Abstract
Objectives
To evaluate the applicability of MRI for the quantitative assessment of anterior talofibular ligaments (ATFLs) in symptomatic chronic ankle instability (CAI).
Methods
Between 1997 and 2010, 39 patients with symptomatic CAI underwent surgical treatment (22 male, 17 female, mean age 25.4 years (15 to 40)). In all patients, the maximum diameters of the ATFLs were measured on pre-operative T2-weighted MR images in planes parallel to the path of the ATFL. They were classified into three groups based on a previously published method with modifications: ‘normal’, diameter = 1.0 - 3.2 mm; ‘thickened’, diameter > 3.2 mm; ‘thin or absent’, diameter < 1.0 mm. Stress radiography was performed with the maximum manual force in inversion under general anaesthesia immediately prior to surgery. In surgery, ATFLs were macroscopically divided into two categories: ‘thickened’, an obvious thickened ligament and ‘thin or absent’. The imaging results were compared with the macroscopic results that are considered to be of a gold standard.
Results
Agreement was reached when comparison was made between groups, based on MRI and macroscopic findings. ATFLs were abnormal in all 39 cases and classified as ten ‘thickened’ and 29 ‘thin or absent’. As to talar tilt stress radiography, a clear cut-off angle, which would allow discrimination between ‘thickened’ and ‘thin or absent’ patients, was not identified.
Conclusion
MRI is valuable as a pre-operative assessment tool that can provide the quantitative information of ATFLs in patients with CAI.
Cite this article Bone Joint Res 2014;3:241–5.
Keywords: Chronic ankle instability (CAI), Anterior talofibular ligament (ATFL), MRI, Stress radiography
Article focus
In cases where surgery is considered for symptomatic chronic ankle instability (CAI), it is imperative not only to detect injured lesions but also to document the extent of ligament tear and the quantity of residual ligamentous tissue.
This study aimed to evaluate the applicability of MRI for the quantitative assessment of anterior talofibular ligaments (ATFLs) in symptomatic CAI.
Key messages
On pre-operative MRI, ATFLs were abnormal in all 39 cases and classified as ten ‘thickened’ and 29 ‘thin or absent’.
In all cases pre-operatively categorised as ‘thickened’, residual ligaments were thick enough to be advanced, as observed during surgery, and graft replacement was not required. In the remaining cases, we were unable to detect bulky or normal residual tissue, and reconstruction had to be performed.
MRI is valuable as a pre-operative assessment tool that can provide the quantitative information of ATFLs in CAI patients.
Strengths and limitations
This study is based on the experience of a single surgeon.
Stress radiography was performed under general anaesthesia immediately prior to surgery.
Small numbers were involved in this study.
Introduction
Acute lateral ankle ligament lesions are the most common injuries sustained in sports and recreational activities.1,2 Although most of these injuries can be treated successfully with conservative treatment, the development of chronic ankle instability (CAI), characterised by the occurrence of repetitive ankle sprains and persistence of symptoms after the initial injury, is not uncommon.3-5 Increased ligamentous laxity is one of the main causes of residual symptoms after ankle sprains, and failure of appropriate conservative management is an indication for surgical treatment.6,7 The anterior talofibular ligament (ATFL) is the main lateral stabiliser of the ankle joint and is most commonly affected first, followed by the calcaneofibular ligament (CFL) and the posterior talofibular ligament (PTFL).8,9 In cases where surgery is considered for symptomatic CAI, it is imperative not only to detect injured lesions but also to document the extent of ligament tear and the quantity of residual ligamentous tissue, as anatomic repair is recommended when the quality of the ruptured ligaments permits, and anatomic reconstruction should be performed when ligaments are attenuated.10,11 Although various imaging techniques such as stress radiography and MRI have been used for diagnosis,12-15 few studies have examined the sensitivities of evaluation methods in providing information about residual ligamentous tissue.16
In this study, we pre-operatively assessed injured ATFLs in symptomatic CAI patients by MRI and stress radiography under general anaesthesia. Using surgical findings as the gold standard, we evaluated the use of these two methods as pre-operative assessment tools. We hypothesised that pre-operative MRI can quantitatively evaluate injured ATFLs, and is useful in surgical planning.
