Abstract
Nasal continuous positive airway pressure (nCPAP) in premature babies may rarely lead to necrosis of the columella. Subsequent functional and cosmetic impairments require surgical corrections to restore nasal anatomy and architecture. The objective of this report is to document the technique of reconstruction in a baby with columella necrosis due to nCPAP treatment. A 21-month-old baby was referred to the oral and maxillofacial unit with a necrotic columella following nCPAP ventilation in a neonatal intensive care unit. Nearly 75% of the vertical columella length was affected. A neocolumella was created using tissues mobilised from the nasal sill region. This report provides a detailed description of a columella reconstruction technique which is valuable to restore aesthetics and function.
Background
Nasal continuous positive airway pressure (nCPAP) is used in intensive care units (ICUs) as a form of respiratory support for premature babies. Robertson et al1 have previously described nasal deformities resulting from nCPAP. Within a period of 6 months, these authors found traumatic nose changes in seven cases or 20% of their entire sample, varying from columella to septum necrosis to flaring of nostrils and snub-nosed deformity.
Yong et al2 compared the incidence of nasal trauma due to nasal prongs or nasal masks for nCPAP in a randomised control trial. The incidence of nasal trauma was 29% and 35% for nasal mask and nasal prong, respectively (p=0.5). Whereas in the former group traumatic changes occurred at the junction between the nasal septum and philtrum, the latter group suffered more frequently from trauma of the nasal septum only. There were no cases of columella necrosis in either group.
In 2010 Fischer et al3 classified nasal trauma secondary to nCPAP into three stages: (1) stage I: non-blanching erythema on an otherwise intact skin; (2) stage II: superficial ulcer or erosion with partial thickness skin loss and (3) stage III: necrosis, resulting in full thickness skin loss. In their series of 989 babies, 420 (42.5%) developed traumatic nose changes secondary to nCPAP with only three patients (0.7%) presenting a stage III defect. They further stated that risk of trauma increased in neonates (1) <32 weeks of gestational age, (2) <1500 g at birth weight, (3) with >5 days under nCPAP or (4) with >14 days’ stay in the neonatal ICU.
Apart from discomfort and potential risk of infection nCPAP might lead to nasal trauma with long-term functional or cosmetic impairments.3 Although rare, surgical repair of a necrotic columella is challenging but mandatory to re-establish anatomical architecture of the nose. Although instances of columella necrosis secondary to nCPAP have been reported, the reconstructive strategies for such cases are not well documented. This article describes a technique of reconstruction in a baby with columella necrosis due to nCPAP treatment.
Case presentation
A 21-month-old baby was referred to the oral and maxillofacial unit of the Wilgers Private Hospital, Pretoria, Republic of South Africa, to reconstruct a columella defect. According to the mother, the baby was born prematurely and received nCPAP ventilation in the neonatal ICU for 3 months via nasal prong leading to a pressure necrosis of the columella.
A full thickness skin loss of the columella was noted, exposing the nasal septum, which was covered by a thin layer of granulation tissue. Nearly 75% of the columella vertical length was lost. Moreover, small pressure marks were found bilaterally on the superior border of the alar wing of the nose, with the right side being more affected.
Treatment
Under general anaesthesia and orolaryngeal intubation, the columella was reconstructed using a modified Cronin technique.4 With the baby in supine position, facial disinfection and cleaning of the nose was performed with chlorhexidine gluconate 2% (Medical Distributors, Midrand, Republic of South Africa), followed by draping (figure 1). No local anaesthesia was used due to potentially insufficient blood supply in this region. The initial incision was made from one alar base to the other in a V-shape manner to maintain the anatomy of the labiocolumella junction (figures 2 and 3). The second incision was performed perpendicular to the surface of the anterior nasal floor around 3 mm behind the nostril along the nasal sill on each side. The two incisions were then connected with a blunt scissor. While maintaining the pedicles at the alar bases, mobilisation of the nasal sill tissue towards the nasal tip was performed with a single skin hook, in a gentle continuous upward pull (figure 4).
