Abstract
Adhesive systems are selected based on their bond strengths achieved while testing in laboratories. These bond strengths can predict the longevity of a restoration to some extent. There were several discrepancies in the reported bond strengths. To critically review the reliability of macro-bond strength tests used to evaluate resin-tooth interface. Relevant literature published between January 1983 and May 2013 was collected from PubMed database, Google scholar, and hand-searched journals of Conservative Dentistry, Endodontics and Dental materials. Variables that influence the test outcome are categorized into substrate-related factors, factors related to specimen properties, preparation of specimens, and test methodology. Impact of these variables on the test outcome is critically analyzed. There is lack of a standard format for reporting the bond strength tests, which could lead to misinterpretation of the data and bonding abilities of adhesives.
Keywords: Bond strength test, push-out, shear, tensile, variables
INTRODUCTION
Longevity of a restoration is predicted to some extent by its adhesive ability, and this in turn can be measured by bond strength testing. Over the years, clinicians have relied upon laboratory evaluations to choose the adhesive systems to use in their daily practice. Though the validity of bond strength tests to predict clinical performance of dental adhesives is questionable,[1] existing evidence shows that clinical performance can be predicted by appropriate types of laboratory study results.[2,3] The realization of an acceptable and valid test method for assessing adhesive resin-tooth interface is a difficult endeavor.[4] Hence the purpose of this two parts review is to critically discuss the reliability of various bond strength test methods used to test the adhesion between tooth and composite resin. In the first part macro-tests and in the second part micro-test methods are analyzed critically.
TYPES OF BOND STRENGTH TESTS
An ideal bond strength test should be accurate, clinically reliable, and less technique-sensitive. It should involve the use of relatively unsophisticated and inexpensive test protocols.[5]
Oilo[6] classified them into qualitative screening tests and quantitative tests. Qualitative tests study bond failures, and quantitative tests predict the load capacity and lifetime of the bond.[6] Bond strength can be assessed by laboratory methods and clinical performance. It can be measured statically using a macro- or micro-test set-up, basically depending upon the size of the bond area.[5] The nominal bond strength is calculated by dividing the maximum applied force by the bonded cross-sectional area.[7]
International Standards Organization (ISO) Technical Specification No. 11405 provides guidance on substrate selection, storage, and handling as well as essential characteristics of different test methods for quality testing of the adhesive bond between restorative materials and tooth structure. It also presents some specific test methods for bond strength measurements.[8]
LABORATORY TESTS
Clinical trials are the ultimate tests for evaluating dental restorations; however, they cannot identify the exact reason for failure due to the simultaneous impact of diverse stresses on restorations within the aggressive oral cavity.[2] Laboratory tests gather data quickly and easily on a specific parameter/property. It is possible to measure one specific parameter while keeping all other variables constant. Various experimental groups can be tested simultaneously within one study set-up. The final objective of a laboratory test should obviously be to gather data in prediction of the eventual clinical outcome.[5] It is very likely that there will never be a single laboratory test or an assortment of tests that will accurately predict the clinical performance of a specific material.[9] These laboratory bond strength tests can be static or dynamic tests.[10]
Static tests
In static tests, load is applied when the test specimen is stationery unlike dynamic tests where the specimen is in dynamic state. Static tests are categorized into macro-tests where the bond area is >3 mm2 and micro-tests with <3 mm2 bond area.[5]
Macro-test methods
The macro-bond strength can be measured in shear, tensile, or using a push-out protocol.[11] Though macro-tests are known for their simplicity, they have their inherent shortcomings.[12] Micro-bond strength test methods, with bond area less than 3 mm2 will be discussed in the second part of this review.
Macro-shear (SBS) test
In a shear bond test, two materials are connected via an adhesive agent and loaded in shear until fracture occurs. It was the most widely used test[13] as no further specimen processing was required after the bonding procedure.[5] The pull-out test is a type of shear bond test that can be used to test the retentive ability of endodontic posts.[14]
A meta-analysis of factors involved in bond strength testing revealed the significant influence of various parameters like those related to the dentin substrate, composite, and bonding area,[15] storage conditions of the bond assemblies, and test design.[16] Another source of variability is the different configurations employed to apply the shear force, including wire loops, points, and knife edges.[17] The most frequently ignored guideline in the test protocol following the ISO/TS 11405 specification (2003)[8] was that “a limitation of the bonding area is important.”
Macro-tensile (TBS) test
In a tensile bond test, load will be exerted on either sides of the test specimen. The specimen can be held by active or passive gripping methods. Active gripping method involves mechanical fastening of specimen to gripping device, such as glue or clamps, whereas in passive gripping method, specimen is placed in a testing device without the aid of glue or mechanical gripping.[18] In the tensile test, stresses are far more homogeneous across the interface than in shear and, therefore, maximum principal stress values are much closer to the nominal strength.[12,19] It can be used to measure, for instance, the bond strength of cements to hard materials such as ceramics and metal alloys.[5]
Push-out (PO) test
In this method, load is applied through a plunger mounted in the universal testing machine. The plunger must provide near complete coverage of the testing material without touching the root canal wall.[20] This method is useful to test adhesion of root canal sealers[21] and retention of posts luted in root canals.[22]
A finite element analysis[23] recommended that 1. Pin diameter should be 0.85 times smaller than the filler diameter but it should not be so small as to puncture the filler material; 2. Push-out bond strength formula (F = 2πrT)[21] is only suitable for a specimen thickness larger than 0.6 times the filler, where F = failure load, P = girth quotient, r = radius of the filling material, T = thickness of the specimen; 3. When the elastic modulus of the filler (Ef) is smaller than that of dentin (Ed), the modified formula for the push-out bond strength test is (F = 2πrT) √Ed /Ef, otherwise the formula is (F = 2πrT) √Ef /Ed, where Ed = Elastic modulus of dentin and Ef = Elastic modulus of filler.