Patients and Methods
Patient population
Between March 1997 and December 2010, 39 symptomatic CAI patients underwent surgical treatment at our hospital. Clinical criteria were the same as those described in previous reports.3,4,7 Patients had either a history of repetitive ankle sprains or persistent ankle pain that occurred after an acute lateral ankle sprain. The indication for surgical treatment was failure in conservative management after appropriate rehabilitation. There were 22 men and 17 women with a mean age of 25.4 years (15 to 40). The mean time between initial injury and surgery was 5.3 years (4 months to 20 years). All patients were evaluated pre-operatively by MRI and stress radiography was performed under general anaesthesia.
MRI
MRI was performed with a Hitachi Medical Corporation 0.4-T unit (Hitachi Electronics, Tokyo, Japan). The foot was placed in a neutral position and images were taken of each ankle in planes parallel to the path of the ATFL. Axial images were obtained using the following parameters: 16 cm field of view; 256 × 256 matrix; and 3 mm slice thickness with a 0.5 mm intersection gap. T1-weighted spin echo images were generated with a repetition time (TR) of 500 ms and echo times (TE) of 20 ms (500/20), and T2-weighted fast spin echo images were generated with a TR of 3500 ms and TE of 117 ms (3500/117).
Pre-operative MRI evaluation
On T2-weighted images, maximum diameters of the ATFLs were measured and classified into three categories based on a previously published method17 with modifications: ‘normal’, diameter = 1.0 to 3.2 mm; ‘thickened’, diameter > 3.2 mm; ‘thin or absent’, diameter < 1.0 mm (Fig. 1). Cases in which the continuity of the ATFL could not be confirmed were classified as ‘absent’.
Figs. 1a - 1c.
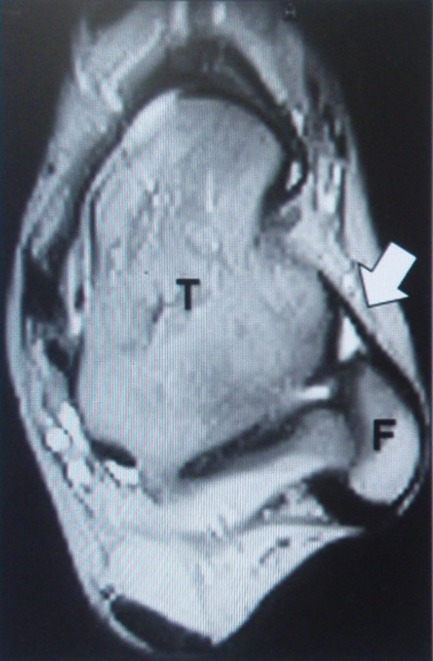

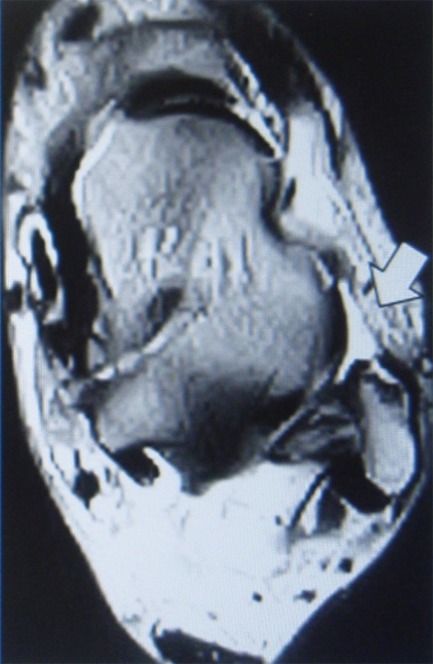
Axial T2-weighted images showing typical ATFL findings (white arrows). T and F denote tibia and fibula, respectively, the MRI evaluation was undertaken pre-operatively, and maximum diameters of the anterior talofibular ligaments (ATFLs) were measured.
