Abstract
Traditional interlocked intramedullary (IM) nails have recently been modified to provide enhanced angular stability. These so-called ‘angle-stable’ IM nails are designed to eliminate construct toggle and also provide increased axial, bending, and torsional stiffness. While this added stability is needed for small fracture gaps to heal, angle-stable nails may be too stiff for large fracture gaps to unite. Even though relative stability is recommended for large fracture gaps, recent in vivo data indicates that traditional nails may allow for too much motion for healing to occur. The current study evaluated a modified technique for implanting an angle-stable nail which allows for an intermediate amount of stability. The compliance of the nail construct was adjusted by over-drilling the near cortex interlocking hole. This led to increased construct motion in torsion, but less so in axial compression and bending. This modification creates stability which is partway between angle-stable and traditional IM nail designs. These findings were unchanged after 50,000 fatigue loading cycles. By carefully selecting the magnitude of over-drilling, the compliance of the construct can easily be modified as it is being implanted. This design modification may lead to more reliable fracture union since the surgeon can tailor the nail compliance to the injury and bone quality.
Introduction
Interlocked intramedullary nailing has been used for several decades to treat a variety of long bone fractures1. One recent innovation is the so-called ‘angle-stable’ nail which eliminates screw-to-nail toggle2-6. Such toggle is inherent in traditional interlocked nails which use screws that are intentionally undersized by ˜0.13 mm relative to the nail holes (Figure 1a)7. The slightly oversized nail holes assist in targeting and insertion of the screws without binding5,7. However, the screw-to-nail toggle leads to interfragmentary motion which is particularly noticeable in torsion2,7'10. In vivo studies have shown that eliminating this toggle leads to superior healing for simple fractures in sheep3,5. This work led to several commercially available angle-stable nail designs which all eliminate the screw-nail hole clearance inherent in traditional nails25,11'14. As such, they require careful coaxial alignment of the bone and nail holes.
Figure 1. Traditional interlocked IM nails are designed with slightly oversized, unthreaded interlocking holes (a); this clearance facilitates screw insertion but also allows for construct toggle to occur. Interposing a collar between the screw head and nail with the addition of nail hole threads creates a fixed angle device (b). Overdrilling the near cortex increases the compliance of the angle-stable design proportional to the amount of overdrilling (c).

An alternative design proposed by Garlock et al., allows the bone and nail holes to be misaligned yet still create an angle-stable construct7. The interlocking nail hole is threaded and an oversized collar is interposed between the screw head and nail (Figure 1b). As the screw is tightened, the collar compresses and the screw becomes secured to the nail. The collar allows the near cortical drill hole to be misaligned in any direction by up to 0.6 mm yet still retain angular stability. This reduces the alignment requirements of other angle-stable designs. Mechanical testing of these constructs revealed a reduction in angular deformation from 8.2° (traditional nail) to 2.7° (collared angle-stable nail) at ± 1.5 Nm of torque. Both nails were evaluated by Kubacki et al., in an in vivo canine femur fracture model with a 10 mm segmental defect and periosteal stripping9,10. While all traditional interlocking IM nails progressed to a hypertrophic nonunion, 6/10 angle-stable animals progressed to union. The remaining angle-stable animals showed signs of stress-shielding and did not unite. The toggle inherent in traditional nails may explain the proliferation of tissue in those animals since callus formation is associated with greater interfragmentary motion for secondary healing15-20. Findings of stress shielding from the angle-stable canine data suggest that these IM nails were likely too rigid for segmental defects16,18.
In related work on locking plates, Bottlang et al., sought to reduce near cortex stress shielding by overdrilling the near hole by 0.8 mm for a 4 mm screw15. This increased the interfragmentary motion adjacent to the plate, significantly increased the formation of callus, and led to better healing16. Similar to Bottlang's work, the collared angle-stable nail described above relies on the purchase of the screw to the implant and purchase into the far cortex7. The collared angle-stable IM nail can thus maintain angular stability even though the screw purchases into just the far cortex. By over-drilling the near cortex, the collared end of the screw would have more space to move which would likely increase the motion across the fracture. This is not the case for traditional interlocking IM nails which rely on bicortical screw purchase.
