Abstract
Aim:
To evaluate the sealing ability of MICRO-MEGA Mineral Trioxide Aggregate, Endosequence, Biodentine as furcation repair materials using a dye extraction leakage method.
Materials and Methods:
Forty mandibular molars were randomly divided according to the material used for perforation repair. Group I- (left unsealed) control, Group II-MICRO-MEGA Mineral Trioxide Aggregate, Group III - Endosequence, Group IV - Biodentine. All samples were subjected to orthograde and retrograde methylene blue dye challenge followed by dye extraction with 65% nitric acid. Samples were then analyzed using Ultra violet (UV) Visible Spectrophotometer.
Results:
Biodentine showed highest dye absorbance, whereas Endosequence showed lowest dye absorbance when compared with other repair materials.
Conclusion:
Within the limitations of this study, it was observed that Endosequence showed better sealing ability when compared with other root repair materials.
Keywords: Dye extraction, furcation repair, perforation, sealing ability
INTRODUCTION
Maintaining the integrity of the natural dentition is important for proper function and natural esthetics. Endodontic therapy can play a vital role in achieving this goal. Occasionally mishaps occur during endodontic treatment. One of them is perforation of root canal wall, which can significantly impact the long-term prognosis of the tooth. Furcation perforation refers to a mid-curvature opening into the periodontal ligament space and is the worst possible outcome in root canal treatment.[1] It has been reported that perforations were the second greatest cause of failure.[2] To prevent bacterial contamination, perforations should be repaired as quickly as possible with a biocompatible material.[3] An ideal perforation repair material should provide an adequate seal, be biocompatible, not affected by blood contamination, not be extruded during condensation, bactericidal, induce bone formation and healing, radiopaque, induce mineralization, cementogenesis and easy in manipulation and placement.[4]
Several materials have been proposed for sealing of perforations. These materials include Zinc-oxide Eugenol cement (Intermediate Restorative Material, Super- Ortho Ethoxy Benzoic Acid), Glass ionomer cement, Resin cements, Resin – modified Glass ionomer cement and Mineral Trioxide Aggregate. However, the divergent outcomes have demonstrated that so far no material has satisfied all the ideal requirements.[5]
Today, most preferred furcation repair materials are bioactive materials like Mineral Trioxide Aggregate, Biodentine.[1] Recently, Endosequence root repair material have been developed as ready to use, premixed bioceramic material recommended for perforation repair, apical surgery, apical plug, and pulp capping.[6]
Thus, the present study is designed to evaluate the sealing ability of MICRO-MEGA Mineral Trioxide Aggregate, Endosequence, and Biodentine in repair of furcation perforations using dye extraction method.
MATERIALS AND METHODS
Forty extracted human mandibular molars with non-fused and well developed roots were used in this study. Cracked teeth were discarded. After extracting, the teeth were kept in 5% sodium hypochlorite for 30 minutes. They were then cleaned from any debris and washed under tap water and kept in normal saline until next step. Molars were amputated 3 mm below the furcation area using a tapered diamond stone. A standardized access cavity was prepared in every molar with a round bur #2, and the root canal orifices were located.
Sticky wax was placed over the orifices of each canal and the sectioned root surface including pulpal floor. It was then coated with two successive layers of varnish in an attempt to increase the marginal seal. To ensure each perforation was centered between the roots, a black marker pen was used to mark the location of the defect. Artificial perforation of 1 mm in diameter was created from the external surface of the tooth with a #2 round carbide bur mounted on a high-speed hand piece with air water coolant [Figure 1a]. The chamber and perforation were flushed with water and dried.
Figure 1.