Dynamic tests
Under clinical circumstances, the adhesive interface of a restoration is hardly submitted to acute tensile stresses. It is rather exposed to cyclic, sub-critical loadings produced during chewing.[24] It is necessary to supplement static bond-strength data with dynamic fatigue data in better simulation of clinical functioning.[25] Different fatigue protocols were used like Macro/Micro shear fatigue test,[25,26] Macro/Micro push-out fatigue test,[27] Micro-tensile fatigue test,[10] Micro-rotary fatigue test[28] Micro-4-point-bend fatigue test.[29]
There are two approaches to determine fatigue: Fatigue limit by stair case approach and fatigue life approach.[30] When a comparison was made between these two approaches, it was found that shear bond strength was not a good indicator for the fatigue behavior of the bonds.[31] Unfortunately, despite an alleged need, no standard for fatigue testing of adhesives today exists.[32]
VARIABLES INFLUENCING MACRO-BOND STRENGTH TEST RESULTS
Variables related to the clinical situation and the substrate treatment
Many factors influence bond strength test results [Figure 1].
Figure 1.
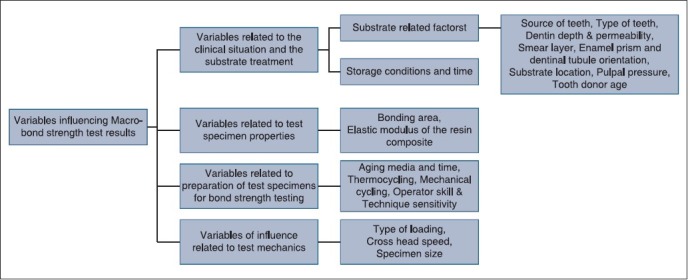
Variables influencing Macro-test results
Substrate related factors
Many variables related to substrate (enamel/dentin) and their treatments affect the bond strength. Unfortunately all these factors cannot be easily controlled.[16]
Source of teeth
Due to the inadequate availability of human teeth, animal teeth were used in many in vitro studies.[33,34,35,36,37] Bovine enamel and dentin give bond strength values similar to that of human permanent teeth.[34,35]
Conversely, some studies reported high shear and tensile bond strength in human enamel compared to bovine enamel.[36] Push-out bond strength was also significantly higher in human root dentin compared to bovine root dentin.[37]
Inconsistent recommendations were proposed regarding the use of bovine substrate as an alternative to human substrate in bonding/adhesive strength studies.[38] If bovine teeth are used, superficial layers of dentin have to be used as dentinal tubules are larger than human dentinal tubules.[39] Porcine teeth could also be potential substitutes for in vitro tooth adhesion investigations.[40] It must be remembered that for better accuracy of the bond strength tests human teeth are preferred.
Type of teeth
Various types of teeth were used to study bond strengths, and the results of enamel SBS were significantly varied with both tooth type and adhesive system.[41,42] In a study reported, high shear bond strengths were observed in canines when compared to that of molars.[43]
In some studies, there were significant differences between the bond strength values of teeth in the upper and lower arches.[44] To obtain reliable results in enamel bond strength studies, the same tooth type from the upper or lower arches should be used.
Dentin depth and permeability
Dentin permeability increases almost logarithmically with cavity depth.[45] In majority of studies, lower shear bond strengths were reported with increased dentin depth and permeability,[43,46] and this permeability is less when smear layer was retained. As bonding systems became more hydrophilic, the sensitivity of shear bond strengths to dentin depth was not significant.[47]
A relationship was established between percentage area of solid dentin available for bonding and the shear bond strength acquired. The percentage area of solid dentin available for bonding was expressed as the difference between the total area of dentin and the percentage area of exposed dentinal tubules.[48]
Contrary to shear bond strengths, no differences were observed in tensile bond strengths of newer adhesives.[49,50] Studies with different percentage areas of solid dentin available for bonding are more reliable than studies at different dentin depths.
Smear layer
Contradictory studies were reported by researchers regarding the effect of smear layer.[51,52] Significant differences in bond strengths were reported at different dentin depths but not if the smear layer was left undisturbed.[53] Quality of smear layer (density rather than thickness) can affect the bond strengths to dentin.[51] Since either removal or modification of smear layer is a justified protocol in dentistry, the need of bond strength studies performed with intact smear layer is questionable.
Enamel prisms and dentinal tubule orientation
Due to its prismatic morphology, enamel exhibits anisotropic mechanical properties. Composite resin restorations will have a longer life span if the enamel walls are given marginal forms to produce transverse sections of enamel prisms rather than longitudinal sections.[54] Midcoronal dentin had similar shear strengths in the two orientations whereas they were different in central and cusp areas. This was due to different dentinal tubule orientation.[55] Hence, while comparing adhesives, orientation of enamel prisms and dentinal tubules must be considered.