Currently, there are no data in the literature which show how to incrementally control the amount of torsional motion in an angle stable-nail at the point of surgery. In the current study, an angle-stable IM nail implantation technique was modified to create a controlled increase in construct motion by over-drilling the near cortex hole (Figure 1c). One concern was the robustness of this design. Thus, the construct was also subjected to fatigue testing to ensure the integrity of the construct. It was hypothesized that, similar to Bottlang, over-drilling the near cortex hole would increase the compliance of the construct while still maintaining fatigue resistance15,16. Biomechanical data from this modified angle-stable IM nail was compared to historical controls for reference.
Materials and Methods
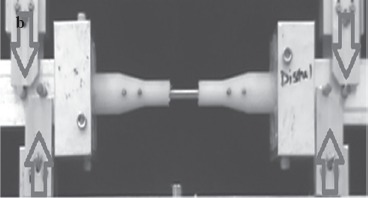
A previously described angle-stable titanium IM nail-interlocking screw construct (Ti6Al4VELI, United Titanium, G&S Titanium, Wooster, OH) and bone analog was the basis for this study7. The nails were 7.5 mm in diameter and had a length of 143 mm. Two 3.5 mm screws were used on either end to interlock the nail to the analog which was segmentally defected with a 30 mm gap (Figure 2). The collars had a 0.4 mm wall thickness and an internal diameter which was 0.6 mm greater than the screw. All screws were secured with a torque wrench to 1.5 Nm.7 Briefly, the bone analog (30% glass filled Nylon 6-6, McMaster-Carr) material mimicked the dimensional and mechanical properties of a canine femur7,8. The bone analogs were machined to include larger diameters at the ends which gradually reduced to a smaller diameter centrally. This was designed to represent the basic hourglass shape of the femur. In addition to the segmental defect, the ‘endosteal’ diameter in the central third was 2.5 mm greater than the nail to ensure the nail and interlocking hardware were the sole load path. Pilot tests confirmed that the nail did not contact the bone analog anywhere along its length except via the interlocking hardware. Detailed dimensions can be found in Garlock et al7. Six samples were tested; the number of replications was anticipated to provide a minimum power of 0.87.
Figure 2. Six fracture analogs were stabilized with 0.5 mm overdrilled collared angle-stable IM nails (Figure 1(c)). The 7.5 mm nails were straight and the endosteal diameter was intentionally oversized by 2.5 mm to ensure the interlocking hardware was challenged as the primary load path. Prior to and after fatigue testing, the constructs were loaded in separate experiments in torsion, compression (a), and four-point bending (b).

The collared angle-stable IM nail design described previously allows for over-drilling of the near cortex without loss of stability. This is due to the screw-collarnail union which creates a fixed angle construct (Figure 1b, 1c). Screw purchase solely in the far cortex still provides bone-to-nail interlocking and prevents toggle from occurring. Pilot tests revealed that progressively enlarging the near cortex hole in 0.2 mm increments caused proportional increases in construct compliance in torsion, axial compression, and bending. The effect was greatest, however, in torsion.
The pilot tests showed that over-drilling the near cortex 0.5 mm was anticipated to yield construct compliance which was partway between the angle-stable and traditional IM nails7. The specimens were prepared for testing per Garlock et al. (Figure 2) by potting both ends of the construct in room temperature-curing epoxy in potting cups7. The exposed portion of the construct between the cups was 174 mm, the typical femur length of a canine femur. The specimens were tested in torsion, compression, and bending for 10 sinusoidal cycles in separate experiments with a materials testing machine (8304 Test Resources, Shakopee, MN) before and after fatigue testing. The constructs were loaded to ±1.5 Nm, 120 N, and 1.43 Nm, in torsion (positive (counterclockwise) and negative (clockwise) rotation through neutral), axial compression, and bending, respectively, with the machine in load-control mode7. The bipolar torsional test was performed at a cyclic frequency of 0.5 Hz (˜1 Hz per direction); the remaining tests were performed in the compressive direction only at 1 Hz; all data were sampled at 80 Hz. The axial compression and bending load magnitudes represent physiologic magnitudes for a medium canine (20 kg)7. While the physiologic torque is estimated to be 0.6 Nm, 1.5 Nm was necessary to elucidate the linear range for stiffness calculations7. Data from the tenth cycle from all tests were analyzed using established methods8,9. Briefly, stiffness was assessed for all loading modes by taking the slope of the linear range of the load (torque, axial compressive or bending force) versus the test machine actuator motion (angular displacement, compressive or bending linear displacement). The torsional stiffness was determined separately for the positive and negative rotation directions. The maximum angular displacement for the torsional tests was taken as the angular displacement that occurred during the tenth ±1.5 Nm peak-peak torsion cycle.
