Abstract
Salivary gland tumours comprise almost 5% of head and neck malignancies. Minor salivary gland tumours account for 10–15% of all salivary gland neoplasms and are usually malignant. The second most common minor salivary gland tumour (12–40% globally) is mucoepidermoid carcinoma. Mucoepidermoid carcinoma is more frequent in females, occurs in the fifth decade of life and is usually found in the parotid gland. However, the palate is a frequent site when it occurs in the minor glands. We report a case of a high-grade variant of mucoepidermoid carcinoma in the right retromolar trigone of a 21-year man which was treated with wide excision of the tumour with a 1.5 cm margin. Reconstruction was done with a buccal fat pad posteriorly with a pedicled lateral tongue flap. Temporal stripping and right coronoidectomy was carried out in case of post-surgical wound contraction. The patient is currently under periodic review.
Background
A review of the literature indicates that mucoepidermoid carcinoma (MEC) is the second most common malignant minor salivary gland neoplasm. The retromolar area is a rare site for the presentation: a review of 265 minor salivary gland tumours showed only 6.4% occurred in the retromolar region.1 The authors here report a case of high-grade MEC in a 21-year-old man in the right retromolar trigone. After 8 months of follow-up there have been no complications or lesion recurrence.
Case presentation
A 21-year-old man presented with a 2-month history of swelling in his lower right back teeth region. The swelling was insidious in onset and had gradually grown to its current size. The patient had a 15-day history of pain which was sudden in onset, dull and continuous, and was worse while eating food. His past medical, dental, social and family history was unremarkable. On intraoral examination, a solitary well-defined oval-shaped erythematous swelling of size 1.0×0.8 cm was noticed in the right retromolar area distal to 48 extending anteriorly from the distal surface of 48 to the anterior part of the right faucial pillars posteriorly; medially it extended to the depth of the right lingual vestibule, and laterally into the right retromolar trigone musculature (figure 1). The surface of the swelling was depressed at the centre (mimicking a sinus tract), and was irregular with everted margins. The swelling was soft to firm, and was tender on palpation associated with bleeding.
Figure 1.

Clinical photograph showing a solitary erythematous swelling in the right retromolar area.
Investigations
An orthopantomogram revealed a permanent set of dentition without any osseous invasion (figure 2). A mandibular axial CT revealed a soft tissue expansile mass 1.6×1.2 cm in size in the right retromolar trigone without any bony invasion (figure 3). Haematological evaluation revealed normal values after which an incisional biopsy was performed in the perilesional area under local anaesthesia and the tissue sample was submitted for histopathological evaluation. An H&E stained microscopic tissue section showed overlying dysplastic stratified squamous epithelium with underlying connective tissue exhibiting strands, cords and whorls of squamous cells which were polygonal to ovoid in shape with eosinophilic cytoplasm and predominantly vesicular nuclei. Duct-like areas of varying sizes with a central lumen were also noted. A few large cells with foamy cytoplasm and prominent nuclei resembling mucous cells were also evident. At the periphery, salivary gland tissue exhibited loss of acinar and lobular architecture. The lesional tissue was mainly composed of epidermoid cells with very few mucous cells and minimal cystic changes, suggestive of MEC (figure 4). TNM staging of the lesion was T1N0M0.
Figure 2.

Orthopantomograph revealing permanent dentition without any osseous invasion of the tumour.
Figure 3.