Figure 1.

The appearance of the columella defect at the time of surgery.
Figure 2.
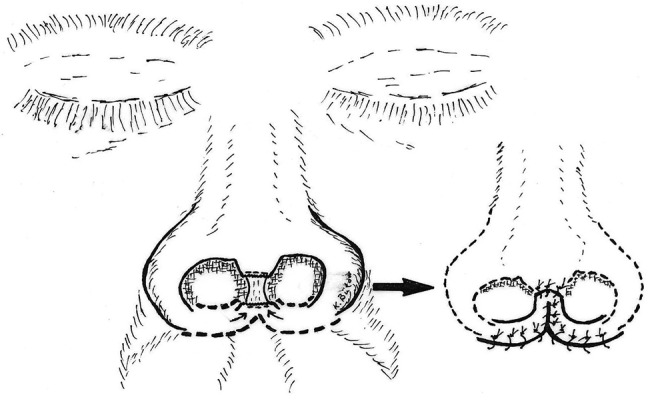
A diagram highlighting the two main incisions (fat dashed lines).
Figure 3.

The first incision along the nasolabial fold.
Figure 4.

Mobilisation of the neocolumella under gentle, steady upward pull.
Once adequate mobilisation was achieved, the scar tissue at the nasal tip and the former columella base was trimmed. The newly formed columella was finally sutured to the nasal tip at the previously trimmed margin (figure 5).
Figure 5.

The final results after columella reconstruction.
Outcome and follow-up
Figure 6 shows the patient during a 5-year follow-up control. Although residual scarring due to pressure from the nasal prongs used for nCPAP was visible at the alar wings, the patient and his family are very satisfied with the nose structure as well as the nasal tip projection.
Figure 6.
A 5-year postoperative control, oblique and lateral views.
Discussion
The pathogenesis of nasal injuries in premature babies undergoing nCPAP with facial masks and nasal prongs has been described to be similar to decubitus ulcers or pressure sores. nCPAP devices exert continuous and unrelieved local pressure onto the columella which is situated over the anterior maxillary spine and the nasal septum. This pressure compromises perfusion, leading to tissue necrosis.5 Such pressure effects might be further increased by the immature skin of the newborn as well as the end-vascularisation of the columella and nostrils.3
Columella reconstruction is a challenge due to the lack of skin and underlining tissue, its unique contour and scarce vascularity.6 In addition, to gain enough tissue, usually the width of the nasal sill has to be compromised. Most patients seem to consider narrowing of the sill an aesthetic advantage. In this case the tissue used to form the new columella was gained through a ring-like rotation of the anterior nasal floor and sill area.
Rotating the nasal sill with the anterior nasal floor tissue superiorly to create a columella is based on the principle of Cronin's columella lengthening technique.4 7 Alternatively, superiorly pedicled intranasal composite skin flaps might be utilised, as described already in children suffering from holoprosencephaly with complete median cleft,8 type IV according to the classification of DeMyer and colleagues.9
The design of the nasal prongs should be re-evaluated to avoid pressure injuries during nCPAP in premature babies. Robertson et al1 noted the following design flaws which may lead to such trauma: (1) the shape of the prong is not anatomical, (2) their bases do not allow for projection of the columella beyond the alar rim, (3) nasal prongs run perpendicular to the base and do not converge as in infants nasal passages and (4) their bases are closest together where the columella is widest. They thus concluded that tapering nasal prongs would be better.
