence:
Level 5; Single case report.
Keywords: Lateral ankle sprain, mobilization with movement
BACKGROUND
Ankle sprains, a common pathology suffered during physical activity, occur at an estimated rate of more than 23,000 per day in the United States.1 Based on recent literature reports, ankle sprains occurs at an incidence rate of 2.15 per 1,000 person‐years in the United States. Approximately 49.3% of ankle sprain occur during athletic related activities, with basketball contributing up to 41.1%.2 In basketball, it has been reported that approximately 60% of all injuries involve the lower extremity and approximately 25% of these injuries are ankle sprains.3
Due to the anatomical structure of the ankle, the anterior talofibular ligament (ATFL) is the most commonly injured ligament and is most susceptible to injury during a plantarflexion (PF) and inversion (IV) mechanism.2,4 The combined motion of PF and IV is a common mechanism of injury (MOI) and routinely leads to the diagnosis of a lateral ankle sprain (LAS). Brian Mulligan has theorized, however, that this MOI may result in a positional fault of the fibula, instead of a LAS. According to his theory, the ATFL pulls on the fibula at the distal tibiofibular joint creating a positional fault between the tibia and fibula. The positional fault, as opposed to the ligament sprain, is the main source of pain, dysfunction, and decreased range of motion.5,6
Under this hypothesis, Mulligan proposed that the Mobilization with Movement (MWM) treatment for LASs corrects the positional fault that may occur as a result of the PF and IV mechanism.5,6 The technique consists of a pain‐free sustained anterior‐posterior (AP) cranial glide of the lateral malleolus on the tibia. With the glide maintained, the patient then performs active PF and IV with clinician overpressure at end range. Following the MWM, the glide is maintained with a specific tape application applied in the direction of the MWM to help maintain the corrected position of the fibula. The entire application of the technique should be pain‐free for the patient and should produce immediate and long‐lasting benefits.5 The resolution of the patient's symptoms during the MWM application would be the clinical indication of a positional fault and would guide the clinician in choosing to apply this intervention.5,6
With acute LASs, however, a patient may be too tender to allow performance of the traditional MWM technique. The principles of MWM application require pain‐free application of the technique and guide the clinician in adjusting hand placement, force application, and the line of drive of the mobilization to produce the desired outcome. Additionally, padding may be applied to help alleviate point tenderness at the distal fibula.5,6 Tenderness to pressure may delay the use of this intervention and, in turn, delay healing and return to function. Therefore, a modification of the MWM joint mobilization and taping technique that allowed for earlier pain‐free application of the technique would be beneficial. The purpose of this case report is to present the use of a modified Mobilization‐with‐Movement to treat a patient diagnosed with a LAS.
CASE DESCRIPTION
Subject Characteristics
The subject, a 23 year‐old female collegiate basketball player, reported ankle pain following a PF and IV mechanism that occurred during a basketball game. The patient removed herself from competition and reported directly to her athletic trainer. She had participated in competitive basketball for over 13 years and had a history of repetitive LASs. The most recent LAS had occurred approximately one year earlier and had resolved over the course of 1 to 2 weeks with traditional conservative care. The patient did not report having any ankle complaints prior to the most recent injury.
Clinical Impression
When the patient initially reported to her athletic trainer at the team bench, she stated that her pain was a 7 out of 10 on the Numeric Rating Scale (NRS). While she was able to bear weight and walk at the time of injury, weight‐bearing exacerbated her pain. Observation did not reveal signs of significant pathology (e.g., gross deformity, ecchymosis, edema) and the patient only reported tenderness to palpation over the sinus tarsi area on the affected limb during the courtside examination. The patient displayed limited and painful range of motion (ROM) when examined actively and passively in all directions. The anterior drawer and inversion talar tilt tests were positive for pain and mild laxity, but produced a firm‐end feel. Kleiger's Test was negative for laxity and pain. The remainder of the initial courtside exam (e.g., negative Ottawa Ankle Rules, normal dermatome assessment, etc.) was consistent with a sprain of the anterior talofibular ligament (ATFL) and calcaneofibluar ligament (CFL). The immediate working diagnosis was a Grade 1+ right ATFL and CFL ligament sprain. The patient was immediately treated with rest, ice, compression, and elevation (RICE), while also being fitted for crutches to allow for non‐weight‐bearing ambulation until a full reexamination could be conducted the next day.