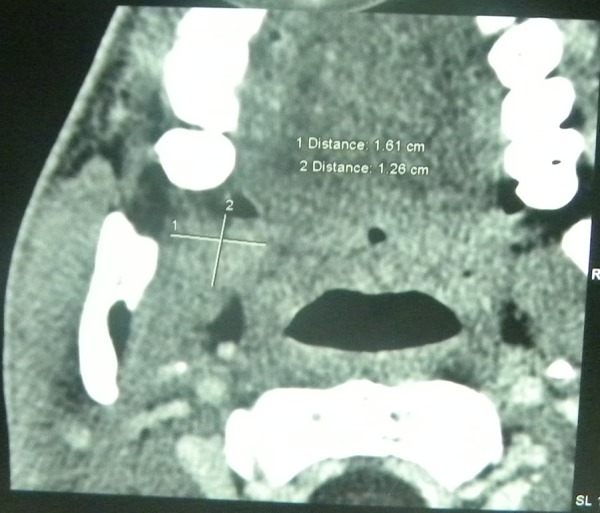
Mandibular axial CT revealing a soft tissue expansile mass in the right retromolar area.
Figure 4.
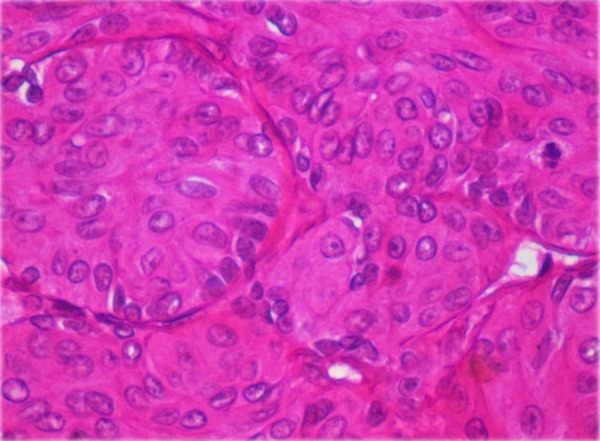
High-powered microscopic view showing epidermal cells with very few mucous cells and minimal cystic changes suggestive of mucoepidermoid carcinoma.
Differential diagnosis
Malignant minor salivary gland tumour and metastatic tumour was considered in the differential diagnosis.
Salivary gland tumours comprise almost 5% of head and neck malignancies. Minor salivary gland tumours account for 10–15% of all salivary gland neoplasms and most are malignant.2 Therefore, in light of the history, clinical presentation and an overview of the literature, malignant minor salivary gland tumour was considered.
Secondary malignancies in the jaw bones represent approximately 1–3% of all metastatic tumours, and are more than 2.5–5 times as common as metastatic tumours in oral soft tissues with a predominance in the posterior mandible and retromolar trigone.3 The present case suggested metastatic tumour should be considered as it was in the retromolar region as a soft tissue mass with no any obvious aetiology based on the patient's history.
Treatment
After presurgical evaluation, the entire procedure was carried out under general anaesthesia. Surgical intervention included wide excision of the tumour with a 1.5-cm margin all around (figures 5 and 6). Reconstruction was carried out with a buccal fat pad posteriorly with a pedicled lateral tongue flap (figures 7 and 8). Temporal stripping and right coronoidectomy was done in case of trismus due to post-surgical wound contraction (figure 9). In addition, 17, 18, 47 and 48 were extracted in order to prevent graft impingement (figure 10).
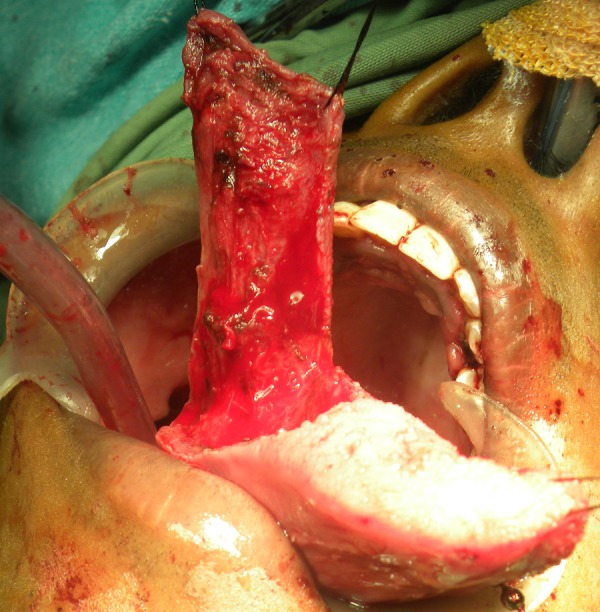
Figure 5.