Substrate location
Very few macro-test studies were reported regarding effect of regional variables (occlusal/buccal dentin) on dentin bonding. High shear bond strengths to occlusal dentin were observed than buccal dentin[56] whereas tensile bond strengths were 20-30% higher for buccal dentin.[57] Thus, substrate location has to be specified while studying bond strength.
Pulpal pressure
The simulation of in vivo conditions may be refined by applying hydrostatic intrapulpal pressure to the pulp chamber of extracted teeth during adhesive application.[58] To simulate dentinal liquor, distilled water or saline have often been used.[59,60,61] Studies showed varied results[59,60,61,62] as the effect of hydrostatic intrapulpal pressure on shear bond strength depends on the type of bonding system employed.[61]
Tooth donor age
In older teeth, as a result of the reduction in tubule diameter, there is also a decrease in dentin permeability.[63] Though mechanical properties of aged dentin vary from those of younger dentin,[64] similar tensile bond strengths were observed.[49,65] More studies are needed to draw any conclusion.
Storage conditions and time
Distilled water, saline, 0.05% saturated solution of thymol, 0.5% chloramine-T, 2% gluteraldehyde, and 10% formalin solutions were studied as storage media for bond strength tests.[11,66] Storage in sodium hypochlorite (NaOCl) resulted in lower bond strengths, while sterilization with the autoclave negatively affected the bond strength. Storage in 10% formalin resulted in varied bond strengths.[67,68] Camps et al.[69] recommended cryopreservation up to 12 weeks or short-term refrigeration not more than two days. According to the ISO technical specification 11405, bond strengths should be measured immediately post-extraction but not more than six months.[8]
Variables related to test specimen properties
Bonding area
Very few studies evaluated the influence of area on “macro-bond” strengths. Sano et al. reported that for specimens with rectangular bonding areas between 0.25-11.65 mm2, tensile bond strength to dentin was shown to decrease as bonding area increased, following a logarithmic function.[70] A similar trend was noticed in shear bond strengths where smaller surface areas had significantly higher values when compared with those of larger areas.[71]
The ISO/TR 11405 does not identify a specific value for bond area but it mentions a clear delimitation of the bonding area as an important requirement and shows a diagram of a split mould with a 3-mm diameter hole.[8] It is recommended that the diameter of the bonded surface must be taken into consideration while comparing bond strengths.
Elastic modulus of the resin composite
The use of stiffer composites may significantly increase bond strength values. There was a weak but statistically significant correlation between dentin bond strength and composite flexural properties.[19,72,73] Hence, while testing bond strength of an adhesive, it is recommended to select a composite resin with a comparable elastic modulus.
Variables related to specimen preparation for bond strength testing
Several researchers have attempted to age the composite substrate in order to mimic the situation of bonding new composite to old composite in the oral cavity.[50,74]
Aging media and time
The most common storage type for test pieces is water for various time intervals up to three months. This may be at room temperature or simulated mouth temperature. Artificial saliva and sodium hypochlorite were also used for ageing of the samples. Aging did not have any effect on the tensile bond strength of composite to dentin,[50] while six months of aging in water decreased shear bond strength.[74]
Thermal cycling
Thermal cycling has been used as a technique to simulate clinical conditions. Mair found that oral temperature changes between −4°C-0°C when eating ice cream and 60°C-65°C when eating a hot cheese sandwich.[75] Majority of studies showed that thermocycling significantly reduced the shear bond strengths of dentin.[74,76,77] Miyazaki et al. found decrease in the mean enamel bond strength after thermocycling, while dentin bond strengths significantly decreased after 30,000 thermal cycles.[78,79]
Thermal changes in teeth have also been modeled by the finite element approach.[80] As most of the time restorations are subjected to a very small temperature variation, thermal cycling may not have a significant effect but it can lead to spontaneous debonding of specimens.[81] A short thermal cycling regimen of 500 cycles is recommended by the ISO TR 11450 standard (2003).[8]
Mechanical cycling
The amount of load exerted while chewing and swallowing varies between 70-150 N,[82] and cyclic compression is the most common stress that was active in the mouth.[83] Majority of in vitro studies used monotonic tests such as tensile, compression, shear, or flexural strength to study the properties of a material.[84] As these tests cannot simulate cumulative damage (fatigue) that occurs in the mouth, studies with fatigue tests are recommended for better clinical relevance.[75]
A metallic plunger attached to a cyclic loading machine is placed in contact with the restoration, and a fixed amount of cyclic axial load is delivered at frequency of 2-3 cycles/s.[85] Load application of 500,000 cycles is equivalent to six months and 1,000,000 cycles is equivalent to one year of in vivo mastication.[86] A reduction in shear bond strength was observed when 100 N load and 500,000 cycles were applied.[85]
Operator skill and technique sensitivity
Operator skill[87,88] and technique sensitivity[89,90] influenced the dentin bond strengths. Hence, it is recommended to involve different operators with uniform basic training in each series of experiments.
Variables of influence related to test mechanics
Specimen size
Size of specimen affects the size of bond area, which was discussed in the section bonding area.