During follow‐up examination the next day, the physical exam findings were consistent from the court‐side evaluation across the palpation, ROM, and special test assessments; however, observation revealed the patient now presented with visually observed mild edema and ecchymosis at the sinus tarsi. As a result of these findings, the patient began a traditional conservative rehabilitation program. Initial treatment during the acute inflammatory phase included the continued use of RICE and crutches. The use of electrical stimulation for pain control, gentle active ROM, and isometric strengthening exercises were also utilized. After the acute inflammatory phase, traditional range of motion and strengthening exercises, as well as gentle massage techniques were added to the rehabilitation protocol for the next week (Table 1).
Table 1.
Therapeutic & Rehabilitation Timeline.
| Time | Intervention(s) | Settings/Parameters |
|---|---|---|
| Day 1‐3 | RICE, ROM exercises & isometric exercises |
|
| Day 4‐7 | Resistance Bands, Proprioception/Balance exercises, PNF exercises, Effleurage, Ice & Electrical Stimulation (Sensory level pain; 80‐150pps) |
|
| Day 8‐10 | Resistance Bands, Proprioception/Balance exercises, PNF exercises, Effleurage, Ice & Electrical Stimulation (Sensory level pain; 80‐150pps) |
|
| Day 10 | Re‐examination; initiation of modified MWM and taping technique | Modified MWM treatment (1 set of 10 repetitions) followed by tape application. |
| Day 11 | Modified MWM and taping; Full participation at practice | Modified MWM treatment (1 set of 10 repetitions) followed by tape application. |
| Day 12‐15 | No Treatment. | Patient participated in away competitions; Ankle was taped with a traditional ankle tape application only. |
| Days 16‐18 | Patient returned from away competitions; modified MWM treatments and taping applied. | Modified MWM treatment with tape − 1 × 10 (Day 16 and 17 only).Patient discharged on Day 18 |
| Day 60 | Follow up; No treatment | Patient reported being able to complete the remainder of the competitive season without a reoccurrence of symptoms and as being asymptomatic in activities of daily living. |
Revised Clinical Impression
After completing 10 days of conservative treatment from the time of injury, the patient reported pain levels that had only minimally improved during ROM or weight bearing activities (Figures 3 and 4). Additionally, her ROM deficiencies had not improved and she was unable to progress in her rehabilitation protocol. As a result, it was determined that a reexamination was needed and a second opinion was sought.
Figure 3.
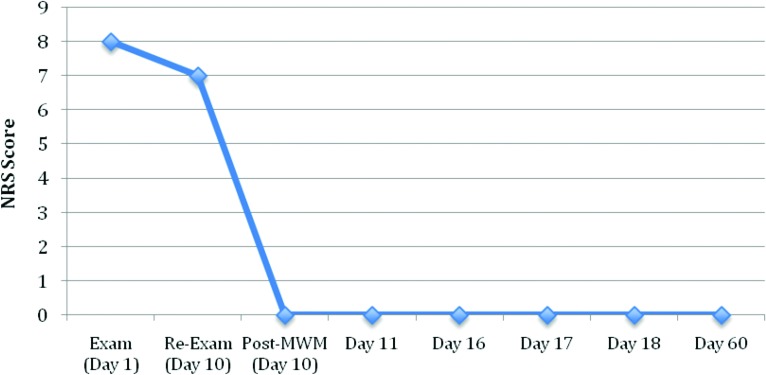
Patient Reported Pain During Weight Bearing (Double Limb Stance) on Numerical Rating Scale.
Figure 4.