Fatigue testing was performed for 50,000 cycles of combined axial (120 N) and torsional (0.75 Nm) loading7. The supraphysiologic torque magnitude was used to challenge the constructs' performance in its more vulnerable mode6,8. The 50,000 fatigue cycle magnitude represents 12 weeks of unrestricted cage activity by a canine7. The findings from these experiments were compared to historical controls of a traditional interlocked IM nail and a collared angle-stable IM nail that was not over-drilled with a one-way ANOVA and Fisher LSD posthoc testing (a = 0.05)7,21. The historical controls were biomechanically tested with the same protocol used in the current study. Data from the current study were also compared before and after fatigue testing with the paired t-test (a = 0.05). Prior to all statistical analyses, normality was confirmed for all data.
Results*
All over-drilled angle stable specimens (Figure 1c) completed the fatigue testing protocol to 50,000 cycles. The stiffness tended to increase after cycling in axial compression and torsion and decrease in bending, though these findings were not significant (Table 1). The pre-fatigue axial stiffness of the over-drilled IM nails (1,351±167 N/mm) was significantly greater than the historical traditional IM nail (1,171±15 N/mm, p=0.032) (Figure 1a) but was not significantly different from the non-over-drilled angle-stable IM nails (1,445±28 N/mm, p=0.227) (Figure 1b). Following fatigue cycling, the axial stiffness of the non-over-drilled nail (1,664±201 N/mm) was significantly greater than the traditional nail (1,334±15 N/mm, p=0.005) and the over-drilled angle stable nail (1,461±123 N/mm, p=0.039). The over-drilled constructs were toggle free (zero degrees of toggle) similar to the angle stable nails without over-drilling and significantly less than the traditional nail (4.6±1.3° of toggle, p<0.001). The total angular deformation of the over-drilled IM nails (4.3±0.2°) was significantly less than the historical traditional IM nail (8.2±1.1°, p<0.001) and significantly greater than the non-over-drilled anglestable IM nails (2.7±0.1°, p=0.002). The angle stable nail without over-drilling exhibited torsional positive and negative stiffness magnitudes which ranged from 1,137±68 to 1,189±15 N-mm/deg when considering all pre-fatigue and post-fatigue magnitudes for both rotation directions. These values were significantly greater (p<0.001 for all comparisons) than the corresponding torsional stiffness magnitudes for the traditional nail (range 802±4 to 843±79 N-mm/deg) and the over-drilled angle-stable nails (762±74 to 801±8 N-mm/deg). While the over-drilled angle stable nails tended to be lower for all comparisons with the traditional IM nails, this finding was not significant (p=0.065-0.876). None of the bending stiffness magnitude comparisons were significant (p=0.195), though the traditional nail tended to be greater than both angle stable nail designs.
Table 1.