Intra-operative photograph showing a wide surgical excision around the tumour.
Figure 6.
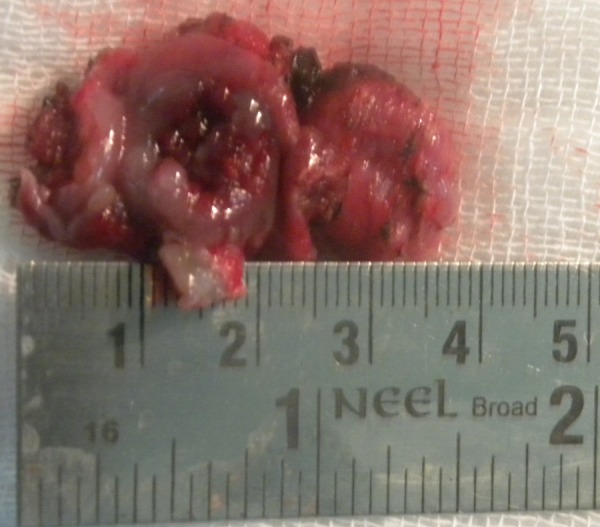
Excised tumour.
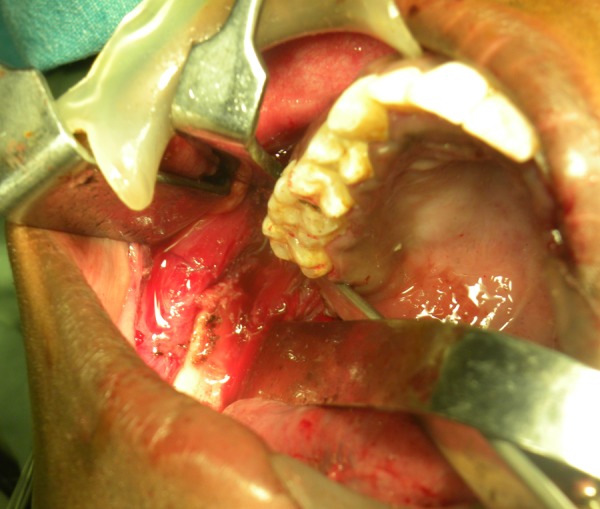
Figure 7.
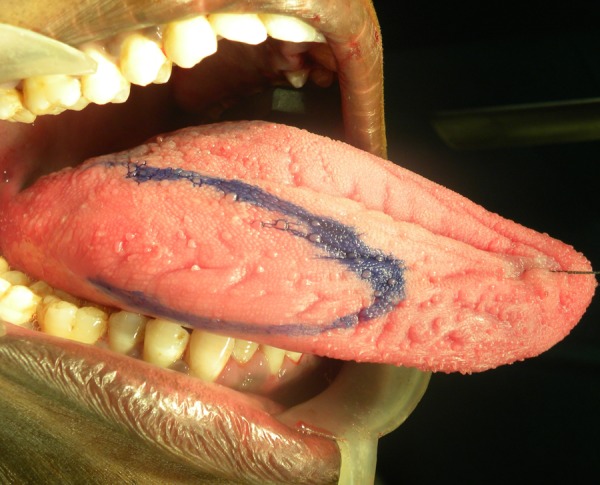
Presurgical markings before elevation of a pedicled lateral tongue flap.
Figure 8.
Surgical session showing the dissected flap.