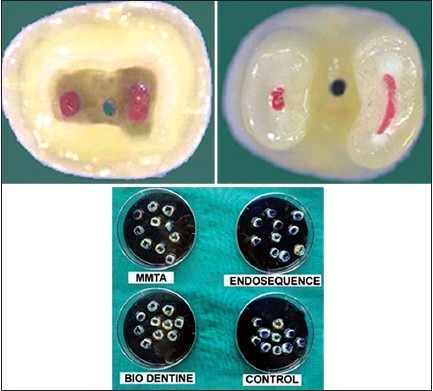
1a: Pulpal floor view of perforation 1b: View of perforation from external surface 1c: Placement of samples in petri dishes
Then, the teeth were randomly divided into four groups.
Group I: Ten molars, in which perforations were left unsealed (Positive control).
Group II: Ten molars, in which perforations were repaired with MICRO-MEGA Mineral Trioxide Aggregate.
Group III: Ten molars, in which perforations were repaired with Endosequence.
Group IV: Ten molars, in which perforations were repaired with Biodentine [Figure 1b].
Each group was placed in separate petri dishes containing 2% methylene blue such that all the teeth were immersed in dye up to the CEJ for retrograde dye challenge, and dye was added to access chamber of each teeth so that it was filled for orthograde dye challenge [Figure 1c]. All samples were stored for 48 hrs. After removal from the dye, teeth were rinsed under running water for 40 minutes and varnish was removed with a polishing disc.
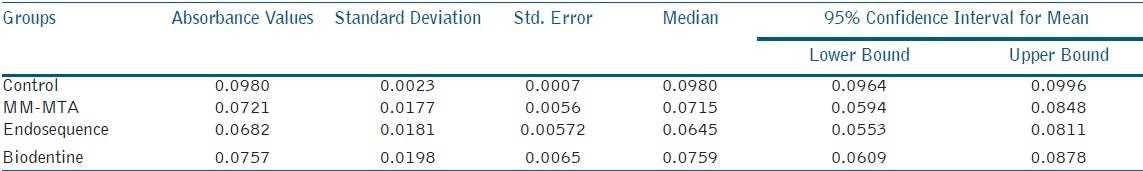
The teeth were placed in vials containing 1 ml of concentrated (65 wt %) nitric acid until complete dissolution. Vials were centrifuged at 9000 rpm for seven minutes. Two hundred μl of the supernatant from each sample was then analyzed in a UV-visible spectrophotometer at 545 nm wavelength using concentrated nitric acid as the blank, and readings were recorded as absorbance units. One-way ANOVA and Tukey's multiple comparison test [Table 1] were done using the Statistical Package SPSS (Statistical package for social science, version 4)
Table 1.
Mean values of four different experimental groups
RESULTS
The mean absorbance values of experimental groups and controls in the current study showed that the positive control samples (Group I) in which perforations were left unrepaired had the highest dye absorbance (0.87 ± 0.09487) of all groups denoting the accuracy of the technique. This was followed by Biodentine (Group IV), which had dye absorbance values (0.49 ± 0.07379) significantly higher than MM-MTA (Group II) and Endosequence (Group III) showed lower dye absorbance than remaining groups.
DISCUSSION
The perforations irrespective of location or etiology may interfere with the prognosis of endodontic treatment. This iatrogenic or mechanical or pathological communication between root canal system and external tooth surface should be sealed with a biocompatible materials as soon as possible.[4] The present study evaluated the sealing ability of MICRO-MEGA Mineral Trioxide Aggregate, Endosequence, and Biodentine as furcation repair materials in mandibular molars using a dye extraction leakage method.