Type of loading
The choice of testing assembly has great influence on stress distribution. The use of a knife-edge chisel causes severe stress concentration at the load application area than wire loop[12,17] and stainless steel tape allowed more uniform stress distribution at the bond interface.[91]
The distance between the point of load application and the bonded interface in shear tests also affects stress distribution.[92] In an attempt to standardize the test protocol, specific jigs have been prepared, such as Ultradent jig and SDI rig.[5]
In a push-out bond test, punch diameter may affect the bond strength. No effect was observed when the diameter was 90% of the canal diameter but bond strength was lower when the punch diameter was 50-60% of the canal size.[93]
Cross head speed
Conflicting findings were published on the influence of crosshead speed on dentin bond strengths. Different cross-head speeds may influence the shear bond strength and the fracture pattern in dentin substrate.[94,95] Shear bond strength using crosshead speeds of 0.50 mm/min and 0.75 mm/min should be preferred due to their better cohesive versus adhesive results.[96] A similar contradiction was observed with two studies that evaluated the effect of crosshead speed on tensile bond strength.[50,97]
GUIDE LINES
Present day data reporting high dentin bond strengths by not utilizing standardized protocol may mislead the scientific community. The following would improve the validity of dental adhesive evaluations:
A universal sample size needs to be established for future tensile bond strength studies.
Existing variables that are standardized by the International Organization for Standardization should be adhered to by researchers.
Products should undergo a combination of testing.
Improvement in standardization of study variables should be combined with standardized data from gap measurement tests, microleakage tests, and the clinical usage tests for a better clinical correlation.[98]
CONCLUSION
Researchers should make every effort to design a more standardized test methodology while evaluating bond strength test. Data to be included while reporting a study are type of test, tooth notation, source of teeth, type of substrate, depth and location of substrate, direction of enamel rods and dentinal tubules, existence of pulpal pressure, status of smear layer, storage medium and time of extracted teeth, film thickness of the adhesive, dimensions of area of contact, mechanical properties of composite, aging protocol, thermal cycling regime, type and rate of load application, cross head speed, and type of failure. Despite their inherent shortcomings, macro-bond strength tests may continue to be used for evaluating the adhesion of dental materials to tooth structure due to their simplicity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sudsangiam S, van Noort R. Do dentin bond strength tests serve a useful purpose? J Adhes Dent. 1999;1:57–67. [PubMed] [Google Scholar]
- 2.Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;28:215–35. [PubMed] [Google Scholar]
- 3.Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B. Clinical effectiveness of contemporary adhesives: A systematic review of current clinical trials. Dent Mater. 2005;21:864–81. doi: 10.1016/j.dental.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Stanley HR. An urgent plea for a standardized bonding (adhesion) test. J Dent Res. 1993;72:1362–3. doi: 10.1177/00220345930720100101. [DOI] [PubMed] [Google Scholar]
- 5.Van Meerbeek B, Peumans M, Poitevin A, Mine A, Van Ende A, Neves A, et al. Relationship between bond-strength tests and clinical outcomes. Dent Mater. 2010;26:e100–21. doi: 10.1016/j.dental.2009.11.148. [DOI] [PubMed] [Google Scholar]
- 6.Oilo G. Adhesion of dental materials to dentine: Debonding tests. In: Thylstrup A, Leach SA, Qvist V, editors. Dentine and dentine reactions in the oraI cavity. Oxford: IRL Press Ltd.; 1987. pp. 219–24. [Google Scholar]
- 7.Versluis A, Tantbirojn D, Douglas WH. Why do shear bond tests pull out dentin? J Dent Res. 1997;76:1298–307. doi: 10.1177/00220345970760061001. [DOI] [PubMed] [Google Scholar]
- 8.Dental materials - testing of adhesion to tooth structure. Second ed. Switzerland: 2003. Technical specification ISO/TS 11405. [Google Scholar]
- 9.Heintz SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007;9:77–106. [PubMed] [Google Scholar]
- 10.Poitevin A, De Munck J, Cardoso MV, Mine A, Peumans M, Lambrechts P, et al. Dynamic versus static bond-strength testing of adhesive interfaces. Dent Mater. 2010;26:1068–76. doi: 10.1016/j.dental.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Salz U, Bock T. Testing adhesion of direct restoratives to dental hard tissue - A review. J Adhes Dent. 2010;12:343–71. doi: 10.3290/j.jad.a19741. [DOI] [PubMed] [Google Scholar]
