Abstract
The association between urological malignancies and paraneoplastic syndromes has been well documented. We report a case of recurrent dermatomyositis manifesting as a sign of metastatic recurrence of non-muscle-invasive transitional cell carcinoma of the bladder, a relationship which has only been referred to in a few reports. The case highlights a few important clinical challenges; firstly, the importance of thorough investigation for underlying malignancy in patients with dermatomyositis, as successful treatment of such malignancy can lead to resolution of paraneoplastic symptoms, and secondly, a high index of suspicion of recurrence in cases where paraneoplastic manifestations recur. Metastatic pulmonary recurrence without local evidence of disease at a follow-up of 4 years makes this case unique. Moreover, in the light of our experience and reported literature, a framework is suggested to approach such a diagnostic dilemma in the future. Description of the case will guide clinicians in the future, in case they encounter such an unusual clinical scenario. This could also serve as a hypothesis-generating source for designing future research as well.
Keywords: Bladder cancer, bladder neoplasm, dermatomyositis, paraneoplastic, transitional cell carcinoma
INTRODUCTION
Dermatomyositis (DM) is an inflammatory myopathy characterized by proximal muscle weakness and pathognomic cutaneous manifestations (heliotrope rash, periorbital edema, Gottron's papules). It is associated with underlying malignancy in around 25% of adults, most commonly males in the sixth to eighth decades.[1,2] The most frequently involved tumors are ovarian and lung, whereas an association with bladder cancer is a relatively rare phenomenon.[1,2] The pathogenesis of paraneoplastic DM is still relatively unknown, although there is some evidence to support the involvement of humoral and cell-mediated immune systems, and the presence of tumor antigens provoking an autoimmune response.[2] Treatment of DM is empirical, often involving a combination of steroids and immunomodulatory drugs, including azathioprine and cyclophosphamide.[2] Where DM is associated with underlying malignancy, tumor therapy may lead to resolution of DM.[2] Interestingly, a reverse relationship also exists, whereby a flare of DM occurs with tumor recurrence,[3,4,5] an association that is demonstrated in this report.
CASE REPORT
A 67-year-old woman with recently diagnosed DM was referred by her general practitioner to the urology team with a 2-month history of frank hematuria in December 2007. Both intravenous urogram (IVU) and renal tract ultrasound scan (USS) were normal. A chest X-ray was also unremarkable [Figure 1a]. Flexible cystoscopy, however, revealed a 4-cm papillary tumor on the posterior wall of the urinary bladder. She underwent transurethral resection of bladder tumor (TURBT) with a single dose of intravesical mitomycin-C. Histology confirmed a poorly differentiated transitional cell carcinoma (TCC) of the bladder (G3pT1). Six weeks later, a repeat cystoscopy, resection of scar, and multiple bladder biopsies were carried out, with no evidence of residual tumor on histopathology. The option of adjuvant intravesical therapy was discussed at this time; however, the patient declined. Her DM responded and cystoscopic surveillance showed no recurrences for 4 years. A computed tomography (CT) scan of the chest, as part of her disease follow-up [Figure 1b], revealed only pulmonary fibrosis with no evidence of lung masses or nodules.
Figure 1.
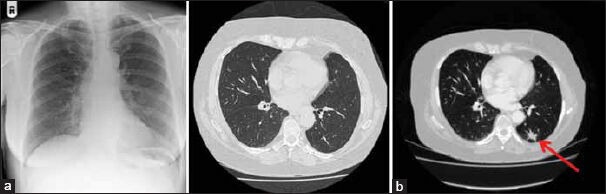
(a) Radiological imaging at the time of bladder cancer diagnosis. Left: Chest X-ray; right: CT chest showing minor fibrosis at the right lung base and right middle lobe. No lung masses identified on either investigation. (b) CT chest at the time of DM recurrence showing pulmonary nodule (red arrow)
Four years after her initial diagnosis of bladder cancer, however, she had a recurrence of DM. Although she did not complain of any urinary symptoms, physicians advised reinvestigation to rule out a recurrence of bladder cancer. A CT urogram and cystoscopy with biopsy were normal; histology showed normal bladder mucosa. In the absence of any positive findings, a CT chest was carried out; this identified a 2-cm lesion in the lower lobe of the left lung [Figure 2]. Further clarification was sought by positron emission tomography (PET) scanning. The radiological impression was of a bronchogenic cancer and the patient was referred for lung lobectomy. Lung histology was reviewed by two independent pathologists and agreed to be metastatic TCC of the bladder [Figure 2]. Six months later, the patient developed bone metastases in the ribs [Figure 3a] with associated fracture and was treated with chemotherapy. Subsequently, she was found to have multiple brain metastases [Figure 3b] and required radiotherapy. Following chemoradiotherapy, repeat CT scans [Figure 3b] showed disease remission with a healed previous fractured rib and reduction in brain metastases. She is alive with some residual disease, however, with no recurrences in the bladder or urinary tract.