Stress radiography
Stress radiography was performed with the maximum manual force in inversion under general anaesthesia. Talar tilt was measured as the angle formed by opposing articular surfaces of the tibia and talus.18
Surgical findings
ATFLs were evaluated and classified into two categories during surgery: ‘thickened’, an obvious thickened ligament; ‘thin or absent’, a maximum diameter of < 1.0 mm or when the path of the ligamentous tissue from the anterior aspect of the distal fibula at the malleolar fossa level to the neck of the talus was undetectable (Fig. 2).
Figs. 2a - 2b.

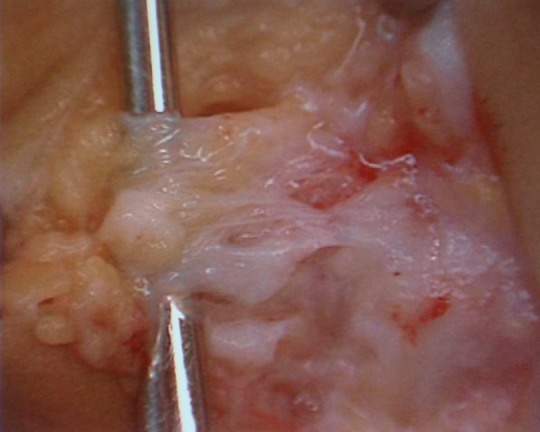
Photographs showing the typical intra-operative appearance of injured anterior talofibular ligaments (ATFLs), either a) ‘thickened’ or b) ‘thin or absent’.
Reliability analysis
A total of five patients were selected randomly and two orthopaedic surgeons classified their ATFLs on MRI. During surgery, two other orthopaedic surgeons who were blinded to use of the MRI evaluated the ATFLs; two of these were classified as ‘thickened’ and three ‘thin or absent’ on MRI, which agreed with our categorisation based on surgical findings.
Statistical analysis
Descriptive data are reported as mean (sd) and range. We used conventional statistical tests to compare outcomes in the two groups (‘thickened’ and ‘thin or absent’). The chi-squared test was used for dichotomous variables, and the Mann–Whitney U test for all ordinal variables. Two-sided p-values < 0.05 were considered statistically significant. Data were analysed using Microsoft Excel (Microsoft Corporation, Redmond, Washington). A logistic regression analysis was performed using SPSS (SPSS Inc., Chicago, Illinois), with p < 0.05 considered statistically significant.
Results
ATFLs in all patients were abnormal at surgery. ‘Thickened’ and ‘thin or absent’ ATFLs were observed in ten and 29 cases, respectively (Table I).
Table I.
Patient demographics categorised by surgical findings
| Variable | Thickened* | Thin or absent* | p-value† |
|---|---|---|---|
| Total: women + men | 10: 5 + 5 | 29: 17 + 12 | |
| Age (years) | |||
| Mean (sd) | 21.4 (6.9) | 25.9 (8.6) | NS |
| Min to max | 15 to 34 | 16 to 40 | |
| Time from initial injury to surgery (years)‡ | |||
| Mean (sd) | 2.3 (2.2) | 6.4 (6.1) | 0.006 |
| < 2 years, n | 7 | 6 | |
| 2 years ≦, n | 3 | 22 | |
*‘thickened’ and ‘thin or absent’ denote the appearance of ATFLs during surgery †p < 0.05 was considered statistically significant. NS, not significant ‡ In one case, the initial injury episode could not be confirmed
There were no gender- or age-related differences between the two groups. The time between initial injury and surgery was significantly different in the two groups (thickened, 2.3 years (sd 2.2); thin or absent, 6.4 years (sd 6.1), p = 0.006).
MRI diagnosis and surgical findings
ATFLs were abnormal on pre-operative MRI in all 39 cases. Injured ligaments were categorised as thickened (10), or thin or absent (29) (Table II).
Table II.