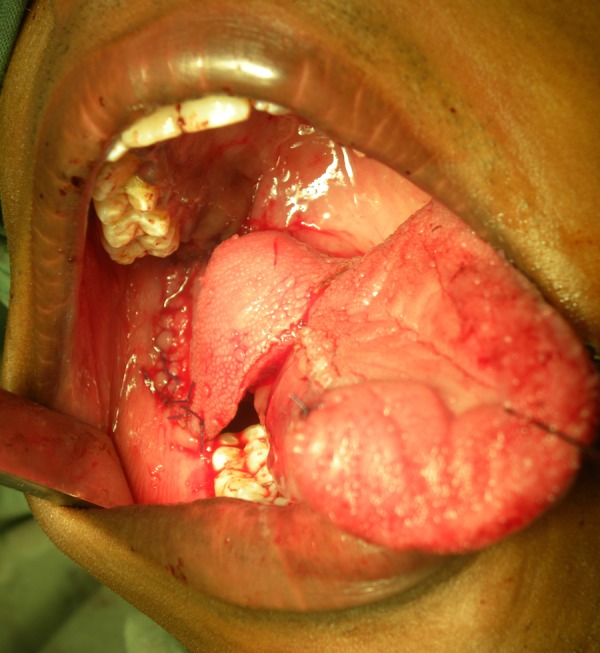
Figure 9.
Photograph showing post-temporal stripping and right coronoidectomy.
Figure 10.
Graft in position.
Outcome and follow-up
After a 6-month follow up, prognosis was excellent and the patient was lesion free and under periodic review. Mouth opening, and the graft recipient and the donor sites were symptom free with normal healing (figures 11–13).
Figure 11.

Follow-up after 3 months.
Figure 12.

Symptom-free graft recipient site with normal healing.
Figure 13.

Post-operative orthopantomograph revealing right coronoidectomy.
Discussion
Epithelial neoplasms originating in the minor salivary glands comprise approximately 10–15% of all salivary gland neoplasms.4 MEC is the most common malignant salivary gland tumour and usually affects the parotid and minor salivary glands of adults.5 Although it accounts for 30% of all cancers of the salivary glands, it accounts for only 10% of all salivary gland tumours and less than 5% of head and neck cancers. Slightly more than 50–60% of these tumours arise in the major salivary glands, with more than 80% occurring in the parotid gland, 8–13% in the submandibular gland, 2–4% in the sublingual gland and the remainder in minor salivary glands, mostly in the palate.6 Other sites are the buccal mucosa, tongue and retromolar area. MEC has a slight female preponderance6–8 and is more common in adults in their fourth to sixth decades, with the highest prevalence during the fifth decade of life.8 The most common presenting symptom is a slowly enlarging painless mass of several years’ duration clinically mimicking a pleomorphic adenoma or other benign neoplasm. Pain or facial nerve palsy may develop, usually in association with high-grade tumours. Low-grade malignancy is characterised by a slow-growing painless swelling which rarely exceeds 5 cm, while high-grade malignancies are rapidly growing, painless, infiltrate into adjacent tissues, and are associated with distant metastases and extra-oral ulceration.7 Minor salivary gland tumours are asymptomatic, fluctuant and red/blue in appearance.6 While all MECs are capable of metastasising, metastases most often occur in high-grade lesions. In addition to lymph nodes, the usual sites of metastases are the lungs and bone.
The origin of MEC is thought to be pluripotent cells of the excretory ducts of glandular structures and the tumour consists of mucous, intermediate and epidermoid cells.5 8 9 Histopathologically, it is classified into three grades, low, intermediate and high, with low grade (48%) being more common than high grade (38.7%) and intermediate grade (13.3%) least common.8 These three histopathological grades are based on degree of cytological atypia, amount of cyst formation, and relative numbers of mucous, epidermoid and intermediate cells.7 Low-grade tumours have a higher ratio of mucous cells and are less aggressive lesions, while high-grade tumours have a smaller proportion of mucous cells and are considered to be a more malignant tumour with poorer prognosis.10 11
MECs are best treated by surgery, the extent of which depends on location, size and histopathological grading.6 10 Local resection is the treatment option for less aggressive low-grade tumours, while high-grade tumours require wide resection with involvement of adjacent structures.10 Treatment for MEC in minor salivary glands is primarily surgical.