- 12.Braga RR, Meira JB, Boaro LC, Xavier TA. Adhesion to tooth structure: A critical review of “macro” test methods. Dent Mater. 2010;26:e38–49. doi: 10.1016/j.dental.2009.11.150. [DOI] [PubMed] [Google Scholar]
- 13.Burke FJ, Hussain A, Nolan L, Fleming GJ. Methods used in dentine bonding tests: An analysis of 102 investigations on bond strength. Eur J Prosthodont Rest Dent. 2008;16:158–65. [PubMed] [Google Scholar]
- 14.Drummond JL, Toepke TR, King TJ. Thermal and cyclic loading of endodontic posts. Eur J Oral Sci. 1999;107:220–4. doi: 10.1046/j.0909-8836.1999.eos1070310.x. [DOI] [PubMed] [Google Scholar]
- 15.De Munck J, Mine A, Poitevin A, Van Ende A, Van Meerbeek G. Testing bond strength. A review of the literature. Dent Mater. 2010;26:e139–40. doi: 10.1016/j.dental.2009.11.148. [DOI] [PubMed] [Google Scholar]
- 16.Leloup G, D’Hoore W, Bouter D, Degrange M, Vreven J. Meta-analytical review of factors involved in dentin adherence. J Dent Res. 2001;80:1605–14. doi: 10.1177/00220345010800070301. [DOI] [PubMed] [Google Scholar]
- 17.DeHoff PH, Anusavice KJ, Wang Z. Three-dimensional finite element analysis of the shear bond test. Dent Mater. 1995;11:126–31. doi: 10.1016/0109-5641(95)80047-6. [DOI] [PubMed] [Google Scholar]
- 18.Armstrong S, Geraldeli S, Maia R, Raposo LH, Soares CJ, Yamagawa J. Adhesion to tooth structure: A critical review of “micro” bond strength test methods. Dent Mater. 2010;26:e50–62. doi: 10.1016/j.dental.2009.11.155. [DOI] [PubMed] [Google Scholar]
- 19.Van Noort R, Noroozi S, Howard IC, Cardew G. A critique of bond strength measurements. J Dent. 1989;17:61–7. doi: 10.1016/0300-5712(89)90131-0. [DOI] [PubMed] [Google Scholar]
- 20.Jainaen A, Palamara JE, Messer HH. Push-out bond strengths of the dentine — sealer interface with and without a main cone. Int Endod J. 2007;40:882–90. doi: 10.1111/j.1365-2591.2007.01308.x. [DOI] [PubMed] [Google Scholar]
- 21.Ungor M, Onay EO, Orucoglu H. Push-out bond strengths: The Epiphany-Resilon endodontic obturation system compared with different pairings of Epiphany, Resilon, AH Plus and gutta-percha. Int Endod J. 2006;39:643–7. doi: 10.1111/j.1365-2591.2006.01132.x. [DOI] [PubMed] [Google Scholar]
- 22.Goracci C, Tavares AU, Fabianelli A, Monticelli F, Raffaelli O, Cardoso PC, et al. The adhesion between fiber posts and root canal walls: Comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004;112:353–61. doi: 10.1111/j.1600-0722.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 23.Chen WP, Chen YY, Huang SH, Lin CP. Limitations of push-out test in bond strength measurement. J Endod. 2013;39:283–7. doi: 10.1016/j.joen.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 24.De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: Methods and results. J Dent Res. 2005;84:118–32. doi: 10.1177/154405910508400204. [DOI] [PubMed] [Google Scholar]
- 25.Braem M. Microshear fatigue testing of tooth/adhesive interfaces. J Adhes Dent. 2007;9:249–53. [PubMed] [Google Scholar]
- 26.Ruse ND, Shew R, Feduik D. In vitro fatigue testing of a dental bonding system on enamel. J Biomed Mater Res. 1995;29:411–5. doi: 10.1002/jbm.820290316. [DOI] [PubMed] [Google Scholar]
- 27.Frankenberger R, Strobel WO, Krämer N, Lohbauer U, Winterscheidt J, Winterscheid B, et al. Evaluation of the fatigue behaviour of the resin-dentin bond with the use of different methods. J Biomed Mater Res B Appl Biomater. 2003;67:712–21. doi: 10.1002/jbm.b.10052. [DOI] [PubMed] [Google Scholar]
- 28.De Munck J, Arita A, Shirai K, Van Landuyt KL, Coutinho E, Poitevin A, et al. Microrotary fatigue resistance of a HEMA-free all-in-one adhesive bonded to dentin. J Adhes Dent. 2007;9:373–9. [PubMed] [Google Scholar]
- 29.Staninec M, Kim P, Marshall GW, Ritchie RO, Marshall SJ. Fatigue of dentin-composite interfaces with four-point bend. Dent Mater. 2008;24:799–803. doi: 10.1016/j.dental.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Draughn RA. Compressive fatigue limits of composite restorative materials. J Dent Res. 1979;58:1093–6. doi: 10.1177/00220345790580031101. [DOI] [PubMed] [Google Scholar]
- 31.Padipatvuthikul P, Mair LH. Comparison of shear bond strength, fatigue limit and fatigue life in resin-bonded metal to enamel bonds. Dent Mater. 2008;24:674–80. doi: 10.1016/j.dental.2007.06.034. [DOI] [PubMed] [Google Scholar]
- 32.Braem M, Lambrechts P, Vanherle G. Clinical relevance of laboratory fatigue studies. J Dent. 1994;22:97–102. doi: 10.1016/0300-5712(94)90010-8. [DOI] [PubMed] [Google Scholar]