The biomechanical behavior of the over-drilled angle-stable IM nail was compared to a traditional interlocked IM nail and an anglestable IM nail without over-drilling. See Figure 1 and text for additional details.
| Axial Compression (N/mm) | Toggle (°) | Total Angular Deformation (°) | Positive Stiffness (N-mm/°) | Negative Stiffness (N-mm/°) | Bending Stiffness (N-mm/mm) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prefatigue | Postfatigue | Prefatigue | Postfatigue | Prefatigue | Postfatigue | Prefatigue | Postfatigue | Prefatigue | Postfatigue | Prefatigue | Postfatigue | |
| Traditional Nail (Figure 1(a)) | 1,171±15, 1%#@ | 1,334±14.9, 11%@ | 4.6±1.3, 29%@ | 4.7±1.4, 30%@ | 8.2±1.19, 14%@ | 8.3±1.29, 16%@ | 830±71, 9%@ | 843±79, 9%@ | 809±16, 2%@ | 802±45, 6%@ | 13,141±1,175, 8.9%∧ | -§ |
| Angle-Stable Nail w/o overdrilling (Figure 1(b)) | 1,445±28, 2%*@ | 1,664±201, 12%*@ | 0*@ | 0*@ | 2.7±0.1, 6%*@ | 2.6±0.1, 2%*@ | 1,137±68, 6%*@ | 1,185±13, 1%*@ | 1,157±63, 5%*@ | 1,189±15, 1% *@ | 11,967±2,675, 22.3%∧ | -§ |
| Overdrilled Angle-Stable Nail (Figure 1(c)) | 1351±167, 12%* | 1461±123, 8%! | 0* | 0* | 4.3±0.2, 6%*! | 4.2±0.2, 5%*! | 762±74, 10%! | 774±73, 9%! | 765±78, 10%! | 801±83, 10%! | 11,133±1,221, 11% | 10,723±497, 4.6% |
Significantly different than traditional nail;
Significantly different than angle stable nail w/o over-drilling;
Data is presented as mean ± 1 SD (standard deviation); the coefficient of variation (ratio of SD to mean) is presented as an additional measure of data dispersion;
From Garlock et al.,
From Donovan et al.;
Not tested
Discussion
The objective of this study was to biomechanically evaluate modifications to an angle-stable IM nail design. It was found that the mechanical behavior of the construct could be reliably adjusted by over-drilling the near cortex without affecting fatigue life.
Over-drilling the near cortex affected the mechanical response of the construct in torsion more than axial compression or bending. Torsional loading with 0.5 mm of over-drilling produced 4.3±0.2° of angular deformation at ±1.5 Nm of torque. This was approximately half the motion observed with a traditional nail (8.2±1.1°), and 60% more motion than the non-over-drilled angle-stable nail (2.7±0.1°). Despite the increase in angular deformation and decreased torsional stiffness, the construct exhibited zero toggle. Over-drilling the near cortex is a simple technique which can be easily adopted intraoperatively; it only requires a range of drill bit sizes. Based on the pilot data from the current study, the increased motion is related to the magnitude of the over-drilling. For simple fractures with small interfragmentary gaps, no over-drilling is likely warranted. As the complexity of the fracture increases (long fracture gaps, comminution), progressive over-drilling may aid in creating a controlled amount of motion which is tailored to the fracture.
Prior in vivo canine data from several studies suggests that an optimal amount of construct stiffness exists when treating open, complex fractures with segmental loss and periosteal stripping9,10'22. For example, Kubacki et al., showed that traditional canine IM nails led to hypertrophic nonunions which were attributed to excessive torsional construct motion (8.2°)9. Angle-stable IM nails allowed significantly less torsional motion (2.7°) though some fractures did not heal and showed signs of stress shielding9. The optimal mechanical environment for this complex fracture likely lies between the two nails. While numerous studies have sought to establish the optimal mechanical environment for fracture healing, differences in host selection, test methods, fracture type, and implants make it difficult to establish definitive recommendations16.
That said, a variety of in vivo animal studies have shown that axial or shear motion can increase or decrease callus formation and maturation15,17,19,23-25. Dejardin et al., studied an angle-stable nail in a 5 mm canine tibial fracture gap2. This construct exhibited similar torsional behavior to the non over-drilled anglestable collared nail7,9,10. All five of Dejardin's angle-stable animals formed a bony union while the traditional nail animals had several cases of nonunion. Kubacki' et al's, in vivo canine cases of nonunion from the non-over-drilled collared angle-stable IM nails may be related to the increased severity of injury and the longer bone defect9,10. These factors have been shown to challenge the healing response9,10,25.