Comparison of pre-operative evaluations and surgical findings
| MRI | Stress radiography | ||
|---|---|---|---|
| Surgical findings | Thickened | Thin or absent | (Talar tilt) |
| Thickened | 10 | 0 | 11.2 ± 4.8 |
| Thin or absent | 0 | 29 | 15.5 ± 6.4 |
| All | 10 | 29 | 14.4 ± 6.3 |
| p-value | 0.037* | ||
* pairwise comparison revealed a significant difference between thickened and thin or absent categories
Comparison with surgical findings revealed that all ten thickened ATFLs were correctly predicted by MRI.
Stress radiography and surgical findings
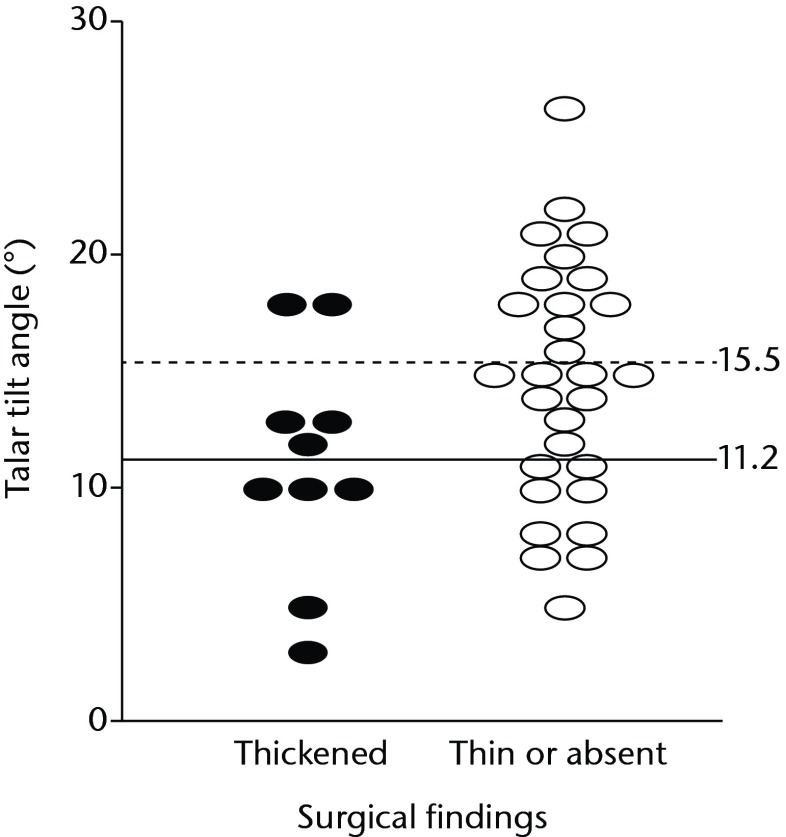
The mean talar tilt was 14.4 (sd 6.3°) (Table II, Fig 3). Comparison of the two groups categorised by surgical findings revealed a significant difference (thickened, 11.2 (sd 4.8°); thin or absent, 15.5 (sd 6.4°); p = 0.037). The angle of talar tilt did not have a significant effect on categorisation based on surgical findings using the logistic regression analysis (odds ratio: 0.872; p = 0.072), and a clear cut-off angle, which would allow discrimination between ‘thickened’ and ‘thin or absent’ patients, was not identified (Fig. 3).
Fig. 3.
Stress radiography data distribution for surgically-established anterior talofibular ligament (ATFL) categories. Angles of talar tilt were significantly different in the two surgically-established groups (thickened, 11.2 (sd 4.8°); thin or absent, 15.5 (sd 6.4°); p = 0.037). A clear cut-off angle was not identified.