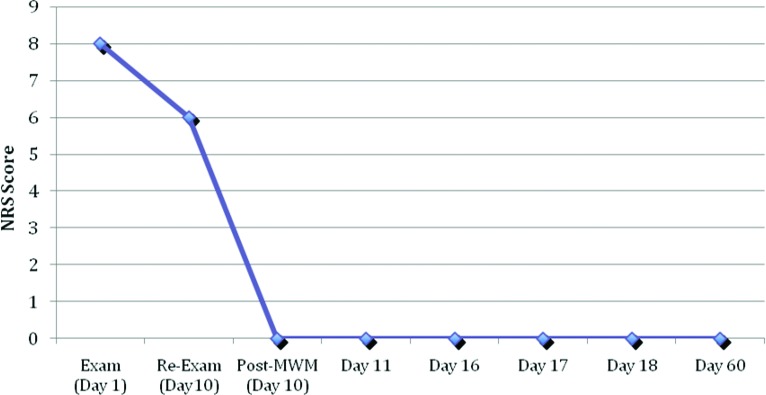
Patient Reported Pain During Active Plantarflexion (PF) & Inversion (IV) on Numerical Rating Scale.
During the reexamination, 10 days after initial injury, the patient rated her pain as a 7 with weight bearing (i.e, double limb stance) and a 6 during active IV and PF. The physical exam still revealed the same findings as the previous exam (e.g., tenderness to palpation at the sinus tarsi, consistent ROM deficiencies, consistent special test results), except edema and ecchymosis had resolved. The Disablement in the Physically Active (DPA) Scale was given to the patient to determine a patient‐centered outcome baseline and she reported an initial score of 29 out of 64, with her greatest areas of dysfunction being impaired motion and muscle function (3 out of 5) on the individual sections of the scale. The use of the Mulligan Concept MWM for lateral ankle sprains was then applied as an assessment technique to determine its efficacy in this subject. Despite the use of different types of padding materials and adjustments to hand placement, force application, and line of drive, the patient's tenderness to palpation prevented the application of the traditional MWM. As such, the MWM was modified by applying the technique approximately 2 inches proximal to the lateral malleolus (Figure 1). The Mulligan Concept protocols (e.g., line of drive, pain‐free application) were followed for the application of this technique and the modified MWM abolished the patient's reported pain during PF and IV activities. As a result, the use of this modified MWM was recommended as the appropriate treatment for the patient's dysfunction associated with the LAS presentation.
Figure 1.

Modified MWM joint mobilization technique for fibular repositioning.
Subject reported outcome measures included the NRS and the DPA Scale. The NRS is commonly applied with the patient rating their pain from 0 (i.e., “no pain”) to 10 (i.e., “worst pain imaginable”). The NRS has been found to be reliable and valid across many patient populations/situations7,8 and the minimal clinically important difference (MCID) value is regularly reported to be 2 points or 33%.9,10 The DPA Scale is a patient‐centered scale designed for the physically active patient and is used to assess measures of impairment, functional limitation, disability, and health‐related quality of life on a 0 (i.e., floor) to 64 (i.e., ceiling) scale.11 Patients answer 16 questions (e.g., “Do I have pain?”) across 11 disablement categories (e.g., pain, stability, overall fitness, well‐being, etc.) on a rating scale from 1 (i.e., no problem) to 5 (i.e., severe). The scores from each question are added together and then 16 points are subtracted to produce the final DPA Scale score. Vela and Denegar11 have indicated the scale is valid and reliable, while also reporting that the MCID value is 9 points in acute cases and 6 points in chronic cases.
Intervention/Outcomes
On Day 10, the modified MWM was administered utilizing a pain‐free sustained glide, followed by pain‐free full PF and IV with clinician generated over‐pressure at end‐range for a single set of 10 repetitions. Upon completing the 10 repetitions, the patient reported that she was no longer experiencing pain during active PF and IV. Additionally, the patient's active ROM was now equal to the uninvolved side in all directions. The patient was then asked to step down from the plinth and walk around the clinic to determine the effect of the intervention with weight bearing activities. The patient reported a resolution of her pain while walking and squatting in the clinic.