One limitation of the current study was the use of a bone analog. However, this material has been validated as a model of canine bone by others8. Further, the analog provides greater consistency such that the effect of the construct design can be more clearly determined. Another limitation is the relatively simple sinusoidal, combined torsion-compression loading mode in fatigue. While in vivo loading during gait is likely much more complex, the loading mode used in the current study is common in the literature for combined loading7. While single mode fatigue loading could have been used, it would likely have been less challenging to the construct. An additional limitation is the in vitro nature of the data from the current study. However, Kubacki et al., used a version of this nail for in vivo canine experiments which showed that the angle stable design led to stress shielding and the traditional nail allows too much motion9. As such, data interpolation of the available suggests that the increased motion afforded by the angle stable nail design in the current study would hopefully yield increased cases of union in vivo.
Further work is needed to determine if the overdrilled near cortex concept enhances healing in an animal model. Such in vivo work should include metaphyseal fractures and osteoporotic bone, both of which would likely benefit from the enhanced fixation of angle-stable screws. In cases of comminution or segmental loss, adjustable construct stiffness via over-drilling of the near cortex would allow interfragmentary motion to be progressively increased. The utility of controlled increases in interfragmentary motion has already been demonstrated in vivo with new plating methods such as the far cortical locking technique16. Extending this concept to the nail via the technique described in the current paper will hopefully enhance fracture care by tailoring the interfragmentary motion to a specific case.
Declaration of Conflicting Interests
Research Funding was provided for this work in the form of a grant. See acknowledgments for further details. Two authors (PA, DL) are listed on patents for the intramedullary nail used in the current study.
Acknowledgments
This research and development project/program was conducted by Kettering University and McLaren-Flint and is made possible by a contract/cooperative agreement that was awarded and administered by the U.S. Army Medical Research & Materiel Command (USAM- RMC) and the Telemedicine & Advanced Technology Research Center (TATRC), under Contract Number: W8xWH-07-2-0119.
Non-Endorsement Disclaimer: The views, opinions, and findings contained in this research are those of the company and do not necessarily reflect the views of the Department of Defense and should not be construed as an official DoD/Army policy unless so designated by other documentation. No official endorsement should be made.
Partial financial support was provided via a grant from the McLaren Foundation.
References
- 1.Vécsei V, Hajdu S, Negrin LL. Intramedullary nailing in fracture treatment: history, science and Kuntscher's revolutionary influence in Vienna, Austria. Injury. 2011;42:S1–S5. doi: 10.1016/S0020-1383(11)00419-0. [DOI] [PubMed] [Google Scholar]
- 2.Déjardin LM, Guiot LP, von Pfeil DJ. Interlocking nails and minimally invasive osteosynthesis. Vet Clin North Am Small Anim Pract. 2012;42:935–962. doi: 10.1016/j.cvsm.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Epari DR, Kassi JP, Schell H, et al. Timely fracture-healing requires optimization of axial fixation stability. J Bone Joint Surg Am. 2007;89:1575–1585. doi: 10.2106/JBJS.F.00247. [DOI] [PubMed] [Google Scholar]
- 4.Horn J, Linke B, Höntzsch D, et al. Angle stable interlocking screws improve construct stability of intramedullary nailing of distal tibia fractures: a biomechanical study. Injury. 2009;40:767–771. doi: 10.1016/j.injury.2009.01.117. [DOI] [PubMed] [Google Scholar]