Discussion
CAI not only limits physical activity, but also leads to an increased risk of osteoarthritis, and patients with severe disability often need surgical treatment to restore mechanical stability.5,19,20 Although various imaging methods, such as stress radiography, MRI, computed tomography, and ultrasonography, are available to facilitate precise diagnosis, the first two methods are most frequently used.7,21
The anterior drawer test and talar tilt stress radiographs are commonly used in the clinical setting.18,22However, these measurements correlate poorly with the degree of ligamentous disruption due to large individual variations.15,17,23Some patients have bilateral ankle sprains, which render comparison with the contralateral side unreliable. Furthermore, some investigators claim that radiographic stress tests cause pain and muscle spasms that restrict movement unless the joint is anaesthetised.14,15,18 To overcome these problems, both stress radiographs in the present study were obtained under general anaesthesia in the operating room and a side-by-side comparison was not performed. The mean angle of talar tilt was smaller in those patients with a thickened ATFL than in those whose ATFL was thin or absent. However, a clear cut-off angle, which would allow discrimination between thickened and thin or absent, was not identified. These data are consistent with previous reports.12,23
MRI is commonly used as a less invasive technique for diagnosing acute lateral ankle ligament injury.15,23,24However, its use in CAI is controversial.12,14,17Cardone et al17 examined 43 CAI patients and developed a set of diagnostic criteria in MRI for abnormalities of the ankle ligament. After comparing the results of stress radiography in 23 patients, they concluded that MRI is more useful than stress radiography for identifying injured ligaments. Chandnani et al12 compared the efficacy of conventional MRI, MR arthrography, and stress radiography in 17 CAI patients and found that MRI has a sensitivity of 50% in the diagnosis of ATFL and CFL tears, which is similar to that of stress radiography. Oae et al14 performed stress radiography, ultrasonography, MRI, and arthroscopy in 15 cases of chronic ankle sprains. Using arthroscopic results as the gold standard, both MRI and stress radiography yielded 93% accuracy in ATFL injury diagnoses. The discrepancy between these two results may be due to the lack of common diagnostic criteria in MRI findings for ankle ligament injury, as well as differences in imaging protocols. In our study, maximum diameters of the ATFLs were measured from T2-weighted axial images in the neutral ankle position, as described by Cardone et al.17 This protocol generates reproducible images, allowing objective evaluation of injured ligaments. In all of our cases, residual ATFLs were diagnosed as abnormal by pre-operative MRI and confirmed during surgery. The accuracy of ATFL injury diagnosis was higher or equal to those previously reported.12,14,17
Several studies have correlated imaging findings with surgical findings in CAI.12,14,16,17 However, to the best of our knowledge, this is the first report to examine the use of MRI in the quantitative evaluation of residual ligamentous tissues in CAI patients. In this study, patients were categorised into three groups according to maximum diameters of residual ATFLs measured by pre-operative MRI. In all cases pre-operatively categorised as thickened, residual ligaments were thick enough to be advanced, as observed during surgery, and graft replacement was not required. In the remaining cases, we were unable to detect bulky or normal residual tissue, and reconstruction had to be performed.25 Retrospectively, surgical procedures can be chosen according to the extent of residual ligamentous tissues predicted by pre-operative MRI. As the reconstruction procedure requires graft preparation, accurate pre-operative planning has substantial merit. In our study, the quantity of ATFLs were well evaluated. However, MRI evaluation of the quality of ligaments is difficult, partially due to the lack of a standard evaluation method. This is an issue to be addressed in future studies.
In conclusion, our results show that MRI is capable of quantitatively evaluating the injured ATFL. We believe that pre-operative MRI is useful as an adjunct to stress radiography in surgical planning.