Following the results of the modified MWM application, tape was applied at the same site of the modified MWM using Mulligan Concept taping principles. The tape application began with a strip of non‐woven adhesive bandage being applied approximately 2 inches proximal to the lateral malleolus, and angled in the same direction as the MWM, while the glide was applied. The bandage was brought behind the distal tibiofibular joint, ending proximally to the beginning of the bandage without the ends over‐lapping. A strip of rigid tape was then cut to the same length as the bandage. The rigid tape was then applied over top of the bandage in the same direction as the MWM during a sustained glide. A second strip of the rigid tape was then applied in the same fashion (Figure 2). Upon completion of the tape application, the patient reported a continued resolution of pain and was told to continue to wear the tape until she reported to the clinic for follow‐up examination the next day.
Figure 2.

Completion of the Modified MWM Mobilization and tape application.
The following day, the patient reported a continued resolution of her symptoms with activities of daily living. The patient was still tender to palpation over her distal lateral ankle, but displayed equal ROM in all directions at the ankle bilaterally. The modified MWM was re‐applied for a single set of 10 repetitions and the patient was again taped using the modified taping technique. Following the application of the intervention, the patient continued to report resolution of her pain with weight‐bearing activities. As such, she was asked to complete various balance and functional activities (e.g., sets of squatting, duck walks, single and double leg hops) in order to determine her ability to return to practice. She completed the activities without a return of her symptoms and the patient was cleared to participate in practice that day with the caveat that she only performed activities that did not produce pain. The patient completed practice without a recurrence of her symptoms and was cleared to travel with the team for two away competitions beginning the next day.
The patient reported to the clinic on Day 16, after having competed in two games with her team. During this time period, she had been able to participate in competition while only receiving a traditional ankle tape application. While she still reported a resolution of her pain with activities of daily living (Figures 3 and 4), she indicated experiencing mild discomfort during game activities and was still tender to palpation over the area of her sinus tarsi. As a result, the use of the modified MWM intervention and taping technique was continued in attempt to produce full resolution of her symptoms during her sport specific activities. The patient received the modified treatment over the next two days while fully participating in team activities.
On Day 18, the patient reported that she did not experience any symptoms during competitive activities on the previous day. As such, a full physical examination was completed. During this examination, the patient did not report any pain during palpation, ROM activities, or functional testing. Her active, passive, and resistive ROMs were equal bilaterally. The anterior drawer and inversion talar tilt tests did not produce pain or abnormal end‐feels. The patient also reported an overall DPA Scale score of 12, which achieved an MCID; however, the patient still reported some deficits on the scale. The patient rated the disablement categories of pain, changing directions, maintaining positions, skill performance, participation in activities and overall fitness as a 2 (i.e., “does not affect”), motion and muscle function as a 3 (i.e., “slightly affects”), while the remaining areas/questions were all rated a 1 (i.e., “no problem”). As a result of the asymptomatic physical exam and a DPA Scale score in the range reported for the uninjured population, the patient was discharged to full competition without further treatment at this time. The patient was able to complete the remaining basketball season without a recurrence of symptoms and was still symptom free over 60 days post‐discharge.
DISCUSSION
Despite the regularity of LASs and the common use of many intervention techniques, debate still exists regarding which intervention is the most appropriate and when each intervention should be applied to appropriately address the patient's presentation. Much of this debate arises because mechanical ankle instability may be present for weeks to months following rehabilitation,4 and the most common predisposing factor for suffering a LAS is a history of previous ankle sprain.12 Additionally, despite the use of common rehabilitation strategies, a previous history of LASs may predispose a patient to chronic ankle instability.13 The efficacy of various rehabilitation techniques has been investigated in order to elucidate which interventions are most effective, but the majority of studies have focused on the short‐term outcomes (e.g., pain, range of motion, return to competition) and little research has focused on the use of mobilizations.4
Typically, acute LASs are managed with the use of RICE during the acute inflammatory stage.14 In more severe cases, immobilization is recommended for optimal healing of the affected ligaments.14,15 Despite common use, insufficient evidence exists to support the effectiveness of the application of RICE in the treatment of LASs.14 Additionally, as the various components of RICE are applied simultaneously, it is difficult to determine which component provides the most effective outcomes for the patient.15 Neuromuscular training strategies (e.g., Proprioceptive Neuromusclar Facilitation exercises, closed kinetic chain balance activities) have been hypothesized to be effective during the proliferation phase of healing to improve functional ankle balance.16,17 Intervals of walking and jogging, once the patient can ambulate long distances without gait alterations, have also been recommended.16 The use of rehabilitation programs incorporating these interventions has demonstrated some ability to reduce the number of future ankle sprains and be helpful in the prevention of CAI.15 The benefits, however, usually occur over weeks to months as the therapy model is built on the concept of pathoanatomical healing believed to be required following a diagnosed LAS when additional factors may need to be considered.