Figure 2.
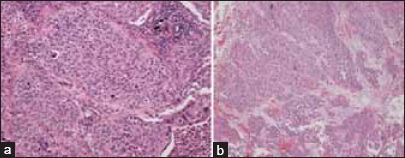
(a) Photomicrograph of tumor resected from the left lower lobe showing a carcinoma with morphological features in keeping with metastatic transitional cell carcinoma. This interpretation was supported by immunohistochemical staining which showed characteristic expression of CK7, CK20, and nuclear staining for p63. Similar appearing metastatic carcinoma was also identified within hilar lymph nodes removed at the time of surgery (hematoxylin and eosin stain, ×100 original magnification). (b) Photomicrograph of tumor resected from the urinary bladder showing transitional cell carcinoma (hematoxylin and eosin stain, ×100 original magnification)
Figure 3.
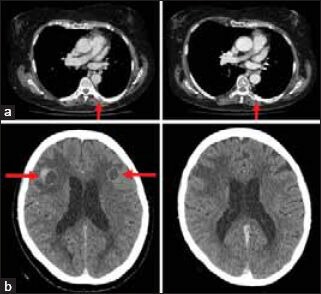
(a) CT chest showing rib metastasis pre- and post-chemotherapy. Left: Area of bone destruction on posterior aspect of left 7th rib in keeping with metastasis (red arrow); right: Healed pathological rib fracture with evidence of callus and bone remodeling (red arrow). (b) CT head showing brain metastases pre- and post-radiotherapy. Left: Pre-radiotherapy; enhancing lesions in left and right frontal lobes consistent with metastases (red arrows). Right: Post-radiotherapy; reduction in the size of frontal lobe metastases
DISCUSSION
TCC of the bladder can be associated with various paraneoplastic syndromes, often manifested in endocrinological, neuromuscular, or hematological forms.[6] Despite this, paraneoplastic DM secondary to bladder TCC has been observed very rarely.[2,3,4,5,6,7,8,9,10] A literature search of the PubMed database (MeSH terms: Urinary bladder neoplasms, transitional cell carcinoma, dermatomyositis) revealed only 12 published reports documenting an association between DM and TCC of the bladder. The recurrence of DM as a first sign of metastatic TCC is extremely rare.
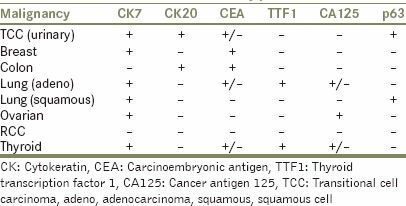
Owing to the morphological overlap between carcinomas from different organs, it can be extremely challenging to determine the origin of metastatic disease. Immunohistochemical methods are often employed to provide the answer. A significant problem, however, is that immunostaining patterns show substantial overlap between different tumors. In order to combat this, we use a combination of immunohistochemical markers to discriminate metastases originating from various sites [Table 1] with the CK7+/CK20+/p63+/CA125– immunophenotype being highly characteristic of bladder TCC.[11,12,13]
Table 1.
Characteristic immunoreactivity patterns in carcinomas
The relationship between DM and malignancy is often complex, particularly in respect to clinical presentation, diagnosis, and treatment. The signs and symptoms of paraneoplastic DM may precede, overlap, or follow the diagnosis of underlying malignancy.[5] Furthermore, relapses of DM following tumor therapy are often an indicator of tumor recurrence or progression and warrant reinvestigation.[3,4,5] With TCC of the bladder, relapses of DM have been found to occur mainly with local recurrence of tumors;[3,4] however, there also appears to be one reported case associated with the development of metastatic disease.[5] This isolated case, described by Federman et al., was a 68-year-old man who redeveloped symptoms of DM 1 year after successful therapy for bladder TCC; he was found to have developed liver metastases. In our case, we describe an unusual representation of DM associated with the development of a single pulmonary metastasis; this occurred after 4 years of DM remission following tumor resection. This case further emphasizes the particular importance of thorough reinvestigation of patients who have relapses of DM. Without comprehensive investigation in this patient, it is possible that a diagnosis of metastatic bladder TCC may have been missed, especially considering the absence of urinary symptoms and positive histology to suggest local recurrence.