- 33.Pashley EL, Tao L, Mackert JR, Pashley DH. Comparison of in vivo vs in vitro bonding of composite resin to the dentin of canine teeth. J Dent Res. 1988;67:467–70. doi: 10.1177/00220345880670020601. [DOI] [PubMed] [Google Scholar]
- 34.Nakamichi I, Iwaku M, Fusayama T. Bovine teeth as possible substitutes in the adhesion test. J Dent Res. 1983;62:1076–81. doi: 10.1177/00220345830620101501. [DOI] [PubMed] [Google Scholar]
- 35.Muench A, da Silva EM, Ballester RY. Influence of different dentinal substrates on the tensile bond strength of three adhesive systems. J Adhes Dent. 2000;2:209–12. [PubMed] [Google Scholar]
- 36.Oesterle LJ, Shellhart WC, Belanger GK. The use of bovine enamel in bonding studies. Am J Orthod Dentofacial Orthop. 1998;114:514–9. doi: 10.1016/s0889-5406(98)70171-4. [DOI] [PubMed] [Google Scholar]
- 37.Galhano G, de Melo RM, Valandro LF, Bottino MA. Comparison of resin push-out strength to root dentin of bovine- and human-teeth. Indian J Dent Res. 2009;20:332–6. doi: 10.4103/0970-9290.57378. [DOI] [PubMed] [Google Scholar]
- 38.Yassen GH, Platt JA, Hara AT. Bovine teeth as substitute for human teeth in dental research: A review of literature. J Oral Sci. 2011;53:273–82. doi: 10.2334/josnusd.53.273. [DOI] [PubMed] [Google Scholar]
- 39.Sanches RP, Otani C, Damiao AJ, Miyakawa W. AFM characterization of bovine enamel and dentine after acid-etching. Micron. 2009;40:502–6. doi: 10.1016/j.micron.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 40.Lopes FM, Markarian RA, Sendyk CL, Duarte CP, Arana-Chavez VE. Swine teeth as potential substitutes for in-vitro studies in tooth adhesion: A SEM observation. Arch Oral Biol. 2006;51:548–51. doi: 10.1016/j.archoralbio.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 41.Hobson RS, McCabe JF, Hogg SD. Bond strength to surface enamel for different tooth types. Dent Mater. 2001;17:184–9. doi: 10.1016/s0109-5641(00)00068-3. [DOI] [PubMed] [Google Scholar]
- 42.Linklater RA, Gordon PH. An ex vivo study to investigate bond strengths of different tooth types. J Orthod. 2001;28:59–65. doi: 10.1093/ortho/28.1.59. [DOI] [PubMed] [Google Scholar]
- 43.Pashley EL, Tao L, Mathews WG, Pashley DH. Bond strengths to superficial, intermediate and deep dentin in vivo with four dentin bonding systems. Dent Mater. 1993;9:19–22. doi: 10.1016/0109-5641(93)90099-c. [DOI] [PubMed] [Google Scholar]
- 44.Oztürk B, Malkoç S, Koyutürk AE, Catalbas B, Ozer F. Influence of different tooth types on the bond strength of two orthodontic adhesive systems. Eur J Orthod. 2008;30:407–12. doi: 10.1093/ejo/cjn006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garberoglio R, Brännström M. Scanning electron microscopic investigation of human dentinal tubules. Arch Oral Biol. 1976;21:355–62. doi: 10.1016/s0003-9969(76)80003-9. [DOI] [PubMed] [Google Scholar]
- 46.Tagami J, Tao L, Pashley DH. Correlation among dentin depth, permeability and bond strength of adhesive resins. Dent Mater. 1990;6:45–50. doi: 10.1016/0109-5641(90)90044-f. [DOI] [PubMed] [Google Scholar]
- 47.Prati C, Pashley DH. Dentin wetness, permeability, thickness and bond strength of adhesive systems. Am J Dent. 1992;5:33–8. [PubMed] [Google Scholar]
- 48.Suzuki T, Finger WJ. Dentin adhesives: Site of dentin vs. bonding of composite resins. Dent Mater. 1988;4:379–83. doi: 10.1016/S0109-5641(88)80053-8. [DOI] [PubMed] [Google Scholar]
- 49.Burrow MF, Takakura H, Nakajima M, Inai N, Tagami J, Takatsu T. The influence of age and depth of dentin on bonding. Dent Mater. 1994;10:241–6. doi: 10.1016/0109-5641(94)90068-x. [DOI] [PubMed] [Google Scholar]
- 50.Takemori T, Chigira H, Itoh K, Hisamitsu H, Wakumoto S. Factors affecting tensile bond strength of composite to dentin. Dent Mater. 1993;9:136–8. doi: 10.1016/0109-5641(93)90090-d. [DOI] [PubMed] [Google Scholar]
- 51.Koibuchi H, Yasuda N, Nakabayashi N. Bonding to dentin with a self-etching primer: The effect of smear layers. Dent Mater. 2001;17:122–6. doi: 10.1016/s0109-5641(00)00049-x. [DOI] [PubMed] [Google Scholar]
- 52.Tani C, Finger WJ. Effect of smear layer thickness on bond strength mediated by three all-in-one self-etching priming adhesives. J Adhes Dent. 2002;4:283–9. [PubMed] [Google Scholar]
- 53.Tao L, Pashley DH. Shear bond strengths to dentin: Effects of surface treatments, depth and position. Dent Mater. 1988;4:71–8. doi: 10.1016/S0109-5641(88)80052-6. [DOI] [PubMed] [Google Scholar]
- 54.Munechika T, Suzuki K, Nishiyama M, Ohashi M, Horie K. A comparison of the tensile bond strengths of composite resins to longitudinal and transverse sections of enamel prisms in human teeth. J Dent Res. 1984;63:1079–82. doi: 10.1177/00220345840630081501. [DOI] [PubMed] [Google Scholar]