Recently, researchers have described that an anteroposterior mobilization of the fibula, combined with RICE, provided significant improvements in ROM compared to the application of RICE alone.14 The combined intervention resulted in increased stride speed within the first and third treatment sessions. Similarly, RICE combined with an osteopathic manipulative treatment led to improvements after a 1‐week follow‐up in patients with unilateral ankle sprains, when compared to RICE alone.15Given the results of studies such as these, combined with anecdotal reports, it may be necessary to examine other potential theories of pathology and treatment for LAS to facilitate the most appropriate treatment for each individual patient.5,6,19
One potential explanation for mechanical ankle dysfunction following a diagnosed LAS is the existence of positional fault between the fibula and tibia.5,19 The positional fault hypothesis has been supported through the demonstration of an anteriorly positioned fibula when compared to the tibia. Evidence of this position fault has been found when using an external measurement device, fluoroscope, and magnetic resonance image to measure positioning of the fibula in relation to the tibia.19‐22 Laboratory research demonstrated the existence of positional faults in patients suffering from chronic and sub‐acute lateral ankle sprains, while clinical research efforts have supported the existence of positional faults in acute pathology.20‐22 Investigators have suggested greater amounts of edema may result in a greater amount of fibular displacement when compared to the tibia.21,23 Additionally, it has also been indicated that patients with CAI may suffer from an anterior positional fault of the talus in the sagittal plane.24 As such, applying interventions to address this malposition, whether through a biomechanical or neuroscience paradigm, may be necessary to provide the most effective outcomes for patients.
Improvement of clinical outcomes examining pain and dysfunction following LASs support the use of MWMs. Hetherington25 applied the LAS MWM following acute ankle sprain and noted improved gait, pain‐free inversion ROM, and balance in patients. Stubbs et al.26 utilized the same MWM to produce an immediate resolution of a collegiate soccer player's symptoms following a week of minimal improvement after suffering an acute LAS. The patient was able to return to activity the next day and completed the collegiate soccer season without recurrence of symptoms or re‐injury.26 O'Brien and Vicenzino27 also reported rapid improvements in ROM and reported pain following the use of this MWM to treat a LAS. Evidence also exists to support the potential use of the MWM tape application to reduce the occurrence of LASs in athletes.28 The tape application, however, does not appear to affect performance in either static or dynamic balancing tasks in relation to chronic ankle injuries in a significant way when compared to traditional methods.29
The MWM for the LAS has not been the only MWM technique used to treat patients who have suffered a LAS. Vicenzino et al.30 indicated the posterior MWM for the talus produced statistically significant increases in dorsiflexion in patients suffering from CAI. Wikstrom et al.31 produced similar results by demonstrating that a single MWM treatment provided improvements in dorsiflexion range in motion, while also resulting in a restoration of normal arthrokinematics and osteokinematics. Green et al.14 also reported a more rapid return to pain‐free ankle dorsiflexion among patients who received this MWM when compared to patients that did not when treating an acute ankle sprain. Similarly, Collins et al.32 reported a significant improvement in ankle dorsiflexion following this treatment in patients who had sustained an ankle sprain. Based on the current literature, it appears MWM joint mobilizations are effective as a means to decrease pain, improve function, improve ROM, and produce more rapid returns to activity in patients suffering from acute and chronic ankle sprains.16,19,27,30‐32 What is unclear at this time, however, is the mechanism of action (e.g., positional fault hypothesis, non‐opioid hypoalgesia) by which the MWM produces these outcomes.6