Radiotherapy should be used only in selected cases because of long term adverse effects; the role of chemotherapy in the management of MEC is generally reserved for patients with aggressive local or metastatic disease which is not amenable to surgical or radiation therapy.9 Prognosis is dependent on clinical stage, site, grading, and adequacy of surgery.12 The 5-year survival rate has been reported to be as high as 95% in low-grade tumours, and 50% in intermediate/high-grade tumours.13
Learning points.
This rare presentation of high-grade variant mucoepidermoid carcinoma in the right retromolar region in a 21-year-old man is thought to be the first described in the literature.
Mucoepidermoid carcinoma should be considered in the differential diagnosis for a swelling of short duration in the retromolar region so an early diagnosis can be made.
Despite the availability of treatments such as micro-vascular surgery, wide surgical excision of the tumour along with temporal stripping and coronoidectomy is of prognostic value in patients from low socioeconomic backgrounds, thereby preventing post-surgical complications such as limited mouth opening.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lutcavage GJ, Schaberg SJ, Fulbright DK, et al. Retromolar trigone mass. J Oral Maxillofac Surg 1993;51:1024–9 [DOI] [PubMed] [Google Scholar]
- 2.Ranganath MK, Matmari V, Narayanaswamy UD, et al. Mucoepidermoid carcinoma presenting as a retromolar mucocele. Ann Maxillofac Surg 2011;1:66–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wood NK, Goaz PW, Kallal R. Multilocular Radiolucencies in Differential Diagnosis of Oral and Maxillofacial Lesions 5th edn 2006:346–7 [Google Scholar]
- 4.Ritwik P, Cordell KG, Brannon RB. Minor salivary gland mucoepidermoid carcinoma in children and adolescents: a case series and review of the literature. J Med Case Rep 2012;6:182–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pires FR, Chen SY, Da Cruz Perez DE, et al. Cytokeratin expression in central mucoepidermoid carcinoma and glandular odontogenic cyst. Oral Oncology 2004;40:545–51 [DOI] [PubMed] [Google Scholar]
- 6.Neville WB, Damm DD, Allen CM, et al. Salivary gland pathology. 2nd edn Oral And Maxillofacial Pathology, 2002:420–3 [Google Scholar]
- 7.Rajendran R. Tumors of the salivary glands. 6th edn Shafer's Text book of Oral Pathology, 2009:232–4 [Google Scholar]
- 8.Qureshi SM, Janjua OS, Janjua SM. Mucoepidermoid carcinoma: a clinico-pathological review of 75 cases. Int J Oral Maxillofac Pathol 2012;3:5–9 [Google Scholar]
- 9.Ali SA, Memon AS, Shaik NA, et al. Mucoepidermoid carcinoma of parotid presenting as unilocular cyst. J Ayub Med Coll Abbottabad 2008;20:141–2 [PubMed] [Google Scholar]
- 10.Kumar AN, Nair PP, Thomas S, et al. Mucoepidermoid carcinoma of sublingual gland: a malignant neoplasm in an uncommon region. BMJ Case Rep 2011;2011:pii: bcr0220113864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fox PC, Ship JA. Salivary gland diseases. 11th edn Burket's oral medicine, 2008:219–20 [Google Scholar]
- 12.Thompson LDR. Mucoepidermoid carcinoma. ENT J 2005;84:762–3 [PubMed] [Google Scholar]
- 13.Jarvi SJ, Giangrande V, Brennan PA. Mucoepidermoid carcinoma of the tonsil: a very rare presentation. Acta Otorhinolaryngol Ital 2013;33:286–8 [PMC free article] [PubMed] [Google Scholar]