Dye penetration technique has long been used in endodontics because of its ease of performance and difficulty of other available techniques. Dye extraction methodology was employed in this study, which according to Camps J and Pashley gave similar results to the fluid – filtration technique as both are based on quantitative measurements of liquid passage within interfaces.[3] In this study, an ultraviolet spectrophotometry was adopted since it is widely used technique because of its rapid analysis and the cost of the analysis is less expensive. Ultraviolet-visible spectrophotometry refers to absorption spectroscopy or reflectance spectroscopy in the ultraviolet-visible spectral region. This means, it uses light in the visible and adjacent (near-UV and near- infrared) ranges. The absorption or reflectance in the visible range directly affects the perceived color of the chemicals involved.[7]
Mineral Trioxide Aggregate was actually introduced as a root-end filling material; however, because of its biocompatibility, it is now also considered as a material of choice to seal perforations.[8] However, Mineral Trioxide Aggregate has certain drawbacks such as difficulty in handling and very slow setting reaction, which might contribute to leakage, surface disintegration, loss of marginal adaptation, and continuity of the material.[9] In order to overcome these difficulties, MICRO-MEGA introduced endodontic repair cement MICRO-MEGA Mineral Trioxide Aggregate. It is a modified Portland cement with added calcium carbonate, which allows the reduction of the setting time.[10] Biodentine is a calcium silicate-based material that has polycarboxylate-based hydro-soluble polymer system described as water-reducing agent to reduce the overall water content of the mix, along with CaCl2 as a setting accelerator.[4] Biodentine bonds chemo-mechanically with the tooth and composite. This has high compressive and flexural strength.
Endosequence is a bioceramic material composed of calcium silicates, zirconium oxide, tantalum oxide, calcium phosphate monobasic thickening agents, and proprietary fillers.[11] Endosequence has been manufactured to overcome some of the difficult handling characteristics of Mineral Trioxide Aggregate.
The manufacturers of Endosequence material claim that premixed Endosequence putty has a working time of approximately 30+ minutes, a setting reaction initiated by moisture and a final set achieved approximately four hours later with the calcium silicate portion of the material produces a calcium silicate hydrate gel and calcium hydroxide. The calcium hydroxide then interacts with phosphate ions to form hydroxyapatite and water. The water produced continues to react with the calcium silicates to precipitate additional gel like calcium silicate hydrate. According to the developers of the Endosequence, the water supplied through this reaction is an important factor in controlling the hydration rate and the setting time of this material.[12]
Shokouhinejad N et al. tested the bioactivity of Endosequence by exposing the set material on phosphate-buffered saline. There was precipitation of apatite crystalline structures, which is indicative of its bioactivity. Endosequence has been shown to have negligible cytotoxicity and capability to induce cytokine expression.[13] In the current study, control group showed high dye absorbance and Endosequence showed less dye absorbance. A significant difference with this material is its particle size, which allows the premixed material to penetrate into the dentinal tubules and bond to adjacent dentin.[14] According to Ghattas SM et al., EndoSequence™ Root Repair material showed sealing ability similar to white mineral trioxide when used as a root-end filling material.[15]
In the current study, another root repair material used is MM-MTA™ (Micro-Mega®) an endodontic repair cement, developed in order to overcome handling properties of Mineral Trioxide Aggregate.[10] It is a modified Portland cement with added calcium carbonate (CaCO3). MICRO-MEGA Mineral Trioxide Aggregate is delivered in MM-MTA caps. It is biocompatible, radiopaque material with properties like faster setting time, homogenous pasty consistency for easy handling and placement. In this study, MICRO-MEGA Mineral Trioxide Aggregate showed less dye absorbance followed by Endosequence but statistically no significant difference when compared with Biodentine. Based on the results of this study, Biodentine showed high dye absorbance than Endosequence and MICRO-MEGA Mineral Trioxide Aggregate. According to Golberg et al., mechanical strength of Biodentine is time-dependent; at least two weeks are necessary to reach a final setting stage. Even after the initial setting, this material continues to improve in terms of internal structure towards a more dense material with a decrease in porosity.[16]