In the case presented, the modified MWM produced an immediate change greater than what is required to produce a minimal clinically important difference (MCID) on the NRS (2 points)9 and DPA Scale (9 points)10 on initial treatment. Over the course of 5 treatments, the technique resolved the patient's complaints, while allowing her to return to competition. Additionally, the modified‐MWM outcomes allowed the patient to participate in sport activities that day without a return of her symptoms. The potential advantage of the modified MWM is that the mobilization can be administered earlier when chemical pain may prevent the application of the traditional MWM due to patient sensitivity to pressure at the lateral malleolus. As the modified technique still followed Mulligan principles, the early application of the technique posed little risk to the patient, while allowing earlier application of the MWM to improve patient outcomes and potentially decrease the risk of a patient developing chronic ankle instability.29
CONCLUSION
The outcomes from this case report provide evidence for the incorporation of MWM into the rehabilitation protocol in patients who have suffered a LAS. Additionally, it provides support for the modified‐MWM technique that may be applied if the traditional technique cannot be used due to patient reported pain. Further research is needed, however, to determine if the modification consistently produces similar outcomes to the traditional MWM or if there is only a subgroup of patients that will respond to this technique more effectively (e.g., when the patient is too point tender to perform at the lateral malleolus). Patient outcomes on a larger population need to be collected to determine its reliability and validity, while further elucidation is needed to understand the mechanism of action by which the outcomes are produced. Additional research is also needed to determine its long‐term effects on chronic ankle instability, and if the modification decreases the period of disablement.
REFERENCES
- 1.Kannus P Renstrom P Treatment for acute tears of the lateral ligaments of the ankle: operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73(2);305‐312 [PubMed] [Google Scholar]
- 2.Waterman B Owens B Davey S Zacchilli M Belmont P The Epidemiology of Ankle Sprains in the United States. J Bone Joint Surg Am, 2010; 92(13);2279‐2284 [DOI] [PubMed] [Google Scholar]
- 3.“Play‐by‐Play” Sport Specific Results and Recommendations. National Athletic Trainers’ Association. Available at http://www.nata.org/play-by-play Accessed August 31 2013.
- 4.Hubbard T Hicks‐Little C Ankle ligament healing after an acute ankle sprain: an evidence‐based approach. J Athl Train. 2008;43(5):523‐529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mulligan B Manual Therapy: Nags, Snags, MWMs, etc. New Zealand: Plan View Services Ltd.; 2010 [Google Scholar]
- 6.Vicenzino B Hing W Rivett D Hall T Mobilisation with movement: the art and science. Elsevier Australia: Melinda McEvoy; 2011 [Google Scholar]
- 7.Ferriera‐Valente MA Pais‐Ribeiro JL Jensen MP Validity of four pain intensity rating scales. Pain. 2011;152(10):2399‐2402 [DOI] [PubMed] [Google Scholar]
- 8.Hjermstad MJ Fayers PM Haugen DF Caraceni A Hanks GW Loge JH, et al. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic review. Journal of Pain and Symptom Management. 2011;41(6):1073‐1093 [DOI] [PubMed] [Google Scholar]
- 9.Pool JJ Ostelo RW Hoving JL Bouter LM de Vet HC Minimal clinically important change of the neck disability index and the numerical rating scale for patients with neck pain. Spine. 2007;32(26):3047‐3051 [DOI] [PubMed] [Google Scholar]
- 10.Farrar JT Young JP LaMoreaux L Werth JL Poole M Clinical importance of changes in chronic pain measured on an 11‐point numerical pain rating scale. Pain. 2001;94:149‐158 [DOI] [PubMed] [Google Scholar]