Funding Statement
None declared
Footnotes
Author contributions:T. Kanamoto: Writing the paper, Data collection and analysis, Statistical analysis
Y. Shiozaki: Data collection and analysis and interpretation of data
Y. Tanaka: Analysis and interpretation of data
Y. Yonetani: Analysis and interpretation of data
S. Horibe: Conception of this study, Study design and coordination
ICMJE Conflict of Interest:None declared
References
- 1.Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med 2005;33:1485–1491 [DOI] [PubMed] [Google Scholar]
- 2.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg [Am] 2010;92-A:2279–2284 [DOI] [PubMed] [Google Scholar]
- 3.Hale SA, Hertel J. Reliability and sensitivity of the foot and ankle disability index in subjects with chronic ankle instability. J Athl Train 2005;40:35–40 [PMC free article] [PubMed] [Google Scholar]
- 4.Hubbard TJ, Hicks-Little CA. Ankle ligament healing after an acute ankle sprain: an evidence-based approach. J Athl Train 2008;43:523–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Rijn RM, van Os AG, Bernsen RM, et al. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med 2008;121:324–331 [DOI] [PubMed] [Google Scholar]
- 6.Delahunt E, Coughlan GF, Caulfield B, et al. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc 2010;42:2106–2121 [DOI] [PubMed] [Google Scholar]
- 7.Hertel J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J Athl Train 2002;37:364–375 [PMC free article] [PubMed] [Google Scholar]
- 8.Broström L. Sprained ankles. I. Anatomic lesions in recent sprains. Acta Chir Scand 1964;128:483–495 [PubMed] [Google Scholar]
- 9.van den Bekerom MP, Oostra RJ, Alvarez PG, van Dijk CN. The anatomy in relation to injury of the lateral collateral ligaments of the ankle: a current concepts review. Clin Anat 2008;21:619–626 [DOI] [PubMed] [Google Scholar]
- 10.de Vries JS, Krips R, Sierevelt IN, Blankevoort L. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev 2006;18:CD004124. [DOI] [PubMed] [Google Scholar]
- 11.Horibe S, Shino K, Taga I, Inoue M, Ono K. Reconstruction of lateral ligaments of the ankle with allogeneic tendon grafts. J Bone Joint Surg [Br] 1991;73-B:802–805 [DOI] [PubMed] [Google Scholar]
- 12.Chandnani VP, Harper MT, Ficke JR, et al. Chronic ankle instability: evaluation with MR arthrography, MR imaging, and stress radiography. Radiology 1994;192:189–194 [DOI] [PubMed] [Google Scholar]
- 13.Nakasa T, Fukuhara K, Adachi N, Ochi M. Evaluation of anterior talofibular ligament lesion using 3-dimensional computed tomography. J Comput Assist Tomogr 2006;30:543–547 [DOI] [PubMed] [Google Scholar]
- 14.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol 2010;39:41–47 [DOI] [PubMed] [Google Scholar]
- 15.Schneck CD, Mesgarzadeh M, Bonakdarpour A. MR imaging of the most commonly injured ankle ligaments. Part II. Ligament injuries. Radiology 1992;184:507–512 [DOI] [PubMed] [Google Scholar]
- 16.Trc T, Handl M, Havlas V. The anterior talo-fibular ligament reconstruction in surgical treatment of chronic lateral ankle instability. Int Orthop 2010;34:991–996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cardone BW, Erickson SJ, Den Hartog BD, Carrera GF. MRI of injury to the lateral collateral ligamentous complex of the ankle. J Comput Assist Tomogr 1993;17:102–107 [DOI] [PubMed] [Google Scholar]
- 18.McCaskie AW, Gale DW, Finlay D, Allen MJ. Chronic ankle instability: the value of talar tilt under general anaesthesia. Br J Sports Med 1995;29:103–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med 2005;39:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med 2006;34:612–620 [DOI] [PubMed] [Google Scholar]
- 21.Tourne Y, Besse JL, Mabit C. Chronic ankle instability: which tests to assess the lesions? Which therapeutic options? Orthop Traumatol Surg Res 2010;96:433–446 [DOI] [PubMed] [Google Scholar]
- 22.Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis 2011;69:17–26 [PubMed] [Google Scholar]
- 23.Breitenseher MJ, Trattnig S, Kukla C, et al. MRI versus lateral stress radiography in acute lateral ankle ligament injuries. J Comput Assist Tomogr 1997;21:280–285 [DOI] [PubMed] [Google Scholar]
- 24.Kreitner KF, Ferber A, Grebe P, et al. Injuries of the lateral collateral ligaments of the ankle: assessment with MR imaging. Eur Radiol 1999;9:519–524 [DOI] [PubMed] [Google Scholar]
- 25.Nakata K, Shino K, Horibe S, et al. Reconstruction of the lateral ligaments of the ankle using solvent-dried and gamma-irradiated allogeneic fascia lata. J Bone Joint Surg [Br] 2000;82-B:579–582 [DOI] [PubMed] [Google Scholar]