- 5.Kaspar K, Schell H, Seebeck P, et al. Angle stable locking reduces interfragmentary movements and promotes healing after unreamed nailing. Study of a displaced osteotomy model in sheep tibiae. J Bone Joint Surg Am. 2005;87:2028–2037. doi: 10.2106/JBJS.D.02268. [DOI] [PubMed] [Google Scholar]
- 6.Wähnert D, Stolarczyk Y, Hoffmeier KL, et al. Long-term stability of angle-stable versus conventional locked intramedullary nails in distal tibia fractures. BMC Musculoskelet Disord. 2013;14:66. doi: 10.1186/1471-2474-14-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garlock AN, Donovan J, LeCronier DJ, et al. A modified intramedullary nail interlocking design yields improved stability for fatigue cycling in a canine femur fracture model. Proc Inst Mech Eng H. 2012;226:469–476. doi: 10.1177/0954411912443627. [DOI] [PubMed] [Google Scholar]
- 8.Lansdowne JL, Sinnott MT, Dejardin LM, et al. In vitro mechanical comparison of screwed, bolted, and novel interlocking nail systems to buttress plate fixation in torsion and mediolateral bending. Vet Surg. 2007;36:368–377. doi: 10.1111/j.1532-950X.2007.00277.x. [DOI] [PubMed] [Google Scholar]
- 9.Kubacki MR, Verioti CA, Patel SD, et al. Angle stable nails provide improved healing for a complex fracture model in the femur. Clin Orthop Relat Res. 2014;472(4):1300–9. doi: 10.1007/s11999-013-3288-9. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayor D, Kubacki M, LeCronier D, et al. Histologic analysis of a grade IIIb femur fracture model stabilized with angle stable and traditional nails. Proc Annual Mich Orthop Soc. 2013 [Google Scholar]
- 11.Smith & Nephew. Trigen meta-nail system, tibial and retrograde femoral nail. Smith & Nephew. 2011.
- 12.Stryker. T2 Proximal Humeral Nailing System. Stryker Corporation. 2010.
- 13.Synthes Orthopaedics. Intramedullary Fixator. Using the Angle Stable Locking System (ASLS). Synthes Inc. 2009.
- 14.Zimmer. Natural Nail System with Stabilize Technology. Zimmer. 2010.
- 15.Bottlang M, Doornink J, Lujan TJ, et al. Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am. 2010;92:12–22. doi: 10.2106/JBJS.J.00780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bottlang M, Lesser M, Koerber J, et al. Far cortical locking can improve healing of fractures stabilized with locking plates. J Bone Joint Surg Am. 2010;92:1652–1660. doi: 10.2106/JBJS.I.01111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheal EJ, Mansmann KA, DiGioia AM 3rd, et al. Role of interfragmentary strain in fracture healing: ovine model of a healing osteotomy. J Orthop Res. 1991;9:131–142. doi: 10.1002/jor.1100090116. [DOI] [PubMed] [Google Scholar]
- 18.Hak DJ, Toker S, Chengla Y, et al. The influence of fracture fixation biomechanics on fracture healing. Orthopedics. 2010;33:752–755. doi: 10.3928/01477447-20100826-20. [DOI] [PubMed] [Google Scholar]
- 19.Park SH, O'Connor K, McKellop H, et al. The influence of active shear or compressive motion on fracture-healing. J Bone Joint Surg Am. 1998;80:868–878. doi: 10.2106/00004623-199806000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093–1110. doi: 10.1302/0301-620x.84b8.13752. [DOI] [PubMed] [Google Scholar]
- 21.Donovan JP, Garlock A, LeCronier D, et al. Assessment of the stability of an alternative interlocking nail for segmental long bone defects. Proc Annual Mich Orthop Soc. 2011 [Google Scholar]
- 22.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed] [Google Scholar]
- 23.Augat P, Burger J, Schorlemmer S, et al. Shear movement at the fracture site delays healing in a diaphyseal fracture model. J Orthop Res. 2003;21:1011–1017. doi: 10.1016/S0736-0266(03)00098-6. [DOI] [PubMed] [Google Scholar]
- 24.Comiskey DP, MacDonald BJ, McCartney WT, et al. The role of interfragmentary strain on the rate of bone healing-a new interpretation and mathematical model. J of Biomech. 2010;43:2830–2834. doi: 10.1016/j.jbiomech.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 25.Augat P, Margevicius K, Simon J, et al. Local tissue properties in bone healing: influence of size and stability of the osteotomy gap. J Orthop Res. 1998;16:475–481. doi: 10.1002/jor.1100160413. [DOI] [PubMed] [Google Scholar]