CONCLUSION
Within the limitations of this study, it was observed that Endosequence showed better sealing ability in furcation repair when compared with other repair materials like MICRO-MEGA Mineral Trioxide Aggregate and Biodentine.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sanghavi T, Shah N, Shah RR. Comparative analysis of sealing ability of biodentine and calcium phosphate cement against mineral trioxide aggregate as a furcal perforation repair material: An in vitro study. National Journal of Integrated Research in Medicine. 2013;4:56–60. [Google Scholar]
- 2.Seltzer S. Endodontic failures – an analysis based on Clinical, roentgen graphic and histologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1967;34:517–30. doi: 10.1016/0030-4220(67)90547-6. [DOI] [PubMed] [Google Scholar]
- 3.Balachandran J, Gurucharan Comparison of sealing ability of bioactive bone cement, mineral trioxide aggregate and Super EBA as furcation repair materials: A dye extraction study. J Conserv Dent. 2013;16:247–51. doi: 10.4103/0972-0707.111326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal V, Singla M, Miglani S, Kohli S. Comparative evaluation of push-out bond strength of ProRoot MTA, Biodentine, and MTA Plus in furcation perforation repair. J Conserv Dent. 2013;16:462–5. doi: 10.4103/0972-0707.117504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El Tawil SB, El Dokkyl NA, El Hamid DA. Sealing ability of MTA versus Portland cement in the repair of furcal perforations of primary molars: A dye extraction leakage model. J Am Sci. 2011;7:1037–43. [Google Scholar]
- 6.Ma J, Shen Y, Stojicic S, Haapasalo M. Biocompatibility of Two Novel Root Repair Materials. J Endod. 2011;37:793–8. doi: 10.1016/j.joen.2011.02.029. [DOI] [PubMed] [Google Scholar]
- 7.Camps J, Pashley D. Reliability of the dye penetration studies. J Endod. 2003;29:592–4. doi: 10.1097/00004770-200309000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Biswas M, Mazumdar D, Neyogi A. Non surgical perforation repair by mineral trioxide aggregate under dental operating microscope. J Conserv Dent. 2011;14:83–5. doi: 10.4103/0972-0707.80729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Girish CS, Ponnappa K, Girish T, Ponappa M. Sealing ability of mineral trioxide aggregate, calcium phosphate and polymethylmethacrylate bone cements on root ends prepared using an Erbium: Yttriumaluminium garnet laser and ultrasonics evaluated by confocal laser scanning microscopy. J Conserv Dent. 2013;16:304–8. doi: 10.4103/0972-0707.114355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tanalp J, Karapinar-Kazandag M. Comparison of the radio opacities of different root-end filling and repair materials. Scientific World Journal. 2013;2:1–13. [Google Scholar]
- 11.Lovato KF, Sedgley CM. Antibacterial activity of endosequence root repair material and proroot MTA against clinical isolates of enterococcus faecalis. J Endod. 2011;37:1542–6. doi: 10.1016/j.joen.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 12.Hirschberg CS, Patel NS, Patel LM, Kadouri DE, Hartwell GR. Comparison of sealing ability of MTA and endosequence bioceramic root repair material: A bacterial leakage study. Quintessence Int. 2013;44:e157–62. [PubMed] [Google Scholar]
- 13.Shokouhinejad N, Nekoofar MH, Razmi H, Sajadi S, Davies TE, Saghiri MA, et al. Bioactivity of endosequence root repair material and bioaggregate. Int Endod J. 2012;45:1127–34. doi: 10.1111/j.1365-2591.2012.02083.x. [DOI] [PubMed] [Google Scholar]
- 14.AlAnezi AZ, Jiang J, Safavi KE. Cytotoxicity evaluation of endosequence root repair material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e122–5. doi: 10.1016/j.tripleo.2009.11.028. [DOI] [PubMed] [Google Scholar]
- 15.Ghattas SM. A comparative evaluation of the sealing ability of two root-end filling materials: An In vitro leakage study using enterococcus faecalis. J Endod. 2011;37:1025–9. doi: 10.1016/j.tripleo.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 16.Zhou HM, Shen Y, Wang ZJ, Li L, Zheng YF, Hakkinen L, et al. In vitro cytotoxicity Evaluation of a novel root repair Material. J Enodod. 2013;39:478–83. doi: 10.1016/j.joen.2012.11.026. [DOI] [PubMed] [Google Scholar]