Currently only three sizes of prongs are available in the market: small, medium and large. These designs are too limited in choice for premature neonates.10 A wider range of shapes and sizes might be of benefit as nose anatomy and dimensions tend to differ between races. The nursing staff needs to be trained on fixation techniques of nCPAP devices, as a proper support of the tubing might avoid excess pressure on the nose. The nasal prongs need to be checked to ensure a proper fit and the hats should to be positioned properly to avoid excessive upward force on the nose.1 The same authors recommended that pressure of the nose prong should be actively relieved for half an hour every 4–6 h.1 If the nose gets red and tender, hydrocolloid dressings (Granuflex, Granubrand BV, Amsterdam, the Netherlands) or silicon sheets (Epi-Derm, Biodermis, Las Vegas, USA) can be used under the nasal prong. These silicon shields significantly reduce rates of nasal injury and decrease its severity by: (1) diminishing the pressure on the columella, dispersing it around the nares and (2) lowering the friction between the prong and skin surface.5
Patient's perspective.
The patient and his family were satisfied with the final aesthetic outcome.
Learning points.
Nasal continuous positive airway pressure in premature babies may rarely lead to necrosis of the columella.
A modified Cronin approach may deliver adequate soft tissue from the nasal sill area to reconstruct a necrotic columella.
Acceptable functional and aesthetic long-term outcomes can be achieved using this minimal invasive surgical technique.
Footnotes
Contributors: YSNJ drafted the initial manuscript, performed subsequent revisions and approved the final manuscript as submitted. RAZ drafted the initial manuscript, performed subsequent revisions and approved the final manuscript as submitted. SYH assisted in performing the surgery, collected photographic records and approved the final manuscript as submitted. KWB performed the surgery, revised the manuscript and approved the final version as submitted.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Robertson NJ, McCarthy LS, Hamilton PA, et al. Nasal deformities resulting from flow driver continuous positive airway pressure. Dis Child Fetal Neonatal Ed 1996;75:F209–F12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yong SC, Chen SJ, Boo NY. Incidence of nasal trauma associated with nasal prong versus nasal mask during continuous positive airway pressure treatment in very low birthweight infants: a randomised control study. Arch Dis Child Fetal Neonatal Ed 2005;90:F480–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fischer C, Bertelle V, Hohlfeld J, et al. Nasal trauma due to continuous positive airway pressure in neonates. Arch Dis Child Fetal Neonatal Ed 2010;95:F447–F51 [DOI] [PubMed] [Google Scholar]
- 4.Cronin TD, Denkler KA, Cronin ED. Correction of secondary unilateral and bilateral nasal deformities: Cronin technique. In: Bardach J, Morris HL. eds Multidisciplinary management of cleft lip and palate. Phiadalphia: WB Saunders Co, 1990:264 [Google Scholar]
- 5.Günlemez A, Isken T, Gökalp AS, et al. Effect of silicon gel sheeting in nasal injury associated with nasal CPAP in preterm infants. Indian Pediatr 2010;47:265–7 [DOI] [PubMed] [Google Scholar]
- 6.Sherris DA, Fuerstenberg J, Danahey D, et al. Reconstruction of the nasal columella. Arch Facial Plast Surg 2002;4:42–6 [DOI] [PubMed] [Google Scholar]
- 7.Bütow K-W. Primary surgical repair of the lip and nose. Treatment of facial cleft deformities. St Louis, Tokyo: Ishiyaku EuroAmerica Inc, 1995:47–8 [Google Scholar]
- 8.Bütow K-W. Construction of the congenitally missing columella in midline clefts. J Craniomaxillofac Surg 2007;35:287–92 [DOI] [PubMed] [Google Scholar]
- 9.Sadove AM, Eppley BL, DeMyer W. Single stage repair of the median cleft lip deformity in holoprosencephaly. J Craniomaxillofac Surg 1989;17:363–6 [DOI] [PubMed] [Google Scholar]
- 10.Maruccia M, Fanelli B, Ruggieri M, et al. Necrosis of the columella associated with nasal continuous positive airway pressure in a preterm infant. Int Wound J 2014;11:335–6 [DOI] [PMC free article] [PubMed] [Google Scholar]