- 55.Watanabe LG, Marshall GW, Jr, Marshall SJ. Dentin shear strength: Effects of tubule orientation and intra tooth location. Dent Mater. 1996;2:109–15. doi: 10.1016/S0109-5641(96)80077-7. [DOI] [PubMed] [Google Scholar]
- 56.Belli S, Unlü N, Ozer F. Bonding strength to two different surfaces of dentin under simulated pulpal pressure. J Adhes Dent. 2001;3:145–52. [PubMed] [Google Scholar]
- 57.Øilo G, Olsson S. Tensile bond strength of dentin adhesives: A comparison of materials and methods. Dent Mater. 1990;6:138–44. doi: 10.1016/s0109-5641(05)80045-4. [DOI] [PubMed] [Google Scholar]
- 58.Pashley DH. In vitro simulations of in vivo bonding conditions. Am J Dent. 1991;4:237–40. [PubMed] [Google Scholar]
- 59.Pioch T, Staehle HJ, Schneider H, Duschner H, Dorfer CE. Effect of intrapulpal pressure simulation in-vitro on shear bond strengths and hybrid layer formation. Am J Dent. 2001;14:319–23. [PubMed] [Google Scholar]
- 60.Nikaido T, Burrow MF, Tagami J, Takatsu T. Effect of pulpal pressure on adhesion of resin composite to dentin: Bovine serum versus saline. Quintessence Int. 1995;26:221–6. [PubMed] [Google Scholar]
- 61.Prati C, Pashley DH, Montanari G. Hydrostatic intrapulpal pressure and bond strength of bonding systems. Dent Mater. 1991;7:54–8. doi: 10.1016/0109-5641(91)90028-w. [DOI] [PubMed] [Google Scholar]
- 62.Pameijer CH, Louw NP. Significance of pulpal pressure during clinical bonding procedures. Am J Dent. 1997;10:214–8. [PubMed] [Google Scholar]
- 63.Murray PE, Stanley HR, Matthews JB, Sloan AJ, Smith AJ. Age-related odontometric changes of human teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:474–82. doi: 10.1067/moe.2002.120974. [DOI] [PubMed] [Google Scholar]
- 64.Senawongse P, Otsuki M, Tagami J, Mjör I. Age-related changes in hardness and modulus of elasticity of dentine. Arch Oral Biol. 2006;51:457–63. doi: 10.1016/j.archoralbio.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 65.Tagami J, Nakajima M, Shono T, Takatsu T, Hosoda H. Effect of aging on dentin bonding. Am J Dent. 1993;6:145–7. [PubMed] [Google Scholar]
- 66.Perdigao J. Dentin bonding - Variables related to the clinical situation and the substrate treatment. Dent Mater. 2010;26:e24–37. doi: 10.1016/j.dental.2009.11.149. [DOI] [PubMed] [Google Scholar]
- 67.Lee JJ, Nettey-Marbell A, Cook A, Jr, Pimenta LA, Leonard R, Ritter AV. Using extracted teeth for research: The effect of storage medium and sterilization on dentin bond strengths. J Am Dent Assoc. 2007;138:1599–603. doi: 10.14219/jada.archive.2007.0110. [DOI] [PubMed] [Google Scholar]
- 68.DeWald JP. The use of extracted teeth for in vitro bonding studies: A review of infection control considerations. Dent Mater. 1997;13:74–81. doi: 10.1016/s0109-5641(97)80015-2. [DOI] [PubMed] [Google Scholar]
- 69.Camps J, Baudry X, Bordes V, Dejou J, Pignoly C, Ladeque P. Influence of tooth cryopreservation and storage time on microleakage. Dent Mater. 1996;12:121–6. doi: 10.1016/S0109-5641(96)80079-0. [DOI] [PubMed] [Google Scholar]
- 70.Sano H, Shono T, Sonoda H, Takatsu T, Ciucchi B, Carvalho R, et al. Relationship between surface area for adhesion and tensile bond strength — evaluation of a micro-tensile bond test. Dent Mater. 1994;10:236–40. doi: 10.1016/0109-5641(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 71.El-Askay FM, Nassif MS, Andrade AM, Reis A, Loguercio AD. Effect of surface area and air drying distance on shear strength of etch-and-rinse adhesive. Braz Oral Res. 2012;26:418–23. doi: 10.1590/s1806-83242012005000013. [DOI] [PubMed] [Google Scholar]
- 72.Thomsen KB, Peutzfeldt A. Resin composites: Strength of the bond to dentin versus mechanical properties. Clin Oral Invest. 2007;11:45–9. doi: 10.1007/s00784-006-0077-9. [DOI] [PubMed] [Google Scholar]
- 73.Hasegawa T, Itoh K, Koike T, Yukitani W, Hisamitsu H, Wakumoto S, et al. Effect of mechanical properties of resin composites on the efficacy of the dentin bonding system. Oper Dent. 1999;24:324–30. [PubMed] [Google Scholar]
- 74.Khoroushi M, Rafiei E. Effect of thermocycling and water storage on bond longevity of two self-etch adhesives. Gen Dent. 2013;61:39–44. [PubMed] [Google Scholar]
- 75.Mair L, Padipatvuthikul P. Variables related to materials and preparing for bond strength testing irrespective of the test protocol. Dent Mater. 2010;26:e17–23. doi: 10.1016/j.dental.2009.11.154. [DOI] [PubMed] [Google Scholar]
- 76.Burger KM, Cooley RL, Garcia-Godoy F. Effect of thermocycling times on dentin bond strength. J Esthet Dent. 1992;4:197–8. doi: 10.1111/j.1708-8240.1992.tb00696.x. [DOI] [PubMed] [Google Scholar]