- 11.Vela LI Denegar C The disablement in the physically active scale, part II: The psychometric properties of an outcomes scale for musculoskeletal injuries. J Athl Train. 2010;45(6):639‐641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bahr R Rahr I Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports. 1997;7:166‐171 [DOI] [PubMed] [Google Scholar]
- 13.Eechaute C Vaes P Duquet W The chronic ankle instability scale: Clinimetric properties of a multidimensional, patient‐assessed instrument. Phys Ther Sport. 2008;9(2):57‐66 [DOI] [PubMed] [Google Scholar]
- 14.Green T Refshauge K Crosbie J Adams R A randomized controlled trial of a passive accessory joint mobilization on acute ankle sprains. Phys Ther. 2001; 81:984‐994 [PubMed] [Google Scholar]
- 15.Eisenhart AW Gaeta TJ Yens DP Osteopathic manipulative treatment in the emergency department for patients with acute ankle injuries. J Am Osteopath Assoc. 2003;103(9):417–421 [PubMed] [Google Scholar]
- 16.Kaminski T Hertel J Amendola N, et al. National Athletic Trainers’ Association Position Statement: Conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528‐545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mattacola CG Dwyer MK Rehabilitation of the ankle after acute sprain or chronic instability. J Athl Train. 2002;37(4):413‐429 [PMC free article] [PubMed] [Google Scholar]
- 18.Hale SA Hertel J Olmsted‐Kramer LC The effect of a 4‐Week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37(6):303‐311 [DOI] [PubMed] [Google Scholar]
- 19.Baker RT Nasypany A Seegmiller JG Baker JG The mulligan concept: mobilizations with movement. Int J Athl Ther Train. 2013;18(1):30‐34 [Google Scholar]
- 20.Kavanagh J Is there a positional fault at the inferior tibiofibluar joint in patients with acute or chronic ankle sprains compared to normals? Man Ther. 1999;4(1);19‐24 [DOI] [PubMed] [Google Scholar]
- 21.Hubbard T Hertel J Sherbondy P Fibular position in individuals with self‐reported chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(1):3‐9 [DOI] [PubMed] [Google Scholar]
- 22.Hubbard T Hertel J Anterior positional fault of the fibula after sub‐acute lateral ankle sprains. Man Ther. 2008;13(1):63‐67 [DOI] [PubMed] [Google Scholar]
- 23.Fukuhara T Sakamoto M Nakazawa R Kato K Anterior positional fault of the fibula after sub‐acute anterior talofibular ligament injury. J Phys Ther Sci. 2012;24(1):115‐117 [Google Scholar]
- 24.Wikstrom E Hubbard‐Turner T McKeon P Understanding and treating lateral ankle sprains and their consequences. Sports Med. 2013;43(6):385‐393 [DOI] [PubMed] [Google Scholar]
- 25.Hetherington B Lateral ligament strains of the ankle, do they exist? Man Ther. 1996; 1(5):274‐275 [DOI] [PubMed] [Google Scholar]
- 26.Stubbs E Baker RT Ramos C Utilizing Mulligan's concept for correcting an anterior positional fault of the fibula following a lateral ankle sprain: A case report. Paper presented at: 2012 Far West Athletic Trainers’ Association Annual Meeting and Clinical Symposium; April 12‐15, 2012, San Diego, CA [Google Scholar]
- 27.O'Brien T Vicenzino B A study of the effects of mulligan's mobilization with movement treatment of lateral ankle pain using a case study design. Man Ther. 1998;3(2):78‐84 [Google Scholar]
- 28.Moiler K Hall T Robinson K The role of fibular tape in the prevention of ankle injury in basketball: a pilot study. J Orthop Sports Phys Ther. 2006;36(9):661‐668 [DOI] [PubMed] [Google Scholar]
- 29.Hopper D Samsson K Hulenik T Ng C Hall T Robinson K The influence of mulligan ankle taping during balance performance in subjects with unilateral chronic ankle instability. Phys Ther Sport. 2009;10(4):125‐130 [DOI] [PubMed] [Google Scholar]
- 30.Vicenzino B Branjerdporn M Teys P Jordan K Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprains. J Orthop Sports Phys Ther. 2006; 36(7):464‐471 [DOI] [PubMed] [Google Scholar]
- 31.Wikstrom E Hubbard T Talar Positional fault in persons with chronic ankle instability. Arch Phys Med and Rehab. 2010;91:1267‐1271 [DOI] [PubMed] [Google Scholar]
- 32.Collins N Teys P Vicenzino B The initial effects of a Mulligan's mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther. 2004; 9:77‐82 [DOI] [PubMed] [Google Scholar]