CONCLUSION
Paraneoplastic DM associated with TCC of the bladder is rare. It is important to search thoroughly for neoplasms in patients with DM. Treatment of underlying malignancy can lead to resolution of DM symptoms. Relapses of DM following successful tumor therapy require reinvestigation for tumor recurrence or progression, even in the absence of symptoms of malignancy.
Footnotes
Source of Support: Urology Research Funds
Conflict of Interest: None.
REFERENCES
- 1.Lakhanpal S, Bunch TW, Ilstrup DM, Melton LJ., 3rd Polymyositis-dermatomyositis and malignant lesions: Does an association exist? Mayo Clin Proc. 1986;61:645–53. doi: 10.1016/s0025-6196(12)62030-8. [DOI] [PubMed] [Google Scholar]
- 2.Mallon E, Osborne G, Dinneen M, Lane RJ, Glaser M, Bunker CB. Dermatomyositis in association with transitional cell carcinoma of the bladder. Clin Exp Dermatol. 1999;24:94–6. doi: 10.1046/j.1365-2230.1999.00415.x. [DOI] [PubMed] [Google Scholar]
- 3.Almog Y, Ben-Yehuda A, Ben-Chetrit E. Dermatomyositis associated with the recurrence of transitional cell carcinomas and Kaposi's sarcoma. Clin Exp Rheumatol. 1991;9:285–8. [PubMed] [Google Scholar]
- 4.Sabio JM, Vargas-Hitos JA, Jimenez-Alonso J. Paraneoplastic dermatomyositis associated with bladder cancer. Lupus. 2006;15:619–20. doi: 10.1177/0961203306071923. [DOI] [PubMed] [Google Scholar]
- 5.Federman DG, Radonich M, Kirsner RS. Fatal bladder cancer and dermatomyositis. South Med J. 2000;93:492–3. [PubMed] [Google Scholar]
- 6.Apaydin R, Gul U, Bahadir S, Siviloglu C, Ofluoglu I. Dermatomyositis without muscle weakness associated with transitional cell carcinoma of the bladder. J Eur Acad Dermatol Venereol. 2002;16:172–4. doi: 10.1046/j.1468-3083.2002.00392_2.x. [DOI] [PubMed] [Google Scholar]
- 7.Rankin WR, Herman JR. Rapidly progressive transitional cell carcinoma associated with dermatomyositis. J Urol. 2002;167:639–40. doi: 10.1016/S0022-5347(01)69103-1. [DOI] [PubMed] [Google Scholar]
- 8.Robinson AJ, Alcock CJ. Dermatomyositis in association with transitional cell carcinoma of the bladder. Clin Oncol (R Coll Radiol) 2001;13:50–1. doi: 10.1053/clon.2001.9214. [DOI] [PubMed] [Google Scholar]
- 9.Russ BW, English JC, Jr, King DH, Halbach DP. Amyopathic dermatomyositis associated with transitional cell carcinoma of the bladder. Cutis. 1999;63:73–6. [PubMed] [Google Scholar]
- 10.Talanin NY, Bushore D, Rasberry R, Rudolph T, Tuli M, Friedman-Musicante R. Dermatomyositis with the features of inclusion body myositis associated with carcinoma of the bladder. Br J Dermatol. 1999;141:926–30. doi: 10.1046/j.1365-2133.1999.03172.x. [DOI] [PubMed] [Google Scholar]
- 11.Somani BK, Prita D, Grant S, Nabi G, N'dow J. Herpetiform cutaneous metastases from transitional cell carcinoma of the urinary bladder: Immunohistochemical analysis. J Clin Pathol. 2006;59:1331–3. doi: 10.1136/jcp.2005.031500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang A, Cai J, Miranda G, Groshen S, Skinner D, Stein JP. Usefulness of CA 125 as a preoperative prognostic marker for transitional cell carcinoma of the bladder. J Urol. 2004;172:2182–6. doi: 10.1097/01.ju.0000143487.20280.ed. [DOI] [PubMed] [Google Scholar]
- 13.Harlamert HA, Mira J, Bejarano PA, Baughman RP, Miller MA, Whitsett JA, et al. Thyroid transcription factor-1 and cytokeratins 7 and 20 in pulmonary and breast carcinoma. Acta Cytol. 1998;42:1382–8. doi: 10.1159/000332172. [DOI] [PubMed] [Google Scholar]