- 77.Helvatjoglu-Antoniades M, Koliniotou-Kubia E, Dionyssopoulos P. The effect of thermal cycling on the bovine dentine shear bond strength of current adhesive systems. J Oral Rehabil. 2004;31:911–7. doi: 10.1111/j.1365-2842.2004.01318.x. [DOI] [PubMed] [Google Scholar]
- 78.Miyazaki M, Sato M, Onose H, Moore BK. Influence of thermal cycling on dentin bond strength of two-step bonding systems. Am J Dent. 1998;11:118–22. [PubMed] [Google Scholar]
- 79.Miyazaki M, Sato M, Onose H. Durability of enamel bond strength of simplified bonding systems. Oper Dent. 2000;25:75–80. [PubMed] [Google Scholar]
- 80.Spierings TA, Peters MC, Bosman F, Plasschaert AJ. Verification of theoretical modeling of heat transmission in teeth by in vivo experiments. J Dent Res. 1987;66:1336–9. doi: 10.1177/00220345870660080901. [DOI] [PubMed] [Google Scholar]
- 81.Tezvergil A, Lassila LV, Vallittu PK. Composite-composite repair bond strength: Effect of different adhesion primers. J Dent. 2003;31:521–5. doi: 10.1016/s0300-5712(03)00093-9. [DOI] [PubMed] [Google Scholar]
- 82.Anderson DJ. Measurement of stress in mastication. I. J Dent Res. 1956;35:664–70. doi: 10.1177/00220345560350050201. [DOI] [PubMed] [Google Scholar]
- 83.Baran G, Boberick K, McCool J. Fatigue of restorative materials. Crit Rev Oral Biol Med. 2001;12:350–60. doi: 10.1177/10454411010120040501. [DOI] [PubMed] [Google Scholar]
- 84.Scherrer SS, Wiskott AH, Coto-Hunziker V, Belser UC. Monotonic flexure and fatigue strength of composites for provisional and definitive restorations. J Prosthet Dent. 2003;89:579–88. doi: 10.1016/s0022-3913(03)00174-4. [DOI] [PubMed] [Google Scholar]
- 85.dos Santos PH, Sinhoreti MA, Consani S, Sobrinho LC, Adabo GL, Vaz LG. Effect of cyclic compressive loading on the bond strength of an adhesive system to dentin after collagen removal. J Adhes Dent. 2005;7:127–35. [PubMed] [Google Scholar]
- 86.Graf H. Bruxism. Dent Clin North Am. 1969;13:659–65. [PubMed] [Google Scholar]
- 87.Sano H, Kanemura N, Burrow MF, Inai N, Yamada T, Tagami J. Effect of operator variability on dentin adhesion: Students vs. dentists. Dent Mater J. 1998;17:51–8. doi: 10.4012/dmj.17.51. [DOI] [PubMed] [Google Scholar]
- 88.Moll K, Fritzenschaft A, Haller B. In vitro comparison of dentin bonding systems: Effect of testing method and operator. Quintessence Int. 2004;35:845–52. [PubMed] [Google Scholar]
- 89.Miyazaki M, Onose H, Moore BK. Effect of operator variability on dentin bond strength of two-step bonding systems. Am J Dent. 2000;13:101–4. [PubMed] [Google Scholar]
- 90.Unlu N, Gunal S, Ulker M, Ozer F, Blatz MB. Influence of operator experience on In vitro bond Strength of dentin adhesives. J Adhes Dent. 2012;14:223–7. doi: 10.3290/j.jad.a22191. [DOI] [PubMed] [Google Scholar]
- 91.Braz R, Sinhoreti MA, Spazzin AO, Loretto SC, Lyra1 AM, Meira-Júnior AD. Shear bond strength test using different loading conditions - a finite element analysis. Braz J Oral Sci. 2010;9:439–42. [Google Scholar]
- 92.Placido E, Meira JB, Lima RG, Muench A, de Souza RM, Ballester RY. Shear versus micro-shear bond strength test: A finite element stress analysis. Dent Mater. 2007;23:1086–92. doi: 10.1016/j.dental.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 93.Pane ES, Palamara JE, Messer HH. Critical evaluation of the push-out test for root canal filling materials. J Endod. 2013;39:669–73. doi: 10.1016/j.joen.2012.12.032. [DOI] [PubMed] [Google Scholar]
- 94.Watanabe LG, Marshall GW, Marshall SJ. Variables Influence on shear bond strength testing to dentin. In: Tagami J, Toledano M, Prati C, editors. Advanced Adhesive Dentistry, 3rd International Kuraray Symposium, Vol. Granada International Symposium. Kuraray Co. Ltd; 1999. pp. 75–9. [Google Scholar]
- 95.Tamura Y, Tsubota K, Otsuka E, Endo H, Takubo C, Miyazaki M, et al. Dentin bonding Influence of bonded surface area and crosshead speed on bond strength. Dent Mater J. 2011;30:206–11. doi: 10.4012/dmj.2010-157. [DOI] [PubMed] [Google Scholar]
- 96.Lindemuth JS, Hagge MS. Effect of universal testing machine crosshead speed on the shear bond strength and bonding failure mode of composite resin to enamel and dentin. Mil Med. 2000;165:742–6. [PubMed] [Google Scholar]
- 97.Oshida Y, Miyazaki M. Dentin bonding system. Part II: Effect of crosshead speed. Bio-Med Mater Eng. 1996;6:87–100. [PubMed] [Google Scholar]
- 98.Stamatacos-mercer C, Hottel TL. The validity of reported tensile bond strength utilizing non-standardized specimen surface areas. An analysis of in vitro studies. Am J Dent. 2005;18:105–8. [PubMed] [Google Scholar]


